Abstract
Background
Methadone maintenance treatment (MMT) reduces the harms of opioid use disorder and is being rapidly scaled-up in China. This study evaluated the real-world implementation of MMT system in Wuhan, China.
Methods
Data extracted from electronic medical records collected in 2010 on 8,811 patients were used to compute for each patient indices of the prescribed and consumed daily methadone doses, an adherence index, dose adjustments following missed doses, the rates of opiate positive urine tests, self-reported drug use, injection drug use (IDU), and the duration of MMT exposure.
Findings
The modal daily doses prescribed were 60 mg and above for 68.5% of patients. Adherence was variable: 51% of patients attended less than 60% and 26% attended 80% to 100% of their treatment days; and patients with long MMT exposure had significantly higher adherence rates than patients with short MMT exposure. The differences between doses dispensed immediately before and after the interruption in dosing days ranged from 0 to 7 mg, independently of the length of the interruption or the prescribed dosing level. The overall rate of opiate positive tests was 20%; 45% of patients had at least one opiate positive test; 29% reported past month drug use and 53% of them reported past month IDU. Adherence and MMT exposure duration correlated significantly with the proportion of opiate negative urine tests (r=0.355, p<0.001; r=0.351, p<0.001, respectively). Treatment for males and females was comparable.
Conclusions
Provision of safe methadone dosing after absences and improving daily attendance are identified as priority improvement areas.
Keywords: Methadone maintenance treatment (MMT), Opioid use disorders, Treatment, China
1. INTRODUCTION
Problems with opiate use, injection drug use (IDU), and transmission of human immunodeficiency virus (HIV) are closely interrelated in China, which has an estimated 780,000 HIV infected individuals and over 2 million registered drug users (Kulsudjarit 2004; Lu and Wang, 2008; Meise et al., 2009; Ministry of Health of the People’s Republic of China, 2012; Narcotics Control Bureau of the Chinese Ministry of Public Security, 2013; Yin et al. 2010). Injection of drugs is associated with 42% of HIV transmissions, and about 45% of people who inject drugs in China are estimated to share needles and injection equipment (Chu and Levy, 2005; Meise et al., 2009; Lu and Wang, 2008). To address these problems, China has undertaken major initiatives over the past decade, including introduction and scale-up of methadone maintenance treatment (MMT; Shen and Yu, 2005; Wu et al., 2007). The early success of small pilot MMT programs introduced in 2004 (Pang et al., 2007) has been followed by rapid expansion of MMT programs (Chu and Levy, 2005; Lu and Wang, 2008; Tang et al., 2006; Shi et al., 2007; Yin et al., 2010) that follow standardized clinical protocols, and physicians providing MMT participate in a structured, centrally-run, national training. By the end of 2013, 412,686 patients had enrolled in 763 clinics established since 2005 (National Center of AIDS Prevention and Control, 2013). Earlier studies evaluating implementation and scale up of MMT programs across China reported use of lower than generally recommended dosages of methadone, misconceptions about MMT (e.g., that MMT is intended primarily for detoxification or short term treatment or that low doses are preferable to avoid perceived harm of methadone), paucity of counseling or other services offered in the clinics, irregular attendance by MMT patients, and high drop-out rates (Gu et al., 2012; Lin et al., 2011; Ren et al., 2013; Sullivan and Wu, 2007; Sullivan et al., 2013).
The current study is based on an initial evaluation of quality of care and treatment effectiveness measures of MMT services in Wuhan, China, which has 20 dispensaries or clinics with a cumulative enrollment between 2006 and 2010 of over 16,000 patients. The study findings, initiated ongoing quality improvement efforts aimed at improving the overall effectiveness of MMT in Wuhan. These quality improvement efforts include a review and revision of the current MMT guidelines and treatment protocols, improved and extended training and supervision of MMT doctors and nurses, and research to evaluate interventions that could be feasible and effective in improving the overall effectiveness of the MMT programs in China.
Data extracted for this study from electronic medical records of all patients enrolled in any of the MMT dispensaries or clinics operating in 2010 in Wuhan included patient characteristics, key MMT characteristics (including data on patterns of methadone dosing and patient attendance), and indicators of treatment response (self-reports of illicit drug use and urine toxicology tests results). Additionally, we explored the data for potential predictors of treatment efficacy and for gender differences.
2. METHODS
2.1. Setting
Wuhan is a sprawling and populous city in central China, with a total population of over 10 million. The first MMT dispensary or clinic opened in Wuhan in April, 2006. By 2010, Wuhan Centers for Disease Prevention and Control (CDC) managed a MMT system consisting of 20 satellite dispensaries (or clinics) covering 8 of the 13 urban districts within the Wuhan metropolitan area. All dispensaries were linked and monitored by a centrally managed computerized clinical database system. Dispensaries are either stand-alone facilities or co-located with detoxification programs or general medical or psychiatric hospitals. In 2010, patient enrollment in each dispensary varied between 177 and 1,606 patients. Each dispensary employed at least one medical doctor, who evaluated patients at treatment entry and prescribed the methadone, and a nurse or pharmacist who dispensed prescribed methadone and observed methadone ingestion. Methadone was dispensed in liquid form (1mg/1ml concentration). Patients were expected to attend clinic every day for their methadone dose, and there was no take-home dosing. At each clinic visit, patients were required to pay a fee of 10 RMB (~$1.50 USD in 2010) before receiving their methadone dose; the fee amount was fixed and did not depend on the methadone dose or the level of services received or offered at the clinic. Patients could meet with the doctor to discuss their methadone treatment (e.g., request a dose change) or other health concerns on an as needed basis. At least once per month, most dispensaries also offered an educational group covering topics such as prevention of common needle-borne infections, including HIV and Hepatitis C virus (HCV), the importance of methadone adherence and retention in treatment, and harms of drug use and overdose prevention. Attendance at such groups was voluntary, and typically only a small number of patients participated in them (less than 20 at each group meeting) (personal communication from Pulin Liu, Mar/Apr 2014). No other psychosocial interventions were offered as a part of the standard treatment.
