Abstract
Background
Sulphadoxine–pyrimethamine (SP) is widely used as an intermittent preventive treatment for malaria in pregnancy (IPTp). However, pharmacokinetic studies in pregnancy show variable and often contradictory findings. We describe population and trimester-specific differences in SP pharmacokinetics among Ugandan women.
Methods
SP (three tablets) were administered to 34 nonpregnant and 87 pregnant women in the second trimester. Seventy-eight pregnant women were redosed in the third trimester. Blood was collected over time points ranging from 0.5 h to 42 days postdose. Data on the variables age, body weight, height, parity, gestational age, and serum creatinine, alanine transaminase and albumin levels were collected at baseline. Plasma drug assays were performed using high-performance liquid chromatography with ultraviolet detection. Population pharmacokinetic analysis was done using NONMEM software.
Results
A two-compartment model with first-order absorption and a lag time best described both the sulphadoxine and pyrimethamine data. Between trimesters, statistically significant differences in central volumes of distribution (V2) were observed for both drugs, while differences in the distribution half-life and the terminal elimination half-life were observed for pyrimethamine and sulphadoxine, respectively. Significant covariate relationships were identified on clearance (pregnancy status and serum albumin level) and V2 (gestational age) for sulphadoxine. For pyrimethamine, clearance (pregnancy status and age) and V2 (gestational age and body weight) were significant. Considering a 25 % threshold for clinical relevance, only differences in clearance of both drugs between pregnant and nonpregnant women were significant.
Conclusion
While clinically relevant differences in SP disposition between trimesters were not seen, increased clearance with pregnancy and the increasing volume of distribution in the central compartment with gestational age lend support to the revised World Health Organization guidelines advocating more frequent dosing of SP for IPTp.
Key Points
| Clinically significant differences in sulphadoxine–pyrimethamine disposition between the second and third trimesters of pregnancy were not observed. |
| Pregnancy and decreasing plasma albumin levels significantly affected clearance, while increasing gestational age significantly affected the central volumes of distribution of both drugs. |
| These findings lend support to the revised World Health Organization guidelines for intermittent preventive treatment for malaria in pregnancy, advocating more frequent dosing of sulphadoxine–pyrimethamine. |
Introduction
In Africa, pregnant women are up to 12 times as likely to contract malaria as their nonpregnant counterparts [1]. This translates into an annual risk burden affecting more than 32 million pregnancies [2]. Malaria contributes significantly to adverse pregnancy outcomes, including maternal anemia, low birth weight (LBW), and pregnancy loss [1]. In order to mitigate these effects, the World Health Organization (WHO) has, since 2004, recommended the use of sulphadoxine–pyrimethamine (SP) as intermittent preventive treatment in pregnancy (IPTp) [3]. The concept of IPTp involves administration of a curative dose of an antimalarial drug to asymptomatic pregnant women at predefined intervals.
While early successes with SP IPTp led to its wide adoption [4], recent concerns over the spread of SP resistance across East and Southern Africa have led to calls for alternative drugs [5–7]. However, despite the demonstrated efficacies of other antimalarial drugs, practical alternatives to SP have remained a challenge [8, 9]. This has been mainly due to implementation barriers such as cost, user acceptability, and convenience of administration, all of which are critical for the success of any IPTp alternative [10]. Moreover, contrary to the above concerns, several reviews [11–13] and recent clinical studies [14–16] have consistently shown that SP continues to offer substantial benefits even in areas with considerable presence of resistance mutations. These benefits have included not only improvements in pregnancy outcomes but also significant reductions in neonatal and infant mortality [17, 18]. These observations suggest that the impact of resistance on the efficacy of SP IPTp is probably overrated and that other determinants of efficacy may be equally important. In fact, mathematical models and clinical studies suggest that geographic differences in acquired antimalarial immunity are a far better predictor of SP efficacy than known molecular markers of resistance [19, 20]. Furthermore, daily prophylaxis with antifolates remains effective against malaria even among human immunodeficiency virus (HIV)-positive children and adults living in areas with high prevalence rates of known resistance-mediating mutations [21, 22].
Until recently, pregnant women were not eligible to participate in pharmacokinetic studies, because traditional methods, involving intense sampling designs, attracted safety and ethical concerns. As such, dosing of antimalarial drugs in pregnancy remained largely empirical. In recent times, however, population pharmacokinetic methods employing sparse sampling designs have provided valuable insights into the pharmacokinetics of antimalarials during pregnancy. While it is now generally appreciated that physiologic changes in pregnancy significantly alter the pharmacokinetics of antimalarial drugs [23–25], several knowledge gaps on the disposition of individual drugs remain. In the case of SP, recent studies have yielded variable and sometimes contradictory findings. For instance, studies from Western Kenya [26] and the north coast of Papua New Guinea [27] have reported clinically significant reductions (30–40 %) in sulphadoxine exposure during pregnancy, in comparison with nonpregnant women. On the other hand, no difference in pyrimethamine exposure was noted among Kenyan women, and yet significantly lower exposure was reported among Papua New Guinean women. In the latter case, reduced exposure was associated with a 38 % treatment failure rate (Plasmodium falciparum) at day 28 [27]. Other than methodologic differences, genetic differences in SP metabolism may underlie these disparities, as has previously been highlighted [28, 29]. In another study, which pooled data from four African countries, pyrimethamine exposure in two countries was shown to be higher during pregnancy, in comparison with postpartum levels [30]. Of peculiar note was the large variability in pharmacokinetic parameters across the four study sites—a phenomenon the authors attributed to pharmacogenetic differences across the continent [30]. Previously, it has been suggested that the increase in physiologic changes in pregnancy occur gradually during gestation [31, 32]. As such, we hypothesized that this would lead to trimester-specific differences in SP disposition—a phenomenon that could possibly have contributed to the conflicting pharmacokinetic literature above. If present, such differences would allow for trimester-specific dose optimization with reference to the nonpregnant state. This study therefore sought to describe trimester and other sources of variability in SP pharmacokinetics among pregnant women. In addition, we sought to model and propose dose modifications that may be required to obtain similar drug exposure in the second and third trimesters of gestation. However, the differences identified in this study were considered clinically nonrelevant and, as such, dose-modification simulations were not performed. Therefore, this study presents population pharmacokinetics with findings limited to the first objective alone.
Materials and Methods
Study Design, Enrollment Criteria, and Sample Size Estimation
This was a population pharmacokinetic study conducted in pregnant and nonpregnant Ugandan women. Between May and October 2013, pregnant women attending the general antenatal clinic and nonpregnant female students from the School of Nursing and Midwifery at Mulago Hospital were invited to participate. Women were enrolled into the study provided that (1) they either had a pregnancy of at least 16 weeks’ gestation or were not pregnant at all; (2) they were HIV negative; (3) they had no history of SP use in the current pregnancy; (4) they had no history of allergy to SP; (5) they had no chronic illness directly or indirectly related to pregnancy; and (6) follow-up was feasible. Follow-up was considered feasible if the participant resided within a radius of 10 km from the study site, had a contact telephone number and was willing to make return visits. In order to control for unaccounted for—but possibly influential—pharmacogenetic differences within the population, the same pregnant women were sequentially dosed in trimester 2 and trimester 3 of gestation.
