Abstract
Background
There are no population-based studies of emergency department (ED) utilization by individuals using prescription pain medications non-medically. We examined whether non-medical use of prescription pain medications was independently associated with increased ED utilization.
Methods
We conducted a retrospective analysis of a nationally representative sample of the non-institutionalized, civilian U.S. population in the National Survey on Drug Use and Health, 2008–2013. We used multivariable logistic regression to examine the association between past year ED utilization and non-medical use of prescription pain medications, defined as use of medications “not prescribed for you or that you took only for the experience or feeling they caused”.
Results
An estimated 10.5 million adults annually reported past year non-medical use (NMU) of prescription pain medications, and 39%, or 4.1 million adults annually, also reported one or more past year ED visits. After adjustment for sociodemographic and clinical characteristics, adults with past year NMU of prescription pain medications had increased odds of past year ED utilization (adjusted odds ratio 1.32; 95% confidence interval 1.24–1.41). In secondary analyses, individuals with more frequent NMU had increased odds of ED utilization in unadjusted analyses, but this association was attenuated with adjustment for the source of prescription pain medication (i.e., physician, friend/family, other source).
Conclusions
Non-medical use of prescription pain medications is associated with increased ED utilization. Further work is needed to identify the optimal role of ED settings in providing screening, education, and treatment referral for individuals using prescription pain medications non-medically.
Keywords: Opioid medications, Non-medical use, Emergency Department, Health services research
1. BACKGROUND
In the past decade, prescribing of opioid medications in the United States has quadrupled (Paulozzi et al., 2011). As the availability of opioid medications has increased so too have rates of opioid-related adverse health outcomes such as opioid overdose and opioid use disorders. Every day, 46 Americans die from an overdose related to prescription opioid medications (Frieden, 2014). In one study, a majority of prescription opioid-related overdose deaths involved the non-medical use of prescription opioids, defined as use without a prescription or use not as prescribed (Hall et al., 2008).
In an effort to describe morbidity associated with opioid medication use, several recent studies have examined Emergency Department (ED) visits related to the complications of opioid use (Cai et al., 2010). Hasegawa et al. (2014) reported that the rate of ED visits for opioid overdose (including heroin) quadrupled from 1993–2010. Yokell et al. (2014) estimated that prescription opioids accounted for nearly four times as many ED visits as heroin in 2010 nationally. More broadly, in 2011, there were an estimated 500,000 ED visits related to non-medical use of prescription pain medications and another 121,000 ED visits involving individuals seeking detoxification from prescription pain medications, an increase of 286% and 348% respectively compared to 2004 (2013b). These studies highlight the multiple pathways to opioid-related ED utilization. However, they have relied on visit-based data extracted from medical records and are limited in their ability to assess patient-reported data on behaviors related to non-medical use of prescription medications.
Therefore, the objectives of this work were to examine utilization of ED services among a nationally representative sample of adults and its association with past year non-medical use of prescription pain medications. We hypothesized that past year non-medical use of prescription pain medications would be independently associated with ED utilization and that this association would be strongest among adults with more frequent non-medical use.
2. METHODS
2.1. Data source
We analyzed data from the 2008 through 2013 National Survey of Drug Use and Health (NSDUH) public use files (2009; 2010; 2011; 2012; 2013a; 2014). The NSDUH is an annual cross-sectional survey that provides nationally representative estimates of substance use and other health-related behaviors among members of the non-institutionalized U.S. civilian population aged 12 years or older. The NSDUH sampling frame includes residents of households or non-institutional group quarters, persons without permanent residence (i.e., homeless people in shelters) and civilians living on military bases. The survey uses a 50-state design with an independent, multistage area probability sample for each state. The NSDUH contains sample weights for each respondent, which account for selection probability, adjust for nonresponse, and enable nationally representative estimates for all aspects of the survey. We restricted our analysis to adult respondents aged 18 years and older. The NSDUH has an annual sample size of approximately 70,000 respondents. The public use dataset includes data on approximately 55,000 respondents, of whom two-thirds are aged 18 years and older. We aggregated data across 6 survey years (2008–2013) to increase the sample size of this population, resulting in a final sample of 228,556 adult respondents.
The NSDUH uses a combination of computer-assisted personal interviewing conducted by a trained interviewer and audio computer-assisted self-interviewing (ACASI). ACASI provides respondents with a private and confidential means of responding to questions in order to maximize validity of reporting of sensitive behaviors such as substance use (Turner et al., 1998). Interviews are conducted in either English or Spanish and take approximately 1 hour to complete. Respondents receive $30 for completing the survey. From 2008 to 2013, the response rate was between 74% and 76%. The NSDUH imputes missing responses for the files made available for public use, and these imputed data were included in study analyses, when available. The NSDUH is sponsored by the Center for Behavioral Health Statistics and Quality within the Substance Abuse and Mental Health Services Administration (SAMHSA) and is conducted by RTI International, Research Triangle Park, North Carolina (2009; 2010; 2011; 2012; 2013a; 2014). Additional details are available online (http://www.samhsa.gov/data/population-data-nsduh).
NSDUH data are de-identified and publicly available. All survey respondents provide informed consent prior to participation. Conduct of the NSDUH was approved by the Research Triangle Institute’s Institutional Review Board. This analysis was reviewed by the Colorado Multiple Institutional Review Board and determined to be Non-Human Subjects Research.