MMT admission was restricted to opiate using local residents at least 18 years old (Meise et al., 2009; Tang et al., 2006a), and after 2006, admission did not require a history of failed prior detoxification attempts (Meise et al., 2009). Patients could miss medication without penalties and could resume treatment by simply returning to the clinic for treatment.
Other treatment options or services were very limited for people using opioids in Wuhan in 2010. Voluntary detoxification centers provided inpatient treatment for opioid, amphetamine-type stimulant, and ketamine use disorders. Some treatment and detoxification centers provided services based on traditional Chinese medicine (herbal medications and non-medication interventions such as acupuncture and massage; Tang et al., 2006a). There were also small needle exchange programs at two sites on the outskirts of Wuhan enrolling a total of about 100 individuals in 2010.
2.2. Data
The study used data from de-identified electronic medical records of all MMT patients who were active in treatment during the year 2010 (i.e., patients who received at least one dose of methadone between January 1 and December 31, 2010 in any of Wuhan’s MMT dispensaries/clinics). The database consists of data collected at treatment entry and follow-up updates collected yearly, including demographic information (e.g., sex, ethnicity, education, marital status, occupation, living situation, income source), drug use data (e.g., age of first use, number of times per day in past month using opiates, amount spent per day on opiates in the past month), behavioral patterns of drug use and risk behaviors (e.g., self-report on needle sharing frequency, drug use methods and routes of administration, sexual activity and condom use), selected social factors (e.g., arrests and crimes committed, family relationship, employment and sources of money, socialization with drug users), treatment history and current treatment related factors (e.g., transportation and commute to MMT clinic, satisfaction with treatment, usefulness of clinic hours, cost of treatment, adequacy of dosing, and satisfaction with the service quality of the clinic). Other data include the results of tests for tuberculosis collected at entry, HIV collected at entry and every 6 months, and syphilis and HCV collected at entry and yearly. Tuberculosis testing consists of a screening chest x-ray followed by confirmatory testing if abnormal. Patient level treatment data include results of urine toxicology tests for illicit opiate use (testing morphine metabolites only), scheduled to be collected monthly, and the dates and doses of methadone administered for each patient.
The characteristics of the study cohort are based on data collected by CDC between April of 2006 and December of 2010 (patient self-report data at treatment entry with follow-up updates, and results of the most current infectious disease test results). The study findings are based on medication dispensing records and urine toxicology results collected between January 1 and December 31, 2010, and the duration of MMT participation prior to active treatment in 2010.
2.3. Data Quality Assessments and Analytic Strategy
We first evaluated the extracted data for overall quality/accuracy and completeness using data quality checks and exploratory analytical tools. We evaluated the patterns of missing data, duplicate data, and patterns of dosing that could be indicative of errors (e.g., unusual changes in daily doses for the same patient). Of the 8,828 individual patients recorded as receiving methadone in 2010, 275 had multiple records of treatment entry data (i.e., the date when they first started methadone, baseline demographics). We used their earliest collected data. Seventeen patient identification numbers were associated with repeated doses in more than one dispensary on the same day. Since it could not be determined if this was the same person dosing in multiple dispensaries or if the same identification number was assigned to different people, we chose to exclude these identification numbers from the analysis. Our final sample for analysis included 8,811 patients.
2.4. Outcome measures
Based on data extracted from the database, we calculated the following process measures and treatment indices for each patient: 1) an episode of active treatment in 2010 was defined as a period between the first and the last recorded dose of methadone, where the patient did not miss more than 14 consecutive days of medication attendance; 2) The mean daily methadone dose delivered, based on the medication consumption data, was calculated as the mean of all doses during the active treatment episode where missing doses are coded as 0 mg; 3) the modal daily methadone dose prescribed was based on the modal (most frequent) value of all doses dispensed during the active treatment episode; 4) for patients who missed 1, 2, 3, 4, 5, 6, 7 to 14, and more than 14 consecutive methadone dosing days, we calculated the differences between the last dose received before and their first dose received after (resumption dose) each of the missing periods, and we compared the differences between these doses as a function of the patient’s prescribed dosing range prior to missing (below 40 mg, 40 to 59.9mg, 60 to 89.9 mg, and 90 mg and above); 5) an adherence index (percentage of days attending treatment and receiving methadone) was calculated as a ratio of days attending the clinic (taking methadone) to the total number of days in an episode of active treatment during 2010; 6) a proportion of urine tests positive for morphine; 7) the MMT exposure duration was calculated as a number of days between the first methadone dose ever received in MMT in Wuhan and the onset of the first treatment episode in 2010, and the MMT exposure rank was calculated using tertiles of the distribution of these values in the entire study sample. Consequently the study participants were classified into three groups: 1) those who started MMT within the past 9 months – short MMT, 2) those who started MMT between 9 and 18 months prior to 2010 – medium MMT; and 3) those who started MMT more than 18 months before their 2010 treatment episode – long MMT.
The clinical database used by the MMT programs in Wuhan does not include data on the missing doses or missed clinic visits. Only the doses that are dispensed and ingested by patients when they come to the clinic and their dates are recorded. The missing doses/visits are represented by missed or lapsed dates and records in the database. In our study, we first computationally supplemented the original database by inserting the missing/lapsed dates and inserting 0 mg as values of for the missing methadone doses before calculating the above defined dosing indicators for each study participant. Data extracted from the database of clinical records and the calculated process measures and indices were used in descriptive statistics to characterize the patient cohort and to evaluate the treatment implementation characteristics. Additionally, we used a regression analysis and the ANOVA to evaluate the relationship between the proportion of urine tests negative for opiates and the mean daily methadone dose delivered, the modal daily methadone dose prescribed, the treatment adherence index, the MMT exposure duration, and gender. Finally, characteristics and outcomes of male and female cohorts were compared using the analysis of variance (t-tests) for continuous variables.
3. RESULTS
3.1. Demographics and Drug Risk Behaviors
The mean (SD) patient age was 41 (7.3) years; range 18 to 72 years; 72.3% (6,217/8,596) were male; 71.6% (6,155/8,596) had a middle school education or less (typically to age 15); 76.2% (6,370/8,355) were living with family members; 59.1% (4,885/8,260) were financially supported by friends or family members, 38.2% (3,156/8,260) were financially supported by salary, temporary work or government assistance, and 2.7% (219/8,260) reported other unspecified sources of support.
