Abstract
Excessive accumulation of lipids can lead to lipotoxicity, cell dysfunction and alteration in metabolic pathways, both in adipose tissue and peripheral organs, like liver, heart, pancreas and muscle. This is now a recognized risk factor for the development of metabolic disorders, such as obesity, diabetes, fatty liver disease (NAFLD), cardiovascular diseases (CVD) and hepatocellular carcinoma (HCC). The causes for lipotoxicity are not only a high fat diet but also excessive lipolysis, adipogenesis and adipose tissue insulin resistance. The aims of this review are to investigate the subtle balances that underlie lipolytic, lipogenic and oxidative pathways, to evaluate critical points and the complexities of these processes and to better understand which are the metabolic derangements resulting from their imbalance, such as type 2 diabetes and non alcoholic fatty liver disease.
Keywords: lipotoxicity, lipolysis, de novo lipogenesis, glyceroneogenesis, fatty liver, NAFLD, ectopic fat, HCC, SCD-1, saturated fat
1. Introduction
Fat accumulates in the presence of excessive caloric intake in order to be used as energy source at a later point in time. In presence of either high fat and/or carbohydrate intake, lipogenesis is stimulated and excess fat is stored as triglycerides (also named triacylglycerols, TAG). During fasting excess plasma free fatty acids (FFA), mainly released by the subcutaneous fat, accumulate in non-adipose tissues (e.g., liver, heart, pancreas and muscle) as triglycerides (TG), and can promote cell dysfunction and death [1]. This phenomenon has different effects dependent on the organ where fat accumulates [2]. Hence excess TG in the liver results in hepatic steatosis, fibrosis and non-alcoholic steatohepatitis (NASH) [3,4]; fat in the pancreas is associated with impaired insulin secretion, β-cell dysfunction and apoptosis [5,6]; excess intramyocardial fat leads to cardiomyopathy, coronary heart disease and sudden death [7,8]; in the skeletal muscles, intramyocellular TGs are associated with insulin resistance and impaired glucose uptake [1,9]. Alterations in lipogenesis and lipolysis are both causes and consequences of insulin resistance [1,7,10,11], since the imbalance in lipid metabolism is the primary cause of lipotoxicity.
In this manuscript we review the mechanisms that regulate lipid synthesis, lipolysis and oxidation in order to understand which are the “primum movens” of metabolic disorders, such as obesity, diabetes, non alcoholic fatty liver disease (NAFLD) and cardiovascular disease (CVD), including endothelial dysfunction, atherosclerosis and coronary heart disease (CHD).
2. Lipogenesis
TG synthesis is a crucial and strictly regulated process that occurs principally in the adipose tissue, but also in the liver, muscle, heart and pancreas. This pathway is used to maintain and control energy homeostasis by a continuous communication between oxidative tissues and peripheral organs, in particular adipose tissue.
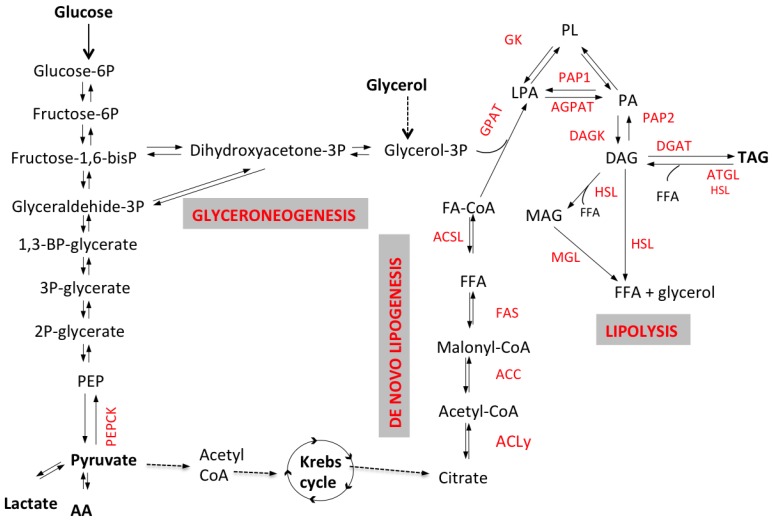
The process of fatty acid esterification into TAG involves the activation of FFA into Acyl-CoA through the formation of monacylglycerol (MAG) and diacyglycerol (DAG) by reacting with glycerol-3-phosphate (G3P) (Figure 1). Several hormones control lipogenesis including insulin that stimulates lipid synthesis and adipogenesis, while glucagon and catecholamines promote acetyl-CoA carboxylase (ACC) phosphorylation and inhibit fatty acids (FA) synthesis. Sources of G3P and Acyl-CoA are plasma glycerol and FFA, but these substrates may also be synthesized de novo. The contribution of glyceroneogenesis and de novo lipogenesis to hepatic TG synthesis is significant, particularly in conditions of insulin resistance, and might be a target for drug intervention. Below we discuss the different pathways involved in lipogenesis and how they are altered in metabolic diseases, particularly NAFLD and type 2 diabetes (T2DM).
Figure 1.
Schematic representation of lipolytic and lipogenic pathways. Triacyglycerol (TAG) synthesis requires the activation of free fatty acids (FFA) into Acyl-CoA by enzyme acyl-CoA synthetase. FFA-CoA and G3P are transformed via acylation, by glycerol-3-phosphate acyltransferase (GPAT) and acylCoA acylglycerol-3-phosphate acyltransferases (AGPAT), to phosphatidic acid (PA); then, after a dephosphorylation by phosphohydrolase (PAP2), diacylglycerols (DAG) are formed. Diacylglycerol acyltransferase (DGAT) catalyzes the conversion of DAG into TAG. In the adipocyte, G3P might come either from glycolysis or from non-carbohydrate substrates via the enzyme phosphoenolpyruvate carboxykinase (PEPCK), through a process named glyceroneogenesis. In the liver G3P can also be synthesized from plasma glycerol. De novo fatty acids synthesis (also referred to as de novo lipogenesis or DNL) occurs in the cytoplasm of various cells (e.g., adipocytes and hepatocytes) where citric acid is converted to acetyl-CoA by ATP-citrate lyase (ACL) and subsequently to malonyl-CoA by acetyl-CoA carboxylase (ACC). DNL occurs mainly in the liver, but it might occur in adipose tissue as well, although with low rates. This process requires the two enzymes ATP-citrate lyase (ACL), acetyl-CoA carboxylase (ACC) and the multi-enzymatic complex fatty acid synthase (FAS). G3P can be synthesized directly from non-carbohydrate substrates such as pyruvate, lactate or amino acids in oxaloacetate, that is converted to G3P either directly from phoenolpyruvate (PEP), via the key enzyme phosphoenolpyruvate carboxykinase (PEPCK), or through synthesis of dihydroxyacetone (DHA). TAG catabolism (i.e., lipolysis) involves several lipases, adipose triglyceride lipase (ATGL), hormone-sensitive lipase (HSL) and monoacylglycerol lipase (MGL) and produces the release of three free fatty acids (FFA) and one glycerol molecule.
2.1. Glycerol-3-Phosphate (G3P) Synthesis and Glyceroneogenesis
The first step of FFA esterification is the reaction with G3P. In adipose tissue the main source of G3P is glucose via glycolysis, since the activity of glycerokinase (GK), the enzyme that transforms glycerol into G3P, is low. This process is stimulated by insulin that promotes the uptake of glucose into the cell but also the transformation of dihydroxyacetone-3P (DHAP) into G3P by glycerophosphate dehydrogenase (Figure 1) and finally the reaction with FFA to synthesize TAG.
