Abstract
Background
Although empirical evidence for the effectiveness of technology-mediated interventions for substance use disorders is rapidly growing, the role of baseline characteristics of patients in predicting treatment outcomes of a technology-based therapy is largely unknown.
Method
Participants were randomly assigned to either standard methadone maintenance treatment or reduced standard treatment combined with the computer-based Therapeutic Education System (TES). An array of demographic and behavioral characteristics of participants (N=160) were measured at baseline. Opioid abstinence and treatment retention were measured weekly for a 52-week intervention period. Generalized linear model and Cox-regression were used to estimate the predictive roles of baseline characteristics in predicting treatment outcomes.
Results
We found significant predictors of opioid abstinence and treatment retention within and across conditions. Among 21 baseline characteristics of participants, employment status, anxiety, and ambivalent attitudes toward substance use predicted better opioid abstinence in the reduced-standard-plus-TES condition compared to standard treatment. Participants who had used cocaine/crack in the past 30 days at baseline showed lower dropout rates in standard treatment, whereas those who had not used exhibited lower dropout rates in the reduced-standard-plus-TES condition.
Conclusions
This study is the first randomized controlled trial, evaluating over a 12-month period, how various aspects of participant characteristics impact outcomes for treatments that do or do not include technology-based therapy. Compared to standard alone treatment, including TES as part of the care was preferable for patients who were employed, highly anxious, and ambivalent about substance use and did not produce worse outcomes for any subgroups of participants.
Keywords: behavioral therapy, participant characteristics, technology-delivered intervention, opioid dependence, randomized controlled trial
1. INTRODUCTION
Media technologies, such as the internet and mobile devices, have shown considerable promise in the delivery of behavioral therapies targeting problematic substance use (Chen et al., 2012; White et al., 2010). Recent systematic reviews and meta-analyses indicate that technology-mediated interventions are effective in the prevention, treatment, and recovery support of substance use disorders (SUDs; Marsch and Dallery, 2012; Moore et al., 2011; Riper et al., 2011). Benefits of technology-mediated health interventions include their ability to expand the reach and effectiveness of care and to enable higher fidelity in the delivery of evidence-based interventions (Bickel et al., 2008; Gustafson et al., 2011; Marsch and Dallery, 2012). Numerous randomized, controlled trials, such as the computer-based Cognitive Behavioral Therapy program (Kiluk et al., 2010) and a web-based Motivational Interviewing and a Motivational Enhancement System (Ondersma et al., 2005, 2007) have provided growing empirical support for the efficacy and effectiveness of technology-mediated interventions for SUDs, including enhanced coping skill acquisition, risk recognition, and substance use reduction.
One of the most extensively studied technology-based interventions for SUDs is the Therapeutic Education System (TES), a fluency building behavioral intervention grounded in the Community Reinforcement Approach (CRA) that has been shown to be efficacious in treating SUDs (Bickel et al., 2008; Marsch et al., 2014). The 65 interactive modules in the TES address problem solving, self-regulation and coping skills in order to assist individuals in implementing positive behavioral changes (Marsch et al., 2011; Marsch et al., 2014).
In one recently published study conducted with opioid-dependent adults in methadone maintenance treatment, the authors found that replacing half of the standard counseling with the computer-based TES programs (referred to as reduced-standard-plus-TES hereafter) produced significantly greater rates of opioid abstinence over a one year follow-up period compared to standard alone treatment (Marsch et al., 2014). Despite the promising results, it is unknown whether including a computer-based TES as part of the care delivery model is still effective for various subgroups of opioid-dependent persons with different baseline characteristics. Opioid-dependent individuals with some characteristics may benefit from a computer-based therapy (Acosta et al., 2012; Cooney et al., 1991; Roman and Johnson, 2002), whereas persons with other characteristics (e.g., greater age, low education) may be served better with standard treatment. Systematic reviews affirm that baseline characteristics can moderate abstinence and study attrition outcomes in SUD treatment (Moore et al., 2011; Najt et al., 2011; White et al., 2010). To our knowledge, only two studies have examined the predictive validity of baseline characteristics, such as cognitive functioning, in the context of technology-based interventions for SUDs (Acosta et al., 2012; Carroll et al., 2011).
