Abstract
Colorectal carcinoma is the third most prevalent cancer in the world. In the most advanced stages, the use of chemotherapy induces a poor response and is usually accompanied by other tissue damage. Significant progress based on suicide gene therapy has demonstrated that it may potentiate the classical cytotoxic effects in colorectal cancer. The inconvenience still rests with the targeting and the specificity efficiency. The main target of gene therapy is to achieve an effective vehicle to hand over therapeutic genes safely into specific cells. One possibility is the use of tumor-specific promoters overexpressed in cancers. They could induce a specific expression of therapeutic genes in a given tumor, increasing their localized activity. Several promoters have been assayed into direct suicide genes to cancer cells. This review discusses the current status of specific tumor-promoters and their great potential in colorectal carcinoma treatment.
1. Background
Colorectal carcinoma (CRC) is the third most prevalent cancer in the world [1]. The main treatments, such as 5-fluorouracil (5-FU) alone or combined (FOLFOX and FOLFIRI), new angiogenesis inhibitors, and epidermal growth factor receptor inhibitors, induce a poor response in most advanced stages and are usually accompanied by other tissue damage [2]. Suicide gene therapy has been widely used in many studies in vitro and in vivo, demonstrating that it may potentiate the classical cytotoxic effects in some tumors [3], including colon cancer [4, 5]. However, gene therapy application in cancer patients has not yet successfully gained clinical significance. The inconvenience still rests with targeting and efficiency of the specificity.
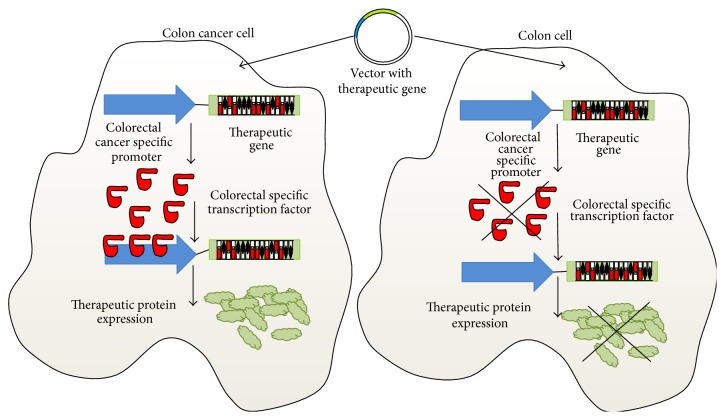
For this purpose, it is necessary to express these genes into specific tumor cells. The main target of gene therapy is to achieve an effective vehicle to hand over therapeutic genes safely into specific cells. One possibility is the use of tumor-specific promoters, overexpressed in cancer cells. They could induce a specific expression of therapeutic genes in a type of tumor increasing their localized activity (Figure 1).
Figure 1.
Schematic representation of a colon cancer specific promoter and the induction of therapeutic gene expression. High levels of specific transcription factors in colon cancer cells are able to induce therapeutic gene expression. By contrast, no expression of these specific transcription factors in normal colon cells avoids the transcription of the therapeutic gene.
For instance, the TTS system (TTF1 gene under the control of hTERT promoter and hSPA1 promoter) shows a selective activity in lung cancer cells but not in other types of cancer or normal cells [6]. Other promoters employed in gene therapy are the α fetoprotein (AFP) promoter (for hepatic cancer) [7, 8] and the erb2 promoter (for breast cancer) [9, 10]. It has been demonstrated that the hTERT promoter is able to direct the expression of the PEA-15 gene, a tumor suppressor gene and inhibitor of cell growth and invasion [11–13], specifically to breast cancer cells, inducing growth suppression and inhibition. This decrease is also observed in the tumor growth of orthotopic animal models, as well as a prolongation of survival time [14]. Similar results have been found by Zhang et al. [15], who have proved the capacity of the tumor-specific promoter hTERT to drive the expression of the apoptin and E1A genes in prostate carcinoma cells and in mouse models. Apoptin, a protein derived from chicken anemia virus VP3 gene, is able to induce selective apoptosis in human tumor and transformed cells but shows little or no cytotoxic effect in many normal human cells [16, 17]. Several promoters such as carcinoembryonic antigen (CEA), cyclooxygenase-2 (COX-2) [18], human telomerase reverse transcriptase [19], and Urokinase-type plasminogen activator receptor (uPAR) [20] have been assayed to direct suicide genes into CRC cells.
In this review, we are going to show the current status of specific tumor-promoters and their great potential in CRC treatment.