G3P can also be synthesized from non-carbohydrate substrates such as pyruvate, lactate or amino acids through glyceroneogenesis that plays a significant role both in adipose tissue and the liver [12] (Figure 1). Since the liver expresses GK, it has been thought that during lipogenesis the main substrate for TG synthesis was plasma glycerol. Studies analyzing plasma very low density lipoprotein (VLDL)-TG composition after ingestion of deuterated water (used as precursor of glyceroneogenesis) have shown that, during the synthesis of TAG, the liver utilizes mainly glycerol derived from glyceroneogenesis (over 54%), while the rest of the glycerol derives either from plasma glycerol (30%) or from plasma glucose through glycolysis (12%) [13]. Thus, glyceroneogenesis is an important pathway in TAG synthesis, while it is likely that the liver utilizes circulating glycerol as gluconeogenic substrate rather than using it for TAG synthesis. Hepatic gluconeogenesis and glyceroneogenesis have the synthesis of glyceraldehyde-3P (Figure 1) in common. We have shown that FFA and visceral fat accumulation are both associated with increased gluconeogenesis, and it is likely that glyceroneogenesis is also increased thus explaining the positive correlation between hepatic and visceral fat [14]. Thiazolidinediones decrease hepatic fat and gluconeogenesis [15,16,17] and promote adipose tissue glyceroneogenesis and TAG re-esterification [18]. The activation of these pathways explains the increase in subcutaneous fat and the decrease in hepatic and visceral fat observed after thiazolidinediones treatment [15,16]. However, data on this topic are still limited and more studies are needed.
2.2. De Novo Lipogenesis
TGs are synthesized either from circulating FFA derived from the diet, peripheral lipolysis or de novo lipogenesis (DNL). DNL occurs primarily in the liver and mostly after a high-carbohydrate meal when only part of the carbohydrates are stored as hepatic glycogen while the excess is converted to fatty acids and TAG [19]. During glycolysis citric acid is converted to acetyl-CoA, malonyl-CoA and palmitate, the first fatty acid synthesized (Figure 1). Other fatty acids are then produced through different mechanisms, e.g., stearic acid by elongation of palmitic acid, palmitoleic acid and oleic acid by desaturation of palmitic and stearic acid respectively.
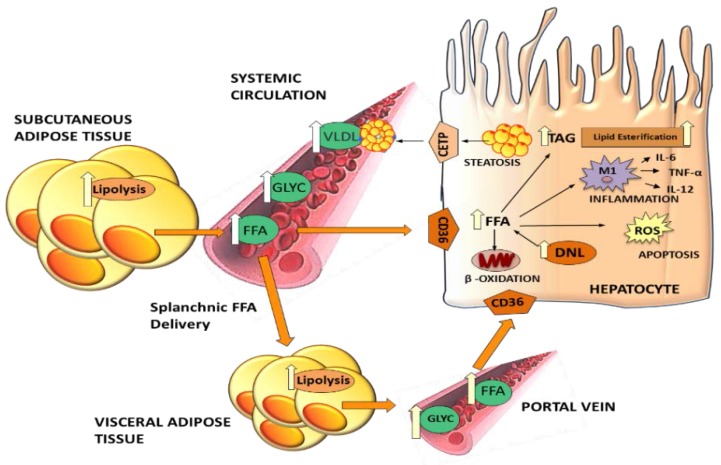
Contribution of DNL to the TAG pool is crucial in the balance between lipolysis and lipogenesis; however, the contribution of DNL to TAG synthesis is still unknown, mainly because it is difficult to measure it in vivo in humans. Published data indicate that increased DNL rates contribute to excess hepatic TAG synthesis and deposition, causing NAFLD [20]. The rate of de novo synthesis of palmitate in humans has been measured using the deuterated water technique [20]. DNL contributes to 10%–35% of the total VLDL-TG pool [21], being higher in overweight compared to lean subjects and in general in insulin resistant states, including NAFLD [20,22,23,24]. Moreover, higher rates of DNL are associated with high postprandial glucose and insulin concentrations [21,25], inflammation, oxidative stress and macrophage infiltration [26] (Figure 2).
Figure 2.
Effects of increased lipolysis on liver dysfunction. Excess lipolysis results in high free fatty acid (FFA) flux into the liver, where FFAs cause steatosis and exert lipotoxic effects. Triglycerides (TAG) synthetized in the liver are secreted into the plasma circulation as very low density lipoproteins (VLDL) causing dyslipidemia. Visceral fat has a preferential role in hepatic fat accumulation since released FFA reach the liver via the portal vein. Also increased hepatic de novo lipogenesis (DNL), inflammation and oxidative stress contribute to liver damage and hepatocyte dysfunction.
Possible mechanisms that explain increased hepatic DNL are the activation of the transcription factors Sterol Response Element Binding Protein 1c (SREBP-1c) and Carbohydrate Response Element Binding Protein (ChREBP). SREBP-1c and ChREBP regulate the expression of the key lipogenic genes acetyl-CoA carboxylase (ACC), fatty acid synthetase (FAS), acetyl-CoA synthetase (ACSS) and ATP-citrate lyase (ACL) [27,28]. SREBP-1c seems to be the predominant regulator of DNL in the liver but not in adipose tissue. In contrast, ChREBP regulates DNL in adipocytes where, unlike in liver cells, it has beneficial metabolic effects since it improves insulin sensitivity, enhances glucose transporter-2 (GLUT2) receptor expression and glucose uptake [29]. Glucose stimulates ChREBP and Liver X Receptor α (LXRα) expression and gene transcription of ACL, FAS, stearoyl-CoA desaturase-1 (SCD-1) [30]. Insulin stimulates lipogenesis through the SREBP-1c expression [31,32] and lack of its activation has been found to be associated with an increase in insulin induced gene (INSIG-1) mRNA and proteins [33].
Adipose tissue DNL is extremely low, both in lean and obese subjects [34], but it can be involved in the dysregulation of metabolic functions of adipose tissue. In the adipose tissue of morbid obese subjects undergoing bariatric surgery, a low expression of lipogenic genes (i.e., ACC, ACSS and ACL) has been associated with a better outcome and improvement of anthropometric variables after surgery [35].
It is becoming evident that DNL is a possible target for metabolic diseases including NAFLD. Drugs like pioglitazone, a peroxisome proliferator-activated receptor gamma (PPARγ) agonist, and liraglutide, a glucagon like peptide 1 receptor agonist have been shown to reduce liver triglyceride and hepatic steatosis also through reduction of DNL [36,37].
2.3. Hepatic TG Secretion as Very Low Density Lipoproteins (VLDL)
Hepatic TGs need to be incorporated into VLDL to be secreted in the systemic circulation; alternatively, they are stored in hepatocytes as lipid droplets (Figure 2). Increased hepatic secretion and impaired clearance of VLDL are associated with high plasma concentrations of TG and low density lipoproteins (LDL) and with decreased concentrations of high density lipoprotein (HDL). High plasma TG and LDL and low HDL are well established risk markers of metabolic syndrome, T2DM [38] and CVD, like the development of coronary heart disease and cardiomyopathy [39]. The enzyme that catalyzes TG synthesis is diacylglycerol acyltransferase (DGAT) (Figure 1) and it exists in mammals in two forms, DGAT1 and DGAT2. DGAT1 is expressed ubiquitously, but mainly in the small intestine, muscle and mammary glands, with low levels found in the liver and adipose tissue; DGAT2 is primarily expressed in the liver and adipose tissue [40]. Although both enzymes catalyze similar reactions and esterify diacylglycerol (DAG) into triacylglycerol, their predominant location influences their metabolic effects. Hence DGAT1 is involved in intestinal lipid absorption and chylomicron formation, while DGAT2 is involved in the synthesis of hepatic TG [40,41]. An impairment in DGAT2 activity results in an increase in hepatic DAG accumulation (Figure 1), making the hepatocytes more susceptible to injury by oxidative stress and inflammatory processes, and suggesting a possible contribution of DAG to the development of NAFLD and progression from simple steatosis to NASH [42]. In subjects with metabolic NAFLD, VLDL secretion is often normal or upregulated indicating that this is not the primary mechanism for the development of liver steatosis [43,44,45]. Indeed it seems that VLDL secretion reaches a plateau indicating a sort of saturation [43]. However, subjects with TM6SF2 mutation are more prone to develop NAFLD/NASH due to a genetic defect in VLDL secretion [46], thus they have reduced plasma concentrations of TG and lipoproteins, despite fatty liver, but they are protected against cardiovascular diseases [47].
