Abstract
Purpose
Assess national trends in utilization, demographics, hospital characteristics, and outcomes of patients undergoing surgical or percutaneous portal decompression since the introduction of the transjugular intrahepatic portosystemic shunt (TIPS).
Materials/Methods
Retrospective analysis of patients undergoing surgical portal decompression and TIPS using Medicare Physician Supplier Procedure Summary files from January 2003 through December 2013 and National/Nationwide Inpatient Sample data from 1993, 2003, and 2012. Utilization rates normalized to annual number of Medicare enrollees, estimated means, and 95% confidence intervals were calculated.
Results
Medicare total annual utilization rate for all portosystemic decompression procedures decreased 6.5% during the study period, from 15.3 in 2003 to 14.3 in 2013 per 1,000,000. TIPS utilization increased 19.4% (10.3 to 12.3 per 1,000,000) while open surgical shunt utilization decreased by 60.0% (5.0 to 2.0 per 1,000,000). TIPS represented 86% of all procedures in 2013. From 1993 to 2012, mean age increased slightly (53.0 to 55.5 years, p-value <0.05). The percentage of procedures performed at teaching hospitals increased, while in-hospital mortality and length of stay decreased by 42% (p<0.05) and 20% (p<0.05), respectively. Of factors evaluated, performance of procedures on an elective basis was the most influential on in-hospital mortality (p<0.01, all years studied) and length of stay (p<0.0001, all years studied).
Conclusions
Approximately two decades following the introduction of TIPS, utilization of all portal decompression procedures has remained relatively stable. TIPS represents the dominant portal decompression technique. In-hospital mortality and mean length of stay following decompression have decreased, partially due to performance of procedures during elective admissions.
Keywords: transjugular intrahepatic portosystemic shunt (TIPS), portal decompression, portal hypertension, utilization trends, interventional radiology
Introduction
In 1902, Gilbert (1) coined the term “portal hypertension” to describe structural changes in the portal circulation that could cause gastrointestinal bleeding. Portal decompression procedures can be life-saving for patients who have complications of portal hypertension, such as variceal bleeding or as cites that cannot be controlled with endoscopic or medical treatments. Vidal (2) used a portocaval shunt for the first time in a human in 1903; the patient lived for 4 months following the surgery (3). Nonselective shunts, such as portocaval or mesocaval shunts, decompress the entire portal system by diverting all portal blood flow but are generally associated with a higher risk of hepatic encephalopathy and liver failure (4). Selective shunts, such as the distal splenorenal shunt (DSRS), were first introduced by Warren in the 1960s (5). Selective shunts attempt to preserve some portal flow while decompressing varices (6). Overall, the various types of surgically created shunts provide >90% control of variceal bleeding and carry similar survival rates (5, 7–9).
The concept of a percutaneously inserted metallic shunt for portosystemic decompression was originally described by Rosch et al. in 1969 (10), but the first human case of transjugular intrahepatic portosystemic shunt (TIPS) creation was not reported until 1989 (11). The first large series of patients who underwent TIPS followed soon after, in 1993 (12). TIPS placement technique was further advanced in the early 2000s with the introduction of e-PTFE covered stent grafts, which have improved patency (13–15).
It is widely believed that TIPS is now the most commonly performed portal decompression procedure. This has been shown using data from a single state (16–17), but not at the national level. It is also not known what effects, if any, the introduction of a minimally invasive alternative to surgical decompression has had on the clinical and hospital setting where portal decompression surgery is performed, and on patient outcomes at a population level. The purpose of this study therefore was to 1) report on long-term national trends in the utilization of portal decompression procedures and 2) evaluate temporal trends in patient demographics, hospital characteristics, and outcomes of patients who underwent portal decompression since the advent of TIPS.