For the nonpregnant women, the exclusion criteria included use of any hormonal contraceptive during the study period or a positive urine human chorionic gonadotropin (HCG) test. It was considered unethical to enroll HIV-positive pregnant women for the reason that HIV status per se has previously been excluded as a source of variability in SP disposition [26]. Also, Ugandan government policy requires that all HIV-positive pregnant women are immediately started on antiretroviral treatment (ART) and, if necessary, placed on daily cotrimoxazole prophylaxis to prevent malaria and other opportunistic infections. Therefore, concurrent use of SP with ART carried the potential for drug interactions (e.g. enzyme induction/repression) likely to affect the study. Concurrent use of SP with cotrimoxazole would also increase their shared toxicity and further complicate the bioanalytic process.
In calculation of the sample size, the following assumptions were made: (1) that a 25 % difference in the magnitude of a pharmacokinetic parameter between the second and third trimesters would be clinically relevant, as suggested in a previous study [27]; (2) that the volume of distribution (Vd/F) and systemic clearance (CL/F) would increase with increasing gestational age; and (3) that the disposition of SP in both pregnant and nonpregnant women would be similar to that in a previous study [27]. At an α value of 0.05 and a β value of 0.1, up to 40 women would be required per trimester, depending on the pharmacokinetic parameter. However, to allow for up to 50 % loss to follow-up, drawing from a previous study [26], a minimum of 60 women were required per trimester.
Clinical Procedures
The study procedures were identical for both pregnant and nonpregnant participants, except that the initial assessment in the pregnant group included estimation of gestational age by fundal height measurement. Other variables collected included body weight (in kilograms), height (in centimeters), and parity (number of previous pregnancies lasting ≥28 weeks). Prior to dosing, 4 mL of venous blood was taken from each participant for baseline biochemical tests, including serum creatinine, albumin, and alanine transaminase (ALT). An aliquot of plasma was frozen for subsequent drug assay. All participants received a standard dose of three SP tablets (Malaren; Rene Industries, Kampala, Uganda), equivalent to 1500 mg of sulphadoxine and 75 mg of pyrimethamine, in line with the Uganda Ministry of Health guidelines on IPTp [33]. All tablets were swallowed whole with plain water under supervision by a midwife. Subjects were required to fast prior to dosing and to delay food intake for at least 3 h after dosing. In addition to the predose blood sample, participants donated, on average, four additional venous blood samples, drawn randomly across the following time points: 0.5, 1, 2, 3, 4, 6, 24, 48, and 72 h, and 7, 10, 14, 28, and 42 days postdose). All participants were seen as outpatients and observed at the clinic for at least 5 h following drug intake to ensure that any cases of vomiting were noted. During the third trimester, women received a second dose of SP (three tablets), in line with the national guidelines [33], after which the above clinical procedures, including baseline biochemical tests and blood sampling, were repeated. After completion of the 42-day follow-up period, the time interval between the second and third trimester doses varied between 2 and 6 weeks. A participant who happened to be in trimester 3 by the end of 42 days was allowed a 2-week wash-out period before subsequent dosing. On the other hand, if they were still in trimester 2 after 42 days, then, depending on the actual gestational age at that point, the participants waited for 4–6 weeks before the next dosing appointment.
Bioanalytic Methods
Drug analysis was performed at the pharmacokinetic laboratory, Department of Pharmacology and Therapeutics, Makerere University. Plasma was extracted and stored at −80 °C until high-performance liquid chromatography (HPLC) analysis. Pure sulphadoxine, pyrimethamine, sulfamethoxazale, and trimethoprim (Sigma-Aldrich, St. Louis, MO, USA) were kindly donated by the Uganda National Drug Authority. Acetonitrile (Merck, Darmstadt, Germany) and other chemicals were imported or purchased locally, and were all of analytic grade. Extraction and quantification of sulphadoxine and pyrimethamine were as per previously validated methods [34, 35]. Separations were performed on reversed phase C-18 columns: 3.5 µm, 75 mm × 4.6 mm (internal diameter) for sulphadoxine; and 5 µm, 150 mm × 4.6 mm for pyrimethamine (Zobrax® SB; ChromTech, Hagersten, Sweden). Sulfamethoxazale and trimethoprim were respectively used as internal standards for sulphadoxine and pyrimethamine analysis. The mobile phase for sulphadoxine consisted of an acetonitrile–phosphate buffer (20:80, v/v, pH 3). Elution was carried out at 25 °C, using a flow rate of 1.2 mL/minute, and detection was achieved by ultraviolet (UV) absorbance at 254 nm. For pyrimethamine, the mobile phase consisted of a phosphate buffer (0.05 M, pH 5), acetonitrile, and concentrated perchloric acid in the ratio 750:300:2.5, v/v/v, respectively. Elution was carried out at 25 °C, using a flow rate of 1.0 mL/min, and detection was achieved by UV absorbance at 270 nm. The lower limits of quantification were 25 µmol/L and 40 ng/mL for the sulphadoxine and pyrimethamine methods, respectively. The chromatographic system that was used consisted of a system controller (model SCL-10AVP), solvent delivery pump (model LC-10ATVP), auto injector (model SIL-10ADVP), column oven (model CTO-10ASVP), and spectrophotometric UV-vis detector (model SPD-10AVP), all supplied by Shimadzu Corporation, Kyoto, Japan. For both low- and high-quality control standards, the interday coefficient of variation (CV) values were, respectively, 6.11 and 7.69 % (N = 22) for sulphadoxine, and 8.78 and 6.79 % (N = 16) for pyrimethamine.
Ethical Statement
The study protocol was reviewed and approved by the Research Ethics Committee at the School of Medicine, Makerere University (# REC REF 2012-074), and the Mulago Hospital Research Ethics Committee (REF #: MREC 397). All study procedures were done in accordance with the ethical standards of the World Medical Association’s Helsinki Declaration (1964) and the International Conference on Harmonization (ICH) guidelines for Good Clinical Practice. The Uganda National Council for Science and Technology granted permission to conduct the study (REF #: HS 1277).
Data Analysis
Model Development
The data were collected from 34 nonpregnant women and 87 pregnant women enrolled in the second trimester, of whom 78 were redosed and sampled in the third trimester. The 78 women in trimester 3 were treated as different individuals, making a total of 199 who contributed in excess of 1100 observations (approximately five observations per individual). For each drug, a population pharmacokinetic model was built in NONMEM version 7.2 software [36, 37], with the aid of Perl-speaks-NONMEM (PsN 3.4.2) [38]. R software (version 3.0.1) [39] and Xpose4 [40] were used for dataset construction, graphical inspection, and statistical analysis. The first-order conditional estimation method with interaction (FOCE-I) was used. On the basis of visual inspection of the data and a review of the literature, one- and two-compartment models with first-order absorption ± absorption lag time (ALAG) were tested for each drug. The first-order absorption rate constant (KA), CL/F, central volume of distribution (V2/F), peripheral volume of distribution (V3/F), intercompartmental clearance (Q), and ALAG were estimated. All parameters were assumed to be log-normally distributed; hence, interindividual variability in the parameters was modeled as exponential random effects. The models were fitted to log-transformed concentration data and the residual error described with the additive. Model discrimination was based on relative objective function values (OFVs) computed in NONMEM as −2× log likelihood. Precision of parameter estimates and goodness-of-fit (GOF) plots were also used in model discrimination.