3. Lipolysis
Lipolysis is a catabolic pathway that promotes mobilization of metabolic fuel from adipose to peripheral tissues in response to appropriate energy demands. Lipolysis occurs mainly in the adipose tissue. The major determinant of total FFA release is total fat, while gender is not as important. Since fat accumulates mainly in subcutaneous adipose tissue (SAT), this is the main contributor to plasma FFA [48]. The amount of visceral adipose tissue (VAT) is small compared to total SAT, although it may reach more than 38% of the total fat [5], thus its contribution to systemic FFA is minimal.
Lipolysis involves the hydrolysis of TAG that results in the release of fatty acids (FA) and glycerol into the circulation (Figure 1 and Figure 2). TAG hydrolysis requires different steps through the action of lipases (Figure 1). Several lipases have been discovered in the last 20 years. The first step, TAG hydrolysis into DAG, is obtained by adipose triglyceride lipase (ATGL) and results in the release of one fatty acid (Figure 1). Subsequently, DAG are converted by the enzyme monoacyglycerol lipase (MGL) into monoacylglycerols (MAG) with the release of one FFA or are completely hydrolyzed by hormone-sensitive lipase (HSL) with the release of two FFAs and one glycerol.
Adipose triglyceride lipase. ATGL is a member of the patatin-like phospholipase family, also named PNPLA2. ATGL is present in several cell types and is localized on lipid droplets’ surface and in the cytosol. It is activated by fasting, glucocorticoids and peroxisome proliferator-activated receptor (PPAR) agonists and exerts its action preferentially in adipose tissue and in presence of a co-activator protein named comparative gene identification-58 (CGI-58) [49,50]. ATGL is also present in oxidative tissues such as the liver, muscle and heart but here it explicates its action in a different way [51,52,53]. It has been hypothesized that hepatic ATGL might be involved in partitioning and routing TG, either promoting FFA release and oxidation or synthesis of VLDL [54]. Overexpression and improvement of hepatic ATGL activity is associated with increased TG turnover and FFA oxidation while hepatic ATGL deficiency is associated with steatosis [54,55]. However, the role of ATGL is still controversial. Although ATGL knockout mice developed hepatic steatosis and had altered levels of hepatic enzymes ALT/AST they had low inflammation compared to wild type mice indicating a possible protective role of the lack of hepatic ATGL against progression to NASH [53,55,56]. Muscle ATGL also has a crucial role in the activation of lipolysis and the prevention of intramuscular lipid accumulation. Exercise and physical activity increase ATGL expression in the muscle, promoting fatty acid utilization and oxidation [50]. A recent study has shown that in the heart, mice overexpressing ATGL are protected against cardiac steatosis and development of cardiac dysfunction [57]. These results suggest a different action of ATGL in non-adipose tissues, but more investigations are necessary to better understand the real functions of this lipase.
Monoacyglycerol lipase (MGL). Another important lipase is MGL that catalyzes the last step of lipolysis, i.e., the transformation of MAG, derived either from TG extracellular hydrolysis (via lipoprotein lipase, LPL), or TG intracellular hydrolysis into one FFA and one glycerol (Figure 1). MGL is ubiquitous in tissues (i.e., it is present in adipose tissue, muscle, liver and heart) but the highest expression is shown in adipose tissue. MGL acts on MAG coming from different sources, intracellular and extracellular TG hydrolysis but also phospholipid hydrolysis.
Hormone-sensitive lipase. HSL is an intracellular neutral lipase capable of hydrolyzing several lipid esters including TG, DAG, MAG, and cholesteryl esters, as well as other lipid and water soluble substrates [58]. However, the main activity of HSL is to hydrolyze DAG into MAG or completely with release of FFAs (Figure 1). HSL is activated mainly by β-adrenergic stimulus and inactivated by insulin, but it needs to be phosphorylated and translocated into lipid droplets to explicate its activity. Early studies in the 1960s concluded that HSL was the rate-limiting enzyme for TG hydrolysis but subsequent studies in knockout HSL mice contributed to elucidate the role of this enzyme. HSL-deficient mice were able to efficiently hydrolyze TG [59], showed no increased TG accumulation in either adipose tissue or liver but had an increased accumulation of DAG that interfered with normal cell metabolism and function [60].
4. Insulin Resistance and Lipolysis
The secretions of several hormones, i.e., catecholamines, glucagon and insulin, are altered in insulin resistant states. These hormones are important since they control lipolysis through direct or indirect pathways. Catecholamines exert the most potent action to promote this catabolic pathway and stimulate lipolysis [61,62]. Glucagon also acts as a lipolytic hormone that stimulates breakdown of triglycerides from lipid droplets [63]. Insulin exerts the opposite action, promoting adipogenesis and inhibiting lipolysis [64]. Higher levels of insulin in the blood are observed in insulin resistant subjects since there is a greater demand of insulin secretion by the beta cells to facilitate peripheral glucose uptake [64].
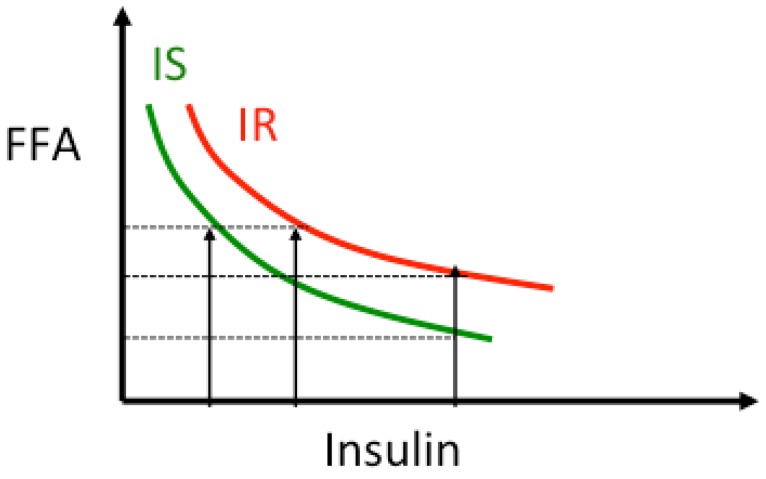
Insulin resistance is often present at the levels of all organs, muscle, liver, heart and adipose tissue, where insulin promotes FA esterification and synthesis of TAG. In addition, insulin suppresses adipose tissue lipolysis and the release of free fatty acid (FFA). The dose-response curve of FFA vs. insulin follows a hyperbolic curve [65]. As subjects become more insulin resistant at the level of adipose tissue the curve shifts to the right indicating that for the same insulin levels plasma FFA are higher (Figure 3). In this condition elevated plasma FFA reduce basal and insulin-stimulated muscle glucose uptake by inhibiting insulin signaling [9]. FFA decrease muscle ATP synthesis [66] and nitric oxide production [67], and impair insulin-stimulated activation of phosphoinositol-3 kinase (PI3K), pyruvate dehydrogenase kinase-isozyme 1 (PDK1), RAC-alpha serine/threonine-protein kinase (also known as proto-oncogene c-AKT), and endothelial nitric oxide synthase (eNOS) [67]. Moreover, high FFA are associated with increased cellular levels of diacylglycerol (DAG), the first step of TAG synthesis (Figure 1). Other lipid metabolites are increased in insulin resistant states, e.g., ceramide, and long-chain fatty acyl-coenzyme A (CoA), and activate transcription factors such as nuclear factor-κB (NF-κB) and inflammatory processes [68].
Figure 3.
Relationship insulin-lipolysis. As insulin concentration increases, lipolysis, and thus plasma free fatty acids (FFA) concentration, is suppressed following a non-linear curve [65,69,70]. In presence of insulin resistance the curve is shifted to the right indicating that for the same insulin levels lipolysis is less suppressed and circulating FFA levels are higher. The product FFA × Insulin is used as an index of adipose tissue-insulin resistance.
Adipose tissue insulin resistance index (Adipo-IR) has been developed to evaluate the degree of antilipolytic effect of insulin. Considering the hyperbolic relationship between FFA and insulin, Adipo-IR is calculated as the product of FFA × insulin [14,65] or as the product of rate of lipolysis × insulin [69,70]. Often FFA concentrations are not increased in the fasting state in insulin resistant subjects [63], but because of higher insulin concentrations the dose response curve is shifted to the right (as shown in Figure 3) [63,64]. On the other hand, suppression of lipolysis at higher insulin levels, e.g., after a glucose load, a meal test or during insulin infusion, is greater in insulin sensitive than insulin resistant subjects (Figure 3). Similar results were observed in non obese patients with NAFLD compared to matched controls [69].