2. Tumor-Promoters in Colorectal Carcinoma
2.1. CEA
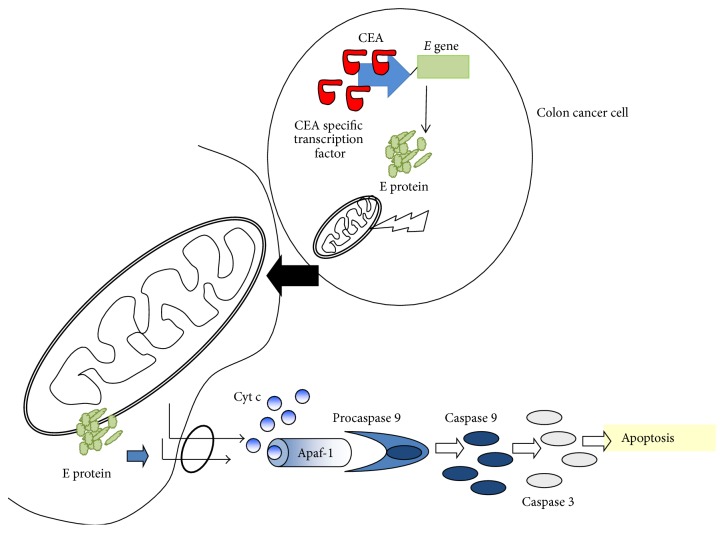
Carcinoma embryonic antigen (CEA) is an oncofetal tumor marker overexpressed in over 90% of colorectal cancer cells but not in normal colon cells [21–23]. High levels of serum CEA and high expressions of CEA mRNA have been detected in patients in the last stages of human colon carcinogenesis [24, 25]. CEA levels have been used for predicting the prognosis and monitoring recurrence and metastasis in patients with stage II CRC [26]. In fact, CEA showed clinical and pathological significance as prognostic markers in the diagnosis of colorectal cancer [26, 27], local recurrence, and overall survival after resection [28]. This elevated CEA promoter expression has also been shown in cancer cell lines versus nontumor cell lines [29, 30]. In response to this tumor specificity, CEA promoter has been studied to drive the expression of therapeutic genes to CEA positive cancer cells [18]. Zhang et al. [30] studied the efficiency of the double system cytosine deaminase (CD) and thymidine kinase (TK) targeted by CEA promoter in CEA positive human gastric cancer cell line (SGC7901) versus a CEA negative human adenocarcinoma cell line (HeLa), showing a greater growth inhibition in SGC7901 (89.8%) than in HeLa line cell (2%). Similar findings were revealed in the CEA positive human colon cancer cell line (LoVo). After 5 days of 5-FC treatment, HeLa cells transfected with CEA-CD were not sensitized by the cytotoxicity, whereas transfected LoVo cells showed a cell growth inhibition of 72.7% [31]. In vivo studies demonstrated a similar effect in LoVo xenografts mice treated with the CEA-CD system [31] and in xenograft SGC7901 treatment with the double system CEA-CD-TK (46% tumor growth inhibition rate (TGIR) versus nontreated tumor control) [30]. Current study of Rama et al. [32] reveled the ability of the CEA promoter to direct E gene expression towards colon cancer cells, inducting a high cell growth inhibition in comparison to normal human colon cells (Figure 2). In addition, in vivo analyses of mice bearing subcutaneous MC-38 colon cancer cells showed a significant decrease in tumor volume and low level of Ki-67 in relation to untreated tumors.
Figure 2.
Antitumor effect of the E gene under CEA promoter. The high transcriptional activity of the CEA promoter in colon cancer cells leads to E gene expression which encodes a cytotoxic protein. The protein E targets mitochondria in colon cancer cells, disrupting their cristae and inducing apoptosis by release of cytochrome c and activation of caspases 9 and 3.
2.2. Cox-2
Cyclooxygenase-2 (Cox-2) is an enzyme which participates together with COX-1 in the oxidation of arachidonic acid to prostaglandin, an essential promoting factor in carcinogenesis and development of tumors [33, 34]. Some studies have demonstrated that uses of inhibitors against Cox-2 suppress colon carcinogenesis [34, 35]. Cox-2 is associated to CRC [36], exhibiting expression in 93% of colon cancers and in 87% of rectal cancers [37], to polyps with high-grade [38, 39], to a higher TNM (tumor, node, metastasis) class, and to higher Dukes' stage [40]. In a study on 35 cases of CRC, 77% of them were Cox-2 positive and 43% showed location in the rectum and left side [41]. This overexpression has been associated with the reduced survival of CRC patients [42]. Furthermore, the recent study has shown higher values of expression in colon cancer (93%) than in rectal cancer (87%), associating this decrease of Cox-2 expression to decreased disease-specific survival and decreased disease-free survival in rectal cancer but not in colon cancer, suggesting the Cox-2 expression as a predictive clinical biomarker of rectal but not colon cancer [37].
This elevated Cox-2 promoter expression has also been shown in cancer cell lines versus nontumor cancer cell lines [43–45]. Wang et al. [45] analyzed the transcriptional activity of Cox-2 promoter by the luciferase reporter gene in colorectal cancer cell lines and normal human intestinal epithelial cell lines. The results proved an increased luciferase activity in all colorectal cancer lines (a median of 83% of the three of them) relative to normal cells (12%). Based on this specific-tumor activity, Cox-2 promoter has been used to target different genes to specific colon cancer cells [43, 45]. The system Cox-2-TK conferred ganciclovir sensitivity to LoVo tumor cells and 52.5 ± 1.2% inhibitory rates but did not affect normal cells [45]. Another similar study has used the Cox-2 promoter to drive the 15-hydroxyprostaglandin dehydrogenase (15-PGDH), a gene suppressed in the majority of cancers. 15-PGDH specific expression, under Cox-2 control promoter in colon cancer cells, inhibited growth and migration of colon cells [43]. In vivo studies demonstrated a similar effect in LoVo xenografts treated with Cox-2-TK, showing 59.4% inhibitory rates versus nontreated LoVo xenografts [45]. Thus, Kaliberova et al. [43] corroborated the effect of the system Cox-2-15-PGDH in LS174T xenografts, disclosing an inhibitory effect on tumor growth compared to nontreated xenografts.
2.3. A33
A33 is a transmembrane glycoprotein member of the immunoglobulin superfamily, present only in the small intestine and colon [20, 46] and is associated with the process of cell adhesion, cell trafficking, and intestinal immune response [47, 48]. A33 overexpression is related to several cancers such as primary and metastatic colorectal carcinomas (95%), diffuse gastric cancers (63%), intestinal-type gastric cancers (83%), and pancreatic cancers (50%) but has been undetected in normal epithelial tissue [49, 50]. However, the expression level of A33 is not correlated to the disease stage and the degree of histological differentiation [51].
Having established this specific expression of A33 in gastrointestinal cancer, several immunotherapy assays have manipulated different humanized A33 antibody fragments, targeting them as specific carriers of other molecules (immunoconjugates) for antitumor treatment [52–54]. Recently, Cafferata et al. [55] have used the A33 promoter in the design of a conditionally replicative adenovirus to specifically drive the essential early E1A gene into CRC cells. E1A is an oncoprotein with several anticancer activities such as decreasing tumorigenic potential, increasing inhibition of cell growth and promoting apoptosis [56, 57]. They showed A33 mRNA expression levels in different colorectal carcinoma cell lines, but not in normal colonic cells, breast cancer cell lines, hepatocellular carcinoma cell lines, fetal lung fibroblast cell lines, melanoma cell lines, and embryonic kidney cells. This was related to the activity of the A33 promoter, essentially active only in human CRC cells whereas human mammary and melanoma cells showed strongly reduced activity. Subsequently, the adenovirus showed specific lytic activity in human colorectal carcinoma cell lines and a slight activity in hepatocellular carcinoma and melanoma cell lines. To improve this therapeutic effect, the A33-E1A adenovirus was combined with 5-FU administration, exhibiting an enhanced lytic effect of 5-FU colon cancer cell lines compared with the 5-FU treatment alone. In vivo, the adenovirus was effective in inhibiting tumor growth in 100% of LoVo xenografts; treated mice survived significantly longer than the control group. However, no evidence was observed in melanoma xenografts. Also, liver metastasis was studied, displaying absence of metastatic nodules (10/11 mice injected with A33-E1A adenovirus) and strongly reduced metastatic areas (1/11). Nonetheless, adding 5-FU in combination with the A33-E1A adenovirus did not significantly improve the tumor growth inhibitory effect observed with A33-E1A adenovirus alone.