Covariate Analysis and Derivation of Secondary Parameter Estimates
Covariate analysis was performed on KA, CL/F, V2/F, and V3/F in a stepwise manner, using the likelihood ratio test at a 5 % significance threshold for forward stepping, followed by a 1 % significance threshold for backward elimination. The covariates age, parity, gestational age, pregnancy status, trimester, height, body weight, and ALT, serum creatinine, and albumin levels were all tested in the model. Because of the gradual increase in the magnitude of the pharmacokinetic changes during pregnancy, it was hypothesized that the key SP pharmacokinetic parameters would differ by trimester; thus, this variable was created from the gestational age data. Body weight and pregnancy status were included in the model for their known influence on clearance, while serum ALT and creatinine were included as surrogate markers for liver and renal function, respectively. Since sulphadoxine and pyrimethamine are highly protein bound, it was biologically plausible that serum albumin levels would influence their disposition. Other covariates, such as gestational age, parity, age, and height, were explored out of scientific curiosity. GOF plots were also inspected in addition to changes in the OFV. Bootstrapping of the covariate modeling step was carried out to ensure that the added covariates were not spurious. This was done by creating 1000 new datasets by resampling with replacement from the original dataset and repeating the covariate step on each new dataset. The inclusion frequency and stability were calculated for each covariate–parameter relationship. A covariate with inclusion frequency of 50 % or more was considered non-spurious and retained in the final conservative model. The distribution half-life (t½α), terminal elimination half-life (t½β), and area under the concentration–time curve (AUC) were calculated post hoc from the CL/F, V2/F, V3/F, and Q estimates.
Model Reliability Testing
Each of the final (reduced) models was fitted to 1000 bootstrap datasets, created by resampling with replacement from the original dataset and the parameters estimated. The summary statistics (mean, median, 2.5th and 97.5th percentiles, minimum, and maximum) for the distribution of each model parameter were obtained. The final model parameter estimates were compared with the mean and percentile 95 % confidence intervals (CIs) of the bootstrap replicates, as described by Ette et al. [41].
Model Validation with Visual Predictive Check
For each drug, a visual predictive check (VPC) was performed using the final covariate model to evaluate correspondence between observations and the model predictions. The distribution quantiles (median and 5th and 95th percentiles) of the observed sulphadoxine or pyrimethamine concentrations were each calculated. The final model was used to simulate 1000 new datasets and used to calculate the 95 % CI for each of the aforementioned quantiles. These quantiles were plotted as lines together with their model-simulated CIs as shaded regions in the plots of observations versus time. The VPCs were stratified on pregnancy status.
Results
Overall, the study procedure and drugs were well tolerated by most participants. One pregnant woman vomited within 1 h of SP intake, and one nonpregnant woman developed a mild skin rash. One pregnant woman discontinued participation in the study because she developed febrile symptoms within 48 h of SP intake. This was later confirmed to be malaria and was treated with a 5-day course of artemether–lumefantrine. Nearly all nonpregnant women (32/34) were nulliparous. Table 1 presents summary statistics for the baseline characteristics for each pregnancy category enrolled in the study. Figure 1 presents concentration–time profiles for both sulphadoxine and pyrimethamine, plotted by pregnancy category.
Table 1.
General characteristics of the study participants, summarized by pregnancy status
| Characteristic/covariable | Nonpregnant (N = 34) | Trimester 2 (N = 87) | Trimester 3 (N = 78) |
|---|---|---|---|
| Number of observations for sulphadoxinea | 172 | 425 | 378 |
| Number of observations for pyrimethaminea | 172 | 418 | 372 |
| Mean age [years (SD)] | 23.7 (4.3) | 22.8 (3.5) | 23.5 (3.7) |
| Median gestational age at dosing [weeks (IQR)] | NA | 20 (18–21) | 28 (28–30) |
| Median body weight [kg (IQR)] | 58.0 (52.9–64.8) | 60.0 (55–66) | 63.5 (59–69.9) |
| Mean height [cm (SD)] | 163.5 (5.95) | 158.8 (5.79) | 158.3 (5.56) |
| Mean serum albumin level [g/dL (SD)] | 44.6 (2.36) | 37.4 (2.74) | 34.1 (2.89) |
| Mean serum creatinine level [µmol/L (SD)] | 71.5 (13.32) | 50.22 (8.84) | 48.0 (10.89) |
| Median ALT level [U/L (IQR)] | 3.3 (1.9–4.6) | 4.0 (3–6) | 3.9 (2.6–5.7) |
ALT alanine transaminase, IQR interquartile range, NA not applicable, SD standard deviation
aExcludes data points at time zero
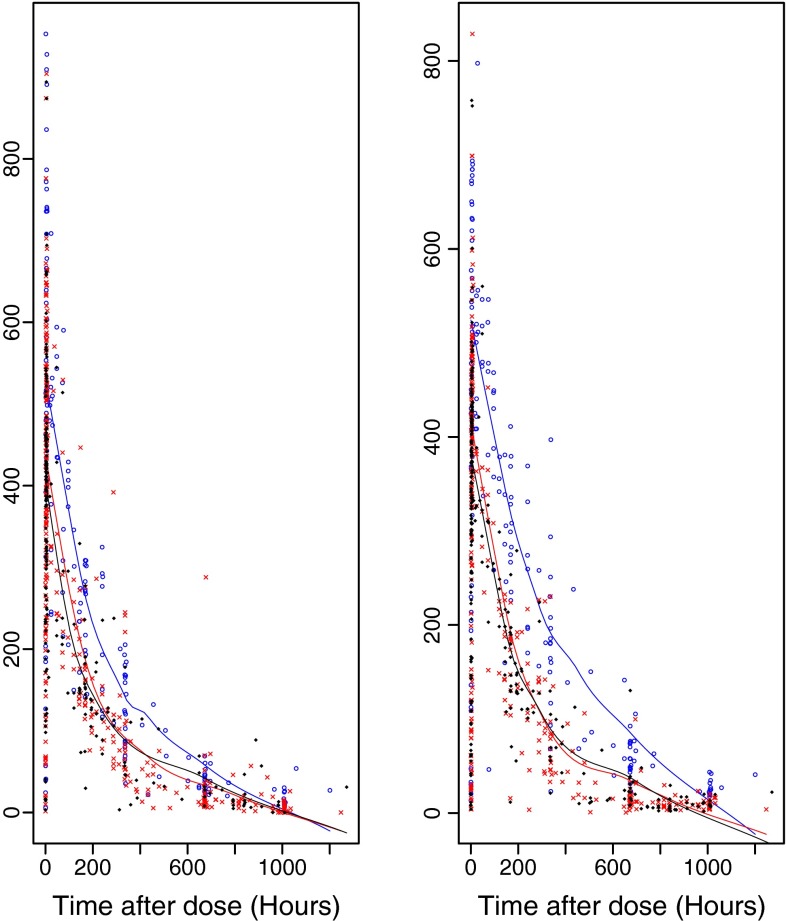
Fig. 1.