At MMT entry, 96% (8,006/8,333) reported heroin alone as their preferred drug; 4% reported a preference for heroin combined with other drugs, or for morphine, benzodiazepines, or other non-specified drugs; 67% (5682/8473) reported injecting drugs in the past month, and 5% of them (294/5682) reported sharing needles in the past month. The mean (SD) age of first drug use was 28 (7.4) years, with 63 as the oldest reported age of initiation. The mean (SD) duration of lifetime drug use was 13.2 (5.5) years. In the month prior to treatment entry, patients reported the mean (SD) of using heroin 3.4 (3.3) times per day and spending 295 (222) RMB (approximately $45 USD in 2010) per day on drugs. The mean (SD) of MMT exposure duration in the study sample was 316 (241) days. See Table 1 for other demographic and drug use behaviors by the MMT duration ranks.
Table 1.
Baseline characteristics at treatment entry by duration in Methadone Maintenance Treatment (MMT) prior to 2010.*
| Demographics and Drug Use Patterns | Short MMT < 9 months |
Medium MMT 9 to 18 months |
Long MMT > 18 months |
||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | F value | P | |
| Age at entry into MMT | 40.3 (7.4) | 40.4 (7.3) | 40.0 (7.2) | 2.49 | 0.083 |
| Age of drug use initiation | 28.5 (7.7) | 28.4 (7.6) | 27.0 (6.9) | 32.88 | 0.000 |
| Daily frequency of drug use (past month) | 3.3 (4.0) | 3.19 (2.5) | 3.7 (3.1) | 17.99 | 0.000 |
| Total number of drug injections (past month) | 91.3 (51.5) | 98.4 (49.8) | 109.7 (56.6) | 59.10 | 0.000 |
| Daily drug cost (RMB) | 266.9 (208.7) | 278.3 (219.5) | 340.5 (229.6) | 89.73 | 0.000 |
| Risk Behaviors | Percent (n/N) | Percent (n/N) | Percent (n/N) | X2 | P |
| Injected drugs (past month) | 67.3 (1914/2842) | 65.1 (1847/2837) | 68.8 (1921/2794) | 8.65 | 0.013 |
| Sexually active (past month) | 49.0 (1368/2793) | 50.9 (1391/2735) | 62.9 (1723/2738) | 127.01 | 0.000 |
| Used condom during last activity | 28.3 (384/1356) | 22.1 (299/1351) | 16.1 (269/1669) | 65.59 | 0.000 |
| Exchanged sex for drugs (past 3 months) | 0.4 (12/2828) | 0.5 (13/2823) | 0.7 (19/2785) | 2.10 | 0.349 |
| Arrested (past 3 months) | 3.0 (86/2836) | 3.2 (90/2827) | 3.8 (106/2792) | 2.85 | 0.240 |
| Committed crime to obtain drugs (past 3 months) | 0.9 (25/2833) | 1.2 (35/2825) | 2.0 (57/2793) | 14.48 | 0.001 |
| Trafficked drugs (past 3 months) | 0.4 (10/2826) | 1.0 (28/2830) | 1.7 (48/2793) | 26.00 | 0.000 |
| Rates of Infectious Diseases | Percent (n/N) | Percent (n/N) | Percent (n/N) | X2 | P |
| HIV | 0.5 (7/1495) | 0.3 (7/2215) | 0.3 (8/2663) | 0.87 | 0.648 |
| HCV | 67.3 (1083/1610) | 70.9 (1599/2254) | 79.8 (2090/2620) | 92.78 | 0.000 |
| Syphilis (RPR) | 3.4 (58/1719) | 2.9 (63/2172) | 1.7 (40/2402) | 13.29 | 0.001 |
| TB | 0.7 (4/594) | 0.9 (9/1005) | 0.5 (7/1532) | 1.85 | 0.396 |
Based on patient self-report data at treatment entry collected by Wuhan CDC between April of 2006 and December of 2010.
3.2. Methadone dosing and adherence
While the modal daily methadone dose prescribed was 60 mg or more for 68.5% of patients, the mean daily methadone dose delivered was below 60 mg for 81.6% of patients and 55.1% received/ingested a mean daily delivered dose of less than 40 mg (see Figure 1).
Fig. 1.
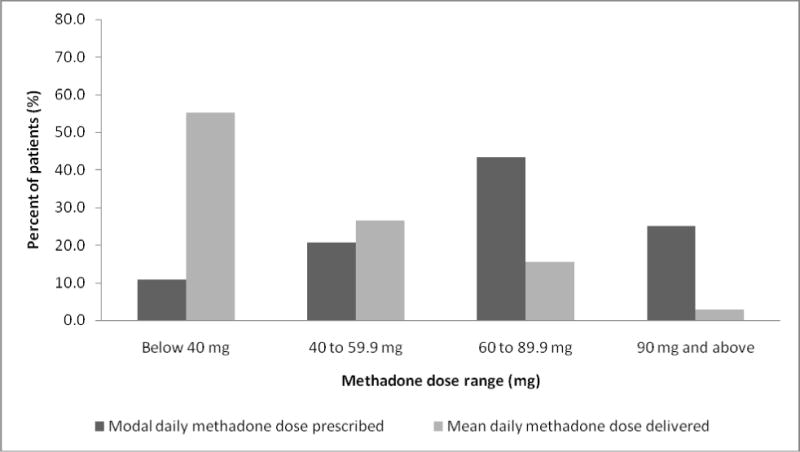
Distributions of prescribed and delivered methadone doses in 2010.
In the entire study sample, the majority (51.4%) of patients attended the clinics and ingested methadone on less than 60% of days in active treatment; 22.8% attended the clinics and ingested their prescribed daily maintenance doses on 60 to 79.9% of days, and 25.8% attended the clinics and ingested their prescribed daily maintenance doses on 80 to100% days in active treatment.