2.4. TERT
Telomere/telomerase interplay has a prominent role in the preservation of genetic chromosome stability and its failure is involved in carcinogenesis [58]. Human telomerase has two subunits: a template RNA component (hTR) and a catalytic subunit called the human telomerase reverse transcriptase (hTERT) [59]. The expression of hTR subunit is expressed in all types of human cells and serves as a template for telomere synthesis; however, hTERT is expressed in cells with high telomerase activity, as tumor cells, but it is not expressed in normal tissues [59–62]. Telomerase is highly active in 90% of malignant tumors [63]. CRC patients with increased levels of hTERT mRNA have been correlated with tumor stage, histological grade, and significantly worse survival than CRC patients with low hTERT levels [58, 64].
Higashi et al. [19] confirmed, using EGFP as reporter gene, the high activity of the hTERT promoter in several tumor cell lines of human esophageal cancer and mouse colon adenocarcinoma, but they did not find activity in normal human fibroblasts. The hTERT promoter has been used to direct the therapeutic genes expression in cancer showing a great tumor-specific capacity [62, 65–67].
Yang et al. [68] used an adenovirus based on the hTERT promoter to deliver both apoptin gene and E1A gene into CRC cells. This adenovirus induced 70–75% of cell growth inhibition in CRC cells, showing 32.3% and 31.5% levels of apoptosis and necrosis, respectively. Conversely, no effect was observed in transfected human gastric epithelium. In concordance with these results, the in vivo experiments with mouse models of CRC proved that this adenovirus provoked a slower tumor growth, increased the median survival time, and reduced the number of metastatic lung nodules with respect to the nontreated CRC mice. Higashi et al. [19] utilized the hTERT promoter to direct in a specific way the expression of two genes, interleukin-18 (IL-18) and TK, to murine colorectal cancer cells. IL-18 is a proinflammatory cytokine that activates the cytotoxicity of CD8+ T, CD4+ T, and NK cells [69, 70]. The mentioned cells were sensitive to ganciclovir and showed high levels of IL-18 secretion. These cells were injected into mice in order to generate colorectal cancer tumors in them. After treating them with ganciclovir, the mentioned tumors were totally eliminated, whereas in the control groups the tumor growth was progressive. Besides, a rise of CD8+ T and CD4+ T cells in the tumor zone was observed, indicative of tumor-specific acquired immunity.
2.5. uPAR
Urokinase-type plasminogen activator receptor (uPAR) gene codes a serine protease that catalyzes the transformation of the inert zymogen plasminogen into plasmin [20, 71]. uPAR gene is upregulated by the activated RAS signaling pathway, the main signaling pathway activated in colon cancer [72]. The components of the uPAR system are overexpressed in diverse human tumors, such as pancreatic, hepatic, breast, and especially gastrointestinal cancers [73–76]. Tumor specific binding of activator protein (AP-1) to uPAR promoter has been detected in ~40% CRC patients, and 39.8% of them showed this tumor specific binding in the resected tumors in contrast to low or absent binding in corresponding normal mucosa [76] demonstrating the tumor specific activity of uPAR in CRC and not in normal tissue. High uPAR protein levels have been correlated with poor 5-year survival in colon cancer patients [50] and increased invasive capacity of tumor cells [77].
Teimoori-Toolabi et al. [78] proved the specific activity of the uPAR promoter in colon and colorectal cancer cell lines. Using the LacZ gene reporter under the control of the uPAR promoter, they observed beta-gal expression in human colorectal carcinoma (HTC116) and in colon cancer cells (SW480), but not in normal colon cells and nontransformed human umbilical vein endothelial cells. Afterward, they used uPAR promoter to deliver TK gene in SW480 and HCT116 cells. The growth of these cells with ganciclovir was significantly decreased.
2.6. FGF18
Fibroblast growth factor 18 (FGF18) is a crucial mitogen in embryonic limb development [79] with a significant participation in the development of cartilage and bone [80, 81]. Its overexpression has been associated to different types of cancer, especially CRC [82, 83]. FGF18 is downstream of Wnt pathways and is highly active in CRC [56, 82, 84]. In a study with 38 CRC and their respective normal mucosa, 34 out of 38 CRC exhibited greater FGF18 mRNA levels than the normal mucosa. Moreover, this overexpression was associated with colon carcinogenesis from adenoma to carcinoma [84], suggesting FGF18 as a novel marker for early detection of colorectal tumors [82].
Teimoori-Toolabi et al. [85] researched the FGF18 promoter activity in SW480, HCT116, human normal colon cells, and umbilical vein endothelial cells. All cells were transiently transfected with a plasmid with LacZ gene reported under FGF18 promoter. Beta-gal staining showed a higher expression in SW480 (5%) and HCT116 (10%) than in human normal colon cells and umbilical vein endothelial cells (0%). After demonstrating the tumor specific activity of FGF18 promoter, this was used in a new plasmid to deliver TK gene to cancer cells. A significantly decreased growth was shown in SW480 and HCT116 cells after ganciclovir treatment.
2.7. KDR
The endothelial cell type-specific tyrosine kinase domain-containing receptor (KDR) is a receptor for the vascular endothelial growth factor (VEGF), playing an essential role in endothelial cell growth and development [86]. KDR expression has been detected in a variety of cancer cells and neogenetic vascular endothelial cells of the neoplasm but has not been detected in normal cells [86–89]. Currently, in a study with 110 CRC patients, single nucleotide polymorphisms (SNP) of KDR were correlated with microvessel density and overall survival [89]. Hansen et al. [90] also linked SNP of KDR with a reduced recurrence risk, this association being higher in CRC patients receiving chemotherapy.
