Abstract
May-Thurner syndrome (MTS) is the pathologic compression of the left common iliac vein by the right common iliac artery, resulting in left lower extremity pain, swelling, and deep venous thrombosis. Though this syndrome was first described in 1851, there are currently no standardized criteria to establish the diagnosis of MTS. Since MTS is treated by a wide array of specialties, including interventional radiology, vascular surgery, cardiology, and vascular medicine, the need for an established diagnostic criterion is imperative in order to reduce misdiagnosis and inappropriate treatment. Although MTS has historically been diagnosed by the presence of pathologic features, the use of dynamic imaging techniques has led to a more radiologic based diagnosis. Thus, imaging plays an integral part in screening patients for MTS, and the utility of a wide array of imaging modalities has been evaluated. Here, we summarize the historical aspects of the clinical features of this syndrome. We then provide a comprehensive assessment of the literature on the efficacy of imaging tools available to diagnose MTS. Lastly, we provide clinical pearls and recommendations to aid physicians in diagnosing the syndrome through the use of provocative measures.
Keywords: May-Thurner, Thrombosis, Diagnostic, Iliac compression, Vascular, Imaging
Core tip: There is currently no gold standard diagnostic criterion in iliac vein compression syndrome. Historically, the presence of pathologic factors has been the main component in diagnosis; however, imaging techniques have led to a more radiologic-based diagnosis. This review details the clinical and radiologic challenges in the diagnosis of Iliac vein compression syndrome and presents clinical pearls that may help in deciding whether an endovascular intervention should be performed.
INTRODUCTION
Iliac vein compression syndrome, also know as May-Thurner syndrome (MTS), is caused by both mechanical and physiologic factors; the chronic pulsatile compression of the left common iliac vein (LCIV) by the right common iliac artery (RCIA) stimulates the formation of fibrotic adhesions that can cause partial or complete iliac vein obstruction over time[1,2]. The true incidence of MTS is not known. However, iliofemoral thrombosis is responsible for approximately 2%-3% of lower limb deep venous thrombosis (DVT) cases and approximately 50%-60% of left sided iliofemoral DVT cases exhibit iliac vein spurs resulting from extrinsic compression[3-6]. Thus, MTS is a reasonably common occurrence and a greater level of clinical suspicion is necessary.
Although MTS has historically been diagnosed by the presence of pathologic features, the use of dynamic imaging techniques has led to a more radiologic based diagnosis. However, a diagnosis of MTS relies on both clinical and imaging findings because the presence of iliac vein compression alone is insufficient for a diagnosis. There are currently no standardized clinical or radiologic diagnostic protocols in place to aid in the identification of MTS. Since MTS is treated by a wide array of specialties, including interventional radiology, vascular surgery, cardiology, and vascular medicine, the need for an established diagnostic criterion is imperative in order to reduce misdiagnosis and inappropriate treatment. MTS patients generally do not respond well to conservative treatments; thus, early diagnosis and treatment is paramount in order to avoid complications such as iliofemoral DVT or venous insufficiency[3,4]. This review will describe the clinical presentations of MTS and focus on the imaging modalities that have been used in aiding and confirming a diagnosis.
HISTORICAL BACKGROUND
In 1851, Virchow noted the first anatomical evidence for MTS when he observed an increased frequency of DVT in the left leg due to the compression of the left iliac vein between the overlying right iliac artery and the fifth lumbar vertebrae[4]. In 1908, McMurrich examined the iliac veins of 107 cadavers and observed that 29.9% had obstructions in the left iliac vein; he deemed that these obstructions were congenital in origin and were responsible for the increased incidence of left lower extremity (LLE) DVT[7]. In 1943, Ehrich and Krumbhaar found that out of 412 cadavers, 95 (23.8%) demonstrated obstructive lesions in the LCIV; the obstructions were comprised of collagen and elastin and were demonstrated to be acquired rather than congenital, as was previously thought[8]. However, a comprehensive understanding of the anatomic variants of MTS was not established until 1957, with the work of May and Thurner.