2.2. Main measures
Our main outcome variable was self-reported past year ED utilization. We created a dichotomous past year ED utilization variable based on non-zero responses to a single survey question, “During the past 12 months… how many different times have you been treated in an emergency room for any reason?” Our primary explanatory variable was self-reported past year non-medical use (NMU) of prescription pain medications, defined as used of prescription pain medications that were “not prescribed for you or that you took only for the experience or feeling they caused.” We created a dichotomous variable to identify individuals reporting any past year non-medical use of prescription pain medications.
In secondary analyses, we categorized respondents’ self-reported frequency of past year NMU of prescription pain medications as 1–29 days, 30–99 days, 100–199 days or 200–365 days consistent with prior definitions of frequency of non-medical use (Jones, 2012; Jones et al., 2014). We hypothesized that more frequent NMU would increase exposure to the risks of opioid medications and therefore increase ED utilization related to opioid-related adverse events.
We also specified two additional patient-reported measures that were deemed potentially relevant to ED utilization among individuals using prescription pain medications non-medically, 1) source of prescription pain medications used non-medically, and 2) past year opioid withdrawal symptoms. First, we created three mutually exclusive categories to characterize respondents’ most recent source of prescription pain medications: 1) one or more physicians; 2) friends or family; or 3) all other sources (i.e., theft, purchase from drug dealer) (Becker et al., 2011; Wang et al., 2014). Second, we created a dichotomous variable to identify individuals reporting past year opioid withdrawal symptoms. Respondents were asked whether they had experienced at least 3 of 9 opioid withdrawal symptoms after cutting back or stopping prescription pain medications. These symptoms included feeling kind of blue or down; vomiting or feeling nauseous; having cramps or muscle aches; having teary eyes or a runny nose; feeling sweaty, having enlarged eye pupils, or having body hair standing up on your skin; having diarrhea; yawning; having a fever; or having trouble sleeping.
2.3. Study covariates
A priori, we identified sociodemographic and clinical characteristics which may confound the association of interest. Sociodemographic variables included gender, age, race/ethnicity, marital status, education, employment, insurance status, family income and rural residence. Clinical characteristics included self-reported health status, dichotomized as ‘excellent/very good/good health’ versus ‘fair/poor health.’ Serious psychological distress was defined as a score ≥13 on the K6 Psychological Distress Scale, a validated screening tool for serious mental illness (Kessler et al., 2003). Substance use characteristics included past year abuse or dependence of: 1) alcohol; 2) cannabis; and 3) other illicit drugs (including heroin, cocaine, hallucinogens and inhalants), based on diagnostic criteria for substance abuse and dependence as specified in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). We created a variable to identify self-reported past year non-medical use of prescription sedative, tranquilizer or stimulant medications. Past month nicotine dependence was based on meeting criteria from the Nicotine Dependence Syndrome Scale or a single question from the Fagerstr m Test of Nicotine Dependence (Heatherton et al., 1991, 1989; Shiffman et al., 2004).
2.4. Statistical analyses
We used the chi-square (χ2) test to examine differences in respondent characteristics, stratified by past year non-medical use of prescription pain medications. For our primary analysis, we used logistic regression to characterize the independent association between NMU of prescription pain medications and ED utilization among all adult survey respondents. We present staged model results to provide context on the role of sociodemographic characteristics, health status and substance use in the association of interest. Model 1 was adjusted for age, gender, race/ethnicity, education, insurance, family income, employment, marital status, rural location, and survey year; Model 2 was additionally adjusted for self-rated health and past year serious psychological distress; and Model 3 additionally adjusted for substance use variables. In subgroup analyses, we replicated Model 3 within pre-specified, clinically relevant subgroups.
In secondary analyses, we calculated unadjusted rates of past year ED utilization stratified by key variables of interest (i.e., frequency of non-medical use). We created a logistic regression model to characterize the association between increasing frequency of NMU of prescription pain medications and ED utilization. In addition to the covariates included in our full primary model, we adjusted for past year opioid withdrawal symptoms (Model 4) and source of prescription pain medications (Model 5) to characterize to contributions of opioid withdrawal and medication seeking to the association of interest. We report all model results as adjusted odds ratios (AOR) and 95% confidence intervals (CI).
All analyses were performed as recommended by SAMHSA and used the Surveyfreq, Surveylogistic, and Surveymeans procedures in SAS 9.4 (SAS Institute Inc., Cary, NC, USA) to account for the complex sampling design of the NSDUH. All statistical tests were two-sided and were considered statistically significant when P<0.05.
3. RESULTS
The study sample consisted of 228,556 adult respondents, representing an estimated 231 million civilian, non-institutionalized adults in the United States. An estimated 10.5 million American adults annually, or 4.6% of the adult population (95% CI 4.4%–4.7%), reported past year non-medical use of (NMU) of prescription pain medications. Adults with past year NMU of prescription pain medications were more likely to be young, male, white, publicly insured or uninsured, and unemployed compared with adults without past year NMU (Table 1). Adults with past year NMU were also more likely to report serious psychological distress, to report non-medical use of other prescription medications and to meet criteria for alcohol, cannabis or other illicit drug use disorder diagnoses.
Table 1.