In subjects with insulin resistance, e.g., obese, type 2 diabetes, NAFLD etc., the Adipo-IR has been found to be increased proportionally to visceral and hepatic fat [3]. Patients with abdominal and ectopic fat accumulation are “metabolically abnormal” compared to subjects with similar total body fat [71], they are more resistant to the antilipolytic effect of insulin with increased fasting lipolysis, but similar FFA concentrations, and impaired suppression of palmitate release during insulin infusion [71].
Excess FFA release not only causes peripheral insulin resistance [68], but also increases insulin secretion and impairs beta cell function [64,72]. Kashyap et al. have shown that chronic (48 h) intravenous infusion of an intralipid emulsion of essential saturated and unsaturated fatty acids plus heparin induces peripheral insulin resistance and stimulates insulin secretion in subjects without a family history of diabetes (FHD) while it markedly impairs insulin secretion in subjects with FHD [72]. The same type of response was observed in human islets incubated with fatty acids [73].
5. Dysfunctional Adipose Tissue: Accumulation and Remodeling
Adipose tissue expansion is a dynamic process that occurs in obesity, but is not always associated with pathological processes [74]. Subcutaneous fat is the main site of fat accumulation but visceral adipocytes are more resistant to the antilipolytic effect of insulin and catecholamines [75,76]. Visceral adipocytes are more lipolytic than subcutaneous adipocytes when incubated with different concentrations of norepinephrine, proportionally to the hepatic fat content [75]. Visceral fat (VF), more than subcutaneous fat, is associated with metabolic abnormalities including insulin resistance and lipotoxicity through the increased release of cytokines and decreased release of adiponectin. For example, visceral adipocyte diameter is higher in patients with more severe NAFLD and was found increased with serum levels of ALT and C- reactive protein [45]. Moreover, VF releases FFA directly into the portal vein and they are, therefore, cleared mainly by the liver [3,5]. Subjects with visceral fat have higher postprandial FFA and are at a higher risk of NAFLD and hepatic insulin resistance [14] (Figure 2).
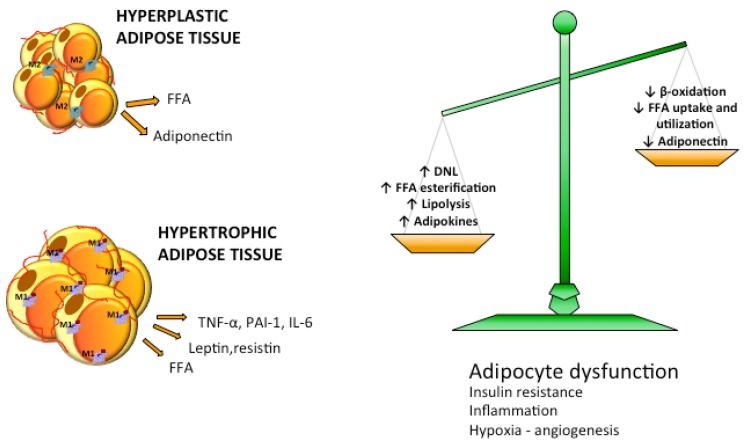
During adipose tissue expansion adipocytes become either hyperplastic, when their number increases through adipogenesis, or hypertrophic, when their size increases via lipogenesis [77] (Figure 4). Adipocytes act both as energy storage and as endocrine organ, being able to produce and release hormones, such as leptin, that is involved in the regulation of appetite; adiponectin, implicated in fatty acid oxidation and insulin action; cytokines like IL6 and tumor necrosis factor-α (TNF-α) that are involved in the regulation of lipolysis and can activate the complement system and vascular homeostasis [78,79,80] (Figure 4). Adipocyte cell size correlates positively with secretion of proinflammatory adipocytokines, e.g., leptin, inteleukin 6 and 8 (IL-6, IL-8), and monocyte chemoattractant protein-1 (MCP-1), as shown by data from cultured adipocytes [81]. In humans, visceral adipocyte size correlates directly with leptin [45] and inversely with adiponectin [82]. Adipose tissue expansion is regulated by storage-related genes like DGAT2, SREBP1c and cell death activator (CIDEA). A hypercaloric diet upregulates lipogenic genes in the adipose tissue [71]. Interestingly it has been shown that when the regulation of these genes in subcutaneous tissue is defective, the subjects tend to accumulate more visceral and ectopic fat [83].
Figure 4.
Imbalance in lipid metabolism causes increased efflux of FFA to adipose tissue. Reduced free fatty acids (FFA) utilization and β-oxidation and increased lipogenic and lipolytic pathways lead to overflow of FFA in the circulation. Adipose tissue activates adipogenesis and increases the number of adipocytes becoming hyperplastic or enlarges adipocyte size becoming hypertrophic. Hyperplastic adipose tissue is normally metabolically healthy while hypertrophic adipose tissue is characterized by dysfunctional adipocytes, insulin resistance, hypoxia and inflammation.
Some obese subjects preserve insulin sensitivity and lipid homeostasis and they are called “metabolically healthy obese” or MHO [71,84]. It has been demonstrated that adipose tissue morphology, more than the total amount of fat, plays an important role in the worsening of glucose and lipid metabolism [79]. Thus, in “metabolically healthy obese” adipocytes tend to be smaller than in obese insulin resistant subjects [85,86], where adipose tissue hypertrophy is accompanied by hypoxia, overproduction of pro-inflammatory cytokines, cellular fibrosis and macrophage infiltration [84,87,88] (Figure 4). Non-obese individuals at risk of T2DM are more prone to develop an obese phenotype with dysregulated adipose tissue, hypertrophic enlargement of adipocytes and reduced circulating adiponectin levels and glucose transporter-4 (GLUT4) expression for glucose uptake [89]. A recent study performed in 29 young healthy men has proposed that adipocyte size is predictive of the response to excess energy intake and could play a role in insulin resistance and inflammatory answer of adipose tissue [86]. Unexpectedly they showed that lean subjects with smaller fat cells responded to 8 weeks excess energy and lipid intake with a rapidly and not protective remodeling, developing insulin resistance, expansion of subcutaneous fat and up regulation of inflammatory markers. In contrast participants with larger subcutaneous adipocytes developed less insulin resistance and ectopic/visceral fat accumulation, probably due to a reduced expandability of these cells [86].
Adipocytes are among the most insulin-sensitive cells. When adipocytes become dysfunctional they become resistant to the anti-lipolytic effect of insulin resulting in a huge increase in the release of FFA and adipokines such as TNF-α and monocyte chemoattractant protein-1 (MCP-1) that play a key role in the development and maintenance of insulin resistance status. TNF-α induces insulin resistance in adipose tissue by altering the normal insulin signaling pathway, stimulating adipocytes lipolysis, decreasing insulin receptor substrate-1 (IRS-1) activity and its substrate phosphorylation and decreasing glucose transporter GLUT4 synthesis and membrane translocation. TNF-α leads to insulin resistance also in non-adipose tissues such as liver and muscle and promote FA mobilization from adipose tissue to oxidative tissues [90]. MCP-1 contributes to microphage infiltration in adipose tissue, insulin resistance and NAFLD [91] (Figure 4). Metabolomic analysis of subcutaneous adipose tissue found that several aminoacids, phosphocholines, ceramides and sphingolipids were increased in insulin resistant vs. insulin sensitive obese subjects and correlated with Adipo-IR [92].
6. Lipid Oxidation
The most important catabolic pathway for TAG and FA degradation is β-oxidation that occurs in mitochondria and produces the energy for homeostasis of cells and tissues (Figure 5). The oxidation of fatty acids occurs in particular during fasting state and carbohydrate starvation. In liver mitochondria, the acetyl-CoA produced during β-oxidation is converted to ketone bodies, i.e., acetoacetate, beta-hydroxybutyrate (BOH), and acetone. Ketone bodies are released and then taken up by other tissues such as the brain, muscle or heart where they are converted back to acetyl-CoA to serve as an energy source. Patients with fatty liver not only have increased VLDL-TG synthesis [43,44], but also increased β-oxidation and release of BOH [69]. However, obesity is also associated with increased levels of β-oxidation by the muscles and heart due to elevated circulating concentrations of FFAs that activate PPAR-α.