Building upon the main outcomes among opioid-dependent participants who were randomized to computer-based TES as part of their care versus those who only received standard treatment (Marsch et al., 2014), we further examine how differently an array of demographic and behavioral characteristics of participants measured at baseline predict treatment outcomes. The characteristics examined in this paper are consistent with those that have been examined in substance abuse treatment research, allowing us to interpret our findings in relation to the broader context of the literature (Ciraulo et al., 2003; Marsch et al., 2005; Weekes et al., 2011).
2. METHODS
2.1. Treatment random assignment
Eligible participants (N = 160, ≥18 years of age) recruited from a large methadone maintenance treatment (MMT) program, were randomly assigned to either (a) standard treatment or (b) reduced-standard-plus-TES condition in an intent-to-treat design. Demographics of the participants, eligibility criteria, general study procedures, and the CONSORT diagram are reported in Marsch et al. (2014).
Participants in the standard treatment condition received substance abuse counseling once a week for the first four weeks, and then every other week over the 52-week intervention period. The content of these sessions was largely similar to many other MMT programs, including discussion of current problems and treatment progress. Participants in the reduced-standard-plus-TES condition received the same standard counseling content offered by counselors to participants in the standard treatment condition during the first half of each scheduled counseling session, and spent the other half of their session using the computer-based TES program.
2.2. Urine drug testing
Participants were asked to provide urine samples to a research staff member at the study site on a weekly basis. Point-of-care qualitative urine test cups (Drug Test Systems, Dover, NH) were used to test for the presence of barbiturates, THC, cocaine, benzodiazepines, methamphetamine, opiates, methadone, oxycodone, and propoxyphene. Opioid abstinence was confirmed when all the urinalysis results for opiates, propoxyphene, and oxycodone were negative (Marsch et al., 2014).
2.3. Measures of baseline characteristics
Categorical baseline characteristics measured with multi-level responses, such as marital status, were dichotomized prior to the predictor analyses (Quinn and Keough, 2002). The Addiction Severity Index (McLellan et al., 1980) was used to measure substance use in the past 30 days, including sedatives, cocaine/crack, and alcohol intoxication. No use was coded as “0” and any use was coded as “1”. Summated scores for the Beck Depression Inventory-II (BDI-II; Beck et al., 1996) and the Beck Anxiety Inventory (BAI; Beck and Steer, 1990) were calculated to assess participants’ level of depression and severity of anxiety symptoms at baseline. The HIV/AIDS Knowledge Test (Marsch and Bickel, 2001) was modified into 25 items to measure HIV/hepatitis knowledge and sexual/drug risk behaviors (0= no correct answers, 25 = a perfect score). Lastly, participants responded to the Stage of Change Readiness and Treatment Engagement Scale (SOCRATES 8A; Miller and Tonigan, 1996). The summated scores were transferred into decile scores for the Recognition, Ambivalence, and Taking Steps sub-scales, ranging from 10 to 90.
2.4. Statistical analyses
Generalized linear models (GLM) with logit link and binomial distribution were conducted to estimate the effect of the predictors on proportion-based binary responses for opioid abstinence (i.e., opioid-positive or –negative; Quinn and Keough, 2002). After examining the predictor effects within each study condition, the study condition was entered into the model with each predictor to explore an interaction effect between a given predictor and the study conditions. Cox proportional hazards regressions analyses were conducted to determine the unique contribution of each predictor on treatment retention within and across study conditions (Cox and Oakes, 1984).
3. RESULTS
3.1. Predictors of opioid abstinence and retention within each study condition
For participants in the reduced-standard-plus-TES condition, eight variables (e.g., being Hispanic) predicted a higher percentage of weeks abstinent (Table 1). Five variables (e.g., more years of education) predicted a lower percentage of total weeks abstinent.
Table 1.