Characteristics of United States, Civilian, Non-Institutionalized Adults by Past Year Non-Medical Use of Prescription Pain Medications, NSDUH 2008–2013 (N=228,556)
| Past Year Non-Medical Use of Prescription Pain Medications, % (N=16,846) | No Past Year Non-Medical Use (N=211,710) | P | |
|---|---|---|---|
| Age (years) | <.001 | ||
| 18–25 | 34% | 14% | |
| 26–34 | 25% | 15% | |
| 35–49 | 25% | 27% | |
| 50+ | 15% | 44% | |
| Male sex | 56% | 48% | <.001 |
| Race/ethnicity | <.001 | ||
| White | 71% | 67% | |
| Black | 9% | 12% | |
| Hispanic | 14% | 14% | |
| Other racea | 5% | 7% | |
| Insurance status | <.001 | ||
| Private | 54% | 67% | |
| Medicare/Medicaid | 14% | 14% | |
| Other insuranceb | 4% | 4% | |
| Uninsured | 27% | 15% | |
| High school graduate | 83% | 86% | <.001 |
| Unemployed | 11% | 5% | <.001 |
| Fair/poor health status | 14% | 13% | 0.22 |
| Serious psychological distressc | 28% | 10% | <.001 |
| Substance used | |||
| Other illicit SUD | 7% | 0.3% | <.001 |
| Alcohol use disorder | 29% | 6% | <.001 |
| Cannabis use disorder | 11% | 1% | <.001 |
| Other prescription drug NMU | 34% | 2% | <.001 |
| Nicotine dependence | 33% | 13% | <.001 |
| Frequency of NMU | |||
| 200–365 days | 8% | --- | |
| 100–199 days | 10% | --- | |
| 30–99 days | 20% | --- | |
| 1–29 days | 62% | --- | |
| Past year opioid withdrawal symptoms | 14% | --- | |
| Source of prescription pain medications | |||
| Physician | 20% | --- | |
| Family or friends | 65% | --- | |
| Other source | 15% | --- |
NSDUH=National Survey on Drug Use and Health. NMU=Non-medical use. 228,556 respondents represent 231 million adults in the United States annually.
Other race was most commonly Asian (69% of category), more than 1 race (19%), Native American (7%), Native Hawaiian (5%).
Other insurance includes Tricare/Veterans Affairs/Champus (32% of category) and other health insurance (68%).
Serious psychological distress defined as a score ≥13 on K6 Psychological Distress Scale.
Abuse or dependence diagnoses based on Diagnostic and Statistical Manual of Mental Disorders, 4th edition.
Other illicit drugs includes cocaine, heroin, hallucinogens and inhalants.
Other prescription drug’ includes sedatives, tranquilizers and stimulants.
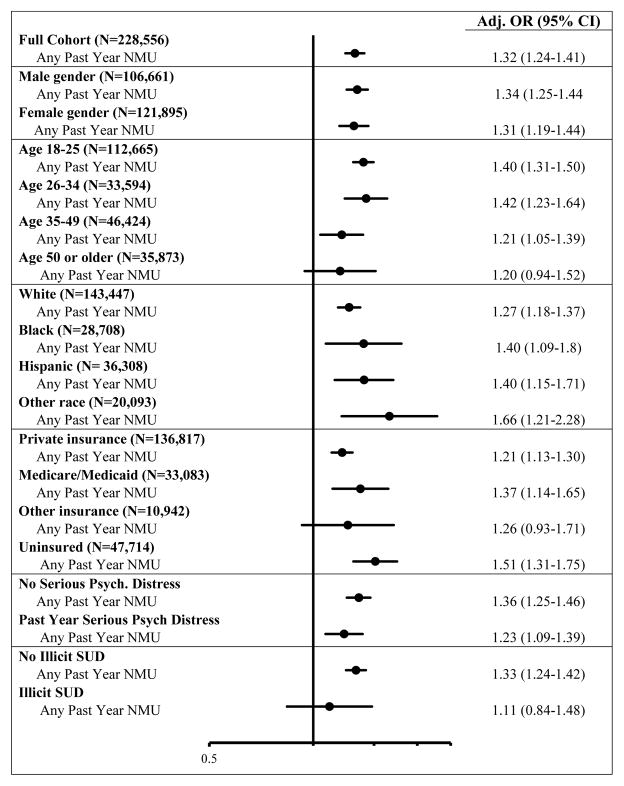
Adults with past year NMU of prescription pain medications were more likely to have visited the ED in the past year compared to adults without past year NMU (39.1% vs. 27.5%; P<0.001). From 2008–2013, an estimated 4.1 million U.S. adults annually reported both past year NMU of prescription pain medication and one or more ED visits. In multivariable modeling, NMU of prescription pain medications was independently associated with past year ED utilization (AOR 1.32; 95% CI 1.24–1.41; Table 2). Among the other substance use variables examined, past year illicit substance use disorder (AOR 1.41; 95% CI 1.20–1.67), past year nicotine dependence (AOR 1.29; 95% CI 1.23–1.34) and past year alcohol use disorder (AOR 1.09; 95% CI 1.03–1.15) were each independently associated with past year ED utilization. In subgroup analyses, NMU of prescription pain medications was independently associated with ED utilization in multiple subgroups (Figure 1) except for among individuals aged 50 or older, individuals with other insurance (i.e., Veterans Affairs) and individuals meeting criteria for an illicit substance use disorder.
Table 2.