Methods
To assess long-term national utilization trends, Medicare provider claims from the Physician Supplier Procedure Summary (PSPS) Master Files from 2003 through 2013 were obtained from the Centers for Medicare and Medicaid Services. These files aggregate claims information for all patients with Medicare Supplemental Medical Insurance (Medicare Part B). PSPS claims data were extracted at 2-year intervals between 2003 and 2013 using Current Procedural Terminology codes for the following portal decompression procedures: open portocaval shunt, open renoportal shunt, open caval-mesenteric shunt, open splenorenal shunt – proximal, open splenorenal shunt – distal, and transvenous intrahepatic portosystemic shunt insertion. Utilization rates were normalized to annual number of Medicare Part B enrollees (18) and reported as number of procedures per 1,000,000 enrollees. To assess temporal trends in utilization, percent change over time were calculated for the normalized utilization numbers for each calendar year. This part of our study employs similar methodology to that described for other studies of national trends in procedural utilization (19–22).
To evaluate trends in patient demographics and outcomes and characteristics of hospitals where portal decompression procedures were performed, we obtained National/Nationwide Inpatient Sample (NIS) data from the Healthcare Cost and Utilization Project (HCUP) database from 1993, 2003, and 2012. NIS is the largest publicly available all-payer inpatient health care database in the United States. NIS contains data on patient demographics, clinical outcomes, hospital characteristics, and resource utilization for 20% of hospital stays in the United States, which equates to over 7 million hospitalizations a year. All patients who underwent portal decompression procedures were identified with the International Classification of Diseases, Ninth Revision, Clinical Modification code for intra-abdominal venous shunt (39.1). Sampling weights provided by HCUP were used to produce estimates of population means and 95% confidence intervals (CI) for the total number of patients in the United States who underwent portosystemic decompression, their demographic characteristics, characteristics of the hospitals where the procedures were performed, in-hospital mortality and mean length of stay. Indications for decompression were classified based on diagnosis codes into variceal bleeding, ascites, variceal bleeding and ascites, hydrothorax/effusion, Budd-Chiari, cirrhosis/chronic liver disease, and other. If multiple diagnoses were identified, the most specific was used. Population estimates were considered statistically different if 95% CIs did not overlap. Regression analyses were performed using methods to account for use of sample survey data; results were considered significant if p<0.05.