Within-Group Generalized Linear Model Analyses and Interaction Tests
| Percentage of total study weeks with opioid abstinence | Dropout during total study weeks | ||||
|---|---|---|---|---|---|
| Predictor Variables | TES B | Standard B | TES HR | Standard HR | |
| 1 | Age | 0.00a(0.00) | −0.01b(0.00) | 0.97a | 0.98a |
| 2 | Gender (male) | −0.15a(0.09) | −0.51b(0.09) | 1.18a | 1.25a |
| 3 | Ethnicity (Hispanic) | 0.57a(0.09) | 0.15b(0.09) | 1.50a | 1.01a |
| 4 | Race (White) | 0.59a(0.08) | −0.04b(0.08) | 1.17a | 1.40a |
| 5 | Marital status (married) | −0.10a(0.13) | −0.80b(0.16) | 0.87a | 0.53a |
| 6 | Years education | −0.08a(0.02) | −0.03a(0.02) | 0.89a | 1.07a |
| 7 | Employment status (employed) | −0.16a(0.08) | −0.48b(0.08) | 1.22a | 1.08a |
| 8 | HIV+ (positive) | −0.23a(0.12) | −0.45b(0.20) | 1.33a | 2.39a |
| 9 | HCV+ (positive) | 0.58a(0.08) | 0.02b(0.09) | 1.00a | 1.25a |
| 10 | Past 30 days sedative use | 0.41a(0.08) | −0.09b(0.09) | 1.26a | 1.01a |
| 11 | Past 30 days cocaine/crack use | −0.43a(0.08) | −0.24a(0.08) | 1.76a | 0.68b |
| 12 | Past 30 days alcohol use to intoxication | 0.55a(0.09) | −0.17b(0.11) | 0.83a | 1.48a |
| 13 | Currently on probation or parole | 0.24a(0.11) | −0.04a(0.16) | 0.93a | 1.41a |
| 14 | Past 30 days sexual behavior | −0.29a(0.08) | −0.05b(0.08) | 1.56a | 1.27a |
| 15 | Past 30 days injection drug use | −0.28a(0.09) | −0.07a(0.08) | 1.88a | 1.98a |
| 16 | Beck Depression Inventory | 0.00a(0.00) | 0.00a(0.00) | 1.01a | 1.02a |
| 17 | Beck Anxiety Inventory | 0.03a(0.00) | −0.03b(0.00) | 1.00a | 1.01a |
| 18 | HIV and Hepatitis Knowledge | 0.00a(0.02) | −0.02a(0.02) | 1.01a | 1.04a |
| 19 | Recognition | 0.00a(0.00) | 0.00a(0.00) | 1.01a | 1.00a |
| 20 | Ambivalence | 0.00a(0.00) | −0.02b(0.00) | 1.00a | 0.99a |
| 21 | Taking Steps | 0.00a(0.00) | 0.01b(0.00) | 1.00a | 1.00a |
Note: Gender Female=0, Male =1; Ethnicity Not Hispanic = 0, Hispanic =1; Race Non-White=0, White = 1; Marital Status Non-married =0, Married = 1; Employment Unemployed = 0, Employed = 1; HIV+ HIV negative = 0, HIV positive = 1; Past 30 days sedative use No = 0, Yes = 1; Past 30 days cocaine/crack use No = 0, Yes = 1; Past 30 days alcohol use to intoxication No = 0, Yes = 1; Probation or parole No=0, Yes =1; Last week sexual behavior No=0, Yes=1; Last week injection drug use No=0, Yes=1
Values in bold indicate p < .05, and values in bold and underlined indicate p < .01. The first section presents results from generalized linear modeling analyses that examined each predictor's unique contribution to the percentage of total study weeks with opioid abstinence within each study condition. Higher positive coefficients indicate a greater contribution to the percentage of study weeks with opioid abstinence. The numbers in parentheses are standard errors of unstandardized regression coefficients, B. Labels in the parentheses refer to categories with a value of "1" for dichotomized variables. Superscripts a and b denoted across conditions indicate significant interaction effects of the predictor. The second section represents hazard ratios from Cox-regression analyses.
For participants in the standard treatment condition, only SOCRATES Taking Steps sub-scale scores predicted higher percentages of total weeks with opioid abstinence. Eight predictors (e.g., older age, being male, married and employed) revealed negative associations with percentage of total weeks with opioid abstinence.