May and Thurner, for whom the syndrome is named, found that 22% of 430 cadavers exhibited lesions in the LCIV; these lesions were described as “spurs” and were postulated to arise from the chronic compression of the LCIV by the RCIA. The spurs were categorized as central, lateral, or resulting in partial obliteration, based on location and size. Central spurs occur on the anteroposterior plane and split the lumina in two, lateral spurs occur along the sides of the LCIV, and partial obliteration results in the lumen being covered in a lattice of spurs and results in decreased venous flow[7,8]. In 1965, Cockett et al[9] further expounded the field by determining that patients with LCIV spurs could remain asymptomatic for a period of time due to the formation of venous collaterals. However, it was ruled that spur formation was an irreversible process, making early diagnosis integral for MTS patients.
ROLE OF CLINICAL PRESENTATION IN DIAGNOSIS
The clinical presentation and history of the patient are critical components in formulating a diagnosis of MTS. MTS is particularly prevalent in younger and middle aged women (mean age = 42), although it also affects men[5]. Patients most commonly present with DVT, but may also present with LLE swelling, pain, venous claudication, ulcerations, nausea, and varicose veins. Rarer symptoms include phlebitis, phlegmasia alba dolens, phlegmasia cerulea dolens, and bilateral or right sided symptoms[3,5-7,10]. MTS can present either acute or chronically; acute presentation of MTS is the sudden onset of left leg edema and is usually easier to diagnose, while the chronic phase of MTS is much more difficult to identify and requires a comprehensive investigation of patient history, physical examination, and diagnostic imaging studies[7]. The clinical stages of MTS can be further delineated as being either Stage I, asymptomatic LCIV compression; stage II, the formation of an intraluminal spur; or Stage III, the occurrence of left iliac vein DVT[11].
A patient history that reveals recurrent DVT, unexplained LLE edema, venous claudication, or varicosities should create suspicion for MTS as a cause. Additionally, physical examination that demonstrates LLE swelling, skin hyperpigmentation, varicose veins, telangiectasias, or evidence of ulceration in the ankle area are supportive of MTS[7,12]. Iliofemoral thrombosis can also be a result of trauma, surgery, immobilization, recent catheterization, radiation and malignancies and all these explanations must be ruled out in order to diagnose MTS[13]. Once differential diagnoses have been investigated, diagnostic imaging tests should be undertaken in order to confirm the presence of MTS anatomy and determine the best modality of treatment.
DIAGNOSTIC IMAGING CRITERION AND TECHNIQUES
Several studies have confirmed the presence of LCIV compression in an asymptomatic patient population; these suggest that LCIV compression is a normal anatomic variant and not necessarily a pathologic condition[14-16]. Moreover, McDermott et al[1] found that the degree of LCIV compression in a single patient can vary over a short period of time (Figure 1); thus, the finding of May-Thurner anatomy in a single imaging study may just reflect the volume status of patient and may not be sufficient to suspect or confirm MTS[1]. Although there is no established diagnostic imaging criterion for MTS, studies recommend that the imaging standard for appropriate diagnosis of MTS should exhibit persistent narrowing of the iliac vein due to the presence of permanent iliac spurs, regardless of patient positioning during the imaging study. Thus, normal variant LCIV compression may be ruled out by placing the patient in prone position as such positioning may demonstrate a decrease in collateral flow or reveal normal iliac vein patency[1]. A visualization of greater than 50% stenosis in the luminal diameter of the vein is considered an adequate indicator of LCIV compression related to MTS[17]. An additional secondary indicator of MTS is the presence of venous collaterals, presence of intraluminal spurs, and changes in hemodynamic flow greater than 2 mmHg across the stenotic region with the patient in supine positioning[1,4,17]. The MTS diagnostic imaging modalities include ultrasonography, pleythysmography, computed tomography (CT), magnetic resonance venography (MRV), ascending contrast venography, hemodynamic studies, and intravascular ultrasound (IVUS) (Figure 2). The advantages and disadvantages of each imaging technique in the diagnosis of MTS are discussed below.
Figure 1.