All data analyses were performed using commercially available software (SAS Version 9.3, SAS Institute, Cary, North Carolina and Excel 2010, Microsoft, Redmond, Washington). Institutional review board approval was not required because these public domain data do not involve individually identifiable health information.
Results
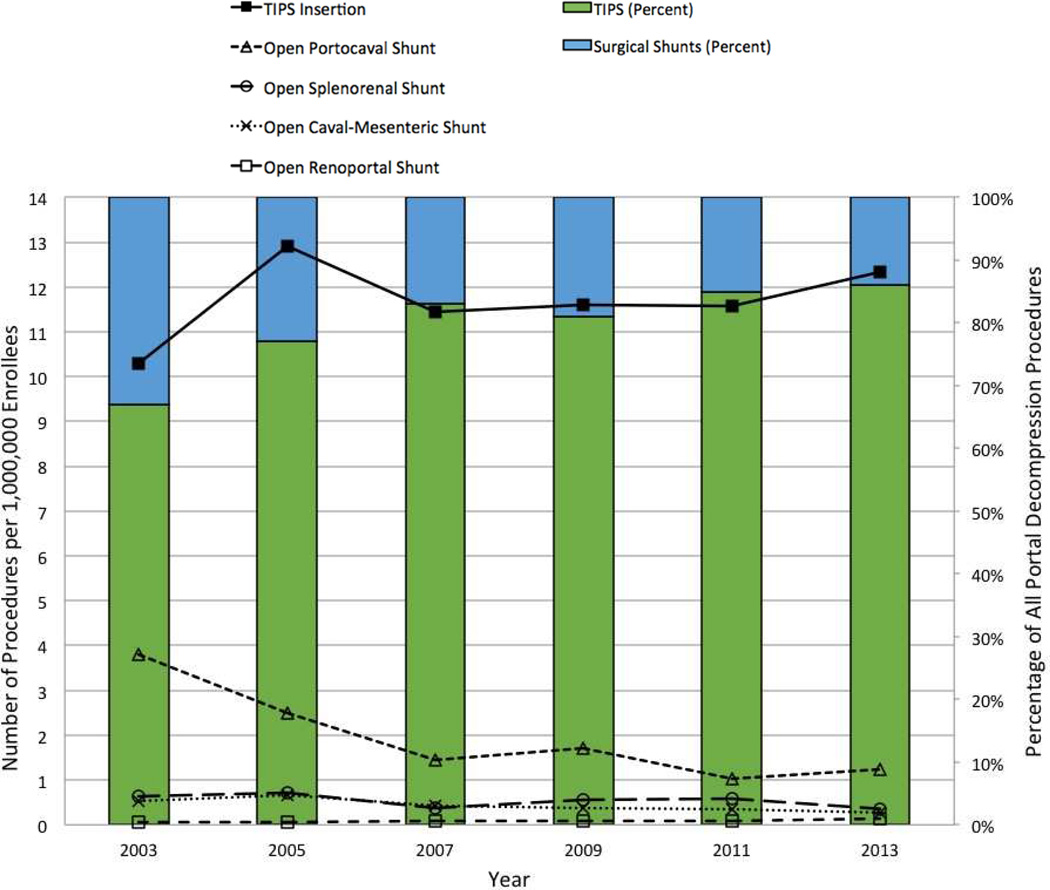
Between 2003 and 2013, the annual utilization rate for all portosystemic shunt procedures performed in the Medicare population decreased from 15.3 to 14.3 per 1,000,000 enrollees, a decrease of 6.5%. The utilization rate for TIPS procedures during this time increased 19.4% (from 10.3 to 12.3 per 1,000,000) while it decreased by 60.0% for all open surgical shunts (from 5.0 to 2.0 per 1,000,000). The most commonly performed open surgical shunt remains the portocaval shunt, followed by the splenorenal shunt. In 2003, TIPS insertion represented 67.3% of all portosystemic shunt procedures whereas in 2013 it represented 86.1% of all procedures (Figure 1).
Figure 1. Trends in portal decompression shunts from 2003 to 2013.
Line graphs correspond the number of procedures per 1,000,000 Medicare enrollees (left y-axis). TIPS and open surgical shunt bar graphs correspond to percentage of all portal decompression procedures (right y-axis).
In the wider population represented in the NIS dataset, patient demographics remained similar between 1993 and 2012, as summarized in Table 1. Overall, patients who received portosystemic shunts tended to be in their mid-50s, with a white, male predominance. Between 1993 and 2012, there was a slight increase in the mean patient age, from 53.0 (95% CI: 51.6–54.4) to 55.5 (95% CI: 54.6–56.3) years old. The other demographic characteristics did not change significantly in this time period. There was a trend toward increased proportion of portosystemic decompression procedures occurring during elective admissions, from 21% (95% CI: 16–26%) to 28% (95% CI: 24–31%) of overall admissions. Indications for portal decompression are listed in Table 2. The four most common indications were variceal bleeding, ascites, variceal bleeding and ascites, and cirrhosis/chronic liver disease.
Table 1.
Patient demographics and admission status by year
| 1993 | 2003 | 2012 | |
|---|---|---|---|
| Number of discharges | |||
| 4,624 | 5,780 | 5,880 | |
| Mean age, years (95% CI) | |||
| 53.0 (51.6 – 54.4) | 55.3 (54.2 – 56.3) | 55.5 (54.6 – 56.3) | |
| Gender, percentage (95% CI) | |||
| Male | 60 (57 – 63) | 66 (64 – 69) | 65 (62 – 68) |
| Female | 39 (30 – 48) | 34 (31 – 36) | 35 (32 – 38) |
| Race, percentage (95% CI) | |||
| White | 61 (52 – 70) | 59 (52 – 67) | 66 (63 – 70) |
| Non-white | 39 (30 – 48) | 41 (33 – 48) | 34 (30 – 37) |
| Admission type, percentage (95% CI) | |||
| Elective | 21 (16 – 26) | 28 (21 – 34) | 28 (24 – 31) |
| Non-Elective | 79 (74 – 84) | 72 (66 – 79) | 72 (69 – 76) |
Table 2.