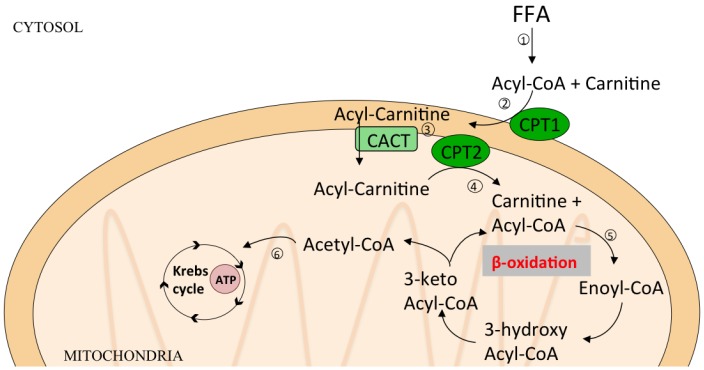
Figure 5.
Pathways of β-oxidation. β-oxidation is the catabolic pathway that occurs in mitochondria and produces energy from TG hydrolysis. (1) FFA are transformed to Acyl-CoA in cytosol; (2) protein Carnitine Palmitoyl Transferase-1 (CPT1) catalizes the transfer of the acyl group of a long-chain fatty acyl-CoA to carnitine to form acylcarnitines (mainly Palmitoylcarnitine); (3) Carnitine Acyltranferase (CACT) transfers acylcarnitine across outer mitochondrial membrane; (4) Carnitine Palmitoyl Transferase-2 (CPT2) reconverts acylcarnitine in acylCoA and carnitine; (5) Acyl-CoA enters in β-oxidation cycle and is degraded in several Acetyl-CoA molecules; (6) Acetyl-CoA enters in Krebs cycle to produce energy as Adenosine Triphosphate (ATP).
Glucose and hormones like insulin, glucagon and catecholamines that control lipolysis and lipogenesis modulate substrate availability for β-oxidation. Accelerated glucose metabolism could inhibit β-oxidation due to increased production of pyruvate that is transformed to malonyl-CoA, reducing the fatty acid catabolic pathway [93]. Also excessive FFA can impair mitochondrial function leading to abnormal FA oxidation. In this condition, the mitochondria tend to oxidize more glucose than lipids, even in resting condition. During a stress condition, when there is an increased energy demand, the cell is unable to switch from FA to carbohydrate oxidation. This determines the depletion of Krebs cycle intermediates and accumulation of ACC, thus contributing to insulin resistance (Figure 5).
7. Saturated or Unsaturated Fat?
Although unsaturated fatty acids were thought to be more susceptible to oxidative stress, recent work has instead demonstrated that a higher unsaturated/saturated fat ratio is protective against the development of metabolic diseases.
FFA plasma composition is determinant in maintenance of homeostasis. For example, palmitate, compared to other fatty acids, is more “toxic” [94]. Palmitate, but not oleate, impairs hepatic insulin signaling and induces apoptosis in hepatocyte cell lines and also impairs beta cell response. Oleate on the other hand seems to have a “protective” role since the coincubation of the two fatty acids reduces the “toxic” effect of palmitate [94]. This clearly indicates different metabolic signaling of single fatty acids and that different lipid bioactive species could shift the balance towards an adverse metabolic profile. Dietary polyunsaturated fatty acids (PUFA) and conjugated-linoleic acids (CLA) are lipid species that have been shown to have beneficial effects in maintaining lipid homeostasis, promoting loss of adiposity via increasing lipolysis and fatty acid oxidation and inhibiting lipogenesis [95]. These classes of FFA also exhibit anti-inflammatory and anti-oxidative properties via PPAR activation and reduced production of pro-inflammatory cytokines [96,97]. On the contrary saturated fatty acids (SFA) enhance production of reactive oxygen species and proinflammatory cytokines. SFA, in particular palmitic acid, activate mitochondrial depolarization, lead to apoptosis and suppress autophagy and lipid droplet production, which are both protective mechanisms to prevent lipotoxicity [98]. Moreover, SFA are precursors of ceramides that are bad substrates for the synthesis of cardiolipin, an important protein in the mitochondrial membrane. Impaired synthesis of cardiolipin results in increased membrane permeability and release of cytochrome C in the cytosol, causing also in that case apoptosis [99]. Thus, PUFA/SFA ratio has been used as a plasma biomarker of favorable lipid profile.
Animal studies have shown that an increased plasma PUFA/SFA ratio is associated with a favorable serum lipid profile and activation of hepatic enzymes involved in antioxidative pathways [100]. In hamsters, a diet with a high PUFA/SFA ratio prevented fat accumulation in white adipose tissue, increased expression of hepatic lipolytic enzymes, enhanced fatty acid β-oxidation and decreased hepatic SREBP-1c mRNA expression and plasma insulin levels [101]. These data were confirmed in a small group of subjects where an increase in PUFA versus SFA dietary intake was associated with reduced abdominal subcutaneous fat, in particular in obese subjects [102].
Plasmatic levels of free fatty acids are considered important parameters of lipolysis, since they reflect fat mobilization from adipose tissue to the circulation in response to energy demand. However, FFA composition and specific ratios are potential biomarkers in chronic metabolic diseases. The palmitate/linoleate ratio (16:0/18:2n6) is considered an index of DNL because it is a ratio of the first and main product of DNL, palmitate, and an essential fatty acid, linoleate, introduced by diet [103,104].
The ratios of palmitoleate/palmitate (16:1n7/16:0) and oleate/stearate (18:1n7/18:0) reflect enzyme activity of stearoyl-CoA desaturase (SCD-1), which add an unsaturation bond to fatty acid precursors palmitate or stearate [105,106,107,108,109,110]. Since SCD-1 activity is referred as the last stage of DNL, increase in either palmitoleate/palmitate (16:1n7/16:0) and/or oleate/stearate (18:1n7/18:0) ratios, especially in fasting state, were associated with an adverse metabolic profile, i.e., visceral fat accumulation, insulin resistance, and increased fasting and post-prandial plasma TG concentrations [104,109].
8. Lipotoxicity: Causes and Consequences
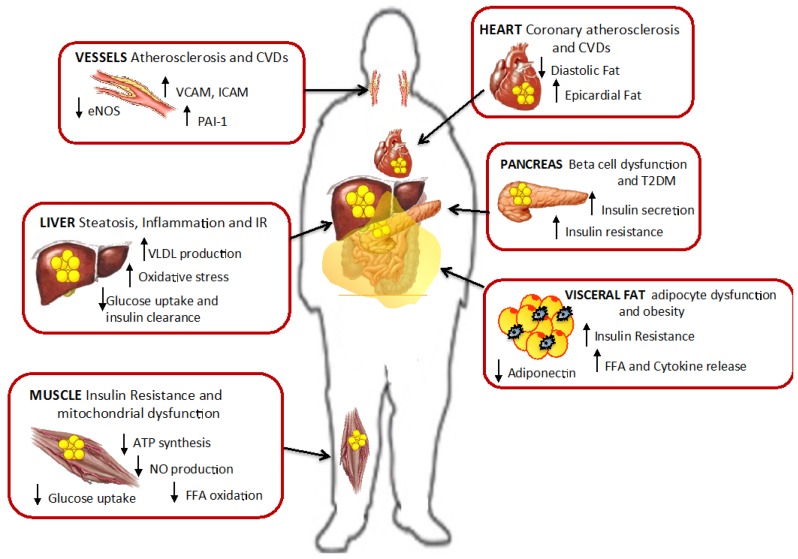
The imbalance of DNL, lipolysis and β-oxidation results in excess FFA released into the circulation that only in part are taken up by the adipose tissue and the rest by other tissues like the liver, muscle, heart and pancreas [2,111] (Figure 6). In presence of insulin resistance, adipose tissue capacity to metabolize these lipids is limited, so excess lipids also accumulate as ectopic fat and promote lipotoxicity [2]. Lipotoxicity triggers negative effects on multiple cellular processes including impaired insulin signaling [67,112], oxidative stress [113,114], alterations in local renin-angiotensin system [115], enhanced adrenergic sensitivity of vascular smooth muscle cells [116], and mitochondrial dysfunction [111].