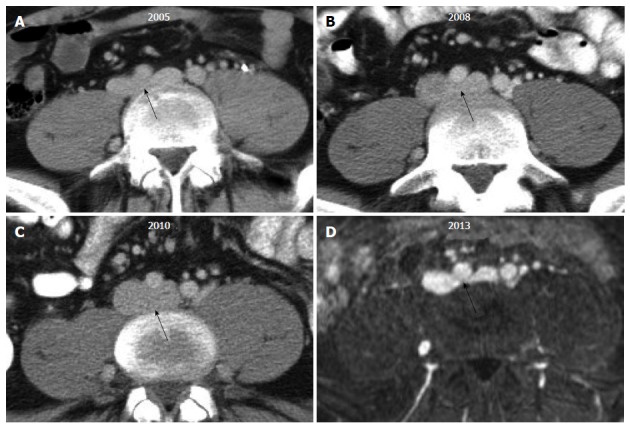
Transverse computed tomography and magnetic resonance images of the proximal left common iliac vein (black arrow) in a single patient across multiple time points illustrate the challenge of diagnosing May-Thurner syndrome. The degree of venous compression can vary substantially from one imaging study to another based upon the patient’s volume status.
Figure 2.
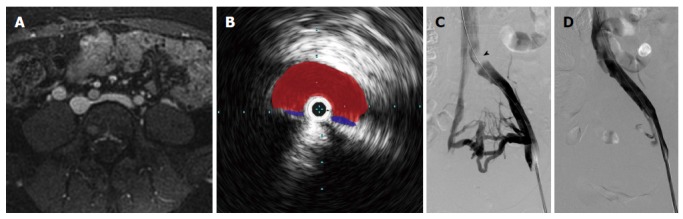
The appearance of May-Thurner syndrome on multiple imaging modalities from a single patient. A: Axial T1 fat-saturated magnetic resonance image following the administration of an intravascular contrast agent demonstrates > 50% narrowing of the left common iliac vein by the overlying right common iliac artery; B: Intravascular ultrasound with the transducer within the left common iliac vein (blue) demonstrates near complete obliteration of the vessel’s lumen due to compression by the right common iliac artery (red); C: Digital subtraction angiography with contrast injection from a vascular sheath in the left external iliac vein demonstrates an obliquely oriented silhouette of the right common iliac artery compressing the left common iliac vein (arrowhead); multiple left-to-right pelvic collaterals are also present, signifying that the compression is hemodynamically significant; D: Following the placement of an uncovered stent, the compression is resolved, and there is no longer filling of the cross-pelvic collaterals.
Ultrasonography
Color Doppler ultrasonography (CDUS) is often the initial diagnostic modality in determining venous insufficiencies and DVT because it is noninvasive, bares no risk to the patient, is easy to perform, and is accurate in determining the location, severity, and cause of venous insufficiencies[18]. Ultrasound can usually identify acute iliofemoral DVT, a common result of MTS[7]. However, ultrasound has significant limitations in visualizing abnormalities of the iliac veins because of the deep location of the veins in the pelvis; skilled sonographers are unable to visualize the iliac veins in approximately 20% of cases. Moreover, ultrasound does not reveal the specific anatomic characteristics of MTS such as iliac vein compression or intraluminal spurs[4,18]. However, in a case report by Oğuzkurt et al[3], a diagnosis of MTS was initially reached by transabdominal ultrasonography alone and later confirmed by CT, venography, and pressure measurements. Although transvaginal ultrasound can be used to determine the pathological reflux in the internal iliac veins in women, it does not allow for good imaging of the common iliac veins and is therefore not a very useful tool in the diagnosis of MTS[19]. Overall, ultrasound is a useful mechanism for determining venous patency, but a negative study result does not rule out the possibility of MTS and therefore more imaging tests are needed in order to establish a diagnosis.
Pleythysmography
Air pleythysmography (APG) is a noninvasive test that can determine the degree of venous reflux and evaluate any proximal obstructions[7]. Hurst et al[5] utilized APG to determine the degree of iliac vein obstruction in 9 patients in order to confirm a suspected diagnosis of MTS. In all 9 cases, APG was unable to detect any iliac vein obstructions despite the presence of occlusions or stenosis in all patients. Hurst et al[5] thus concluded that APG has a low sensitivity in confirming a diagnosis of MTS. Although APG can be useful in evaluating the severity of venous symptoms, it can be nondiagnostic due to the presence of collateral pathways and a lack of sufficient narrowing to impact the flow dynamics[4,5]. Therefore, APG is not considered a routine diagnostic tool for MTS and more invasive tests are required in order to confirm a diagnosis of MTS.