Indications for portal decompression by year
| 1993 | 2003 | 2012 | |
|---|---|---|---|
| Number of admissions by indication (%) | |||
| Variceal bleeding | 471 (10.2) | 2,026 (35.2) | 2,140 (36.4) |
| Ascites | 64 (1.2) | 1,780 (30.8) | 1,330 (22.6) |
| Variceal bleeding and ascites | 77 (1.7) | 1,223 (21.0) | 1,800 (30.6) |
| Hydrothorax/effusion | 18 (0.5) | 97 (1.7) | 105 (1.8) |
| Budd-Chiari | 46 (0.9) | 15 (0.2) | 15 (0.3) |
| Cirrhosis/chronic liver disease | 3,418 (73.4) | 451 (7.9) | 305 (5.2) |
| Other | 530 (12.1) | 188 (3.2) | 185 (3.1) |
The majority of portosystemic decompression procedures occurred at large, academic hospitals in urban locations (Table 3). Between 1993 and 2012, the percentage of procedures performed at teaching hospitals increased from 60.7% (95% CI: 50.7–70.8%) to 78.7% (95% CI: 76.5–81.0%). The proportion of procedures performed at large hospitals (defined as the top one-third of hospitals in a given region and location/teaching combination by bed size) or urban hospitals (defined as located in a metropolitan statistical area) did not change significantly. Similarly, the proportion of procedures occurring at hospitals with larger decompression procedure volumes (defined as greater than 12 procedures per year) stayed relatively stable.
Table 3.
Hospital characteristics by year
| 1993 | 2003 | 2012 | |
|---|---|---|---|
| Hospital type, percentage (95% CI) | |||
| Large | 65.2 (54.3 – 76.0) | 78.1 (71.1 – 85.1) | 73.9 (70.7 – 77.1) |
| Urban | 98.9 (98.6 – 99.1) | 98.4 (97.4 – 99.5) | 98.6 (98.2 – 98.9) |
| Teaching | 60.7 (50.7 – 70.8) | 76.3 (70.4 – 82.3) | 78.7 (76.5 – 81.0) |
| High case volume (>12/year) | 46.7 (39.2 – 54.3) | 57.6 (50.7 – 64.5) | 55.3 (48.2 – 62.4)* |
Data from 2011 used due to change in NIS sampling design rendering 2012 hospital-level volume data not comparable to previous years.
In-hospital mortality decreased during our study period for overall and non-elective admissions while mean length of stay (LOS) decreased for overall admissions (Table 4). Inhospital mortality for all patients undergoing decompression procedures decreased by 42%, from 1993, where in-patient mortality rate was 18.4% (95% CI: 14.4–22.3%) to 2012, where it was 10.5% (95% CI: 8.9–12.3%). In-hospital mortality for non-elective admissions decreased from 21% (95% CI: 16–25%) to 13% (95% CI: 11–15%) over the time period. The mean LOS in 1993 was 13.4 days (95% CI: 12.0–14.7 days) compared with 2012, where it was 10.7 days (95% CI: 9.9–11.4 days), a decrease of 20.1%. As expected, mean LOS was shorter for elective admissions in all years studied, with mean LOS for non-elective admissions almost twice that for elective admissions in 2013 (12.3 days compared to 6.4 days).
Table 4.