Association Between Non-Medical Use of Prescription Pain Medications and Emergency Department Utilization, NSDUH 2008–2013 (N=228,556)
| Past Year ED Utilization | ||||
|---|---|---|---|---|
| Unadjusted | Model 1 | Model 2 | Model 3 | |
| Odds Ratio, 95% CI | Adjusted OR, 95% CI | Adjusted OR, 95% CI | Adjusted OR, 95% CI | |
| Non-medical use of prescription pain medications | 1.69 (1.60–1.79) | 1.60 (1.52–1.70) | 1.45 (1.38–1.53) | 1.32 (1.24–1.41) |
| Age (years) | ||||
| 18–25 | REF | REF | REF | REF |
| 26–34 | 1.24 (1.20–1.28) | 1.25 (1.19–1.31) | 0.86 (0.82–0.90) | 0.85 (0.81–0.88) |
| 35–49 | 1.10 (0.96–1.05) | 1.10 (1.04–1.15) | 0.72 (0.69–0.76) | 0.71 (0.68–0.75) |
| 50+ | 0.86 (0.82–0.90) | 0.96 (0.92–1.01) | 0.74 (0.70–0.78) | 0.75 (0.71–0.78) |
| Male sex | 1.23 (1.19–1.28) | 1.17 (1.13–1.22) | 1.16 (1.12–1.20) | 1.18 (1.13–1.22) |
| Race/ethnicity | ||||
| White | REF | REF | REF | REF |
| Black | 1.65 (1.58–1.72) | 1.39 (1.33–1.45) | 1.42 (1.36–1.48) | 1.45 (1.39–1.51) |
| Hispanic | 0.99 (0.94–1.05) | 0.84 (0.80–0.89) | 0.84 (0.79–0.89) | 0.88 (0.83–0.93) |
| Other race | 0.76 (0.71–0.81) | 0.75 (0.70–0.80) | 0.74 (0.70–0.80) | 0.76 (0.71–0.82) |
| Insurance status | ||||
| Private | REF | REF | REF | REF |
| Medicare/Medicaid | 2.29 (2.18–2.40) | 1.67 (1.58–1.77) | 1.49 (1.40–1.58) | 1.46 (1.38–1.55) |
| Other insurance | 1.46 (1.38–1.55) | 1.27 (1.20–1.36) | 1.20 (1.12–1.28) | 1.18 (1.10–1.26) |
| Uninsured | 1.28 (1.23–1.33) | 1.01 (0.96–1.06) | 0.98 (0.93–1.03) | 0.95 (0.90–0.99) |
| High school graduate | 0.62 (0.59–0.64) | 0.77 (0.70–0.80) | 0.84 (0.80–0.88) | 0.86 (0.82–0.90) |
| Family income | ||||
| <$20,000 | REF | REF | REF | REF |
| $20,000–49,999 | 0.70 (0.67–0.72) | 0.86 (0.83–0.90) | 0.91 (0.87–0.95) | 0.91 (0.87–0.95) |
| $50,000–74,999 | 0.54 (0.52–0.57) | 0.75 (0.71–0.79) | 0.81 (0.77–0.86) | 0.82 (0.78–0.87) |
| >$75,000 | 0.44 (0.42–0.46) | 0.66 (0.62–0.69) | 0.73 (0.69–0.77) | 0.74 (0.70–0.78) |
| Unemployed | 1.34 (1.25–1.43) | 1.10 (1.03–1.17) | 1.16 (1.04–1.18) | 1.14 (1.09–1.19) |
| Good health status | 0.40 (0.39–0.42) | --- | 0.50 (0.48–0.52) | 0.51 (0.49–0.53) |
| Serious psych. distress | 2.13 (2.03–2.23) | --- | 1.67 (1.59–1.75) | 1.60 (1.53–1.68) |
| Substance use | ||||
| Other illicit SUD | 2.58 (2.22–3.00) | --- | --- | 1.41 (1.20–1.67) |
| Alcohol use disorder | 1.30 (1.23–1.38) | --- | --- | 1.09 (1.03–1.15) |
| Cannabis use disorder | 1.73 (1.58–1.89) | --- | --- | 1.07 (0.97–1.19) |
| Other prescription drug NMU | 1.56 (1.45–1.67) | --- | --- | 1.06 (0.96–1.16) |
| Nicotine dependence | 1.69 (1.63–1.76) | --- | --- | 1.29 (1.23–1.34) |
NSDUH=National Survey on Drug Use and Health; ED=Emergency Department; OR=odds ratio; CI=confidence interval; SUD=substance use disorder; NMU=non-medical use. Model 1 adjusted for age, gender, race/ethnicity, education, insurance, family income, employment, marital status, rural location, and survey year. Model 2 includes Model 1 plus self-rated health and past year serious psychological distress. Model 3 includes Model 2 plus abuse or dependence of alcohol, cannabis, and other illicit drugs (heroin, cocaine, hallucinogens and inhalants), non-medical use of other prescription medications, and nicotine dependence.
Figure 1.
Subgroup Analyses of Non-Medical Use of Prescription Pain Medications and Emergency Department Utilization, NSDUH 2008–2013
NMU=Non-medical use; SUD=Substance use disorder. All models adjusted for age, gender, race/ethnicity, education, insurance, family income, employment, marital status, rural location, survey year, self-rated health, past year serious psychological distress, abuse or dependence of alcohol, cannabis, and other illicit drugs (heroin, cocaine, hallucinogens and inhalants), non-medical use of other prescription medications, and nicotine dependence. Referent=Individuals without past year non-medical use in specified subgroup.