CT
CT with intravenous contrast in a transverse plane has proven to be a useful modality in confirming the diagnosis of MTS[14,18,20]. A CT examination of the abdomen or pelvis can rule out extrinsic reasons of compression as well as identify acute DVT and collateral pathways; however, a normal CT with 10-mm cuts cannot always establish a diagnosis of MTS because small iliac spurs are often too difficult to visualize and fibrosis can conceal the underlying vasculature[7,8,21]. However, a CT analysis utilizing narrower cuts 3 to 5-mm can be sufficient enough to visualize the structural details that may be previously missed. Chung et al[21] utilized spiral CT venography to evaluate iliac vein compression due to MTS in 27 out of 44 patients presenting with lower extremity DVT; Oguzkurt et al[22] found that CT images in a transverse plane showed the compression of the LCIV by the LCIA in all 10 patients tested. Additionally, in a study conducted by Liu et al[17], CT venography was found to have a high sensitivity and specificity in confirming MTS over other imaging modalities and that it can also distinguish between non-thrombotic and thrombotic MTS. The advantages of CT venography over CDUS or traditional venography include lack of operator dependence, clearer imaging of the pelvic veins, and a shorter exam time; however, the radiation dose is contraindicated in instances of pregnancy and large amount of contrast medium required for CT venography are contraindicated in patients with renal impairment[22]. Overall, CT venography is a useful diagnostic tool in demonstrating iliac vein compression, although more studies are required in order to fully evaluate the sensitivity and specificity of CT images in diagnosing MTS.
MRV
Several studies have advocated that MRV is a suitable imaging modality in diagnosing MTS (Figure 3)[4-7,13]. In a case study by Wolpert et al[13], MRV was able to confirm a diagnosis of MTS in all 9 patients that presented with the condition; moreover, MRV was able to reveal the anatomic abnormalities of MTS as well as rule out the presence of DVT or pelvic masses. Additionally, Shebel et al[7] found that MRV was able to confirm the presence of nonocclusive iliac spurs (thus confirming a diagnosis of MTS) in 5 patients that had normal DUS results. The primary advantages of MRV in the diagnosis of MTS include its noninvasiveness, ability to analyze all pelvic structures, and lack of operator dependence[13]. Additionally, MRV can estimate the degree of venous collateral flow, which greatly assists in the diagnosis of MTS[23]. Lastly, MRV can be performed without contrast, which is beneficial to patients with contraindications such as contrast allergies or renal impairment[8]. Conversely, the primary disadvantage of MRV in the diagnosis of MTS is that the vasculature above bifurcations has nonlaminar flow, which sometimes presents a confusing image[13]. Additionally, MRV studies are expensive, take significant time to perform, and are hard to perform on severely ill patients[18].
Figure 3.

Magnetic resonance venography with axial (A), sagittal (B), and coronal (C) reformatted images demonstrating May-Thurner syndrome anatomy with compression of the left common iliac vein (white arrowhead) by the right common iliac artery (black arrowhead).
Although MRV is a beneficial diagnostic option, a single MRV study may not be sufficient enough to diagnose MTS; McDermott et al[1] found that the degree of left iliac vein compression significantly differs in the same patient when undergoing repeated MRV imaging within a short period of time due to factors such as volume status or patient positioning[1,8]. Because MTS is a chronic condition with the development of permanent adhesions and intraluminal spurs, the degree of left iliac vein compression should not change significantly over time or depend on patient positioning. Thus, the sole finding of MTS anatomy on one MRV study may not be sufficient enough to confirm a diagnosis of MTS and more imaging studies may be necessary in order to reach a definitive diagnosis.
Contrast venography/hemodynamic studies
Contrast venography has widely been considered the gold standard diagnostic modality for MTS and has been utilized to confirm a diagnosis of MTS in several studies[5,6,12,24]. The procedure demonstrates the degree of iliac vein stenosis and can visualize any pelvic venous collaterals. Contrast dye must be injected in either the popliteal or femoral veins, as the standard method of dye injected into the dorsum of the foot is not adequate to fully visualize the iliac venous system[7,8]. Venography also allows for hemodynamic evaluation of MTS through pressure gradient measurements; iliofemoral stenosis is considered significant with a measurement of greater than 2 mmHg at rest and greater than 3 mmHg during periods of exercise. However, a nondiagnostic result does not rule out MTS because the patient is tested while at rest; exercise is usually required to increase blood flow to demonstrate a significant pressure gradient[4,7]. Although ascending venography almost always provides the evidence needed for a confirmed diagnosis of MTS, it is time consuming, invasive, cannot be performed in patients with widespread iliofemoral DVT and can result in post-procedural complications such as phlebitis[18].