In-hospital mortality and length of stay by year
| 1993 | 2003 | 2012 | |
|---|---|---|---|
| In-hospital mortality, percentage (95% CI) | |||
| Overall | 18.4 (14.4– 22.3) | 12.4 (10.5 – 14.5) | 10.6 (8.9 – 12.3) |
| Elective admission | 9.6 (4.9 – 14.2) | 4.9 (1.5 – 8.3) | 4.6 (2.5 – 6.8) |
| Non-elective admission | 20.7 (16.0 – 25.5) | 15.3 (12.9 – 17.7) | 12.9 (10.8 – 15.0) |
| Mean length of stay, days (95% CI) | |||
| Overall | 13.4 (12.0 – 14.7) | 11.3 (10.1 – 12.5) | 10.7 (9.9 – 11.4) |
| Elective admission | 9.0 (7.1 – 10.9) | 7.5 (5.0 – 9.9) | 6.4 (5.2 – 7.6) |
| Non-Elective admission | 14.5 (12.9 – 16.1) | 12.7 (11.5 – 14.0) | 12.3 (11.4 – 13.2) |
Exploratory analysis was performed to assess the factors associated with decreased in-hospital mortality and LOS over the course of the study period (Table 5). Multivariable regression modeling of all factors that had changed significantly over the course of the study period (patient mean age, teaching hospital status) and elective versus non-elective admission found that admission status was the only variable that was consistently associated with increased mortality (p<0.01, all years studied), with an odds of in-hospital mortality 2.5–3.6 times higher for non-elective compared to elective admissions. LOS was also associated with admission status across all years (p<0.0001, all years studied), with estimated mean LOS 5.3–6.2 days longer for non-elective admissions. Unexpectedly, older age was associated with shorter mean LOS, although the difference was minimal (0.6–1.2 days shorter per 10 years older age, p<0.05). Teaching hospital status was also associated with longer mean LOS in 2003 and 2012 (2.0–2.1 days longer, p<0.05).
Table 5.
Multiple regression models of survival to discharge and length of stay
| Variables | 1993 | 2003 | 2012 | |||
|---|---|---|---|---|---|---|
| Survival to discharge | Odds ratio | p-value | Odds ratio | p-value | Odds ratio | p-value |
| Age | 1.00 | 0.982 | 1.00 | 0.011 | 1.00 | 0.022 |
| Teaching hospital | 0.97 | 0.878 | 0.75 | 0.197 | 0.76 | 0.287 |
| Elective admission | −2.50 | 0.004 | −3.60 | <0.001 | −3.10 | <0.001 |
| Length of stay | Beta | p-value | Beta | p-value | Beta | p-value |
| Age | −0.06 | 0.012 | −0.08 | 0.023 | −0.12 | 0.003 |
| Teaching hospital | 0.65 | 0.614 | 1.96 | 0.016 | 2.09 | 0.002 |
| Elective admission | −5.60 | <0.0001 | −5.34 | <0.0001 | −6.15 | <0.0001 |
Discussion
Chronic liver disease and cirrhosis is the 12th most common cause of death in the United States, accounting for approximately 36,000 deaths per year, or 115 deaths per 1,000,000 population (23). Portal hypertension is a major complication seen in chronic liver disease and can result in bleeding esophageal varices, refractory ascites, hepatic hydrothorax, hepatorenal syndrome, and hepatopulmonary syndrome. Portal decompression procedures have proven benefits in secondary prevention of variceal bleeding and ascites that cannot be controlled via endoscopic or medical treatments (24–25). Portal decompression may also be used in the setting of hepatic hydrothorax and Budd-Chiari syndrome (26).
Over the past two decades, there have been many advances in the medical and procedural treatments of cirrhosis and portal hypertension. One of the largest changes with regard to portal decompression has been the development of TIPS as an alternative to surgical shunts. Results of multicenter prospective randomized trial published in 2006 (27) showed DSRS and TIPS to be similarly efficacious in the control of refractory variceal bleeding in Child–Pugh class A and B patients. Both resulted in similar short and long-term survival and similar costs (28) but reintervention rate was significantly greater for TIPS compared with DSRS. On the other hand, a more recent analysis in 2010 (29) of three prospective randomized trials and one retrospective case-controlled study concluded that surgical shunting had improved 2-year survival and less frequent shunt failure compared with TIPS.