The analyses of methadone dosing and adherence data show different patterns of results for different groups of patients based on their MMT exposure rank. While the distribution of the modal daily methadone doses prescribed does not differ substantially between the patients with short, medium, and long MMT exposure (see Figure 2a), the distribution of the mean daily methadone doses delivered and adherence levels show that substantially more patients with long MMT exposure (28.9%) than patients with short MMT exposure (10%) had taken the mean daily methadone doses of 60 mg and above, see Figure 2b).
Fig. 2.
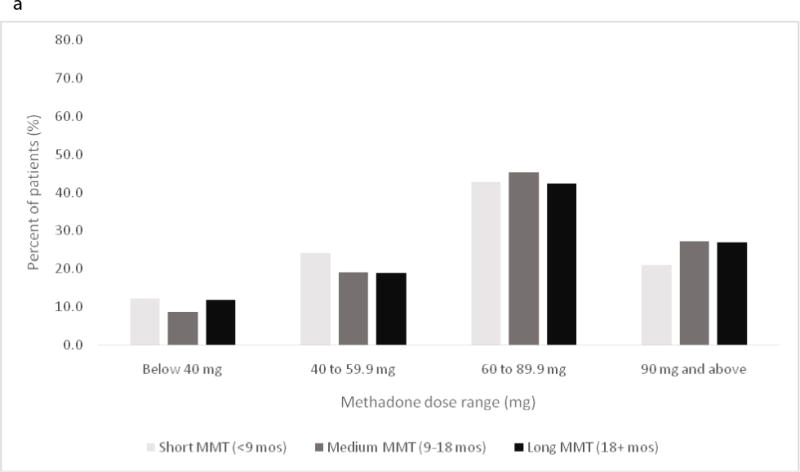
a. Distributions of the modal daily methadone maintenance dose prescribed across the three durations of MMT exposure in 2010. b. Distributions of the mean daily methadone dose delivered across the three durations of MMT exposure in 2010
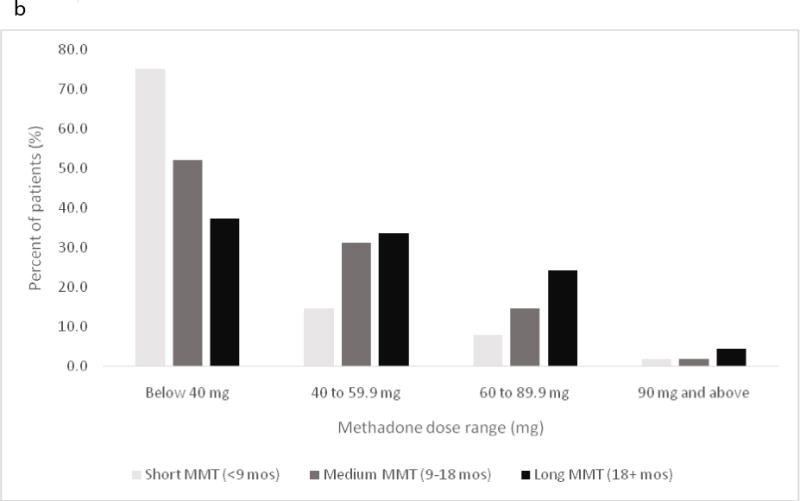
Similarly, substantially more patients with long MMT exposure (44.2%) attended the clinics and ingested 80 to 100% of their prescribed daily maintenance doses than patients with short MMT exposure (16.2% of these patients attended the clinics and ingested 80 to 100% of their prescribed daily maintenance doses) (See Figure 3). There were also statistically significant differences in the overall means of the adherence index among the three MMT exposure duration groups: 48% in the short MMT exposure group; 58% in the medium MMT exposure group; and 72% in the long MMT exposure group (F(2,8810)=798, p<0.001).
Fig. 3.
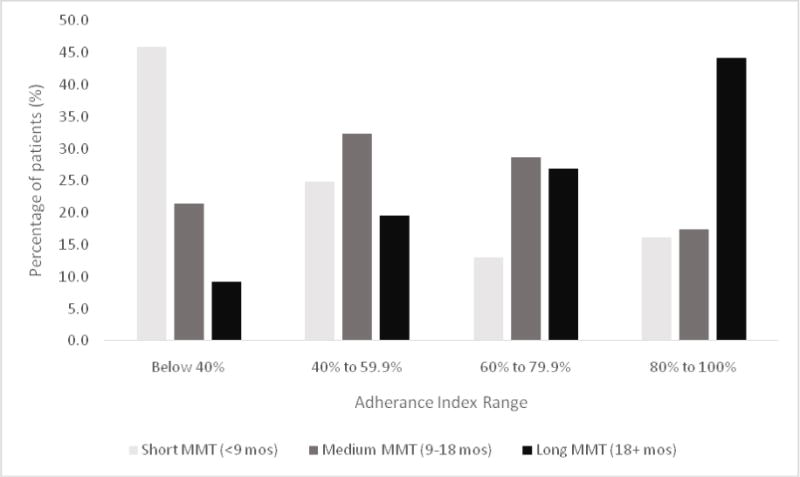
Distribution of patients with different levels of daily adherence across the three durations of MMT exposure in 2010.
The mean difference between the last methadone dose dispensed before missing 1, 2, 3, 4, 5, 6, 7–14, and more than 14 consecutive days of methadone dosing ranged from 0 mg to 7 mg regardless of the prescribed dosing range prior to missing (below 40 mg, 40 to 59.9 mg, 60 to 89.9 mg, and 90 mg and above), the number of days missed before resumption of methadone dosing, or their MMT exposure duration. There were 9,882 dosing instances (involving 3,226 patients) in 2010 where a patient received a resumption methadone dose of 60 mg or more (range 60 to 230 mg) after missing between 7 and 14 days of dosing.