IVUS
IVUS, using either a 12.5-MHz or 20-MHz ultrasound transducer, can accurately determine LCIV vessel size and morphology, and can verify the presence of MTS anatomy[10,25,26]. Knipp et al[6] utilized IVUS to confirm a diagnosis of MTS in 36 out of 58 patients; (62.1%) and defined the IVUS criteria for an MTS diagnosis as the lack of an evident venous lumen proximate to the IVUS catheter. In a small scale study conducted by Forauer et al[10], IVUS was not only used to confirm a diagnosis of MTS in all patients (n = 16), but information provided by the study was also found to influence the endovascular management of approximately 50% of the cases while also assisting with stent placement choice and accuracy. Moreover, in some studies, IVUS was found to have a higher success than venography in identifying obstructions[27-29]. Overall, IVUS is a useful modality in the diagnosis of MTS, although more studies are needed to truly evaluate its advantages over other diagnostic techniques.
CLINICAL PEARLS TO IMPROVE MTS DIAGNOSIS
There are several clinical pearls that can be considered in the diagnosis of MTS. For instance, if ultrasound is possible and allows for visualization of the iliac veins, provocative maneuvers (i.e., placing the patient in supine vs lateral positions or imaging during valsalva) may be performed to help demonstrate permanent vascular changes. These provocative maneuvers may also be used at the time of venography. Supine and prone CT or magnetic resonance imaging and cone beam CT at the time of venography may reveal the true state of common iliac vein. Additionally, due to the nil per os status for the procedure, the patient may be hypovolemic causing the IVC and iliac veins to easily flatten; in these cases, an IV bolus of 500-1000 cc of normal saline may be provided to the patient.
TREATMENT OPTIONS
Due to the mechanical nature of the obstruction, MTS patients generally do not respond well to conservative treatments[4]. In the past, surgical management of MTS has resulted in variable outcomes, as it is correlated with a high morbidity rate and has varied success in reestablishing venous patency[4,5]. Currently, the use of endovascular techniques in the treatment of MTS patients is considerably successful and carries less risk than invasive surgical treatments[8]. Common endovascular treatment options include catheter-directed thrombolysis, angioplasty, and ultimately stent placement[3,5,6,10,24]. Angioplasty has been found to be associated with low long-term patency rates, which indicates that the iliac vein compression may not be alleviated with solely the use of balloon angioplasty[30]. Additionally, stent placement is often necessary; however, stents are also associated with poor long-term patency rates, thus making diagnostic accuracy even more critical in the treatment of MTS patients as the choice to stent should be not be chosen lightly[8]. Overall, more studies are needed in order to fully evaluate the endovascular treatment that can provide the best outcome[8].
CONCLUSION
Prompt diagnosis is critical in MTS patients in order to avoid potential complications and the permanent consequences of intraluminal spur development. Currently, there is no diagnostic criteria in place to confirm a diagnosis of MTS. Imaging techniques such as CT, IVUS, MRV, and ascending venography have been useful in verifying a diagnosis; conversely, ultrasonography and pleythysmography, while useful in evaluating DVT and venous obstructions, cannot effectively be used to diagnose MTS and are best used in conjunction with other imaging techniques. Overall, the identification of MTS relies on both clinical and image findings, and more studies are needed in order to develop a comprehensive protocol for both.