Despite the lack of evidence showing superiority of TIPS over surgical shunts, TIPS has become much more common than surgical shunts. In the Medicare population, TIPS placements increased 51% between 2003 and 2013, while open surgical procedures decreased by about the same percentage. TIPS represented 86% of all portal decompression procedures performed in 2012. In a study including data between 2002–2005 from a single state, Rosemurgy et al. found a similar preference for TIPS, with TIPS performed 12 times more often than surgical shunts (17).
The exact reasons for the shift to TIPS cannot be derived from our data, but may include provider or patient preference for a minimally invasive procedure over open surgery. TIPS may be a more viable option in the non-elective or unstable patient. Additionally, TIPS may be a more viable intervention in patients with poor modified MELD of Childs-Pugh scores due to lower risk of complications and faster recovery (30). Physician volumes have been shown to be correlated with outcomes for portal decompression surgery but not with TIPS (16), and lack of expertise within the surgical community with performing these complex operations may also be a contributor to the observed long-term trends (31).
Although there is an overwhelming preference toward the use of TIPS, utilization rate per 1,000,000 Medicare patients for all decompression procedures has remained similar from 2003 to 2013. This is likely a result of the fact that the indications for portal decompression procedures (surgical or TIPS) have not changed, and that they remain reserved primarily for patients with portal hypertension that fail to respond to a combination of pharmacological/medical and endoscopic therapy (32).
From 1993 to 2012, patient gender, race and primary discharge diagnoses of those undergoing portal decompression were similar, while mean age increased slightly. The top indications for portal decompression were variceal bleeding and/or ascites in 2003 and 2012. There was a slight shift in distribution of where these procedures are being performed, with more being done at teaching/academic hospitals (60.7% in 1993 versus 78.7% in 2012). Additionally, the observed in-hospital mortality and mean LOS has significantly decreased, which is likely multifactorial. Of factors that we were able to elucidate from the NIS database, increasing completion of these procedures on an elective basis seems to be the most influential on decreasing mortality. Improvements in patient selection, surgical/procedural technique, and periprocedural management also likely contributed to these findings.
Our study has limitations. Medicare data used for the trend analysis portion of this study is predominately composed of claims for services to the elderly; therefore, the younger population may have different utilization rates. Additionally, PSPS files are composed of aggregate claims, which do not provide detailed patient specific factors such as demographics, comorbidities, and LOS. However, Medicare data have the advantage of representing complete claims data on about 25% of all physician services provided in the United States. Furthermore, the data collection method of PSPS files is uniform through multiple years. To complement the PSPS data, we also analyzed NIS data from the HCUP database, which is composed of hospital discharge data for individuals covered by Medicare, Medicaid, private insurance and the uninsured. This allowed us to evaluate a broader patient population and analyze primary diagnoses, hospital characteristics, LOS, and patient demographics such as sex, age, and race. However, our analysis is limited by apparent inconsistencies in coding practices over the time period studied. For example, analysis of indications for decompression from the 1993 showed that the vast majority of patients (73.4%) did not have a more specific diagnosis beyond cirrhosis/chronic liver disease; it is unlikely that such a large proportion of patients did not have a more specific indication (e.g. variceal bleeding) for portal decompression. Finally, as with all claims or discharge summary data, there is the possibility of miscoded or absent data, as accuracy of the database is dependent upon adequate documentation and coding performed as part of routine clinical and billing practice.
Conclusion
Approximately two decades following the introduction of TIPS, the overall utilization for all portal decompression procedures has remained stable, with increasing preference toward the use of TIPS over open surgical shunting. The in-hospital mortality and mean LOS following portal decompression have decreased, in part due to performance of procedures during elective admissions.
Acknowledgements
Funding/Support: SWK is supported by grant KL2 TR000421 from the National Institutes of Health, National Center for Advancing Translational Sciences. The funders/sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflicts of interest.