Concentration–time profiles for pyrimethamine (left panel) and sulphadoxine (right panel). The blue circles and blue smoother lines represent data for nonpregnant women. The red crosses and red lines represent data for pregnant women in trimester 2. The black diamonds and black lines represent data for pregnant women in trimester 3
Sulphadoxine Pharmacokinetics
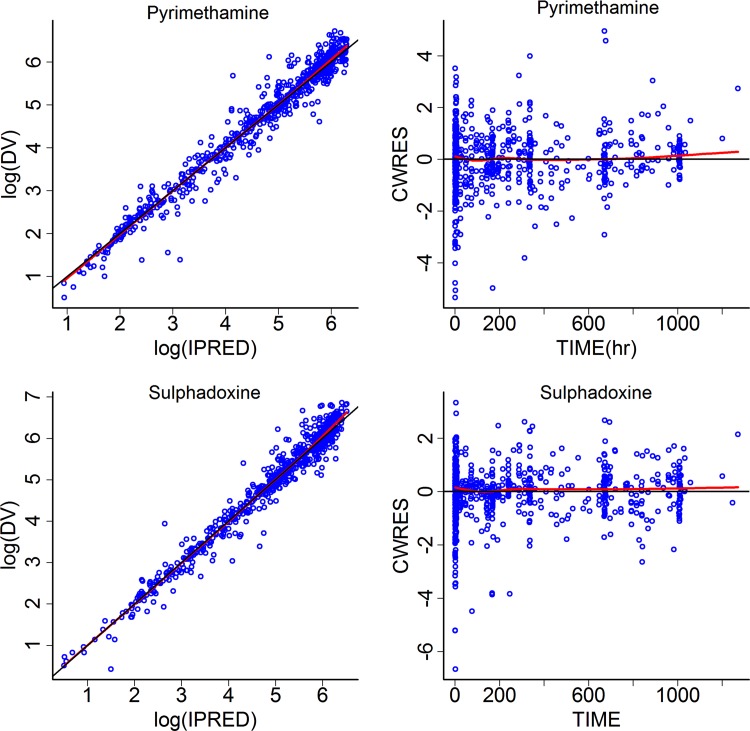
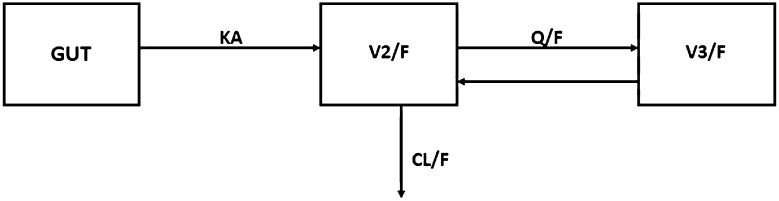
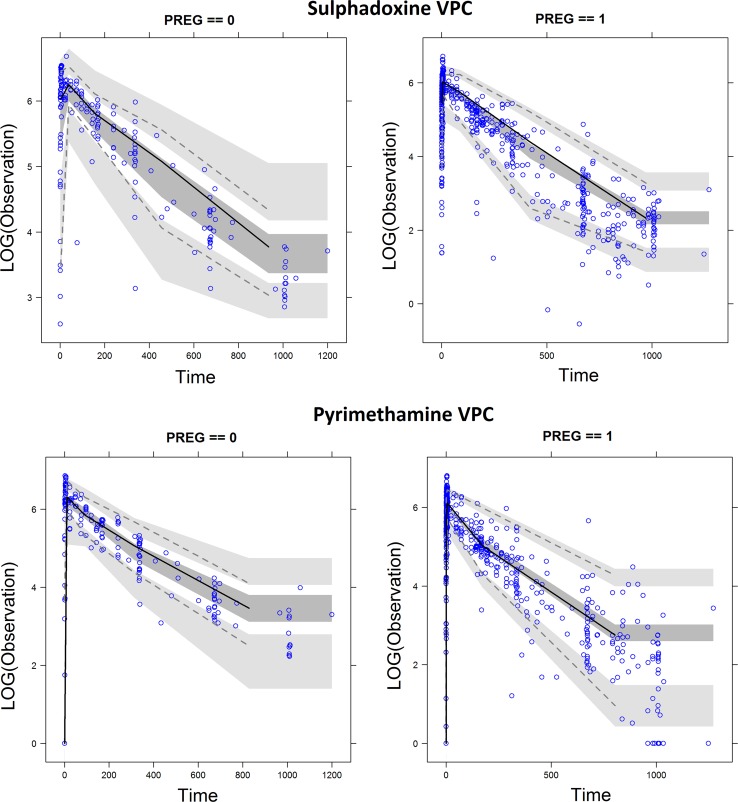
The sulphadoxine dataset contained 1174 data points, of which 975 were measured concentration records beyond time zero. Five women in the third trimester had detectable concentrations at time zero, which affected the parameter and residual estimation processes. These were treated as missing data, hence improving the estimation process. A two-compartment model with first-order absorption and an absorption lag best described the data, as shown by the GOF plots in Fig. 2 and the model structural diagram in Fig. 3. Estimation of the bioavailability fraction did not improve the model in terms of changes in the OFV and GOF plots, hence bioavailability was assumed to be equal to 1. The interindividual variabilities in V2/F and V3/F were less than 10E−6 and were therefore not estimated but fixed at zero. The interindividual variability in the absorption lag was not estimated, in order to avoid overparameterization problems. Statistically significant covariate relationships were identified on CL/F (pregnancy status and albumin), KA (trimester), and V2/F (gestational age). The CL/F–albumin covariate relationship had less than 50 % inclusion frequency at the covariate bootstrap stage, hence it was removed from the final model. The CI of one of the KA relations with trimester included zero, hence the KA–trimester relationship was also removed from the final model. The parameters of the base, as well as the final covariate models, are presented in Table 2, along with interindividual variability and residual error terms. Bootstrap results are also shown in Table 2 and demonstrate robust fixed and random parameter estimates for the final model. The VPC plot (Fig. 4) showed good correspondence between the observed and model-simulated data. Table 3 summarizes the primary and secondary pharmacokinetic parameters across the three pregnancy categories.
Fig. 2.
Plots of observed concentrations (DV) versus individual predictions (IPRED) (left panels) and conditional weighted residuals (CWRES) versus time (right panels) for pyrimethamine (upper panels) and sulphadoxine (lower panels). The red lines show the trends of the data, and the black lines indicate the expected trends. The blue circles represent observed data, and darker coloring of the circles indicates overlapping observations
Fig. 3.
Structure of the two-compartment model used in the final pharmacokinetic analysis of both sulphadoxine and pyrimethamine. CL/F systemic clearance, F bioavailability, GUT absorption compartment, KA first-order absorption rate constant, Q/F intercompartmental clearance, V 2 /F volume of distribution in the central compartment, V 3 /F volume of distribution in the peripheral compartment
Table 2.