Figure 6.
Ectopic fat accumulation and effect of lipotoxicity. Fat accumulation in non-adipose tissues promotes cell dysfunction, insulin resistance and inflammation in liver, muscle, pancreas and visceral fat. Also in vessels and heart lipotoxicity leads to increased risk for cardiovascular diseases and atherosclerosis. Modified from Gaggini M. et al. [2].
8.1. The Role of FFA in Lipotoxicity
Several studies have shown that elevation of plasma FFA not only stimulates fat accumulation but also induces cellular transformation by altering the expression of several genes associated with energy metabolism and inflammation, oxidative stress and cell apoptosis.
Elevated plasma FFAs promote peripheral and hepatic insulin resistance, reduce basal and insulin-stimulated glucose uptake in muscle by inhibiting insulin signaling [9]. In the skeletal muscle, fat accumulation reduces translocation of GLUT4 to the plasma membrane in response to insulin stimulation leading to the development of insulin resistance and T2DM [117]. Intramyocellular lipid content causes mitochondrial dysfunction and impaired glucose metabolism correlating with the severity of insulin resistance [118,119]. High FAs decrease muscle ATP synthesis [66], nitric oxide production [112], and impair insulin-stimulated activation of several genes, such as phosphoinositol-3 kinase (PI3K), pyruvate dehydrogenase kinase, isozyme 1, RAC-alpha serine/threonine-protein kinase (also known as proto-oncogene c-Akt), and endothelial nitric oxide synthase (eNOS) [112]. High plasma concentrations of FFAs are also associated with increased markers of endothelial activation, e.g., vascular cell adhesion molecule (VCAM) and intercellular adhesion molecule (ICAM), and increased markers of inflammation, such as plasminogen activator inhibitor-1 (PAI-1) and MCP-1, suggesting an increased risk for atherosclerotic cardiovascular disease [95].
The FFA lipotoxic effect is not limited to the muscle but also extends to other oxidative tissues such as the liver, heart and pancreas (Figure 6). Elevated FFAs stimulate hepatic TG synthesis and production of VLDL [43,44], hepatic insulin resistance, inflammation and fibrosis with the development of fatty liver disease and steatohepatitis [14,120]. Several studies have found a strong association between metabolic syndrome and NAFLD, liver damage, and hepatocellular carcinoma (HCC) [121,122,123,124]. NAFLD/NASH is the second leading etiology of HCC and is currently the most common cause of chronic liver disease [125]. The risk of cancer is high in NAFLD/NASH even in the absence of cirrhosis [126,127], and NAFLD/NASH is currently the most rapidly growing indication for liver transplantation (LT) in patients with HCC [128]. In particular, derangements in lipid metabolism lead not only to hepatic TG accumulation but also to lipotoxicity, oxidative stress and apoptosis [3,98,122,124,129,130]. Adipose tissue insulin resistance is likely to play a significant role since it is related to increased liver damage [124,131]. The mechanisms might be mediated by an increased synthesis of saturated fatty acids, ceramides, phosphatidylcholines, monoacyl-, diacyl- and triacyl-glycerols (MAG, DAG and TAG) and downregulation of lysophosphocholine (LPC), causing mitochondrial dysfunction, oxidative injury and apoptosis by the elevation of lipid peroxides and free radicals [132,133,134].
Ectopic fat can accumulate in the pancreas and induce β-cells dysfunction and dysregulated insulin secretion that is one of the main causes of the onset of T2DM [64]. In vitro studies on human β-cells showed that palmitic acid caused a dose-dependent reduction of glucose-stimulated insulin release and an increased cell death [73]. Development of β-cells lipotoxicity in non-diabetic subjects, but genetically predisposed to develop T2DM, was associated with impaired insulin release and secretion [72] (Figure 6).
Cardiac fat accumulates around the heart as pericardial or extrapericardial fat or as intramyocardial TG. Cardiac fat is associated with cardiomyocyte dysfunction and with the development of cardiac disease [7,135] coronary atherosclerosis and calcification [136,137]. Thus, it has been hypothesized that epicardial fat might be responsible for cardiac lipotoxicity, oxidative stress and insulin resistance [7]. However, lipolysis in the epicardial fat results in FFA release directly into the coronaries. Since FFA are the main cadiac energy substrate, epicardial fat, if not hypertrophic and dysfunctional, might have a non harmful role being an immediate source of energy.
8.2. Lipidomics and the Discovery of Harmful Lipids
Recent advances in omics technology have allowed the accurate identification of several lipid classes and their composition that are possible predictors of metabolic abnormalities. Among these lipids, increased intracellular concentrations of TG, diacylglycerols (DAG), glycerophosphocholine (GPC), phosphocholines (PC), ceramides and sphingomyelin have been implicated in the development of metabolic diseases including diabetes and non-alcoholic fatty liver disease [99,138,139,140,141,142,143,144,145,146,147].
DAGs are lipid intermediates that in normal conditions are converted to TAG or phospholipids (PL) (Figure 1). Recent studies have hypothesized that DAG might be implicated in the development of insulin resistance, inflammatory signaling and also dysmetabolic diseases [42,148,149]. The increment of intracellular DAG is able to activate protein kinase Cε (PKCε) that has an inhibitory effect on phosphorylation of insulin receptor substrate-2 (IRS2). Consequently DAGs promote the development of hepatic insulin resistance and hyperglycemia mainly through lack of suppression of gluconeogenesis. Initial studies in animal models were confirmed in obese subjects with NAFLD where hepatic DAG accumulation was positively correlated with hepatic insulin resistance [150]. Several analyses of liver tissue (both normal and steatotic livers) in human and murine specimens revealed a dramatic fold change in DAG composition, in particular an increase in DAG containing monounsaturated fatty acids [151].
Ceramides are molecules derived from sphingolipids, and they have been implicated in apoptosis [152]. Increased serum levels of ceramides were associated with insulin resistant states. However, there are more than 200 ceramides, so it is possible that not all lipids, but only some of them, are really implicated in cell damage and inflammation [68]. In particular, recent analysis of lipidomic data focused on the number of double bonds (i.e., degree of desaturation) as a possible way to find lipid biomarkers of disease [149].
9. Summary and Conclusions
A complex network of pathways, responding to several endogenous and exogenous stimuli, characterizes lipid metabolism. The alterations in adipogenesis, lipolysis and lipid oxidation are key factors in the development of metabolic disorders such as obesity, diabetes, NAFLD and CVD. Excess lipolysis results in excess release of FFAs into the circulation that are then taken up not only by adipose tissue but also by the liver, muscle, pancreas and/or heart, thus limiting excursions in plasma FFA concentrations and generating a lipotoxic profile in the organs. However, not all obese subjects are insulin resistant and have alterations in lipolysis and lipogenesis, and only those that develop cellular lipotoxicity are at risk of metabolic disorders.
The recent development of omics techniques allowed the discovery of plasma and tissue biomarkers of lipotoxicity. These are molecules that mark altered lipid mechanisms involved in the onset and/or progression of metabolic diseases, such as diacylglycerols (DAG), ceramides and long-chain fatty acids. The exposure to high FFA increases the production of these lipid intermediates and metabolites. These compounds are able to activate transcription factors involved in inflammatory processes and oxidative stress, leading to lipotoxicity. A lot of work still needs to be done and only the multi-omics approach, e.g., lipidomics, metabolomics, transcriptomics, genomics and fluxomics, will elucidate pathways that are still unclear and determine which molecules are implicated.
In conclusion, lipids appear to be key players in metabolic derangement, especially when they accumulate as visceral or ectopic fat. In this condition, lipids exert a lipotoxic action, causing cell dysfunction and organ damage. Extensive knowledge of mechanisms involved in lipid metabolism and its control is necessary to identify early biomarkers of cardio-metabolic diseases, new pharmacological strategies and to provide new behavioral lifestyle interventions.