Cox proportional hazards regression indicated that dropout rates decreased as one unit increased in the age of participants in the reduced-standard-plus-TES group (HR = .97, p < .05), but dropout rates increased when participants in both conditions were involved in risky drug injection behaviors in the past 30 days at baseline (HR = 1.88 for participants in the reduced-standard-plus-TES condition; HR = 1.98 for participants in the standard condition, p < .05).
3.2. Interaction effects: Predictors of opioid abstinence and retention across conditions
Three predictors (employment status, BAI score and Ambivalence score) showed significant interaction effects across study conditions on the outcome of opioid abstinence (Table 1). Being employed predicted significantly worse outcomes in the standard condition relative to the reduced-standard-plus-TES condition (B = 0.30, p < 0.01, d = .11). Higher BAI scores predicted better opioid abstinence for the reduced-standard-plus-TES condition participants by 0.06 (p < 0.01, d = .57) compared to those in the standard condition. Higher Ambivalence scores predicted better opioid abstinence for the reduced-standard-plus-TES condition participants by 0.02 (p < 0.01, d = .40) compared to those in the standard condition.
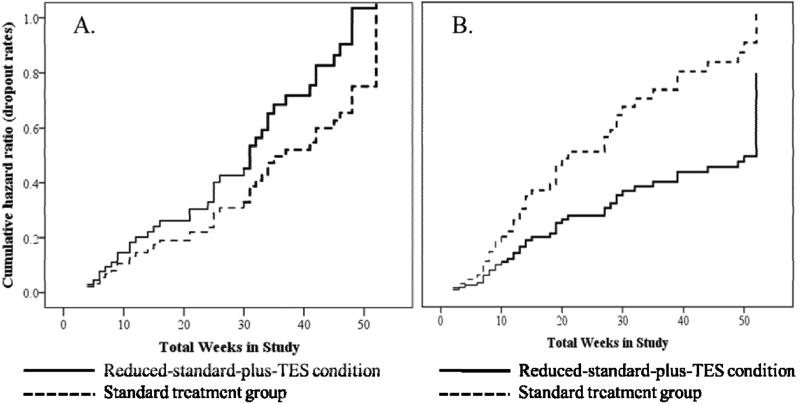
Different dropout rates and patterns were observed in the hazard ratios across study arms as related to past 30 days cocaine/crack use at baseline. Participants who had used cocaine/crack in the past 30 days at baseline (n = 76) were more likely to drop out, especially approximately 30 weeks after the intervention started, when they were assigned to the reduced-standard-plus-TES condition compared to the standard treatment condition (Fig. 1A). For participants who had not used cocaine/crack in the past 30 days at baseline (n = 84), lower dropout rates emerged at approximately 10 weeks after the intervention started when they were assigned to the reduced-standard-plus-TES condition (Fig. 1B).
Figure 1.
Cocaine/crack use at baseline and dropout rate changes across study conditions over the 52 study weeks. (A) The hazard ratio for participants with cocaine/crack use in the past 30 days at baseline. (B) The hazard ratio for participants with no cocaine/crack use in the past 30 days at baseline.
4. DISCUSSION
The current study examined a wide array of patient characteristics at baseline and their moderating impact on treatment outcomes when the computer-based TES intervention was or was not offered as part of the treatment model. The predictor analyses allowed us to identify a set of specific baseline characteristics of the participants that demonstrated different treatment outcomes across study arms. The-reduced-standard-plus-TES condition resulted in relatively better treatment outcomes compared to the standard alone treatment for subgroups of participants with four baseline characteristics: employment status, high anxiety scores, high ambivalence scores for opioid abstinence; and past 30 days cocaine/crack use for study retention.
Although speculative, the self-directed and self-paced aspect of TES, or fluency-building programing employed in the TES system worked well for the patients with high anxiety scores at baseline. For greater ambivalent attitudes, perhaps individuals who were ambivalent about continuing substance use had positive experiences with the TES by receiving immediate feedback and scores reflecting mastery of relevant coping skills and knowledge, and these learning experiences motivated them to reduce their problematic opioid use. The reported retention result suggests that it may be clinically important to incorporate a targeted intervention for cocaine and crack use as part of treatment for opioid dependence.