Base and final model parameter estimates for sulphadoxine and pyrimethamine among Ugandan women
| Parameter | Sulphadoxine | Pyrimethamine | ||||
|---|---|---|---|---|---|---|
| Base model (RSE %) | Final (RSE %) | Bootstrap 95 % CI | Base model (RSE %) | Final (RSE %) | Bootstrap 95 % CI | |
| KATV [/h] | 0.606 (13.0) | 0.664 (18.5) | 0.5144–0.872 | 1.05 (9.7) | 1.216 (5.7) | 0.960–1.673 |
| V 2/F TV [L] | 10.53 (2.0) | 10.74 (2.8) | 10.27–11.21 | 153.60 (2.8) | 153.915 (2.2) | 145.07–161.09 |
| CL/F TV [L/h] | 0.0253 (23.0) | 0.0059 (27.8) | 0.0057–0.014 | 0.799 (3.4) | 0.545 (5.0) | 0.492–0.608 |
| V 3/F TV [L] | 211.3 (30.0) | 161.71 (33.8) | 74.13–190.74 | 49.53 (15.1) | 51.224 (16.1) | 38.79–67.71 |
| Q TV [L/h] | 0.0297 (21.0) | 0.029 (17.4) | 0.018–0.032 | 0.282 (24.8) | 0.297 (30.9) | 0.201–0.937 |
| ALAGTV [h] | 0.363 (12.0) | 0.371 (11.8) | 0.271–0.449 | 0.394 (1.3) | 0.394 (1.3) | 0.378–0.492 |
| Age–CL | – | – | – | – | 0.016 (36.2) | 0.017–0.046 |
| Albumin–CLa | – | 0.013 (11.5) | – | – | – | – |
| Pregnancy–CLb | – | 0.0284 (16.3) | 1.918–4.906 | – | 0.319 (15.8) | 0.398–0.779 |
| Gestation–V 2 c | – | 0.0093 (14.1) | 0.0063– 0.0116 | – | 0.0079 (23.1) | 0.005–0.011 |
| Body weight–V 2 d | – | – | – | – | 0.0084 (23.7) | 0.004–0.013 |
| IIVe_KA | 98.13 (10.0) | 102.6 (11.3) | 80.19–121.52 | 115.2 (10.0) | 120.9 (10.3) | 97.61–146.36 |
| IIVe_CL | 56.92 (21.0) | 44.6 (17.7) | 27.77–51.68 | 35.6 (9.3) | 30.5 (13.3) | 21.80–38.80 |
| IIVe_V 2 | – | 0 (fixed) | – | 16.67 (24.4) | 8.1 (62.9) | 2.168–17.71 |
| IIVe_V 3 | – | 0 (fixed) | – | 105.97 (15.3) | 109.3 (12.9) | 77.03–142.9 |
| IIVe_Q | 65.72 (19.0) | 52.3 (17.5) | 36.32–71.53 | 84.12 (17.7) | – | – |
| Residual (CV %) | 33.7 (8.0) | 33.1 (8.5) | 27.655–37.996 | 25.92 (19.6) | 27.2 (7.5) | 21.50–29.99 |
ALAG absorption lag time, CI confidence interval, CL systemic clearance, CV % percentage coefficient of variation, F bioavailability, IIV interindividual variability, KA first-order absorption rate constant, Q intercompartmental clearance, RSE % percentage relative standard error, TV typical value of parameter without influence of covariate, V 2 volume of distribution in the central compartment, V 3 volume of distribution in the peripheral compartment
aIncrease in CL with unit decrease in albumin level; this covariate had less than 50 % inclusion at the bootstrap stage and is included in this table because of its strong biologic plausibility
bIncrease in CL with pregnancy
cExponential increase in V 2 with weekly increase in gestational age
dExponential increase in V 2 per kilogram increase in body weight
eIIV; expressed as CV %
Fig. 4.
Visual predictive checks (VPCs) for the sulphadoxine pharmacokinetic model (upper panels) and the pyrimethamine pharmacokinetic model (lower panels). The solid lines represent the observed 50th percentiles, and the dashed lines represent the 2.5th (lower) and 97.5th (upper) percentiles. The shaded areas around the lines represent the 95 % confidence intervals around the respective percentiles. PREG pregnancy
Table 3.
Pharmacokinetic parameters by pregnancy status as determined by Bayesian prediction post hoc
| Parameter | Estimate (CI) | P valuea | ||
|---|---|---|---|---|
| Nonpregnant | Trimester 2 | Trimester 3 | ||
| Sulfadoxine | ||||
| KA [/h] | 0.73 (0.49–0.91) | 0.57 (0.26–0.77) | 0.87 (0.55–1) | 0.0001b |
| CL/F [L/h] | 0.01 (0.01–0.01) | 0.04 (0.03–0.04) | 0.04 (0.03–0.04) | 0.7518 |
| V 2/F [L] | 8.92 (7.87–9.0) | 10.7 (10.55–10.84) | 11.7 (11.6–11.8) | 1.20E−61* |
| Q [L/h] | 0.03 (0.02–0.03) | 0.03 (0.02–0.03) | 0.03 (0.03–0.03) | 0.9519 |
| t ½α [h] | 217.8 (126.4–344.9) | 180.3 (60.3–287.9) | 194.8 (112.2–302.8) | 0.08 |
| t ½β [h] | 620.3 (953.2–1289.9) | 331.5 (215.8–492.9) | 364.5 (211.8–532.9) | 0.01* |
| AUCinf [µmol·h/L] | 793,100 (735,200–847,000) | 144,600 (120,100–169,600) | 144,100 (107,600–170,500) | 0.9382 |
| Pyrimethamine | ||||
| KA [/h] | 1.05 (0.79–1.30) | 1.89 (0.74–1.43) | 1.39 (0.82–1.56) | 0.5172 |
| CL/F [L/h] | 0.59 (0.49–0.64) | 0.92 (0.79–1.01) | 0.94 (0.77–1.06) | 0.5788 |
| V 2/F [L] | 128.7 (119.7–133.4) | 155.3 (145–161.8) | 171.6 (158.3–180.8) | 1.68E−9* |
| V 3/F [L] | 52.9 (27.5–70.5) | 54.6 (37.2–68.9) | 60.2 (45.6–62.5) | 0.3217 |
| t ½α [h] | 55.4 (32.2–91.9) | 52.9 (35.7–79.9) | 57.7 (35.7–79.9) | 0.02* |
| t ½β [h] | 279.7 (211.6–302.7) | 232.2 (183.2–261.9) | 253.8 (213–262.8) | 0.1485 |
| AUCinf [ng·h/L] | 133.03 (117.3–153.1) | 87.66 (74.1–95.3) | 87.4 (70.9–97.9) | 0.9535 |
AUC inf area under the concentration–time curve from time zero to infinity, CI confidence interval, CL systemic clearance, F bioavailability, KA first-order absorption rate constant, Q intercompartmental clearance, t ½α distribution half-life, t ½β terminal elimination half-life, V 2 volume of distribution in the central compartment, V 3 volume of distribution in the peripheral compartment
* Statistically significant difference at P < 0.05
aAs determined by a student’s t test comparing trimester 2 and trimester 3 data alone
bThe KA–trimester relationship failed the covariate bootstrap stage and was therefore considered a spurious finding
Pyrimethamine Pharmacokinetics
The pyrimethamine dataset contained 1161 data points, of which 962 were measured concentration records beyond time zero. A two-compartment model with first-order absorption and an absorption lag best described the data, as shown by the GOF plots in Fig. 2 and the model structural diagram in Fig. 3. Interindividual variabilities were estimated for all parameters, except for ALAG and Q/F, in order to avoid overparameterization problems. Statistically significant covariate relationships were identified on CL/F (pregnancy status and age) and V2/F (gestational age and body weight). The parameters of the base, as well as the final covariate models, are presented in Table 2, along with interindividual variability and residual error terms. Bootstrap results are also shown in Table 2 and demonstrate robust fixed and random parameter estimates for the final model. The VPC plot (Fig. 4) showed good correspondence between the observed and model-simulated data. Table 3 summarizes the primary and secondary pharmacokinetic parameters across the three pregnancy categories.