The specific activity of the KDR promoter to deliver both TK and CD genes (KDR/CD-TK) in colon cancer cells has been studied. CD/TK mRNA levels were detected in SW480 and SW620 cells (KDR positive human colon adenocarcinoma) exhibiting both high sensibility to the prodrugs 5-FC and ganciclovir. However, none of these results were observed in LS174T cells (KDR negative human colon carcinoma) [91, 92].
3. Conclusions
Tissue-specific promoters are able to improve gene delivery to tumor tissue, reducing at the same time the effect on healthy tissues and increasing the efficacy against cancer cells. Currently, a great amount of tumor-specific promoters are known and several in vivo and in vitro assays have revealed their specific activity in CRC, as well as their potential use. However, more assays will be needed in order to demonstrate and enhance their efficacy. One possibility is the use of enhancers, whose assays have proven to increase the transcriptional activity of these promoters. The use of tissue-specific promoters to deliver the expression of suicide genes for the selective killing of tumors may be a novel strategy for cancer treatment.
Acknowledgments
This research was funded by FEDER, Plan Nacional de Investigación Científica, Desarrollo e Innovación Tecnológica (I+D+I), and Instituto de Salud Carlos III (FIS), through projects PI11/01862 and PI11/0257.
Conflict of Interests
The authors declare no conflict of interests.
Authors' Contribution
All authors have contributed equally to the drafting of the paper. All authors read and approved the final version of the paper.
References
- 1.Jemal A., Bray F., Center M. M., Ferlay J., Ward E., Forman D. Global cancer statistics. CA: A Cancer Journal for Clinicians. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Van Cutsem E., Köhne C.-H., Hitre E., et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. The New England Journal of Medicine. 2009;360(14):1408–1417. doi: 10.1056/nejmoa0805019. [DOI] [PubMed] [Google Scholar]
- 3.Prados J., Melguizo C., Rama A. R., et al. Gef gene therapy enhances the therapeutic efficacy of doxorubicin to combat growth of MCF-7 breast cancer cells. Cancer Chemotherapy and Pharmacology. 2010;66(1):69–78. doi: 10.1007/s00280-009-1135-1. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz R., Prados J., Melguizo C., et al. 5-Fluorouracil-loaded poly(ε-caprolactone) nanoparticles combined with phage E gene therapy as a new strategy against colon cancer. International Journal of Nanomedicine. 2012;7:95–107. doi: 10.2147/IJN.S26401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rama A. R., Prados J., Melguizo C., et al. E phage gene transfection associated to chemotherapeutic agents increases apoptosis in lung and colon cancer cells. Bioengineered Bugs. 2011;2(3):163–167. doi: 10.4161/bbug.2.3.15533. [DOI] [PubMed] [Google Scholar]
- 6.Fukazawa T., Maeda Y., Matsuoka J., et al. Drug-regulatable cancer cell death induced by BID under control of the tissue-specific, lung cancer-targeted TTS promoter system. International Journal of Cancer. 2009;125(8):1975–1984. doi: 10.1002/ijc.24584. [DOI] [PubMed] [Google Scholar]
- 7.Lai Y.-H., Lin C.-C., Chen S.-H., Tai C.-K. Tumor-specific suicide gene therapy for hepatocellular carcinoma by transcriptionally targeted retroviral replicating vectors. Gene Therapy. 2015;22(2):155–162. doi: 10.1038/gt.2014.98. [DOI] [PubMed] [Google Scholar]
- 8.Cai X., Zhou J., Chang Y., Sun X., Li P., Lin J. Targeting gene therapy for hepatocarcinoma cells with the E. coli purine nucleoside phosphorylase suicide gene system directed by a chimeric α-fetoprotein promoter. Cancer Letters. 2008;264(1):71–82. doi: 10.1016/j.canlet.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 9.Vernimmen D., Gueders M., Pisvin S., Delvenne P., Winkler R. Different mechanisms are implicated in ERBB2 gene overexpression in breast and in other cancers. British Journal of Cancer. 2003;89(5):899–906. doi: 10.1038/sj.bjc.6601200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maeda T., O-Wang J., Matsubara H., et al. A minimum c-erbB-2 promoter-mediated expression of herpes simplex virus thymidine kinase gene confers selective cytotoxicity of human breast cancer cells to ganciclovir. Cancer Gene Therapy. 2001;8(11):890–896. doi: 10.1038/sj.cgt.7700389. [DOI] [PubMed] [Google Scholar]
- 11.Xie X., Bartholomeusz C., Ahmed A. A., et al. Bisphosphorylated PEA-15 sensitizes ovarian cancer cells to paclitaxel by impairing the microtubule-destabilizing effect of SCLIP. Molecular Cancer Therapeutics. 2013;12(6):1099–1111. doi: 10.1158/1535-7163.MCT-12-0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee J., Bartholomeusz C., Krishnamurthy S., et al. PEA-15 unphosphorylated at both serine 104 and serine 116 inhibits ovarian cancer cell tumorigenicity and progression through blocking beta-catenin. Oncogenesis. 2012;1, article e22 doi: 10.1038/oncsis.2012.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Botta G., Perruolo G., Libertini S., et al. PED/PEA-15 modulates coxsackievirus-adenovirus receptor expression and adenoviral infectivity via ERK-mediated signals in glioma cells. Human Gene Therapy. 2010;21(9):1067–1076. doi: 10.1089/hum.2009.181. [DOI] [PubMed] [Google Scholar]