Our statistical analyses are also clinically significant. For example, a one unit increase in the ambivalence scores resulted in a 2% increase in the abstinence rate for those in the reduced standard-plus-TES group. The ambivalence scores ranged from 10 to 90. With this wide range in the ambivalence scores, if someone has a baseline ambivalent score of 60, s/he is likely to have 60% better abstinence rates when assigned to the reduced-standard-plus-TES group compared to those who have a baseline ambivalent score of 30.
Our analyses were designed to address empirical questions, whether patients with certain characteristics will do better or worse when the technology-based therapy was offered as part of the care. Some may speculate whether a technology-based intervention can be effective and feasible for subgroups of participants that are presumed to be difficult to treat. We found that TES was not contraindicated for any subgroup examined. That is, those 18 non-significant moderating characteristics reported here (e.g., age, ethnicity, past risky behaviors) imply that these characteristics should not be considered as technology-specific barriers (Choo et al., 2012) in receiving the computer-based TES as part of the care.
Although not assessed here, poor computer literacy could be a barrier for achieving a positive treatment outcome from a technology-based therapy. Examining computer literacy or eHealth literacy (Norman and Skinner, 2006) and its relation to outcomes could have been meaningful. In this trial, however, TES was intentionally designed to be useful by a broad array of users and did not assume any prior computer experience. Future work on technology-based SUD interventions should ensure the lack of computer literacy at baseline does not work against patients as a built-in barrier or discriminatory factor.
In summary, the results of the present study identify subgroups of substance users that can benefit from technology-assisted SUD interventions. A clinician may conclude that offering TES as part of the service delivery model can: 1) work better than standard alone treatment especially for patients who are employed, highly anxious, or ambivalent about continuation of substance use; and 2) is also effective for persons presenting for addiction treatment with those 18 non-significant moderator characteristics, as we found that including TES as part of the care was not contraindicated for these subgroups.
Highlights.
The study examined a technology-based behavioral intervention for SUDs.
Baseline characteristics of participants were examined as moderating factors.
Treatment outcomes include opioid abstinence and treatment retention.
Interaction effects between study arms and treatment outcomes emerged.
Specific sub-groups particularly benefited from the technology-based Therapeutic Education System.
Acknowledgments
Role of Funding Source. The research study reported in this manuscript was supported by NIH/NIDA R01 DA021818. The preparation of this manuscript was partially supported by NIH/NIDA P30DA029926.
Funders did not have any influence on study design, data collection, analysis or report of the data, writing the manuscript, the decision to submit the paper for publication or any constraints on publishing the results.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors. All authors agree that persons listed as authors fully qualify for authorship. SJK and LAM conceptualized and designed the study. And, LAM served as Principal Investigator on the clinical trial. HG and MA participated in providing feedback on the conceptualization and also helped manage the clinical trial. YA-M collected data. SJK analyzed the data, and wrote the first and final drafts. SJK, LAM, HG, and MA contributed to the writing and review of the paper.
Conflict of Interest. All authors declare that they have no conflicts of interest. In addition to her academic affiliation, Dr. Marsch is affiliated with HealthSim, LLC, the health-promotion software development organization that developed the web-based Therapeutic Education System referenced in this manuscript. Dr. Marsch has worked extensively with her institutions to manage any potential conflict of interest. All research data collection, data management, and statistical analyses were conducted by individuals with no affiliation to HealthSim, LLC.
Contributor Information
Sunny J. Kim, Center for Technology and Behavioral Health, Dartmouth Psychiatric Research Center, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Dartmouth College, 85 Mechanic Street, Suite B4-1, Lebanon, NH 03766, USA.
Lisa A. Marsch, Center for Technology and Behavioral Health, Dartmouth Psychiatric Research Center, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Dartmouth College, 85 Mechanic Street, Suite B4-1, Lebanon, NH 03766, USA, Lisa.A.Marsch@Dartmouth.Edu, http://www.c4tbh.org
Honoria Guarino, National Development and Research Institutes, Inc., 71 W. 23rd St., New York, NY 10010, USA, guarino@ndri.org.