3.3. Drug use during treatment
Past month drug use (during MMT treatment in 2010) was reported by 29.2% (1,572/5,392), and 52.5% of those who reported drug use (826/1,572) also reported IDU in the past month. Additionally, 45.4% (3,374/7,429) of patients had at least one opiate positive test during MMT treatment in 2010, and the overall mean (SD) of all opiate positive tests in the study sample was 20% (30%). There were also statistically significant differences in the overall rates of opiate positive urine test results among the three MMT exposure duration groups: 37% in the short MMT exposure group; 16% in the medium MMT exposure group; and 10% in the long MMT exposure group (F(2,7428)=615, p<0.001). The reported rates of drug use and injection drug use during MMT also differed significantly across the three MMT exposure duration groups: in the short MMT duration group, 40% reported drug use in the past month and 26% reported injection drug use in the past month, in the long MMT duration group, 27% reported drug use in the past month and 7% reported injection drug use in the past month (p<0.001 for both variables).
In the regression analysis, adherence with daily methadone dosing and MMT exposure duration correlated significantly (r=0.355, p<0.001; r=0.351, p<0.001, respectively) with the proportion of opiate negative urine tests; the mean daily methadone dose delivered, the modal daily methadone dose prescribed, and gender were not significantly associated with the proportion of opiate-negative tests (p=0.400, p=0.486, and p=0.878, respectively).
3.4. Gender Differences
At treatment entry, female compared to male patients were significantly younger, had an earlier age at initiation of drug use, had fewer years of drug use, and were more likely to have been sexually active in the past month and more likely to have exchanged in sexual acts for drugs in the past three months (all p values < 0.001; see Table 2 for details). During treatment, there were no significant differences between female and male patients in the proportions of opiate-negative urine toxicology tests (p=0.8) or patterns of methadone adherence (p=0.5). There were small differences between females and males in the mean daily methadone dose delivered (42 mg vs. 39 mg) and the modal daily methadone dose prescribed (72 mg vs. 58 mg).
Table 2.
Baseline characteristics of male and female MMT patients in 2010.*
| Demographics and Drug Use Patterns | Females | Males | ||
|---|---|---|---|---|
| Mean (SD), n | Mean (SD), n | t-test | P | |
| Age at entry into MMT | 39.4 (7.0) n=2379 |
41.8 (7.3) n=6,217 |
13.5 | <0.001 |
| Age at initiation of drug use | 26.9 (7.3) n=2316 |
28.4 (7.4) n=6047 |
8.59 | <0.001 |
| Years of drug use | 12.6 (5.3) n=2316 |
13.3 (5.6) n=6047 |
5.73 | <0.001 |
| Daily frequency of drug use in the past month | 3.4 (2.9) n=2291 |
3.4 (3.4) n=6003 |
0.85 | <0.001 |
| Total number of injections in the past month | 104.7 (59.9) n=1569 |
97.9 (50.4) n=4094 |
4.27 | <0.001 |
| Daily drug cost (RMB) | 311.8 (237.4) n=2300 |
288.5 (215.0) n=6003 |
4.3 | <0.001 |
| Number of sexual partners (past three months) | 1.1 (2.5) n=1379 |
1.02 (1.1) n=3195 |
1.06 | 0.291 |
| Risk Behaviors | Females | Males | ||
| Percent (n/N) | Percent (n/N) | x2 (1 df) | P | |
| Injected drugs (past month) | 67.1 (1574/2345) | 67.0 (4109/6128) | 0.01 | 0.94 |
| Sexually active (past month) | 58.8 (1348/2291) | 52.5 (3134/5975) | 27.2 | <0.001 |
| Used condom during last activity | 23.0 (306/1333) | 21.2 (646/3043) | 1.62 | 0.203 |
| Exchanged sex for drugs (past 3 months) | 1.1 (25/2334) | 0.3 (19/6102) | 18.8 | <0.001 |
| Arrested (past 3 months) | 2.7 (62/2340) | 3.6 (220/6115) | 4.719 | 0.03 |
| Committed crime to obtain drugs (past 3 months) | 0.9 (20/2338) | 1.6 (97/6113) | 6.625 | 0.01 |
| Trafficked drugs (past 3 months) | 0.6 (13/2342) | 1.2 (73/6107) | 6.89 | 0.009 |
Based on patient self-report data at treatment entry collected by Wuhan CDC between April of 2006 and December of 2010.
4. DISCUSSION
This study assessing all methadone maintained patients in Wuhan, China, found that a low proportion of patients adhered adequately to daily methadone dosing—overall, only 25.8% received 80% or more of their daily doses while in treatment—and a significant correlation between poor adherence to daily treatment regimen and ongoing illicit opiate use during treatment. Additionally, the study found that when methadone dispensing was resumed for patients even following prolonged periods of missed methadone dosing, the methadone doses were not reduced in consideration of the loss of tolerance to methadone, potentially putting patients at risk of opiate overdose. Although China has undertaken a massive expansion of MMT in order to reduce problems with drug use and HIV transmission, the findings suggest that there is significant room for improving MMT implementation and treatment outcomes in China.
The study findings also show a strong effect of the duration of exposure to MMT on improved daily adherence to treatment and consequently on the mean daily methadone doses delivered and ingested and on improved drug use outcomes. There are several possible interpretations of these findings. One is that staying in MMT longer leads to better treatment outcomes (Ward et al., 1999; Zhang et al., 2003). Alternatively, those who entered treatment earlier may have different characteristics than those who came later (though, in our study, there were no clinically meaningful differences in their baseline data), or those who remain in treatment the longest are those who are doing well, while those who entered at the same time but had worse outcomes were no longer in treatment in 2010. Future studies can be designed to provide better explanations for these findings.
The research evidence accumulated to date and supported by the findings of the current study, underscores some broad similarities between China, the U.S. and other countries in challenges of treating people with opioid use disorder, despite vast differences in environment, culture, and socioeconomic opportunities. The patterns of daily methadone adherence found in the current study are compatible with problems of inconsistent treatment participation and suboptimal retention reported in several earlier studies in China, and elsewhere in the world (Gu et al., 2012; Lawrinson et al., 2008; Sullivan et al., 2013; Wu et al., 2013; Zhang et al., 2013). One study of 58 methadone programs in low and middle income countries with 27,047 participants found that the average retention after 12 months was 54.3% and comparable to retention rates in high income countries (Feelemyer et al., 2014).