Footnotes
Conflict-of-interest statement: The authors declared no conflicts of interest and have no financial disclosures.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: May 8, 2015
First decision: July 10, 2015
Article in press: September 16, 2015
P- Reviewer: Chan WP, Chen F S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
References
- 1.McDermott S, Oliveira G, Ergül E, Brazeau N, Wicky S, Oklu R. May-Thurner syndrome: can it be diagnosed by a single MR venography study? Diagn Interv Radiol. 2013;19:44–48. doi: 10.4261/1305-3825.DIR.5939-12.1. [DOI] [PubMed] [Google Scholar]
- 2.Heijmen RH, Bollen TL, Duyndam DA, Overtoom TT, Van Den Berg JC, Moll FL. Endovascular venous stenting in May-Thurner syndrome. J Cardiovasc Surg (Torino) 2001;42:83–87. [PubMed] [Google Scholar]
- 3.Oğuzkurt L, Ozkan U, Tercan F, Koç Z. Ultrasonographic diagnosis of iliac vein compression (May-Thurner) syndrome. Diagn Interv Radiol. 2007;13:152–155. [PubMed] [Google Scholar]
- 4.O’Sullivan GJ, Semba CP, Bittner CA, Kee ST, Razavi MK, Sze DY, Dake MD. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000;11:823–836. doi: 10.1016/s1051-0443(07)61796-5. [DOI] [PubMed] [Google Scholar]
- 5.Hurst DR, Forauer AR, Bloom JR, Greenfield LJ, Wakefield TW, Williams DM. Diagnosis and endovascular treatment of iliocaval compression syndrome. J Vasc Surg. 2001;34:106–113. doi: 10.1067/mva.2001.114213. [DOI] [PubMed] [Google Scholar]
- 6.Knipp BS, Ferguson E, Williams DM, Dasika NJ, Cwikiel W, Henke PK, Wakefield TW. Factors associated with outcome after interventional treatment of symptomatic iliac vein compression syndrome. J Vasc Surg. 2007;46:743–749. doi: 10.1016/j.jvs.2007.05.048. [DOI] [PubMed] [Google Scholar]
- 7.Shebel ND, Whalen CC. Diagnosis and management of iliac vein compression syndrome. J Vasc Nurs. 2005;23:10–17; quiz 18-19. doi: 10.1016/j.jvn.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Brazeau NF, Harvey HB, Pinto EG, Deipolyi A, Hesketh RL, Oklu R. May-Thurner syndrome: diagnosis and management. Vasa. 2013;42:96–105. doi: 10.1024/0301-1526/a000252. [DOI] [PubMed] [Google Scholar]
- 9.Cockett FB, Thomas ML, Negus D. Iliac vein compression.--Its relation to iliofemoral thrombosis and the post-thrombotic syndrome. Br Med J. 1967;2:14–19. doi: 10.1136/bmj.2.5543.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forauer AR, Gemmete JJ, Dasika NL, Cho KJ, Williams DM. Intravascular ultrasound in the diagnosis and treatment of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2002;13:523–527. doi: 10.1016/s1051-0443(07)61535-8. [DOI] [PubMed] [Google Scholar]
- 11.Ibrahim W, Al Safran Z, Hasan H, Zeid WA. Endovascular management of may-thurner syndrome. Ann Vasc Dis. 2012;5:217–221. doi: 10.3400/avd.cr.12.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel NH, Stookey KR, Ketcham DB, Cragg AH. Endovascular management of acute extensive iliofemoral deep venous thrombosis caused by May-Thurner syndrome. J Vasc Interv Radiol. 2000;11:1297–1302. doi: 10.1016/s1051-0443(07)61304-9. [DOI] [PubMed] [Google Scholar]
- 13.Wolpert LM, Rahmani O, Stein B, Gallagher JJ, Drezner AD. Magnetic resonance venography in the diagnosis and management of May-Thurner syndrome. Vasc Endovascular Surg. 2002;36:51–57. doi: 10.1177/153857440203600109. [DOI] [PubMed] [Google Scholar]
- 14.Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39:937–943. doi: 10.1016/j.jvs.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 15.Moreland NC, Ujiki M, Matsumura JS, Morasch MD, Eskandari MK, Pearce WH, Kibbe MR. Decreased incidence of left common iliac vein compression in patients with abdominal aortic aneurysms. J Vasc Surg. 2006;44:595–600. doi: 10.1016/j.jvs.2006.05.046. [DOI] [PubMed] [Google Scholar]