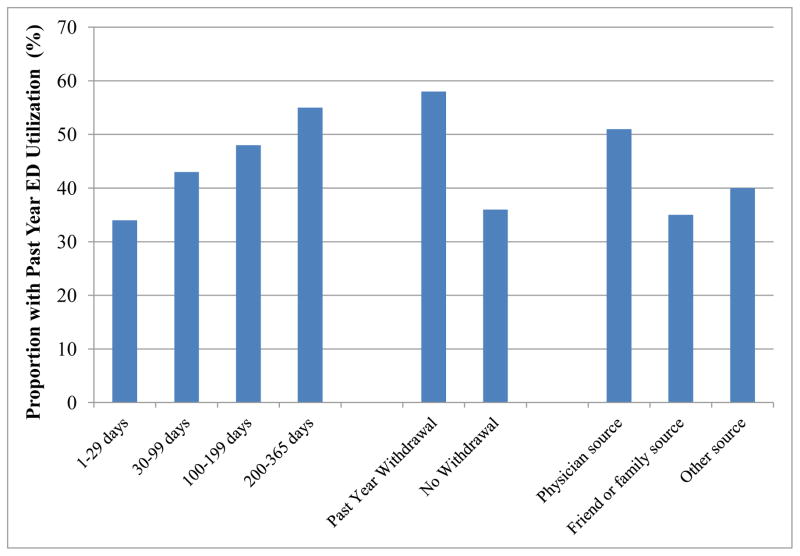
In secondary analyses, individuals with more frequent past year NMU of prescription pain medications were more likely to report past year ED utilization. This relationship exhibited a ‘dose-response’ relationship with past year ED utilization increasing incrementally with increasing NMU (Figure 2). In multivariable models, this association persisted with adjustment for sociodemographic characteristics, health status, substance use and opioid withdrawal (Table 3; Models 1–4). However, after adjustment for source of prescription pain medications (Table 3; Model 5), NMU was not significantly associated with ED utilization at any level of NMU frequency compared to no past year NMU. In this model, a physician source of prescription pain medications used non-medically was significantly associated with past year ED utilization (AOR 2.44; 95% CI 1.75–3.39) compared to adults without past year NMU.
Figure 2.
Unadjusted Past Year Emergency Department Utilization Among Adults with Past Year Non-Medical Use of Prescription Pain Medications, NSDUH 2008–2013 (N=16,846)
ED=Emergency Department. Unadjusted past year Emergency Department utilization stratified by frequency of past year non-medical use, past year opioid withdrawal symptoms, and source of prescription pain medications used non-medically.
Table 3.
Frequency of Non-Medical Use of Prescription Pain Medications and Emergency Department Utilization, NSDUH 2008–2013 (N=228,556)
| Past Year ED Utilization | ||||||
|---|---|---|---|---|---|---|
| Unadjust ed | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Odds Ratio, 95% CI | Adjusted OR, 95% CI | Adjusted OR, 95% CI | Adjusted OR, 95% CI | Adjusted OR, 95% CI | Adjusted OR, 95% CI | |
| Frequency of NMU | ||||||
| 200–365 days | 3.20 (2.70–3.97) | 2.86 (2.40–3.41) | 2.46 (2.06–2.94) | 2.07 (1.71–2.50) | 1.69 (1.38–2.07) | 1.08 (0.76–1.55) |
| 100–199 days | 2.41 (2.05–2.84) | 2.09 (1.78–2.45) | 1.76 (1.49–2.08) | 1.53 (1.28–1.82) | 1.34 (1.11–1.60) | 0.85 (0.59–1.23) |
| 30–99 days | 2.01 (1.80–2.26) | 1.83 (1.64–2.05) | 1.66 (1.48–1.86) | 1.49 (1.31–1.70) | 1.38 (1.20–1.58) | 0.91 (0.66–1.25) |
| 1–29 days | 1.38 (1.27–1.49) | 1.36 (1.25–1.47) | 1.26 (1.16–1.36) | 1.18 (1.09–1.28) | 1.15 (1.06–1.25) | 0.78 (0.56–1.09) |
| No past year NMU | REF | REF | REF | REF | REF | REF |
| Past year opioid withdrawal symptoms | 3.53 (3.13–3.98) | --- | --- | --- | 1.62 (1.39–1.89) | 1.62 (1.38–1.90) |
| Source of prescription pain medications | ||||||
| Physician | 2.79 (2.39–3.27) | --- | --- | --- | --- | 2.44 (1.75–3.39) |
| Family or friends | 1.43 (1.34–1.53) | --- | --- | --- | --- | 1.30 (0.93–1.80) |
| Other source | 1.71 (1.50–1.94) | --- | --- | --- | --- | 1.41 (1.07–1.85) |
| No past year NMU | REF | --- | --- | --- | --- | REF |
NSDUH=National Survey on Drug Use and Health; ED=Emergency Department; OR=odds ratio; CI=confidence interval; NMU=Non-medical use. Model 1 adjusted for age, gender, race/ethnicity, education, insurance, family income, employment, marital status, rural location, and survey year. Model 2 includes Model 1 plus self-rated health and past year serious psychological distress. Model 3 includes Model 2 plus abuse or dependence of alcohol, cannabis, and other illicit drugs (heroin, cocaine, hallucinogens and inhalants), non-medical use of other prescription medications, and nicotine dependence. Model 4 includes Model 3 plus past year opioid withdrawal symptoms. Model 5 includes Model 4 plus self-reported source of prescription pain medications.