- 14.Xie X., Tang H., Liu P., et al. Development of PEA-15 using a potent non-viral vector for therapeutic application in breast cancer. Cancer Letters. 2015;356(2):374–381. doi: 10.1016/j.canlet.2014.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang M., Wang J., Li C., et al. Potent growth-inhibitory effect of a dual cancer-specific oncolytic adenovirus expressing apoptin on prostate carcinoma. International Journal of Oncology. 2013;42(3):1052–1060. doi: 10.3892/ijo.2013.1783. [DOI] [PubMed] [Google Scholar]
- 16.Kovalenko O. A., Kaplunov J., Herbig U., detoledo S., Azzam E. I., Santos J. H. Expression of (NES-)hTERT in cancer cells delays cell cycle progression and increases sensitivity to genotoxic stress. PLoS ONE. 2010;5(5) doi: 10.1371/journal.pone.0010812.e10812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Panigrahi S., Klonisch T., Los M. The art of killing: double stroke with apoptin and survivin as a novel approach in cancer therapy. Cancer Biology and Therapy. 2008;7(7):1061–1062. doi: 10.4161/cbt.7.7.6492. [DOI] [PubMed] [Google Scholar]
- 18.Qiu Y., Peng G.-L., Liu Q.-C., Li F.-L., Zou X.-S., He J.-X. Selective killing of lung cancer cells using carcinoembryonic antigen promoter and double suicide genes, thymidine kinase and cytosine deaminase (pCEA-TK/CD) Cancer Letters. 2012;316(1):31–38. doi: 10.1016/j.canlet.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 19.Higashi K., Hazama S., Araki A., et al. A novel cancer vaccine strategy with combined IL-18 and HSV-TK gene therapy driven by the hTERT promoter in a murine colorectal cancer model. International Journal of Oncology. 2014;45(4):1412–1420. doi: 10.3892/ijo.2014.2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robbins K. C., Summaria L., Hsieh B., Shah R. J. The peptide chains of human plasmin. Mechanism of activation of human plasminogen to plasmin. The Journal of Biological Chemistry. 1967;242(10):2333–2342. [PubMed] [Google Scholar]
- 21.Long H., Li Q., Wang Y., Li Q., Liu T., Jie P. Effective combination gene therapy using CEACAM6-shRNA and the fusion suicide gene yCDglyTK for pancreatic carcinoma in vitro. Experimental and Therapeutic Medicine. 2013;5(1):155–161. doi: 10.3892/etm.2012.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou X., Xie G., Wang S., et al. Potent and specific antitumor effect for colorectal cancer by CEA and Rb double regulated oncolytic adenovirus harboring ST13 gene. PLoS ONE. 2012;7(10) doi: 10.1371/journal.pone.0047566.e47566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu C., Sun Y., Wang Y., et al. CEA promoter-regulated oncolytic adenovirus-mediated Hsp70 expression in immune gene therapy for pancreatic cancer. Cancer Letters. 2012;319(2):154–163. doi: 10.1016/j.canlet.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 24.Michl M., Koch J., Laubender R. P., et al. Tumor markers CEA and CA 19-9 correlate with radiological imaging in metastatic colorectal cancer patients receiving first-line chemotherapy. Tumor Biology. 2014;35(10):10121–10127. doi: 10.1007/s13277-014-2280-7. [DOI] [PubMed] [Google Scholar]
- 25.Wang W., Li Y., Zhang X., et al. Evaluating the significance of expression of CEA mRNA and levels of CEA and its related proteins in colorectal cancer patients. Journal of Surgical Oncology. 2014;109(5):440–444. doi: 10.1002/jso.23503. [DOI] [PubMed] [Google Scholar]
- 26.Shibutani M., Maeda K., Nagahara H., et al. Significance of CEA and CA19-9 combination as a prognostic indicator and for recurrence monitoring in patients with stage II colorectal cancer. Anticancer Research. 2014;34(7):3753–3758. [PubMed] [Google Scholar]
- 27.Vukobrat-Bijedic Z., Husic-Selimovic A., Sofic A., et al. Cancer antigens (CEA and CA 19-9) as markers of advanced stage of colorectal carcinoma. Medical Archives. 2013;67(6):397–401. doi: 10.5455/medarh.2013.67.397-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel M. M. Getting into the colon: approaches to target colorectal cancer. Expert Opinion on Drug Delivery. 2014;11(9):1343–1350. doi: 10.1517/17425247.2014.927440. [DOI] [PubMed] [Google Scholar]
- 29.Guo X., Evans T. R. J., Somanath S., et al. In vitro evaluation of cancer-specific NF-kappaB-CEA enhancer-promoter system for 5-fluorouracil prodrug gene therapy in colon cancer cell lines. British Journal of Cancer. 2007;97(6):745–754. doi: 10.1038/sj.bjc.6603930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang G., Liu T., Chen Y.-H., et al. Tissue specific cytotoxicity of colon cancer cells mediated by nanoparticle-delivered suicide gene in vitro and in vivo. Clinical Cancer Research. 2009;15(1):201–207. doi: 10.1158/1078-0432.ccr-08-1094. [DOI] [PubMed] [Google Scholar]
- 31.Liu T., Zhang G., Chen Y.-H., et al. Tissue specific expression of suicide genes delivered by nanoparticles inhibits gastric carcinoma growth. Cancer Biology & Therapy. 2006;5(12):1683–1690. doi: 10.4161/cbt.5.12.3379. [DOI] [PubMed] [Google Scholar]
- 32.Rama A. R., Hernandez R., Perazzoli G., et al. Specific colon cancer cell cytotoxicity induced by bacteriophage E gene expression under transcriptional control of carcinoembryonic antigen promoter. International Journal of Molecular Sciences. 2015;16(6):12601–12615. doi: 10.3390/ijms160612601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karahan N., Güney M., Baspinar S., Oral B., Kapucuoglu N., Mungan T. Expression of gelatinase (MMP-2 and MMP-9) and cyclooxygenase-2 (COX-2) in endometrial carcinoma. European Journal of Gynaecological Oncology. 2007;28(3):184–188. [PubMed] [Google Scholar]
- 34.Zhou L.-H., Hu Q., Sui H., et al. Tanshinone II—a inhibits angiogenesis through down regulation of COX-2 in human colorectal cancer. Asian Pacific Journal of Cancer Prevention. 2012;13(9):4453–4458. doi: 10.7314/apjcp.2012.13.9.4453. [DOI] [PubMed] [Google Scholar]