References
- 1.Gilbert A, Carnot P. Les fonctions hepatiques. Paris: 1902. [Google Scholar]
- 2.Vidal ME. Traitement chirurgical des as cites. Presse med. 1903;2(85):747. [Google Scholar]
- 3.Sandblom P. The history of portal hypertension. J R Soc Med. 1993;86(9):544–546. [PMC free article] [PubMed] [Google Scholar]
- 4.Millikan WJ, Warren WD, Henderson JM, et al. The Emory prospective randomized trial: selective versus nonselective shunt to control variceal bleeding. Ten year follow-up. Ann Surg. 1985 Jun;201(6):712–722. doi: 10.1097/00000658-198506000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warren WD, Zeppa R, Foman JJ. Selective transsplenic decompression of gastroesophageal varices by distal splenorenal shunt. Ann Surg. 1967;166(3):437–455. doi: 10.1097/00000658-196709000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright AS, Rikkers LF. Current management of portal hypertension. J Gastrointest Surg. 2005;9:992–1005. doi: 10.1016/j.gassur.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 7.Fischer JE, Bower RH, Atamian S, et al. Comparison of distal and proximal splenorenal shunts: a randomized prospective trial. Ann Surg. 1981;194:531–544. doi: 10.1097/00000658-198110000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langer B, Taylor BR, Mackenzie DR, et al. Further report of a prospective randomized trial comparing distal splenorenal shunt with end-to-side portacaval shunt. Gastroenterology. 1985;88:424–429. doi: 10.1016/0016-5085(85)90502-5. [DOI] [PubMed] [Google Scholar]
- 9.Harley HA, Morgan T, Redeker AG, et al. Results of a randomized trial of end-to-side portacaval shunt and distal splenorenal shunt in alcoholic liver disease and variceal bleeding. Gastroenterology. 1986;91:802–809. doi: 10.1016/0016-5085(86)90679-7. [DOI] [PubMed] [Google Scholar]
- 10.Rosch J, Hanafee W, Snow H. Transjugular portal venography and radiologic portacaval shunt: an experimental study. Radiology. 1969;92:1112–1114. doi: 10.1148/92.5.1112. [DOI] [PubMed] [Google Scholar]
- 11.Richter GM, Palmaz JC, Noldge G, et al. The transjugular intrahepatic portosystemic stentshunt (TIPSS): a new nonoperative percutaneous procedure. Radiologie. 1989;29:406–411. [PubMed] [Google Scholar]
- 12.LaBerge JM, Ring EJ, Gordon RL, et al. Creation of transjugular intrahepatic portosystemic shunts with the wallstent endoprosthesis: results in 100 patients. Radiology. 1993;187(2):413–420. doi: 10.1148/radiology.187.2.8475283. [DOI] [PubMed] [Google Scholar]
- 13.Barrio J, Ripoll C, Bañares R, et al. Comparison of transjugular intrahepatic portosystemic shunt dysfunction in PTFE-covered stent-grafts vs. bare stents. Eur J Radiol. 2005;55:120–124. doi: 10.1016/j.ejrad.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Tripathi D, Ferguson J, Barkell H, et al. Improved clinical outcome with transjugular intrahepatic portosystemic stent-shunt utilizing polytetrafluoroethylene-covered stents. Eur J Gastroenterol Hepatol. 2006;18:225–232. doi: 10.1097/00042737-200603000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Perarnau JM, Gouge AL, Nicolas C, et al. Covered vs uncovered stents for transjugular intrahepatic portosystemic shunt: a randomized controlled trial. J Hepatol. 2014;60:962–968. doi: 10.1016/j.jhep.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 16.Zervos EE, Osborne D, Angle SC, et al. Impact of hospital and surgeon volumes in the management of complicated portal hypertension: review of a statewide database in Florida. Am Surg. 2010;76(3):263–269. [PubMed] [Google Scholar]
- 17.Rosemurgy AS, Molloy DL, Thometz DP, et al. TIPS in Florida: is its application a result of evidence-based medicine? J Am Coll Surg. 2007;204(5):794–801. doi: 10.1016/j.jamcollsurg.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Medicare and Medicaid Services. 2014 annual report of the boards of trustees of the federal hospital insurance and federal supplementary medical insurance trust funds. [(accessed February 17, 2015)]; http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/Downloads/TR2014.pdf.