Acknowledgments
We acknowledge funding from: FP7/2007–2013 under grant agreement n° HEALTH-F2-2009-241762 for the project “FLIP”; MIUR grant Progetto Bandiera “INTEROMICS”; MIUR grant Progetto Premiale “Environment, life style and cardiovascular diseases: from molecules to man”. CS is a recipient of a fellowship “Dottorato Pegaso Regione Toscana in Biochemistry and Molecular Biology”. MG is a recipient of a GILEAD fellowship to study metabolomics markers of liver disease.
Abbreviations
ACC (acetyl-CoA carboxylase); ACL (ATP-citrate lyase); Adipo-IR (adipose tissue insulin resistance index); AGPAT (acylCoA acylglycerol-3-phosphate acyltransferases); AKT1 (RAC-alpha serine/threonine-protein kinase); ALT (alanine transaminase); AMPK (AMP- Activate protein kinase); AST (aspartate transaminase); ATGL (adipose triglyceride lipase); ATP (Adenosine Triphosphate); CACT (Carnitine Acyltranferase); CEPT (Cholesteryl ester transfer protein); CGI-58 (gene identification-58); ChREBP (Carbohydrate Response Element Binding Protein); CIDEA (Cell death activator); CLA (conjugated-linoleic acids); CPT1 (Carnitine Palmitoyl Transferase1); DAG (Diacylglycerols); DAGK (diacylglycerol kinase); DGAT (diacylglycerol acyltransferase); DHAP (dihydroxyacetone-3-phosphate); DNL (De novo lipogenesis); eNOS (endothelial nitric oxide synthase); FAS (fatty acid synthetase); FFA (free fatty acids); G3P (Glycerol-3-phosphate); GLP-1 (glucagon like peptide 1); GLUT-2 and GLUT-4 (glucose transporter); GPAT (glycerol-3-phosphate acyltransferases); GPC (glycerophosphocholine); HCC (hepatocellular carcinoma); HDL (high density lipoprotein); HSL (hormone-sensitive lipase); ICAM (Intercellular Adhesion Molecule); INSIG-1 (insulin induced gene); IRS-1 and IRS-2 (insulin receptor substrate); LDL (low density lipoprotein); LPC (lysophosphocholine) LXRα (Liver X Receptor α); MAG (Monoacylglycerols); MCP-1 (Monocyte chemoattractant protein-1); MGL (monoacylglycerol lipase); MUFA (monounsaturated fatty acids); NAFLD (Non Alcoholic Fatty Liver Disease); NAFLD (nonalcoholic fatty liver disease); NASH (Non Alcoholic Steatohepatitis); PAI-1 (plasminogen activator inhibitor-1); PAP (phosphohydrolases); PC (phosphocholine); PDK1 (pyruvate dehydrogenase kinase-isozyme 1); PEP (phoenolpyruvate); PEPCK (phosphoenolpyruvate carboxykinase); PI3K (phosphoinositide 3-kinase); PKCε (Protein kinase C isoform ε); PL (phospholipids); PNPLA2 (patatin-like phospholipase); PPAR (peroxisome proliferator-activated receptor); PUFA (polyunsaturated fatty acids); SCD-1 (stearoyl-CoA desaturase-1); SFA (saturated fatty acids); SREBP-1c (Sterol Response Element Binding Protein 1c); T2DM (type 2 diabetes); TAG (Triacylglycerols); TNF-α (tumor necrosis factor-α); VCAM (vascular cell adhesion molecule); VLDL (very low density lipoprotein).
Author Contributions
Chiara Saponaro, Melania Gaggini and Fabrizia Carli searched the literature and wrote the first draft of the manuscript. Amalia Gastaldelli (primary contact) conceived this review and finalized the manuscript. All authors contributed important contents to the drafting of this review and approved the final version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest for this manuscript.
References
- 1.Morelli M., Gaggini M., Daniele G., Marraccini P., Sicari R., Gastaldelli A. Ectopic fat: The true culprit linking obesity and cardiovascular disease? Thromb. Haemost. 2013;110:651–660. doi: 10.1160/TH13-04-0285. [DOI] [PubMed] [Google Scholar]
- 2.Gaggini M., Saponaro C., Gastaldelli A. Not all fats are created equal: Adipose vs. Ectopic fat, implication in cardiometabolic diseases. Horm. Mol. Biol. Clin. Investig. 2015;22:7–18. doi: 10.1515/hmbci-2015-0006. [DOI] [PubMed] [Google Scholar]
- 3.Gaggini M., Morelli M., Buzzigoli E., DeFronzo R.A., Bugianesi E., Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013;5:1544–1560. doi: 10.3390/nu5051544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yki-Jarvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2:901–910. doi: 10.1016/S2213-8587(14)70032-4. [DOI] [PubMed] [Google Scholar]
- 5.Gastaldelli A. Visceral adipose tissue and ectopic fat deposition. In: Bray G.A., Bouchard C., editors. Handbook of Obesity. Volume 1. CRC Press; Boca Raton, FL, USA: 2014. pp. 237–248. [Google Scholar]
- 6.Lim E.L., Hollingsworth K.G., Aribisala B.S., Chen M.J., Mathers J.C., Taylor R. Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011;54:2506–2514. doi: 10.1007/s00125-011-2204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gastaldelli A., Morales M.A., Marraccini P., Sicari R. The role of cardiac fat in insulin resistance. Curr. Opin. Clin. Nutr. Metab. Care. 2012;15:523–528. doi: 10.1097/MCO.0b013e328358be7b. [DOI] [PubMed] [Google Scholar]
- 8.Gaborit B., Kober F., Jacquier A., Moro P.J., Cuisset T., Boullu S., Dadoun F., Alessi M.C., Morange P., Clement K., et al. Assessment of epicardial fat volume and myocardial triglyceride content in severely obese subjects: Relationship to metabolic profile, cardiac function and visceral fat. Int. J. Obes. 2012;36:422–430. doi: 10.1038/ijo.2011.117. [DOI] [PubMed] [Google Scholar]
- 9.Boden G., Lebed B., Schatz M., Homko C., Lemieux S. Effects of acute changes of plasma free fatty acids on intramyocellular fat content and insulin resistance in healthy subjects. Diabetes. 2001;50:1612–1617. doi: 10.2337/diabetes.50.7.1612. [DOI] [PubMed] [Google Scholar]
- 10.Schrauwen P., Hesselink M.K. Oxidative capacity, lipotoxicity, and mitochondrial damage in type 2 diabetes. Diabetes. 2004;53:1412–1417. doi: 10.2337/diabetes.53.6.1412. [DOI] [PubMed] [Google Scholar]
- 11.Boden G. Obesity, insulin resistance and free fatty acids. Curr. Opin. Endocrinol. Diabetes Obes. 2011;18:139–143. doi: 10.1097/MED.0b013e3283444b09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hanson R.W., Reshef L. Glyceroneogenesis revisited. Biochimie. 2003;85:1199–1205. doi: 10.1016/j.biochi.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 13.Kalhan S.C., Bugianesi E., McCullough A.J., Hanson R.W., Kelley D.E. Estimates of hepatic glyceroneogenesis in type 2 diabetes mellitus in humans. Metabolism. 2008;57:305–312. doi: 10.1016/j.metabol.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gastaldelli A., Cusi K., Pettiti M., Hardies J., Miyazaki Y., Berria R., Buzzigoli E., Sironi A.M., Cersosimo E., Ferrannini E., et al. Relationship between hepatic/visceral fat and hepatic insulin resistance in nondiabetic and type 2 diabetic subjects. Gastroenterology. 2007;133:496–506. doi: 10.1053/j.gastro.2007.04.068. [DOI] [PubMed] [Google Scholar]
- 15.Gastaldelli A., Miyazaki Y., Pettiti M., Santini E., Ciociaro D., Defronzo R.A., Ferrannini E. The effect of rosiglitazone on the liver: Decreased gluconeogenesis in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 2006;91:806–812. doi: 10.1210/jc.2005-1159. [DOI] [PubMed] [Google Scholar]