Michelle Acosta, National Development and Research Institutes, Inc., 71 West 23rd Street, 4th floor, New York, NY 10010, USA, acosta@ndri.org.
Yesenia Aponte-Melendez, National Development and Research Institutes, Inc., 71 West 23rd Street, 4th floor, New York, NY, 10010a, USA, aponte-melendez@ndri.org.
REFERENCES
- Acosta MC, Marsch LA, Xie H, Guarino H, Aponte-Melendez Y. A web-based behavior therapy program influences the association between cognitive functioning and retention and abstinence in clients receiving methadone maintenance treatment. J. Dual Diagn. 2012;8:283–293. doi: 10.1080/15504263.2012.723317. doi: 10.1080/15504263.2012.723317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory II (BDI-II) Psychology Corporation; San Antonio: 1996. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. Psychological Corporation; San Antonio: 1990. [Google Scholar]
- Bickel WK, Marsch LA, Buchhalter AR, Badger GJ. Computerized behavior therapy for opioid-dependent outpatients: a randomized controlled trial. Exp. Clin. Psychopharmacol. 2008;16:132–143. doi: 10.1037/1064-1297.16.2.132. doi: 10.1037/1064-1297.16.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD, Nich C, Babuscio TA, Brewer JA, Potenza MN, Ball SA, Martino S, Rounsaville BJ, Lejuez CW. Cognitive function and treatment response in a randomized clinical trial of computer-based training in cognitive-behavioral therapy. Subst. Use Misuse. 2011;46:23–34. doi: 10.3109/10826084.2011.521069. doi: 10.3109/10826084.2011.521069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YF, Madan J, Welton N, Yahaya I, Aveyard P, Bauld L, Wang D, Fry-Smith A, Munafo MR. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol. Assess. 2012;16:1–205. doi: 10.3310/hta16380. doi: 10.3310/hta16380. [DOI] [PubMed] [Google Scholar]
- Choo EK, Ranney ML, Wong Z, Mello MJ. Attitudes toward technology-based health information among adult emergency department patients with drug or alcohol misuse. J. Subst. Abuse Treat. 2012;43:397–401. doi: 10.1016/j.jsat.2012.09.005. doi: 10.1016/j.jsat.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciraulo DA, Piechniczek-Buczek J, Iscan EN. Outcome predictors in substance use disorders. Psychiatr. Clin. North Am. 2003;26:381–409. doi: 10.1016/s0193-953x(02)00106-5. doi: 10.1016/s0193-953x(02)00106-5. [DOI] [PubMed] [Google Scholar]
- Cooney NL, Kadden RM, Litt MD, Getter H. Matching alcoholics to coping skills or interactional therapies: two-year follow-up results. J. Consult. Clin Psychol. 1991;59:598–601. doi: 10.1037//0022-006x.59.4.598. [DOI] [PubMed] [Google Scholar]
- Cox DR, Oakes D. Analysis of Survival Data. Chapman and Hall; London: 1984. [Google Scholar]
- Gustafson DH, Boyle MG, Shaw BR, Isham A, McTavish F, Richards S, Schubert C, Levy M, Johnson K. An e-health solution for people with alcohol problems. Alcohol Res. Health. 2011;33:327–337. [PMC free article] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Babuscio T, Carroll KM. Quality versus quantity: acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction. 2010;105:2120–2127. doi: 10.1111/j.1360-0443.2010.03076.x. doi: 10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA, Ann M, Stephens C, Mudric T, Strain EC, Bigelow GE, Johnson RE. Predictors of outcome in LAAM, buprenorphine, and methadone treatment for opioid dependence. Exp. Clin. Psychopharmacol. 2005;13:293–302. doi: 10.1037/1064-1297.13.4.293. doi: 10.1037/1064-1297.13.4.293. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK. Risk Behavior: Gender Differences During Buprenorphine Treatment.. Paper presented at the Symposium conducted at the 109th Annual Convention of the American Psychological Association; San Francisco, CA. 2001. [Google Scholar]