- 19.Levin DC, Rao VM, Parker L, et al. The changing roles of radiologists, cardiologists, and vascular surgeons in percutaneous peripheral arterial interventions during a recent five-year interval. J Am Coll Radiol. 2005;2:39–42. doi: 10.1016/j.jacr.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 20.Duszak R, Parker L, Levin DC, et al. Evolving roles of radiologists, nephrologists and surgeons in endovascular hemodialysis access maintenance procedures. J Am Coll Radiol. 2010;7:937–942. doi: 10.1016/j.jacr.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 21.Kwan SW, Bhargavan M, Kerlan RK, et al. Effect of advanced imaging technology on how biopsies are done and who does them. Radiology. 2010;256(3):751–758. doi: 10.1148/radiol.10092130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duszak R, Behrman SW. National trends in percutaneous cholecystostomy between 1994 and 2009: perspectives from medicare provider claims. J Am Coll Radiol. 2012;9:474–479. doi: 10.1016/j.jacr.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Deaths: final data for 2013, tables 10, 11. [(accessed February 17, 2015)]; http://www.cdc.gov/nchs/fastats/liver-disease.htm.
- 24.Boyer TD, Haskal ZJ. AASLD practice guidelines: the role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension. Hepatology. 2010;51(1):1–16. doi: 10.1002/hep.23383. [DOI] [PubMed] [Google Scholar]
- 25.Bari K, Garcia-Tsao G. Treatment of portal hypertension. World J Gastroenterol. 2012;18(11):1166–1175. doi: 10.3748/wjg.v18.i11.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Siramolpiwat S. Transjugular intrahepatic portosystemic shunts and portal hypertension-related complications. World J Gastroenterol. 2014;20(45):16996–17010. doi: 10.3748/wjg.v20.i45.16996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henderson JM, Boyer TD, Kutner M, et al. Distal splenorenal shunt versus transjugular intrahepatic portal systemic shunt for variceal bleeding: A randomized trial. Gastroenterology. 2006;130:1643–1651. doi: 10.1053/j.gastro.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 28.Boyer TD, Henderson MJ, Heery AM, et al. Cost of preventing variceal rebleeding with transjugular intrahepatic portal systemic shunt and distal splenorenal shunt. J Hepatol. 2008;48:407–414. doi: 10.1016/j.jhep.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark W, Hernandez J, McKeon B, et al. Surgical shunting versus transjugular intrahepatic portosystemic shunting for bleeding varices resulting from portal hypertension and cirrhosis: a meta-analysis. Am Surg. 2010;76(8):857–864. [PubMed] [Google Scholar]
- 30.Salerno F, Merli M, Cazzaniga M, et al. MELD score is better than Child-Pugh score in predicting 3-month survival of patients undergoing transjugular intrahepatic portosystemic shunt. J Hepatol. 2002;36:494–500. doi: 10.1016/s0168-8278(01)00309-9. [DOI] [PubMed] [Google Scholar]
- 31.Sachs TE, Ejaz A, Weiss M, et al. Assessing the experience in complex hepatopancreatobiliary surgery among graduating chief residents: Is the operative experience enough? Surgery. 2014;156(2):385–393. doi: 10.1016/j.surg.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCormick PA, Dick R, Panagou EB, et al. Emergency transjugular intrahepatic portosystemic stent shunting as a salvage treatment for uncontrolled variceal hemorrhage. Br J Surg. 1994;81:1324–1327. doi: 10.1002/bjs.1800810922. [DOI] [PubMed] [Google Scholar]