4. DISCUSSION
In this study, we examined the association between NMU of prescription pain medications and ED utilization in a nationally representative sample. The 10.5 million U.S. adults with past year NMU of prescription pain medications were significantly more likely to report past year ED utilization. After adjusting for important sociodemographic and clinical factors, we identified an independent association between past year NMU of prescription pain medications and ED utilization. In secondary analyses, the association between NMU of prescription pain medications and ED utilization was noted in several subgroups.
We estimate that 4.1 million U.S. adults report both past year NMU of prescription pain medications and one or more past year ED visits. This estimate is substantially higher than existing visit-based estimates of ED utilization directly attributed opioid medications (i.e., overdose or detoxification). By comparison, in 2010, there were an approximately 136,000 ED visits nationally related to opioid overdose with 84% of these visits potentially involving prescription opioids (Yokell et al., 2014). In the most recent data available from the Drug Abuse Warning Network in 2011, there were 121,000 ED visits nationally involving individuals seeking detoxification from prescription pain medications, and 500,000 visits related to non-medical use of prescription pain medication (SAMHSA, 2013b). These prior estimates include only those visits in which an opioid-related adverse health outcome was diagnosed and documented and so likely underestimate the full impact of non-medical use of opioids on ED utilization. First, self-reported ED utilization in the NSDUH also includes opioid-related adverse events that were not diagnosed by ED providers. For example, receipt of high-dose opioid medications has previously been linked to injuries due to motor vehicles and fractures (Gomes et al., 2013; Saunders et al., 2010). Such adverse events may also result from NMU of prescription pain medications, but this link may not be identified in busy ED settings. Second, our estimate may also include ED visits intended to obtain prescription pain medications for non-medical use and visits related to pain in which prescribed medications were subsequently used non-medically. From NSDUH data, we cannot determine the relative proportions of these different visit types. Future approaches should consider incorporating more detailed assessments of healthcare utilization in national surveys such as the NSDUH and developing more sophisticated tools for identifying opioid-related visits in analyses of existing medical record data.
Our estimate of self-reported ED utilization by adults with past year NMU of prescription pain medications also includes ED visits that were not related to NMU. Importantly, these visits may still provide opportunities for screening, patient education, intervention or referral to treatment. The feasibility and effectiveness of ED-based programs to screen for, intervene on or prevent NMU of prescription pain medications require further study.
In our secondary analysis, we identified an association between a physician source of prescription pain medications and increased ED utilization, and this association fully accounted for the apparent ‘dose-response’ effect of increasing NMU frequency. This finding may reflect riskier use and higher rates of opioid-related adverse events by individuals obtaining prescription pain medications from physicians compared to those obtaining medications from other sources. Prior work has shown that a physician source is associated with more frequent non-medical use and is a common source among patients in treatment programs (Brands et al., 2004; Rosenblum et al., 2007). Alternatively, the link between increased ED utilization and a physician source may represent attempts to obtain opioid medications. While the rate of ED visits involving pain complaints remained stable from 2001 to 2010, an opioid medication was administered in the ED or prescribed at discharge in 31% of all ED visits nationally in 2010, up from to 21% in 2001 (Chang et al., 2014; Mazer-Amirshahi et al., 2014). In a more recent study, approximately 1 in 6 patients discharged from the ED received an opioid medication at discharge (Hoppe et al., 2015). The safe and effective management of pain remains challenging, and non-pharmacologic pain management options are not adequately accessible (Coffin and Banta-Green, 2014). Evidence-based tools and accessible pain care resources are needed to support clinicians’ ability to accurately diagnose and treat pain in ED settings. Similarly, integration of prescription drug monitoring programs into routine clinical care and accessible substance use disorder treatment services may support providers’ efforts to identify and appropriately care for patients seeking opioid medications for non-medical use (Gugelmann and Perrone, 2011).
Although past year opioid withdrawal was reported by a minority of respondents, this experience was significantly associated with ED utilization in our secondary analysis. Opioid withdrawal symptoms may drive ED utilization for individuals seeking symptom management, referral to treatment, or additional opioid medications. In the context of increasing scrutiny on the supply of prescription opioid medications and rising rates of heroin use (Cicero et al., 2014; Dart et al., 2015; Unick et al., 2013), opioid withdrawal symptoms may also play a role in an individual’s transition from prescribed to illicit opioids. Well-meaning efforts to prevent the adverse health effects of prescription pain medications will continue in the years ahead, and their consequences, both intended and unintended, warrant ongoing examination.
Our findings should be interpreted in the context of the limitations of our study. First, data on non-medical use of prescription opioid medications and ED utilization were self-reported. Underreporting of non-medical use may be present. Perceived “medical use” of prescription pain medications and associated adverse health outcomes are not captured in this dataset. Both would lead to an underestimation of the population-level impact of prescription pain medications and would be expected to bias our findings toward the null. Self-reported past year ED utilization could not be verified with other data sources such as medical record or claims data. Second, the survey is cross-sectional and does not provide longitudinal follow-up of individual respondents. We cannot attribute causality nor can we determine the timing of reported events. We believe that whether non-medical use of prescription pain medications occurred before or after ED utilization, study findings identify a problem in need of attention. Third, as survey data are observational, we cannot exclude residual confounding. Importantly, though we did adjust for self-reported health status and psychological distress, pain is not assessed by the NSDUH. Untreated or inadequately treated pain may drive both ED utilization and non-medical use of prescription pain medications. Further study of this issue will benefit from the inclusion of patient-reported data on pain and pain-related function. Fourth, as the survey does not collect information for specific ED visits, we are not able to examine the reason for individual encounters. We cannot ascertain whether individual ED visits were related to NMU or explore the mechanism of NMU-related ED visits. Opioid overdose, requests for detoxification or requests for pain medications pose different clinical challenges and will require different interventions. Finally, the NSDUH does not collect data on specific pain medications used non-medically in the past year and so estimates of past year non-medical use include both opioid and non-opioid pain medications. Among NSDUH respondents reporting past year non-medical use of pain medications, >96% reported a lifetime history of using an opioid medication non-medically, which likely account for the vast majority of reported past year non-medical use.