Discussion
For both sulphadoxine and pyrimethamine, we found statistically significant differences in V2/F, while t½α and t½β were statistically different for pyrimethamine and sulphadoxine, respectively, between the second and third trimesters of gestation. However, assuming a 25 % threshold for the magnitude of difference to be clinically relevant, these differences (all less than 10 %) were not sufficient to support trimester-specific dose modifications. Clinically relevant differences in clearance were, however, observed between pregnant and nonpregnant women, consistent with most previous studies. The increase in sulphadoxine clearance with pregnancy would be expected to result in significantly lower AUC values in comparison with nonpregnant values. Both Karunajeewa et al. [27] and Green et al. [26] reported similar trends among women in Papua New Guinea and Western Kenya, respectively. Nyunt et al. [30] reported a similar trend among Malian women, although no difference was observed among Zambian women. Increases in sulphadoxine clearance may be attributed to increased renal perfusion and glomerular filtration—changes typical of pregnancy [23, 31]. As shown in Table 2, a unit decrease in the serum albumin level was associated with an increase in CL/F of 0.013 L/h. However, despite the failure to meet our stringent covariate bootstrap criteria, this inverse relationship might be contributory to the big increase in clearance seen with pregnancy. This may be so because pregnancy comes with reduced albumin biosynthesis [31], as well as increased urinary excretion [42], both of which reduce the amount of albumin-bound sulphadoxine. Consequently, this increases the availability of sulphadoxine for glomerular filtration. The above observations gave a strong biologic reason to retain the albumin–CL relationship in the model. No difference in clearance was observed pre- and postpartum in the Zambian women studied by Nyunt et al. [30]. This explains the departure of their findings from the trend seen in other studies.
A peculiar finding in this study was the exceptionally long t½β of sulphadoxine, estimated at over 620 h (approximately 26 days) in nonpregnant women. Among pregnant women in trimesters 2 and 3, the t½β values were estimated at 331 h (13.8 days) and 364 h (15 days), respectively. This may be attributed to the large V3/F, estimated at 161.7 L in this population. Despite arriving at similar model structures, Karunajeewa et al. [27] estimated a V3/F of only 1.11 L. A review of past studies suggests that sulphadoxine bioavailability approximates 1 regardless of the administration route [43]. This testifies to its optimal lipophilic–hydrophilic character, which also predicts diffusion beyond the intravascular space. This observation, together with the fact that the extravascular volume of distribution increases in pregnancy [31, 32], suggests that sulphadoxine cannot possibly have a V3/F of just 1.11 L in pregnant women. Given the large V3/F in our study and the fact of sampling from V2/F, t½β was bound to be rather long. We are therefore inclined to accept the present findings, for which further assurance is provided by the good diagnostic plots, as well as the robustness of the bootstrap and VPC analysis.
In contrast to previous studies, we were able to estimate quite precisely the lag time on both sulphadoxine and pyrimethamine absorption. This is consistent with the increased gut transit times associated with well-established pregnancy [31]. Despite arriving at similar structural models, Karunajeewa et al. [27] could not estimate the lag time on the absorption of both drugs. Possible reasons may include the lack of concentration data at time points earlier than 1 h postdose, or the existence of pharmaceutical differences in the tablet formulation, creating significant differences in dissolution characteristics. During pregnancy, maternal blood volumes increase by 40–50 % over and above nonpregnant volumes [44]. We found an increase in V2/F of both drugs of approximately 25 mL/week associated with increasing gestational age. This steady increase in V2/F results in dilutional effects, which, coupled with decreased protein binding and increased renal clearance, will decrease the effective time above the minimum inhibitory concentration (MIC) achievable with each subsequent dose. Considering that both drugs show time-dependent pharmacodynamic effects, this would most likely shorten the duration of the prophylactic effect responsible for much of the effectiveness of SP in IPTp. Fortunately, the revised WHO policy on IPTp recommends more frequent dosing of SP [8]—a strategy likely to counteract these changes.
In comparison with nonpregnant women, there was a 58 % increase in pyrimethamine clearance during pregnancy. This increase can significantly lower AUC values, as shown previously [27]. While Green et al. [26] reported no difference in mean pyrimethamine concentrations between women pre- and postpartum, Nyunt et al. [30] reported higher mean pyrimethamine concentrations among both Malian and Zambian women prepartum. Higher pyrimethamine concentrations in the latter study correlated with significantly lower pyrimethamine clearance prepartum in comparison with the postpartum period. The available literature suggests that pyrimethamine disposition is complex, involving multiple pathways with as yet unidentified metabolites. Only 15–30 % of pyrimethamine is excreted unchanged in the urine [45]. In addition, there are indications that pyrimethamine may be a substrate as well as an inhibitor of the cytochrome P450 (CYP) 2C8, CYP2C9 and CYP2D6 enzyme systems [46]—an effect likely to decrease its metabolism. However, pregnancy itself is known to increase the activity of CYP2C9 and CYP2D6 [47, 48], with a counter-effect of increasing pyrimethamine metabolism. It is therefore possible that the net effect of these interactions, coupled with polymorphisms within individual CYP subfamilies, underlies the differences in pyrimethamine clearance observed in the present and previous studies.
Besides synergism, Wang et al. [49] demonstrated that pyrimethamine potentiates sulphadoxine activity by an as yet ill-understood mechanism. This might explain earlier observations that pyrimethamine is the critical player in determining the efficacy of SP [50, 51]. Higher pyrimethamine concentrations during pregnancy may therefore be advantageous in IPTp and may underlie the continued effectiveness of IPTp despite the considerable presence of SP resistance mutations in Southern Africa [14, 16]. We were unable to find recent studies reporting SP IPTp effectiveness data from the East African region. However, going by the reduced pyrimethamine exposure in our study, together with the findings by Green et al. [26] in Kenya, a relative reduction in the effectiveness of SP IPTp within the East African region would not be surprising. SP IPTp acts by clearing asymptomatic parasites, followed by posttreatment prophylaxis. Resistance to SP develops in a stepwise manner, with increasing numbers of mutations conferring increasing levels of resistance and consequently decreasing the duration of posttreatment prophylaxis [7]. Because both sulphadoxine and pyrimethamine show linear kinetics, dose increases would minimally restore effectiveness against resistant parasites [7, 50]. This is so because optimal drug concentrations would not last long enough to achieve a sustained prophylactic effect; moreover, the risks of toxicity would most likely increase. Possible ways around this challenge would be more frequent dosing of SP or coadministration of SP with drugs that decrease its renal clearance. The use of probenecid to retard renal clearance of SP has been proposed [52] and may warrant further research.
Conclusion
This study did not find clinically relevant differences in the pharmacokinetics of sulphadoxine or pyrimethamine on the basis of trimester. Increased clearance with pregnancy and increasing V2/F with increasing gestational age were observed for both drugs. Respectively, these changes would be expected to lower total SP exposure and reduce the time above the MIC, hence decreasing the duration of the prophylactic effect during pregnancy. The present findings lend support to recent revisions in SP IPTp policy, advocating for more frequent dosing of SP in order to enhance the effectiveness of IPTp.
Acknowledgments
The authors are sincerely grateful to Nantume Anthony, Mirembe Esther Joyce, Katusiime Sikola, and Namulindwa Margaret—midwives who assisted with clinical data collection. Our heartfelt appreciation goes to all of the women who kindly agreed to participate in this study.
Compliance with Ethical Standards
Ethical statement
The study protocol was reviewed and approved by the Research Ethics Committee at the School of Medicine, Makerere University (# REC REF 2012-074), and the Mulago Hospital Research Ethics Committee (REF #: MREC 397). All study procedures were done in accordance with the ethical standards of the World Medical Association’s Helsinki Declaration (1964) and the International Conference on Harmonization (ICH) guidelines for Good Clinical Practice. The Uganda National Council for Science and Technology granted permission to conduct the study (REF #: HS 1277).
Conflict of interest statement
COO, KRB, MN, GOE, FWO, JB, JKM and CO report no conflicts of interest.
Funding statement
This work was funded through Grant Number 5R24TW008886 supported by the following offices of the USA: Office of the US Global Aids Coordinator (OGAC), National Institutes of Health (NIH), and Health Resources and Services Administration (HRSA). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the supporting offices.