Possible reasons for low adherence observed in the current study include both patient-related factors associated with having a substance use disorder (e.g., overall disorganization, poor decision-making, potentially impaired cognitive functions and impulsivity) and program-related or societal factors, including lack of understanding among patients and clinical personnel about the effective ways to use methadone, requiring daily payment of fees which may be a disincentive to daily attendance, and problems with accessibility of treatment, including transportation difficulties, distance to clinics, limited treatment hours, and interference with work or other responsibilities (Wu et al., 2013). An additional barrier to adherence is the possibility of arrest for drug use by public security officers targeting patients entering and leaving methadone clinics (Meng and Burris, 2013; Yang et al., 2014; Zhang et al., 2013).
The very limited services provided along with methadone in Wuhan MMT programs are comparable to low-intensity or minimal services programs that have been evaluated elsewhere, most notably by McLellan et al., (1993). While low-intensity or minimum services programs offered benefits over no treatment (Schwartz et al., 2006, 2007), they were found sub-optimal for the majority of MMT patients (Deering et al., 2014; McLellan et al., 1993), and the results of the current study are in line with these other findings. Regardless of the reasons for low adherence, missed doses leave patients at increased risk for opioid withdrawal, craving, and relapse, as reflected in the study findings that low adherence with daily methadone dosing was associated with illicit opiate use during treatment. Offering additional effective interventions educating patients about the benefits of high adherence to methadone treatment and/or helping them to develop skills and plans focusing on improved treatment adherence may also potentially lead to improved overall attendance.
The findings that physicians prescribed doses on average 60 mg/day or greater indicate good compliance with China CDC treatment recommendations regarding methadone doses (Yin et al., 2010). However, due to a low adherence to daily clinic attendance and missing of prescribed daily maintenance doses, the average ingested dose was low, below 40 mg/day for the majority of MMT patients in 2010. This finding is consistent with earlier studies elsewhere. For example, a study evaluating 17 years of methadone prescribing in the US found that “Thirty-four percent of patients receive doses below 60 mg/day, while 17 percent receive doses below 40 mg/day”(Pollack et al., 2008).
The finding that the methadone dose was not reduced following missed doses, even after more than one week of missed medications and even for patients receiving higher methadone dosages, raises important safety concerns, since patients can quickly lose tolerance to methadone after their last dose and are at risk of methadone overdose if they are reinitiated at a high dose (Baxter et al., 2013). The finding that doses were not reduced following prolonged absences also suggests that physicians (as well as patients) do not fully appreciate the risks of methadone treatment, how it works, and appropriate safe and effective prescribing practices.
Nearly half of the patients had at least one opiate positive urine test during MMT. Although the overall proportion of opiate-positive urine tests during treatment was relatively low, this rate may underestimate the extent of use because urine toxicology tests were infrequent and often missed in part because of poor clinic attendance. While urine tests are planned/scheduled for each patient once per month in Wuhan MMT programs, in reality they were obtained when patients presented to the clinic, not truly randomly, and collected less often than intended weakening the potential clinical utility of this data.
Gender did not markedly affect treatment characteristics or treatment outcomes (28% of patients were female). The statistically significant differences between male and female drug users obtained in these comparisons are primarily driven by the large sample size and are of limited clinical importance. Both females and males had similar rates of subtherapeutic ingested daily doses (78% for females and 71% for males). Adherence with treatment was low in both groups, with only 25% of females and 26% of males coming to the clinic and receiving prescribed medication on 80 to 100% of treatment days. Since the outcomes and problems experienced for males and females were similar, the study findings suggest that general approaches to improving treatment and treatment outcomes may be of greater value at present than developing gender-specific interventions.
4.1. Study limitations
While providing a very large pool of real-world data, the database comes from one city in China, and the results of the current study may not generalize to all of China or other countries. Differences in patient populations (e.g., the prevalence of HIV in Wuhan patients was less than 0.5% in 2010, considerably lower than in some other regions of China), and potential differences in program implementation may limit the generalizability of the findings. Nonetheless, it is important to note that the Wuhan MMT program follows the same clinical guidelines and protocols used throughout China, its MMT patient population is similar to many urban regions of China with a large proportion of IDUs and a high prevalence of HCV, and Wuhan MMT physicians receive the same education, training, and monitoring as MMT physicians throughout China.
Additionally, the database was designed for clinical monitoring and not for research. There are missing baseline and self-report data. Self-report data cannot be independently verified for accuracy. Urine toxicology screens were obtained when patients presented to the clinic, not truly randomly or collected as often as intended. Other than methadone dosing, self-reported drug use, and morphine-derivative urine toxicology, there is little information about other drug use or other services provided, co-morbid psychiatric conditions, or other treatment outcomes. When patients enter the MMT program, they are evaluated using a standard set of questions regarding their demographics, drug use and related history, risk behaviors, and they are also tested for infectious diseases. Throughout their MMT participation, patients data obtained at baseline is updated (repeated evaluations and tests). Despite the MMT staff efforts to update all patients data regularly at uniform intervals, the available database is not completely up-to date (patients miss repeated evaluations for various reasons, and there are no incentives or penalties related to missed evaluations). In our study, we used the latest available record for each of the study participants. Data limitations related to varying timing of the available data records may also have contributed to the observed lack of differences among various study groups.
4.2. Conclusions
The rapid expansion of MMT in China has attracted a large number of admissions, and treatment for males and females appears clinically comparable. Problems documented by the study, including problems providing safe methadone dosing after absences, ensuring that patients receive effective methadone dosages (consistent with known standards for efficacy), and implementing structural or programmatic changes and supplemental interventions aimed at improving treatment adherence and effectiveness have been identified as priority quality improvement areas in China. Based on the findings of the current study and on findings from another recently published study by our team (Zhou et al.,2015), some of the initiatives currently being implemented by the Wuhan CDC include: developing improved guidelines concerning methadone dosing, including safe-dosing of patients who miss medication; developing procedures to incentivize patients to maintain high levels of daily adherence by modifying the required payment schedules; improving educational and drug counseling capacity and expertise in MMT clinics (including increasing training opportunities for MMT physicians and nurses); strengthening communication and collaboration between the MMT personnel and the local police/security organizations to eliminate or minimize the threats/risks to MMT patients resulting from the police and security forces operating in close proximity to MMT clinics; improving data, and data reporting capabilities of the computerized monitoring systems implemented in MMT programs in Wuhan. Additionally, in collaboration with the study investigators, Wuhan CDC is also undertaking a large randomized clinical trial (RCT) evaluating the feasibility and the efficacy of adding different counseling models to standard MMT in China.