- 16.Oguzkurt L, Ozkan U, Ulusan S, Koc Z, Tercan F. Compression of the left common iliac vein in asymptomatic subjects and patients with left iliofemoral deep vein thrombosis. J Vasc Interv Radiol. 2008;19:366–370; quiz 371. doi: 10.1016/j.jvir.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Liu Z, Gao N, Shen L, Yang J, Zhu Y, Li Z, Si Y. Endovascular treatment for symptomatic iliac vein compression syndrome: a prospective consecutive series of 48 patients. Ann Vasc Surg. 2014;28:695–704. doi: 10.1016/j.avsg.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 18.Lamba R, Tanner DT, Sekhon S, McGahan JP, Corwin MT, Lall CG. Multidetector CT of vascular compression syndromes in the abdomen and pelvis. Radiographics. 2014;34:93–115. doi: 10.1148/rg.341125010. [DOI] [PubMed] [Google Scholar]
- 19.Whiteley M, Dos Santos S, Harrison C, Holdstock J, Lopez A. Transvaginal duplex ultrasonography appears to be the gold standard investigation for the haemodynamic evaluation of pelvic venous reflux in the ovarian and internal iliac veins in women. Phlebology. 2014:Epub ahead of print. doi: 10.1177/0268355514554638. [DOI] [PubMed] [Google Scholar]
- 20.Zhu QH, Zhou CY, Chen Y, Wang J, Mo HY, Luo MH, Huang W, Yu XF. Percutaneous manual aspiration thrombectomy followed by stenting for iliac vein compression syndrome with secondary acute isolated iliofemoral deep vein thrombosis: a prospective study of single-session endovascular protocol. Eur J Vasc Endovasc Surg. 2014;47:68–74. doi: 10.1016/j.ejvs.2013.09.030. [DOI] [PubMed] [Google Scholar]
- 21.Chung JW, Yoon CJ, Jung SI, Kim HC, Lee W, Kim YI, Jae HJ, Park JH. Acute iliofemoral deep vein thrombosis: evaluation of underlying anatomic abnormalities by spiral CT venography. J Vasc Interv Radiol. 2004;15:249–256. doi: 10.1097/01.rvi.0000109402.52762.8d. [DOI] [PubMed] [Google Scholar]
- 22.Oguzkurt L, Tercan F, Pourbagher MA, Kizilkilic O, Turkoz R, Boyvat F. Computed tomography findings in 10 cases of iliac vein compression (May-Thurner) syndrome. Eur J Radiol. 2005;55:421–425. doi: 10.1016/j.ejrad.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Gurel K, Gurel S, Karavas E, Buharalıoglu Y, Daglar B. Direct contrast-enhanced MR venography in the diagnosis of May-Thurner syndrome. Eur J Radiol. 2011;80:533–536. doi: 10.1016/j.ejrad.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 24.Binkert CA, Schoch E, Stuckmann G, Largiader J, Wigger P, Schoepke W, Zollikofer CL. Treatment of pelvic venous spur (May-Thurner syndrome) with self-expanding metallic endoprostheses. Cardiovasc Intervent Radiol. 1998;21:22–26. doi: 10.1007/s002709900205. [DOI] [PubMed] [Google Scholar]
- 25.Ahmed HK, Hagspiel KD. Intravascular ultrasonographic findings in May-Thurner syndrome (iliac vein compression syndrome) J Ultrasound Med. 2001;20:251–256. doi: 10.7863/jum.2001.20.3.251. [DOI] [PubMed] [Google Scholar]
- 26.Canales JF, Krajcer Z. Intravascular ultrasound guidance in treating May-Thurner syndrome. Tex Heart Inst J. 2010;37:496–497. [PMC free article] [PubMed] [Google Scholar]
- 27.McLafferty RB. The role of intravascular ultrasound in venous thromboembolism. Semin Intervent Radiol. 2012;29:10–15. doi: 10.1055/s-0032-1302446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raju S, Neglen P. High prevalence of nonthrombotic iliac vein lesions in chronic venous disease: a permissive role in pathogenicity. J Vasc Surg. 2006;44:136–143; discussion 144. doi: 10.1016/j.jvs.2006.02.065. [DOI] [PubMed] [Google Scholar]
- 29.Neglén P, Raju S. Intravascular ultrasound scan evaluation of the obstructed vein. J Vasc Surg. 2002;35:694–700. doi: 10.1067/mva.2002.121127. [DOI] [PubMed] [Google Scholar]
- 30.Kim JY, Choi D, Guk Ko Y, Park S, Jang Y, Lee do Y. Percutaneous treatment of deep vein thrombosis in May-Thurner syndrome. Cardiovasc Intervent Radiol. 2006;29:571–575. doi: 10.1007/s00270-004-0165-7. [DOI] [PubMed] [Google Scholar]