- 35.Mutoh M., Takahashi M., Wakabayashi K. Roles of prostanoids in colon carcinogenesis and their potential targeting for cancer chemoprevention. Current Pharmaceutical Design. 2006;12(19):2375–2382. doi: 10.2174/138161206777698972. [DOI] [PubMed] [Google Scholar]
- 36.Roelofs H. M. J., te Morsche R. H. M., van Heumen B. W. H., Nagengast F. M., Peters W. H. M. Over-expression of COX-2 mRNA in colorectal cancer. BMC Gastroenterology. 2014;14, article 1 doi: 10.1186/1471-230x-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lobo Prabhu K. C., Vu L., Chan S. K., et al. Predictive utility of cyclo-oxygenase-2 expression by colon and rectal cancer. American Journal of Surgery. 2014;207(5):712–716. doi: 10.1016/j.amjsurg.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 38.Wasilewicz M. P., Kołodziej B., Bojułko T., Kaczmarczyk M., Sulzyc-Bielicka V., Bielicki D. Expression of cyclooxygenase-2 in colonic polyps. Polskie Archiwum Medycyny Wewnetrznej. 2010;120(9):313–320. [PubMed] [Google Scholar]
- 39.Sheehan K. M., O'Connell F., O'Grady A., et al. The relationship between cyclooxygenase-2 expression and characteristics of malignant transformation in human colorectal adenomas. European Journal of Gastroenterology & Hepatology. 2004;16(6):619–625. doi: 10.1097/00042737-200406000-00017. [DOI] [PubMed] [Google Scholar]
- 40.Elzagheid A., Emaetig F., Alkikhia L., et al. High cyclooxygenase-2 expression is associated with advanced stages in colorectal cancer. Anticancer Research. 2013;33(8):3137–3143. [PubMed] [Google Scholar]
- 41.Mahmoud A. S., Umair A., Azzeghaiby S. N., Alqahtani F. H., Hanouneh S., Tarakji B. Expression of cyclooxygenase-2 (COX-2) in colorectal adenocarcinoma: an immunohistochemical and histopathological study. Asian Pacific Journal of Cancer Prevention. 2014;15(16):6787–6790. doi: 10.7314/apjcp.2014.15.16.6787. [DOI] [PubMed] [Google Scholar]
- 42.Soumaoro L. T., Uetake H., Higuchi T., Takagi Y., Enomoto M., Sugihara K. Cyclooxygenase-2 expression: a significant prognostic indicator for patients with colorectal cancer. Clinical Cancer Research. 2004;10(24):8465–8471. doi: 10.1158/1078-0432.ccr-04-0653. [DOI] [PubMed] [Google Scholar]
- 43.Kaliberova L. N., Kusmartsev S. A., Krendelchtchikova V., et al. Experimental cancer therapy using restoration of NAD+-linked 15-hydroxyprostaglandin dehydrogenase expression. Molecular Cancer Therapeutics. 2009;8(11):3130–3139. doi: 10.1158/1535-7163.mct-09-0270. [DOI] [PubMed] [Google Scholar]
- 44.Hoffmann D., Wildner O. Restriction of adenoviral replication to the transcriptional intersection of two different promoters for colorectal and pancreatic cancer treatment. Molecular Cancer Therapeutics. 2006;5(2):374–381. doi: 10.1158/1535-7163.MCT-05-0374. [DOI] [PubMed] [Google Scholar]
- 45.Wang Z.-X., Bian H.-B., Yang J.-S., De W., Ji X.-H. Adenovirus-mediated suicide gene therapy under the control of Cox-2 promoter for colorectal cancer. Cancer Biology & Therapy. 2009;8(15):1480–1488. doi: 10.4161/cbt.8.15.8940. [DOI] [PubMed] [Google Scholar]
- 46.T-Tomity I., Takács O. Investigations on the distribution of serum LDH isoenzymes of patients with carcinoma laryngis (author's transl) Laryngologie, Rhinologie, Otologie. 1979;58(12):916–919. [PubMed] [Google Scholar]
- 47.Ulusoy Ç., Darendeliler N. Effects of Class II activator and Class II activator high-pull headgear combination on the mandible: a 3-dimensional finite element stress analysis study. American Journal of Orthodontics & Dentofacial Orthopedics. 2008;133(4):490.e9–490.e15. doi: 10.1016/j.ajodo.2007.10.032. [DOI] [PubMed] [Google Scholar]
- 48.Zajjari Y., Benyahia M., Ibrahim D. M., et al. Non-diabetic renal disease in type II diabetes mellitus patients in Mohammed V military hospital, Rabat, Morocco. Eastern Mediterranean Health Journal. 2012;18(6):620–623. [PubMed] [Google Scholar]
- 49.Hollas W., Boyd D. Regulation of the urokinase receptor by its plasminogen activator. Thrombosis and Haemostasis. 1991;66(6):678–683. [PubMed] [Google Scholar]
- 50.Ganesh S., Sier C. M., Heerding M., Griffioen G., Lamers C. B., Verspaget H. W. Urokinase receptor and colorectal cancer survival. The Lancet. 1994;344(8919):401–402. doi: 10.1016/s0140-6736(94)91427-3. [DOI] [PubMed] [Google Scholar]
- 51.Sato S., Kopitz C., Grismayer B., et al. Overexpression of the urokinase receptor mRNA splice variant uPAR-del4/5 affects tumor-associated processes of breast cancer cells in vitro and in vivo. Breast Cancer Research and Treatment. 2011;127(3):649–657. doi: 10.1007/s10549-010-1042-5. [DOI] [PubMed] [Google Scholar]
- 52.Tomé-Amat J., Herrero-Galán E., Oñaderra M., Martínez-del-Pozo Á., Gavilanes J. G., Lacadena J. Preparation of an engineered safer immunotoxin against colon carcinoma based on the ribotoxin hirsutellin A. FEBS Journal. 2015;282(11):2131–2141. doi: 10.1111/febs.13262. [DOI] [PubMed] [Google Scholar]
- 53.Bendell J. C., Lenz H.-J., Ryan T., et al. Phase 1/2 study of KRN330, a fully human anti-A33 monoclonal antibody, plus irinotecan as second-line treatment for patients with metastatic colorectal cancer. Investigational New Drugs. 2014;32(4):682–690. doi: 10.1007/s10637-014-0088-3. [DOI] [PubMed] [Google Scholar]
- 54.Herbertson R. A., Tebbutt N. C., Lee F.-T., et al. Targeted chemoradiation in metastatic colorectal cancer: a phase I trial of 131I-huA33 with concurrent capecitabine. Journal of Nuclear Medicine. 2014;55(4):534–539. doi: 10.2967/jnumed.113.132761. [DOI] [PubMed] [Google Scholar]