Table 3.
Comparison of females (n=2379) and males (n=6217) on methadone doses and adherence.*
| Females | Males | |
|---|---|---|
| Percent (n/N) | Percent (n/N) | |
| Mean Daily Methadone Dose Delivered | ||
| Below 40 mg | 52.2 (1242) | 56.2 (3491) |
| 40 to 59.9 mg | 26.7 (636) | 26.5 (1645) |
| 60 to 89.9 mg | 17.8 (424) | 14.8 (922) |
| 90 mg and above | 3.2 (77) | 2.6 (159) |
| Modal Daily Methadone Dose Prescribed | ||
| Below 40 mg | 9.3 (222) | 11.1 (693) |
| 40 to 59.9 mg | 18.5 (440) | 21.3 (1325) |
| 60 to 89.9 mg | 43.3 (1030) | 44.0 (2735) |
| 90 mg and above | 28.9 (687) | 23.5 (1464) |
| Adherence Index | ||
| Below 40% | 25.8 (613) | 25.9 (1613) |
| 40 to 59.9% | 26.2 (623) | 25.6 (1594) |
| 60 to 79.9% | 23.5 (560) | 22.5 (1398) |
| 80 to 100% | 24.5 (583) | 25.9 (1612) |
The mean daily methadone dose delivered was calculated as the mean of all doses during the active treatment episode where missing doses are coded as 0 mg; the modal daily methadone dose prescribed was based on the modal (most frequent) value of all doses dispensed during the active treatment episode; an adherence index (percentage of days attending treatment and receiving methadone) was calculated as a ratio of days attending the clinic (taking methadone) to the total number of days in an episode of active treatment during 2010.
The study evaluated the real-world implementation of a large methadone maintenance treatment (MMT) system in China
Electronic medical records on 8,811 patients were used to compute process and outcome measures
Methadone dosing protocols and daily attendance are identified as priority areas for improving treatment
Acknowledgments
Role of Funding Source: The study was supported by China CDC, NIDA DA026797 (PI: Marek C. Chawarski), and the Connecticut Mental Health Center, Department of Mental Health and Addiction Services. None of these institutions influenced the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
None of the authors have conflicts of interest to declare.
Contributors
Authors Carla Marienfeld, Pulin Liu, Xia Wang, Richard Schottenfeld, Wang Zhou, and Marek Chawarskiconceived and designed the study. Authors Pulin Liu, Xia Wang, Wang Zhou, and Marek Chawarski participated in data acquisition. Authors Carla Marienfeld, Pulin Liu, Xia Wang, and Marek Chawarski conducted statistical analyses of data. Authors Carla Marienfeld, Pulin Liu, and Marek Chawarski conducted and managed the literature searches and summaries of previous and related work and prepared tables and figures. All authors participated in interpretation of the study findings and in writing and editing of the manuscript.
Contributor Information
Wang Zhou, Email: wzhou@whcdc.org.
Marek C. Chawarski, Email: marek.chawarski@yale.edu.
References
- Baxter LE, Campbell A, Deshields M, Levounis P, Martin JA, McNicholas L, Payte JT, Salsitz EA, Taylor T, Wilford BB. Safe methadone induction and stabilization: report of an expert panel. J Addict Med. 2013;7:377–386. doi: 10.1097/01.ADM.0000435321.39251.d7. [DOI] [PubMed] [Google Scholar]
- Chu TX, Levy JA. Injection drug use and HIV/AIDS transmission in China. Cell Res. 2005;15:865–869. doi: 10.1038/sj.cr.7290360. [DOI] [PubMed] [Google Scholar]
- Deering D, Sellman DJ, Adamson S. Opioid substitution treatment in New Zealand: a 40 year perspective. N Z Med J. 2014;127:57–66. [PubMed] [Google Scholar]
- Feelemyer J, Des Jarlais D, Arasteh K, Abdul-Quader AS, Hagan H. Retention of participants in medication-assisted programs in low- and middle-income countries: an international systematic review. Addiction. 2014;109:20–32. doi: 10.1111/add.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J, Xu H, Lau JT, Hao Y, Zhong Y, Fan L, Zhao Y, Hao C, Ling W. Misconceptions predict dropout and poor adherence prospectively among newly admitted first-time methadone maintenance treatment clients in Guangzhou, China. Addiction. 2012;107:1641–1649. doi: 10.1111/j.1360-0443.2012.03859.x. [DOI] [PubMed] [Google Scholar]
- Lawrinson P, Ali R, Buavirat A, Chiamwongpaet S, Dvoryak S, Habrat B, Jie S, Mardiati R, Mokri A, Moskalewicz J, Newcombe D, Poznyak V, Subata E, Uchtenhagen A, Utami DS, Vial R, Zhao C. Key findings from the WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS. Addiction. 2008;103:1484–1492. doi: 10.1111/j.1360-0443.2008.02249.x. [DOI] [PubMed] [Google Scholar]
- Lin C, Wu Z, Detels R. Opiate users’ perceived barriers against attending methadone maintenance therapy: a qualitative study in China. Subst Use Misuse. 2011;46:1190–1198. doi: 10.3109/10826084.2011.561905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L, Wang X. Drug Addiction in China. Ann N Y Acad Sci. 2008;1141:304–317. doi: 10.1196/annals.1441.025. [DOI] [PubMed] [Google Scholar]
- McLellan TA, Arndt IO, Metzger DS, Woody GE, O’Brien ChP. The effects of psychosocial services in substance abuse treatment. JAMA. 1993;269:1953–1959. [PubMed] [Google Scholar]