References
- 1.Desai M, ter Kuile FO, Nosten F, McGready R, Asamoa K, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7:93–104. doi: 10.1016/S1473-3099(07)70021-X. [DOI] [PubMed] [Google Scholar]
- 2.Dellicour S, Tatem A, Guerra C, Snow R, ter Kuile FO. Quantifying the number of pregnancies at risk of malaria in 2007: a demographic study. PLoS Med. 2010;7:e1000221. doi: 10.1371/journal.pmed.1000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO). A strategic framework for malaria prevention and control during pregnancy in the African region. Brazaville: WHO Regional Offices for Africa; 2004.
- 4.World Health Organization (WHO). World malaria report 2012. Geneva: WHO; 2013.
- 5.Vallely A, Vallely L, Changalucha J, Greenwood B, Chandramohan D. Intermittent preventive treatment for malaria in pregnancy in Africa: what’s new, what’s needed? Malar J. 2007;6:16. doi: 10.1186/1475-2875-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Menendez C, D’Alessandro U, ter Kuile FO. Reducing the burden of malaria in pregnancy by preventive strategies. Lancet Infect Dis. 2007;7(2):126–135. doi: 10.1016/S1473-3099(07)70024-5. [DOI] [PubMed] [Google Scholar]
- 7.White NJ. Intermittent presumptive treatment for malaria. PLoS Med. 2005;2(1):e3. doi: 10.1371/journal.pmed.0020003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Malaria Policy Advisory Committee and Secretariat Malaria Policy Advisory Committee to the WHO: conclusions and recommendations of September 2012 meeting. Malar J. 2012;11:424. doi: 10.1186/1475-2875-11-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steketee RW. Malaria prevention during pregnancy—is there a next step forward? PLoS Med. 2014;11(9):e1001734. doi: 10.1371/journal.pmed.1001734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steketee RW, Wirima JJ, Slutsker L, Heymann DL, Breman JG. The problem of malaria and malaria control in pregnancy in sub-Saharan Africa. Am J Trop Med Hyg. 1996;55(1 Suppl):2–7. doi: 10.4269/ajtmh.1996.55.2. [DOI] [PubMed] [Google Scholar]
- 11.Kapito-Tembo A, Meshnick SR, van Hensbroek MB, Phiri K, Fitzgerald M, Mwapasa V. Marked reduction in prevalence of malaria parasitemia and anemia in HIV-infected pregnant women taking cotrimoxazole with or without sulfadoxine–pyrimethamine intermittent preventive therapy during pregnancy in Malawi. J Infect Dis. 2011;203(4):464–472. doi: 10.1093/infdis/jiq072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kayentao K, Garner P, Eijk AM, Naidoo I, Roper C, Mulokozi A, et al. Intermittent preventive therapy for malaria during pregnancy using 2 vs 3 or more doses of sulfadoxine–pyrimethamine and the risk of low birth weight in Africa: systematic review and meta-analysis. J Am Med Assoc. 2013;309(6):594–604. doi: 10.1001/jama.2012.216231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ter Kuile FO, Eijk AM, Filler SJ. Effect of sufadoxine–pyrimethamine resistance on the efficacy of intermittent preventive therapy for malaria control during pregnancy: a systematic review. J Am Med Assoc. 2007;297:2603–2616. doi: 10.1001/jama.297.23.2603. [DOI] [PubMed] [Google Scholar]
- 14.Tan KR, Katalenich BL, Mace KE, Nambozi M, Taylor SM, Meshnick SR, et al. Efficacy of sulphadoxine–pyrimethamine for intermittent preventive treatment of malaria in pregnancy, Mansa, Zambia. Malar J. 2014;13:227. doi: 10.1186/1475-2875-13-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clerk CA, Bruce J, Affipunguh PK, Mensah N, Hodgson A, Greenwood B, et al. A randomized, controlled trial of intermittent preventive treatment with sulfadoxine–pyrimethamine, amodiaquine, or the combination in pregnant women in Ghana. J Infect Dis. 2008;198(8):1202–1211. doi: 10.1086/591944. [DOI] [PubMed] [Google Scholar]
- 16.Gutman J, Mwandama D, Wiegand RE, Ali D, Mathanga DP, Skarbinski J. Effectiveness of intermittent preventive treatment with sulfadoxine–pyrimethamine during pregnancy on maternal and birth outcomes in Machinga district, Malawi. J Infect Dis. 2013;208(6):907–916. doi: 10.1093/infdis/jit276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eisele TP, Larsen DA, Anglewicz PA, Keating J, Yukich J, Bennett A, et al. Malaria prevention in pregnancy, birthweight, and neonatal mortality: a meta-analysis of 32 national cross-sectional datasets in Africa. Lancet Infect Dis. 2012;12(12):942–949. doi: 10.1016/S1473-3099(12)70222-0. [DOI] [PubMed] [Google Scholar]
- 18.Menendez C, Bardaji A, Sigauque B, Sanz S, Aponte JJ, Mabunda S, et al. Malaria prevention with IPTp during pregnancy reduces neonatal mortality. PLoS One. 2010;5(2):e9438. doi: 10.1371/journal.pone.0009438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Francis D, Nsobya SL, Talisuna A, Yeka A, Kamya MR, Machekano R, et al. Geographic differences in antimalarial drug efficacy in Uganda are explained by differences in endemicity and not by known molecular markers of drug resistance. J Infect Dis. 2006;193(7):978–986. doi: 10.1086/500951. [DOI] [PubMed] [Google Scholar]
- 20.Cox-Singh J, Lu HY, Davis TM, Ilett KF, Hackett LP, Matusop A, et al. Application of a multi-faceted approach for the assessment of treatment response in falciparum malaria: a study from Malaysian Borneo. Int J Parasitol. 2003;33(13):1545–1552. doi: 10.1016/S0020-7519(03)00199-1. [DOI] [PubMed] [Google Scholar]
- 21.Gasasira AF, Kamya MR, Ochong EO, Vora N, Achan J, Charlebois E, et al. Effect of trimethoprim–sulphamethoxazole on the risk of malaria in HIV-infected Ugandan children living in an area of widespread antifolate resistance. Malar J. 2010;9:177. doi: 10.1186/1475-2875-9-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malamba S, Sandison T, Lule J, Reingold A, Walker J, Dorsey G, et al. Plasmodium falciparum dihydrofolate reductase and dihydropteroate synthase mutations and the use of trimethoprim–sulfamethoxazole prophylaxis among persons infected with human immunodeficiency virus. Am J Trop Med Hyg. 2010;82(5):766–771. doi: 10.4269/ajtmh.2010.08-0408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ward SA, Sevene EJ, Hastings IM, Nosten F, McGready R. Antimalarial drugs and pregnancy: safety, pharmacokinetics, and pharmacovigilance. Lancet Infect Dis. 2007;7(2):136–144. doi: 10.1016/S1473-3099(07)70025-7. [DOI] [PubMed] [Google Scholar]