- 55.Cafferata E. G., Macció D. R., Lopez M. V., et al. A novel A33 promoter-based conditionally replicative adenovirus suppresses tumor growth and eradicates hepatic metastases in human colon cancer models. Clinical Cancer Research. 2009;15(9):3037–3049. doi: 10.1158/1078-0432.ccr-08-1161. [DOI] [PubMed] [Google Scholar]
- 56.Mathonnet M., Descottes B., Valleix D., Labrousse F., Truffinet V., Denizot Y. Quantitative analysis using ELISA of vascular endothelial growth factor and basic fibroblast growth factor in human colorectal cancer, liver metastasis of colorectal cancer and hepatocellular carcinoma. World Journal of Gastroenterology. 2006;12(23):3782–3783. doi: 10.3748/wjg.v12.i23.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mathonnet M., Descottes B., Valleix D., Truffinet V., Labrousse F., Denizot Y. Platelet-activating factor in cirrhotic liver and hepatocellular carcinoma. World Journal of Gastroenterology. 2006;12(17):2773–2778. doi: 10.3748/wjg.v12.i17.2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bertorelle R., Briarava M., Rampazzo E., et al. Telomerase is an independent prognostic marker of overall survival in patients with colorectal cancer. British Journal of Cancer. 2013;108(2):278–284. doi: 10.1038/bjc.2012.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xiong J., Sun W.-J., Wang W.-F., et al. Novel, chimeric, cancer-specific, and radiation-inducible gene promoters for suicide gene therapy of cancer. Cancer. 2012;118(2):536–548. doi: 10.1002/cncr.26289. [DOI] [PubMed] [Google Scholar]
- 60.Chan G., Kamarudin M. N. A., Wong D. Z. H., et al. Mitigation of H 2O 2 -induced mitochondrial-mediated apoptosis in NG108-15 cells by novel mesuagenin C from Mesua kunstleri (King) kosterm. Evidence-Based Complementary and Alternative Medicine. 2012;2012:18. doi: 10.1155/2012/156521.156521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xie X., Hsu J. L., Choi M.-G., et al. A novel hTERT promoter-driven E1A therapeutic for ovarian cancer. Molecular Cancer Therapeutics. 2009;8(8):2375–2382. doi: 10.1158/1535-7163.MCT-09-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xie X., Tang H., Liu P., et al. Development of PEA-15 using a potent non-viral vector for therapeutic application in breast cancer. Cancer Letters. 2015;356(2, part B):374–381. doi: 10.1016/j.canlet.2014.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Byczkowska A., Kunikowska A., Kaźmierczak A. Determination of ACC-induced cell-programmed death in roots of Vicia faba ssp. minor seedlings by acridine orange and ethidium bromide staining. Protoplasma. 2013;250(1):121–128. doi: 10.1007/s00709-012-0383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rampazzo E., Bertorelle R., Serra L., et al. Relationship between telomere shortening, genetic instability, and site of tumour origin in colorectal cancers. British Journal of Cancer. 2010;102(8):1300–1305. doi: 10.1038/sj.bjc.6605644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li X., Liu Y., Wen Z., et al. Potent anti-tumor effects of a dual specific oncolytic adenovirus expressing apoptin in vitro and in vivo. Molecular Cancer. 2010;9, article 10 doi: 10.1186/1476-4598-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tan J., Li W., Wang P. Telomerase reverse transcriptase promoter-driven expression of iodine pump genes for targeted radioiodine therapy of malignant glioma cells. Chinese Journal of Cancer. 2011;30(8):574–580. doi: 10.5732/cjc.010.10580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu L., Wu W., Zhu G., et al. Therapeutic efficacy of an hTERT promoter-driven oncolytic adenovirus that expresses apoptin in gastric carcinoma. International Journal of Molecular Medicine. 2012;30(4):747–754. doi: 10.3892/ijmm.2012.1077. [DOI] [PubMed] [Google Scholar]
- 68.Yang G., Meng X., Sun L., et al. Antitumor effects of a dual cancer-specific oncolytic adenovirus on colorectal cancer in vitro and in vivo. Experimental and Therapeutic Medicine. 2015;9(2):327–334. doi: 10.3892/etm.2014.2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yoshimura K., Hazama S., Iizuka N., et al. Successful immunogene therapy using colon cancer cells (colon 26) transfected with plasmid vector containing mature interleukin-18 cDNA and the Igκ leader sequence. Cancer Gene Therapy. 2001;8(1):9–16. doi: 10.1038/sj.cgt.7700277. [DOI] [PubMed] [Google Scholar]
- 70.Choi I.-K., Lee J.-S., Zhang S.-N., et al. Oncolytic adenovirus co-expressing IL-12 and IL-18 improves tumor-specific immunity via differentiation of T cells expressing IL-12Rβ2 or IL-18Rα . Gene Therapy. 2011;18(9):898–909. doi: 10.1038/gt.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nielsen L. S., Hansen J. G., Skriver L., et al. Purification of zymogen to plasminogen activator from human glioblastoma cells by affinity chromatography with monoclonal antibody. Biochemistry. 1982;21(25):6410–6415. doi: 10.1021/bi00268a014. [DOI] [PubMed] [Google Scholar]
- 72.Allgayer H., Wang H., Shirasawa S., Sasazuki T., Boyd D. Targeted disruption of the K-Ras oncogene in an invasive colon cancer cell line down-regulates urokinase receptor expression and plasminogen-dependent proteolysis. British Journal of Cancer. 1999;80(12):1884–1891. doi: 10.1038/sj.bjc.6690616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hildenbrand R., Niedergethmann M., Marx A., et al. Amplification of the urokinase-type plasminogen activator receptor (uPAR) gene in ductal pancreatic carcinomas identifies a clinically high-risk group. The American Journal of Pathology. 2009;174(6):2246–2253. doi: 10.2353/ajpath.2009.080785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhou Y., Lü X., Li S., Zhan L. Correlation between the overexpression of urokinase receptor isoform uPAR (D1D2) and hepatic cell malignant transformation. Molecular Medicine Reports. 2014;9(5):1689–1696. doi: 10.3892/mmr.2014.2006. [DOI] [PubMed] [Google Scholar]