- Marsch LA, Dallery J. Advances in the psychosocial treatment of addiction: the role of technology in the delivery of evidence-based psychosocial treatment. Psychiatr. Clin. North Am. 2012;35:481–493. doi: 10.1016/j.psc.2012.03.009. doi: 10.1016/j.psc.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA, Grabinski MJ, Bickel WK, Desrosiers A, Guarino H, Muehlbach B, Solhkhah R, Taufique S, Acosta M. Computer-assisted HIV prevention for youth with substance use disorders. Subst. Use Misuse. 2011;46:46–56. doi: 10.3109/10826084.2011.521088. doi: 10.3109/10826084.2011.521088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA, Guarino H, Acosta M, Aponte-Melendez Y, Cleland C, Grabinski M, Brady R, Edwards J. Web-based behavioral treatment for substance use disorders as a partial replacement of standard methadone maintenance treatment. J. Subst. Abuse Treat. 2014;46:43–51. doi: 10.1016/j.jsat.2013.08.012. doi: 10.1016/j.jsat.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O'Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J. Nerv. Ment. Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers' motivation for change: the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychol. Addict. Behav. 1996;10:81–89. doi: 10.1037/0893-164X.10.2.81. [Google Scholar]
- Moore BA, Fazzino T, Garnet B, Cutter CJ, Barry DT. Computer-based interventions for drug use disorders: a systematic review. J. Subst. Abuse Treat. 2011;40:215–223. doi: 10.1016/j.jsat.2010.11.002. doi: 10.1016/j.jsat.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najt P, Fusar-Poli P, Brambilla P. Co-occurring mental and substance abuse disorders: a review on the potential predictors and clinical outcomes. Psychiatry Res. 2011;186:159–164. doi: 10.1016/j.psychres.2010.07.042. doi: 10.1016/j.psychres.2010.07.042. [DOI] [PubMed] [Google Scholar]
- Norman CD, Skinner HA. eHealth Literacy: essential skills for consumer health in a networked world. J. Med. Internet Res. 2006;8:e9. doi: 10.2196/jmir.8.2.e9. doi: 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Chase SK, Svikis DS, Schuster CR. Computer-based brief motivational intervention for perinatal drug use. J. Subst. Abuse Treat. 2005;28:305–312. doi: 10.1016/j.jsat.2005.02.004. doi: 10.1016/j.jsat.2005.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Svikis DS, Schuster CR. Computer-based brief intervention a randomized trial with postpartum women. Am. J. Prev. Med. 2007;32:231–238. doi: 10.1016/j.amepre.2006.11.003. doi: 10.1016/j.amepre.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn GP, Keough MJ. Experimental Design and Data Analysis for Biologists. Cambridge University Press; Cambridge: 2002. doi: 10.1017/CBO9780511806384. [Google Scholar]
- Riper H, Spek V, Boon B, Conijn B, Kramer J, Martin-Abello K, Smit F. Effectiveness of E-self-help interventions for curbing adult problem drinking: a meta-analysis. J. Med. Internet Res. 2011;13:e42. doi: 10.2196/jmir.1691. doi: 10.2196/jmir.1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman PM, Johnson JA. Adoption and implementation of new technologies in substance abuse treatment. J. Subst. Abuse Treat. 2002;22:211–218. doi: 10.1016/s0740-5472(02)00241-6. [DOI] [PubMed] [Google Scholar]
- Weekes JC, Cotton S, McGrady ME. Predictors of substance use among black urban adolescents with asthma: a longitudinal assessment. J. Natl. Med. Assoc. 2011;103:392–398. doi: 10.1016/s0027-9684(15)30335-7. [DOI] [PubMed] [Google Scholar]
- White A, Kavanagh D, Stallman H, Klein B, Kay-Lambkin F, Proudfoot J, Drennan J, Connor J, Baker A, Hines E, Young R. Online alcohol interventions: a systematic review. J. Med. Internet Res. 2010;12:e62. doi: 10.2196/jmir.1479. doi: 10.2196/jmir.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]