Healthcare, public health and policy interventions to prevent harms related to opioid pain medications continue to gain momentum. In March 2015, the U.S. Department of Health and Human Services announced an initiative to expand education, prevention and treatment (HHS, 2015). In April, the Centers for Disease Control and Prevention launched a new public awareness campaign to address what it calls a “prescription painkiller overdose epidemic” (CDC, 2015). Given the level of contact with ED settings by individuals with recent NMU of prescription pain medications documented in this study, ED settings should be integral part of these efforts. Recent studies of ED-based interventions for problematic drug use have yielded mixed results (Bogenschutz et al., 2014; D'Onofrio et al., 2015). In both studies, a minority of participants reported prescription opioids as the primary substance of abuse. Evidence-based strategies for ED-based screening, education and treatment referral are needed and should specifically target high-risk prescription pain medication use. Whether related to an opioid-related adverse event, opioid withdrawal or a request for pain medication, these visits present an important opportunity to engage and education patients. Additionally, with growing evidence to guide treatment of prescription opioid use disorder in other clinical settings (Fiellin et al., 2014), work is also needed to support coordination of care between ED, pain management and substance use treatment settings.
Highlights.
We analyzed non-medical use (NMU) of prescription pain medications and emergency department (ED) use nationally in US.
0.5 million U.S. adults annually used prescription pain medications non-medically.
Past year NMU of prescription pain medications increased odds of past year ED use.
Physician source of pain medications significantly associated with ED use.
Acknowledgments
Sources of Funding/Support
Dr. Frank was supported by the Division of General Internal Medicine, Department of Medicine, University of Colorado School of Medicine and the VA Eastern Colorado Health Care System. Dr. Binswanger was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number R34DA035952. Dr. Calcaterra was supported by the Division of General Internal Medicine, Department of Medicine, University of Colorado School of Medicine and by Denver Health Medical Center. Dr. Levy was supported by the Denver-Seattle Center of Innovation for Veteran-Centered and Value Driven Care. The views expressed in this article are those of the authors and do not necessarily represent the official views of the National Institutes of Health or the US Department of Veterans Affairs.
Role of Funding Sources
The funding organizations had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Footnotes
Contributors
Concept and design (JWF, CL, IAB); data collection (JWF); data analysis (JWF); data interpretation (all authors); drafting of the manuscript (JWF); critical revision of the manuscript for important intellectual content (all authors). JWF had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors have approved of the final article.
Conflicts of interest
No conflict declared.
Previous Presentations
We presented a preliminary version of these findings as an oral presentation at the Society of General Internal Medicine Meeting on April 23, 2015 in Toronto, Canada.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Becker WC, Tobin DG, Fiellin DA. Nonmedical use of opioid analgesics obtained directly from physicians: prevalence and correlates. Arch Intern Med. 2011;171:1034–1036. doi: 10.1001/archinternmed.2011.217. [DOI] [PubMed] [Google Scholar]
- Bogenschutz MP, Donovan DM, Mandler RN, Perl HI, Forcehimes AA, Crandall C, Lindblad R, Oden NL, Sharma G, Metsch L, Lyons MS, McCormack R, Konstantopoulos WM, Douaihy A. Brief Intervention for patients with problematic drug use presenting in emergency departments: a randomized clinical trial. JAMA Intern Med. 2014;174:1736–1745. doi: 10.1001/jamainternmed.2014.4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brands B, Blake J, Sproule B, Gourlay D, Busto U. Prescription opioid abuse in patients presenting for methadone maintenance treatment. Drug Alcohol Depend. 2004;73:199–207. doi: 10.1016/j.drugalcdep.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Cai R, Crane E, Poneleit K, Paulozzi L. Emergency Department visits involving nonmedical use of selected prescription drugs - United States, 2004–2008. MMWR. 2010;61:705–709. doi: 10.3109/15360288.2010.503730. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) [accessed on April 13 2015];Injury Prevention and Control: Prescription Drug Overdose. 2015 http://www.cdc.gov/drugoverdose/
- Chang HY, Daubresse M, Kruszewski SP, Alexander GC. Prevalence and treatment of pain in EDs in the United States, 2000 to 2010. Am J Emerg Med. 2014;32:421–431. doi: 10.1016/j.ajem.2014.01.015. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71:821–826. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Coffin P, Banta-Green C. The dueling obligations of opioid stewardship. Ann Intern Med. 2014;161:307–308. doi: 10.7326/L14-5016-8. [DOI] [PubMed] [Google Scholar]
- D'Onofrio G, O'Connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, Bernstein SL, Fiellin DA. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313:1636–1644. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dart RC, Surratt HL, Cicero TJ, Parrino MW, Severtson SG, Bucher-Bartelson B, Green JL. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372:241–248. doi: 10.1056/NEJMsa1406143. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services (HHS) [accesse d on April 13 2015];HHS takes strong steps to address opioid-drug related overdose, death and dependence. 2015 http://www.hhs.gov/news/press/2015pres/03/20150326a.html.