- 75.Grismayer B., Sato S., Kopitz C., et al. Overexpression of the urokinase receptor splice variant uPAR-del4/5 in breast cancer cells affects cell adhesion and invasion in a dose-dependent manner and modulates transcription of tumor-associated genes. Biological Chemistry. 2012;393(12):1449–1455. doi: 10.1515/hsz-2012-0206. [DOI] [PubMed] [Google Scholar]
- 76.Schewe D. M., Biller T., Maurer G., et al. Combination analysis of activator protein-1 family members, Sp1 and an activator protein-2α-related factor binding to different regions of the urokinase receptor gene in resected colorectal cancers. Clinical Cancer Research. 2005;11(24):8538–8548. doi: 10.1158/1078-0432.CCR-05-0786. [DOI] [PubMed] [Google Scholar]
- 77.Hollas W., Blasi F., Boyd D. Role of the urokinase receptor in facilitating extracellular matrix invasion by cultured colon cancer. Cancer Research. 1991;51(14):3690–3695. [PubMed] [Google Scholar]
- 78.Teimoori-Toolabi L., Azadmanesh K., Amanzadeh A., Zeinali S. Selective suicide gene therapy of colon cancer exploiting the urokinase plasminogen activator receptor promoter. BioDrugs. 2010;24(2):131–146. doi: 10.2165/11530840-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 79.Hajihosseini M. K., Heath J. K. Expression patterns of fibroblast growth factors-18 and -20 in mouse embryos is suggestive of novel roles in calvarial and limb development. Mechanisms of Development. 2002;113(1):79–83. doi: 10.1016/s0925-4773(01)00656-6. [DOI] [PubMed] [Google Scholar]
- 80.Davidson D., Blanc A., Filion D., et al. Fibroblast growth factor (FGF) 18 signals through FGF receptor 3 to promote chondrogenesis. The Journal of Biological Chemistry. 2005;280(21):20509–20515. doi: 10.1074/jbc.m410148200. [DOI] [PubMed] [Google Scholar]
- 81.Ohbayashi N., Shibayama M., Kurotaki Y., et al. FGF18 is required for normal cell proliferation and differentiation during osteogenesis and chondrogenesis. Genes and Development. 2002;16(7):870–879. doi: 10.1101/gad.965702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shimokawa T., Furukawa Y., Sakai M., et al. Involvement of the FGF18 gene in colorectal carcinogenesis, as a novel downstream target of the β-catenin/T-cell factor complex. Cancer Research. 2003;63(19):6116–6120. [PubMed] [Google Scholar]
- 83.Meng Q. H., Xu E., Hildebrandt M. A. T., et al. Genetic variants in the fibroblast growth factor pathway as potential markers of ovarian cancer risk, therapeutic response, and clinical outcome. Clinical Chemistry. 2014;60(1):222–232. doi: 10.1373/clinchem.2013.211490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sonvilla G., Allerstorfer S., Stättner S., et al. FGF18 in colorectal tumour cells: autocrine and paracrine effects. Carcinogenesis. 2008;29(1):15–24. doi: 10.1093/carcin/bgm202. [DOI] [PubMed] [Google Scholar]
- 85.Teimoori-Toolabi L., Azadmanesh K., Zeinali S. Selective suicide gene therapy of colon cancer cell lines exploiting fibroblast growth factor 18 promoter. Cancer Biotherapy and Radiopharmaceuticals. 2010;25(1):105–116. doi: 10.1089/cbr.2009.0643. [DOI] [PubMed] [Google Scholar]
- 86.Su G.-Q., Su G., Huang Z.-H. Adenovirus-mediated tissue-targeted expression of the CDglyTk gene for the treatment of breast cancer. Molecular Medicine Reports. 2012;6(2):321–329. doi: 10.3892/mmr.2012.925. [DOI] [PubMed] [Google Scholar]
- 87.Siemann D. W., Shi W. Efficacy of combined antiangiogenic and vascular disrupting agents in treatment of solid tumors. International Journal of Radiation Oncology Biology Physics. 2004;60(4):1233–1240. doi: 10.1016/j.ijrobp.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 88.Ma J., Li M., Mei L., et al. Double suicide genes driven by kinase domain insert containing receptor promoter selectively kill human lung cancer cells. Genetic Vaccines and Therapy. 2011;9, article 6 doi: 10.1186/1479-0556-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dong G., Guo X., Fu X., et al. Potentially functional genetic variants in KDR gene as prognostic markers in patients with resected colorectal cancer. Cancer Science. 2012;103(3):561–568. doi: 10.1111/j.1349-7006.2011.02194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hansen T. F., Sørensen F. B., Spindler K.-L. G., et al. Microvessel density and the association with single nucleotide polymorphisms of the vascular endothelial growth factor receptor 2 in patients with colorectal cancer. Virchows Archiv. 2010;456(3):251–260. doi: 10.1007/s00428-009-0878-8. [DOI] [PubMed] [Google Scholar]
- 91.Wang Z.-Y., Huang Z.-H., Li Q., Yao X.-J., Yu J.-L., Li Z. A double suicide gene system driven by KDR promoter selectively kills human colon adneocarcinoma SW480 cells. Journal of Southern Medical University. 2010;30(2):224–227. [PubMed] [Google Scholar]
- 92.Liu Y.-D., Wang S.-M., Huang Z.-H., Li Q. Effect of KDR recombinant adenovirus containing double suicide gene on the proliferation of human colon adneocarcinoma SW620 cells. Journal of Southern Medical University. 2009;29(5):887–893. [PubMed] [Google Scholar]