- Meise M, Wang X, Sauter ML, Bao Y-p, Shi J, Liu Z-m, Lu L. Harm reduction for injecting opiate users: an update and implications in China. Acta Pharmacologica Sinica. 2009;30:513–521. doi: 10.1038/aps.2009.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng J, Burris S. The role of the Chinese police in methadone maintenance therapy: a literature review. Int J Drug Policy. 2013;24:e25–34. doi: 10.1016/j.drugpo.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Ministry of Health of the People’s Republic of China. 2012 China AIDS Response Progress Report 2012 [Google Scholar]
- Narcotics Control Bureau of the Chinese Ministry of Public Security. Annual report on drug control in China 2013 2013 [Google Scholar]
- National Center of AIDS Prevention and Control (NCAIDS) Annual Report. 2013 [Google Scholar]
- Pang L, Hao Y, Mi G, Wang C, Luo W, Rou K, Li J, Wu Z. Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS 21 Suppl. 2007;8:S103–107. doi: 10.1097/01.aids.0000304704.71917.64. [DOI] [PubMed] [Google Scholar]
- Pollack HA, D’Aunno T. Dosage patterns in methadone treatment: results from a national survey, 1988–2005. Health Serv Res. 2008;43:2143–2163. doi: 10.1111/j.1475-6773.2008.00870.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren J, Ning Z, Asche CV, Zhuang M, Kirkness CS, Ye X, Fu J, Pan Q. Trends and predictors in methadone maintenance treatment dropout in Shanghai, China: 2005–2011. Curr Med Res Opin. 2013;29:731–738. doi: 10.1185/03007995.2013.796284. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Highfield DA, Jaffe JH, Brady JV, Butler CB, Rouse CO, Callaman JM, O’Grady KE, Battjes RJ. A randomized controlled trial of interim methadone maintenance. Arch Gen Psychiatry. 2006;63:102–109. doi: 10.1001/archpsyc.63.1.102. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Jaffe JH, Highfield DA, Callaman JM, O’Grady KE. A randomized controlled trial of interim methadone maintenance: 10-Month follow-up. Drug Alcohol Depend. 2007;5:30–36. doi: 10.1016/j.drugalcdep.2006.04.017. [DOI] [PubMed] [Google Scholar]
- Shen J, Yu DB. Governmental policies on HIV infection in China. Cell Res. 2005;15:903–907. doi: 10.1038/sj.cr.7290366. [DOI] [PubMed] [Google Scholar]
- Shi J, Zhao LY, Epstein DH, Zhao C, Shuai Y, Yan B, Jin J, Lu L. The effect of methadone maintenance on illicit opioid use, human immunodeficiency virus and hepatitis C virus infection, health status, employment, and criminal activity among heroin abusers during 6 months of treatment in china. J Addict Med. 2007;1:186–190. doi: 10.1097/ADM.0b013e318156cc19. [DOI] [PubMed] [Google Scholar]
- Sullivan S, Wu Z. Rapid scale up of harm reduction in China. Int J Drug Policy. 2007;18:118–128. doi: 10.1016/j.drugpo.2006.11.014. [DOI] [PubMed] [Google Scholar]
- Sullivan SG, Wu Z, Detels R, Group NMMTW Time to first treatment interruption in the Chinese methadone maintenance treatment programme. Drug Alcohol Depend. 2013;133:427–432. doi: 10.1016/j.drugalcdep.2013.06.021. [DOI] [PubMed] [Google Scholar]
- Tang Y-l, Zhao D, Zhao C, Cubells JF. Opiate addiction in China: current situation and treatments. Addiction. 2006a;101:657–665. doi: 10.1111/j.1360-0443.2006.01367.x. [DOI] [PubMed] [Google Scholar]
- Tang YL, Zhao D, Zhao C, Cubells JF. Opiate addiction in China: current situation and treatments. Addiction. 2006b;101:657–665. doi: 10.1111/j.1360-0443.2006.01367.x. [DOI] [PubMed] [Google Scholar]
- Ward J, Hall W, Mattick RP. Role of maintenance treatment in opioid dependence. Lancet. 1999;353:221–226. doi: 10.1016/S0140-6736(98)05356-2. [DOI] [PubMed] [Google Scholar]
- Wu F, Peng CY, Jiang H, Zhang R, Zhao M, Li J, Hser YI. Methadone maintenance treatment in China: perceived challenges from the perspectives of service providers and patients. J Public Health. 2013;35:206–212. doi: 10.1093/pubmed/fds079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369:679–690. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M, Zhou L, Hao W, Xiao SY. Drug policy in China: progress and challenges. Lancet. 2014;383:509. doi: 10.1016/S0140-6736(14)60175-6. [DOI] [PubMed] [Google Scholar]
- Yin W, Hao Y, Sun X, Gong X, Li F, Li J, Rou K, Sullivan SG, Wang C, Cao X, Luo W, Wu Z. Scaling up the national methadone maintenance treatment program in China: achievements and challenges. Int J Epidemiol. 2010;39:ii29–ii37. doi: 10.1093/ije/dyq210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Chow EP, Zhuang X, Liang Y, Wang Y, Tang C, Ling L, Tucker JD, Wilson DP. Methadone maintenance treatment participant retention and behavioural effectiveness in China: a systematic review and meta-analysis. PLoS One. 2013;8:e68906. doi: 10.1371/journal.pone.0068906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Friedmann PD, Gerstein DR. Does retention matter? Treatment duration and improvement in drug use. Addiction. 2003;98:673–684. doi: 10.1046/j.1360-0443.2003.00354.x. [DOI] [PubMed] [Google Scholar]
- Zhou W, Wang X, Zhou S, Xie N, Liu P, Luo L, Peng J, Liu M, Desrosiers A, Schottenfeld R, Chawarski MC. Hepatitis C seroconversion in methadone maintenance treatment programs in Wuhan, China. Addiction. 2015;110:796–802. doi: 10.1111/add.12836. [DOI] [PMC free article] [PubMed] [Google Scholar]