- 24.Wilby KJ, Ensom MH. Pharmacokinetics of antimalarials in pregnancy: a systematic review. Clin Pharmacokinet. 2011;50(11):705–723. doi: 10.2165/11594550-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Nosten F, McGready R, d’Alessandro U, Bonell A, Verhoeff F, Menendez C et al. Antimalarial drugs in pregnancy: a review. Curr Drug Saf. 2006;1(1):1–15. [DOI] [PubMed]
- 26.Green MD, van Eijk AM, ter Kuile FO, Ayisi JG, Parise ME, Kager PA, et al. Pharmacokinetics of sulfadoxine–pyrimethamine in HIV-infected and uninfected pregnant women in Western Kenya. J Infect Dis. 2007;196(9):1403–1408. doi: 10.1086/522632. [DOI] [PubMed] [Google Scholar]
- 27.Karunajeewa HA, Salman S, Mueller I, Baiwog F, Gomorrai S, Law I, et al. Pharmacokinetic properties of sulfadoxine–pyrimethamine in pregnant women. Antimicrob Agents Chemother. 2009;53(10):4368–4376. doi: 10.1128/AAC.00335-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meyer UA, Zanger UM. Molecular mechanisms of genetic polymorphisms of drug metabolism. Ann Rev Pharmacol Toxicol. 1997;37:269–296. doi: 10.1146/annurev.pharmtox.37.1.269. [DOI] [PubMed] [Google Scholar]
- 29.Sarikabhuti B, Keschamrus N, Noeypatimanond S, Weidekamm E, Leimer R, Wernsdorfer W, et al. Plasma concentrations of sulfadoxine in healthy and malaria infected Thai subjects. Acta Trop. 1988;45(3):217–224. [PubMed] [Google Scholar]
- 30.Nyunt MM, Adam I, Kayentao K, van Dijk J, Thuma P, Mauff K, et al. Pharmacokinetics of sulfadoxine and pyrimethamine in intermittent preventive treatment of malaria in pregnancy. Clin Pharmacol Ther. 2010;87(2):226–234. doi: 10.1038/clpt.2009.177. [DOI] [PubMed] [Google Scholar]
- 31.Costantine MM. Physiologic and pharmacokinetic changes in pregnancy. Front Pharmacol. 2014;5:65. doi: 10.3389/fphar.2014.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loebstein R, Lalkin A, Koren G. Pharmacokinetic changes during pregnancy and their clinical relevance. Clin Pharmacokinet. 1997;33(5):328–343. doi: 10.2165/00003088-199733050-00002. [DOI] [PubMed] [Google Scholar]
- 33.National Malaria Control Program . Uganda national malaria control policy 2011. Kampala: Ministry of Health; 2011. [Google Scholar]
- 34.Bergqvist Y, Hjelm E, Rombo L. Sulfadoxine assay using capillary blood samples dried on filter paper—suitable for monitoring of blood concentrations in the field. Ther Drug Monit. 1987;9(2):203–207. doi: 10.1097/00007691-198706000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Minzi OM, Massele AY, Gustafsson LL, Ericsson O. Simple and cost-effective liquid chromatographic method for determination of pyrimethamine in whole blood samples dried on filter paper. J Chromatograp B. 2005;814(1):179–183. doi: 10.1016/j.jchromb.2004.10.049. [DOI] [PubMed] [Google Scholar]
- 36.Beal SL, Sheiner LB. The NONMEM system. Am Stat. 1980;34:118–119. doi: 10.2307/2684123. [DOI] [Google Scholar]
- 37.Boeckmann AJ, Sheiner LB, Beal SL. NONMEM users guides. San Francisco: NONMEM Project Group, University of California; 1994. [Google Scholar]
- 38.Lindbom L, Ribbing J, Jonsson EN. Perl-speaks-NONMEM (PsN)—a Perl module for NONMEM related programming. Comput Methods Programs Biomed. 2004;75(2):85–94. doi: 10.1016/j.cmpb.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 39.R Core Team. R: a language and environment for statistical computing. Version 3.0.1. Vienna: R Foundation for Statistical Computing; 2013.
- 40.Jonsson EN, Karlson MO. Xpose—an S-Plus based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Comput Methods Programs Biomed. 1999;58:51–64. doi: 10.1016/S0169-2607(98)00067-4. [DOI] [PubMed] [Google Scholar]
- 41.Ette EI, Williams PJ, Kim YH, Lane JR, Liu MJ, Capparelli EV. Model appropriateness and population pharmacokinetic modeling. J Clin Pharmacol. 2003;43(6):610–623. doi: 10.1177/0091270003253624. [DOI] [PubMed] [Google Scholar]
- 42.Cheung CK, Lao T, Swaminathan R. Urinary excretion of some proteins and enzymes during normal pregnancy. Clin Chem. 1989;35(9):1978–1980. [PubMed] [Google Scholar]
- 43.Bruno C, Rodolphe T, Rachid SL. Systematic search and analysis of published pharmacokinetic data related to sulfadoxine. Bordeaux: European Toxo Prevention Group; 2005. [Google Scholar]
- 44.Hytten FE, Paintin DB. Increase in plasma volume during normal pregnancy. J Obstet Gynaecol. 1963;70:402–407. doi: 10.1111/j.1471-0528.1963.tb04922.x. [DOI] [PubMed] [Google Scholar]
- 45.Roche Laboratories . Fansidar (sulfadoxine–pyrimethamine) tablets: prescribing information. Nutley: Roche Laboratories; 2004. [Google Scholar]
- 46.Preissner S, Kroll K, Dunkel M, Senger C, Goldsobel G, Kuzman D et al. SuperCYP: a comprehensive database on cytochrome P450 enzymes including a tool for analysis of CYP–drug interactions. Nucleic Acids Research. 2010;38(Database Issue):D237–43. [DOI] [PMC free article] [PubMed]
- 47.Hogstedt S, Lindberg B, Peng DR, Regardh CG, Rane A. Pregnancy-induced increase in metoprolol metabolism. Clin Pharmacol Ther. 1985;37(6):688–692. doi: 10.1038/clpt.1985.114. [DOI] [PubMed] [Google Scholar]
- 48.Yerby MS, Friel PN, McCormick K, Koerner M, Van Allen M, Leavitt AM, et al. Pharmacokinetics of anticonvulsants in pregnancy: alterations in plasma protein binding. Epilepsy Res. 1990;5(3):223–228. doi: 10.1016/0920-1211(90)90042-T. [DOI] [PubMed] [Google Scholar]
- 49.Wang P, Brobey RK, Horii T, Sims PF, Hyde JE. Utilization of exogenous folate in the human malaria parasite Plasmodium falciparum and its critical role in antifolate drug synergy. Mol Microbiol. 1999;32(6):1254–1262. doi: 10.1046/j.1365-2958.1999.01437.x. [DOI] [PubMed] [Google Scholar]
- 50.Watkins WM, Mberu EK, Winstanley PA, Plowe CV. The efficacy of antifolate antimalarial combinations in Africa: a predictive model based on pharmacodynamic and pharmacokinetic analyses. Parasitol Today. 1997;13(12):459–464. doi: 10.1016/S0169-4758(97)01124-1. [DOI] [PubMed] [Google Scholar]
- 51.Schapira A, Bygbjerg IC, Jepsen S, Flachs H, Bentzon MW. The susceptibility of Plasmodium falciparum to sulfadoxine and pyrimethamine: correlation of in vivo and in vitro results. Am J Trop Med Hyg. 1986;35(2):239–245. doi: 10.4269/ajtmh.1986.35.239. [DOI] [PubMed] [Google Scholar]
- 52.Gutman J, Kachur SP, Slutsker L, Nzila A, Mutabingwa T. Combination of probenecid–sulphadoxine–pyrimethamine for intermittent preventive treatment in pregnancy. Malar J. 2012;11:39. doi: 10.1186/1475-2875-11-39. [DOI] [PMC free article] [PubMed] [Google Scholar]