- Fiellin DA, Schottenfeld RS, Cutter CJ, Moore BA, Barry DT, O'Connor PG. Primary care-based buprenorphine taper vs maintenance therapy for prescription opioid dependence: a randomized clinical trial. JAMA Intern Med. 2014;174:1947–1954. doi: 10.1001/jamainternmed.2014.5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frieden T. [accessed on April 11 2015];Ending Opioid Abuse: What Clinicians Can Do. 2014 http://www.medscape.com/viewarticle/831347.
- Gomes T, Redelmeier DA, Juurlink DN, Dhalla IA, Camacho X, Mamdani MM. Opioid dose and risk of road trauma in Canada: a population-based study. JAMA Intern Med. 2013;173:196–201. doi: 10.1001/2013.jamainternmed.733. [DOI] [PubMed] [Google Scholar]
- Gugelmann HM, Perrone J. Can prescription drug monitoring programs help limit opioid abuse? JAMA. 2011;306:2258–2259. doi: 10.1001/jama.2011.1712. [DOI] [PubMed] [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- Hasegawa K, Espinola JA, Brown DF, Camargo CA., Jr Trends in U.S. Emergency department visits for opioid overdose, 1993–2010. Pain Med. 2014;15:1765–1770. doi: 10.1111/pme.12461. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84:791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- Hoppe JA, Nelson LS, Perrone J, Weiner SG Prescribing Opioids Safely in the Emergency Department Study. Opioid prescribing in a cross section of US emergency departments. Ann Emerg Med. 2015;66:253–259. e251. doi: 10.1016/j.annemergmed.2015.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM. Frequency of prescription pain reliever nonmedical use: 2002–2003 and 2009–2010. Arch Intern Med. 2012;172:1265–1267. doi: 10.1001/archinternmed.2012.2533. [DOI] [PubMed] [Google Scholar]
- Jones CM, Paulozzi LJ, Mack KA. Sources of prescription opioid pain relievers by frequency of past-year nonmedical use United States, 2008–2011. JAMA Intern Med. 2014;174:802–803. doi: 10.1001/jamainternmed.2013.12809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Krantz MJ, Mehler PS. Treating opioid dependence. Growing implications for primary care. Arch Intern Med. 2004;164:277–288. doi: 10.1001/archinte.164.3.277. [DOI] [PubMed] [Google Scholar]
- Mazer-Amirshahi M, Mullins PM, Rasooly I, van den Anker J, Pines JM. Rising opioid prescribing in adult U.S. emergency department visits: 2001–2010. Acad Emerg Med. 2014;21:236–243. doi: 10.1111/acem.12328. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Jones CM, Mack KA, Rudd RA. Vital signs: overdoses of prescription opioid pain relievers - United States, 1999–2008. MMWR. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- Rosenblum A, Parrino M, Schnoll SH, Fong C, Maxwell C, Cleland CM, Magura S, Haddox JD. Prescription opioid abuse among enrollees into methadone maintenance treatment. Drug Alcohol Depend. 2007;90:64–71. doi: 10.1016/j.drugalcdep.2007.02.012. [DOI] [PubMed] [Google Scholar]
- SAMHSA. 2008 National Survey on Drug Use and Health: Public Use File Codebook. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. [Google Scholar]
- SAMHSA. 2009 National Survey on Drug Use and Health: Public Use File Codebook. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2010. [Google Scholar]
- SAMHSA. 2010 National Survey on Drug Use and Health Public Use File Codebook. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2011. [Google Scholar]
- SAMHSA. 2011 National Survey on Drug Use and Health Public Use File Codebook. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2012. [Google Scholar]
- SAMHSA. 2012 National Survey on Drug Use and Health Public Use File Codebook. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013a. [Google Scholar]
- SAMHSA. Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013b. [PubMed] [Google Scholar]
- SAMHSA. 2013 National Survey on Drug Use and Health Public Use File Codebook. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. [Google Scholar]
- Saunders KW, Dunn KM, Merrill JO, Sullivan M, Weisner C, Braden JB, Psaty BM, Von Korff M. Relationship of opioid use and dosage levels to fractures in older chronic pain patients. J Gen Int Med. 2010;25:310–315. doi: 10.1007/s11606-009-1218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Unick GJ, Rosenblum D, Mars S, Ciccarone D. Intertwined epidemics: national demographic trends in hospitalizations for heroin- and opioid-related overdoses, 1993–2009. PLoS One. 2013;8:e54496. doi: 10.1371/journal.pone.0054496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang KH, Fiellin DA, Becker WC. Source of prescription drugs used nonmedically in rural and urban populations. Am J Drug Alcohol Abuse. 2014;40:292–303. doi: 10.3109/00952990.2014.907301. [DOI] [PubMed] [Google Scholar]
- Yokell MA, Delgado MK, Zaller ND, Wang NE, McGowan SK, Green TC. Presentation of prescription and nonprescription opioid overdoses to US emergency departments. JAMA Intern Med. 2014;174:2034–2037. doi: 10.1001/jamainternmed.2014.5413. [DOI] [PubMed] [Google Scholar]