- 16.Belfort R., Harrison S.A., Brown K., Darland C., Finch J., Hardies J., Balas B., Gastaldelli A., Tio F., Pulcini J., et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N. Engl. J. Med. 2006;355:2297–2307. doi: 10.1056/NEJMoa060326. [DOI] [PubMed] [Google Scholar]
- 17.Sanyal A.J., Chalasani N., Kowdley K.V., McCullough A., Diehl A.M., Bass N.M., Neuschwander-Tetri B.A., Lavine J.E., Tonascia J., Unalp A., et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N. Engl. J. Med. 2010;362:1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tordjman J., Chauvet G., Quette J., Beale E.G., Forest C., Antoine B. Thiazolidinediones block fatty acid release by inducing glyceroneogenesis in fat cells. J. Biol. Chem. 2003;278:18785–18790. doi: 10.1074/jbc.M206999200. [DOI] [PubMed] [Google Scholar]
- 19.Hellerstein M.K. De novo lipogenesis in humans: Metabolic and regulatory aspects. Eur. J. Clin. Nutr. 1999;53(Suppl. 1):S53–S65. doi: 10.1038/sj.ejcn.1600744. [DOI] [PubMed] [Google Scholar]
- 20.Donnelly K.L., Smith C.I., Schwarzenberg S.J., Jessurun J., Boldt M.D., Parks E.J. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J. Clin. Investig. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Timlin M.T., Parks E.J. Temporal pattern of de novo lipogenesis in the postprandial state in healthy men. Am. J. Clin. Nutr. 2005;81:35–42. doi: 10.1093/ajcn/81.1.35. [DOI] [PubMed] [Google Scholar]
- 22.Flannery C., Dufour S., Rabol R., Shulman G.I., Petersen K.F. Skeletal muscle insulin resistance promotes increased hepatic de novo lipogenesis, hyperlipidemia, and hepatic steatosis in the elderly. Diabetes. 2012;61:2711–2717. doi: 10.2337/db12-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma W., Wu J.H., Wang Q., Lemaitre R.N., Mukamal K.J., Djousse L., King I.B., Song X., Biggs M.L., Delaney J.A., et al. Prospective association of fatty acids in the de novo lipogenesis pathway with risk of type 2 diabetes: The cardiovascular health study. Am. J. Clin. Nutr. 2015;101:153–163. doi: 10.3945/ajcn.114.092601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai D., Yuan M., Frantz D.F., Melendez P.A., Hansen L., Lee J., Shoelson S.E. Local and systemic insulin resistance resulting from hepatic activation of ikk-beta and nf-kappab. Nat. Med. 2005;11:183–190. doi: 10.1038/nm1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marques-Lopes I., Ansorena D., Astiasaran I., Forga L., Martinez J.A. Postprandial de novo lipogenesis and metabolic changes induced by a high-carbohydrate, low-fat meal in lean and overweight men. Am. J. Clin. Nutr. 2001;73:253–261. doi: 10.1093/ajcn/73.2.253. [DOI] [PubMed] [Google Scholar]
- 26.Bechmann L.P., Hannivoort R.A., Gerken G., Hotamisligil G.S., Trauner M., Canbay A. The interaction of hepatic lipid and glucose metabolism in liver diseases. J. Hepatol. 2012;56:952–964. doi: 10.1016/j.jhep.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 27.Shimano H., Yahagi N., Amemiya-Kudo M., Hasty A.H., Osuga J., Tamura Y., Shionoiri F., Iizuka Y., Ohashi K., Harada K., et al. Sterol regulatory element-binding protein-1 as a key transcription factor for nutritional induction of lipogenic enzyme genes. J. Biol. Chem. 1999;274:35832–35839. doi: 10.1074/jbc.274.50.35832. [DOI] [PubMed] [Google Scholar]
- 28.Dentin R., Pegorier J.P., Benhamed F., Foufelle F., Ferre P., Fauveau V., Magnuson M.A., Girard J., Postic C. Hepatic glucokinase is required for the synergistic action of chrebp and SREBP-1c on glycolytic and lipogenic gene expression. J. Biol. Chem. 2004;279:20314–20326. doi: 10.1074/jbc.M312475200. [DOI] [PubMed] [Google Scholar]
- 29.Herman M.A., Peroni O.D., Villoria J., Schon M.R., Abumrad N.A., Bluher M., Klein S., Kahn B.B. A novel chrebp isoform in adipose tissue regulates systemic glucose metabolism. Nature. 2012;484:333–338. doi: 10.1038/nature10986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Musso G., Gambino R., Cassader M. Recent insights into hepatic lipid metabolism in non-alcoholic fatty liver disease (NAFLD) Prog. Lipid. Res. 2009;48:1–26. doi: 10.1016/j.plipres.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 31.Schwarz J.M., Linfoot P., Dare D., Aghajanian K. Hepatic de novo lipogenesis in normoinsulinemic and hyperinsulinemic subjects consuming high-fat, low-carbohydrate and low-fat, high-carbohydrate isoenergetic diets. Am. J. Clin. Nutr. 2003;77:43–50. doi: 10.1093/ajcn/77.1.43. [DOI] [PubMed] [Google Scholar]
- 32.Shimomura I., Matsuda M., Hammer R.E., Bashmakov Y., Brown M.S., Goldstein J.L. Decreased IRS-2 and increased SREBP-1c lead to mixed insulin resistance and sensitivity in livers of lipodystrophic and ob/ob mice. Mol. Cell. 2000;6:77–86. doi: 10.1016/S1097-2765(05)00010-9. [DOI] [PubMed] [Google Scholar]
- 33.Boden G., Salehi S., Cheung P., Homko C., Song W., Loveland-Jones C., Jayarajan S. Comparison of in vivo effects of insulin on SREBP-1c activation and INSIG-1/2 in rat liver and human and rat adipose tissue. Obesity. 2013;21:1208–1214. doi: 10.1002/oby.20134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo Z.K., Cella L.K., Baum C., Ravussin E., Schoeller D.A. De novo lipogenesis in adipose tissue of lean and obese women: Application of deuterated water and isotope ratio mass spectrometry. Int. J. Obes. Relat. Metab. Disord. 2000;24:932–937. doi: 10.1038/sj.ijo.0801256. [DOI] [PubMed] [Google Scholar]
- 35.Garrido-Sanchez L., Vendrell J., Fernandez-Garcia D., Ceperuelo-Mallafre V., Chacon M.R., Ocana-Wilhelmi L., Alcaide J., Tinahones F.J., Garcia-Fuentes E. De novo lipogenesis in adipose tissue is associated with course of morbid obesity after bariatric surgery. PLoS ONE. 2012;7:e31280. doi: 10.1371/journal.pone.0031280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Armstrong M.J., Hull D., Guo K., Barton D., Hazlehurst J.M., Gathercole L.L., Nasiri M., Yu J., Gough S.C., Newsome P.N., et al. Glucagon-like peptide 1 decreases lipotoxicity in non-alcoholic steatophepatitis. J. Hepatol. 2015 doi: 10.1016/j.jhep.2015.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beysen C., Murphy E.J., Nagaraja H., Decaris M., Riiff T., Fong A., Hellerstein M.K., Boyle P.J. A pilot study of the effects of pioglitazone and rosiglitazone on de novo lipogenesis in type 2 diabetes. J. Lipid. Res. 2008;49:2657–2663. doi: 10.1194/jlr.M800165-JLR200. [DOI] [PubMed] [Google Scholar]
- 38.Krauss R.M. Lipids and lipoproteins in patients with type 2 diabetes. Diabetes Care. 2004;27:1496–1504. doi: 10.2337/diacare.27.6.1496. [DOI] [PubMed] [Google Scholar]
- 39.Van de Weijer T., Schrauwen-Hinderling V.B., Schrauwen P. Lipotoxicity in type 2 diabetic cardiomyopathy. Cardiovasc Res. 2011;92:10–18. doi: 10.1093/cvr/cvr212. [DOI] [PubMed] [Google Scholar]
- 40.Zammit V.A. Hepatic triacylglycerol synthesis and secretion: DGAT2 as the link between glycaemia and triglyceridaemia. Biochem. J. 2013;451:1–12. doi: 10.1042/BJ20121689. [DOI] [PubMed] [Google Scholar]
- 41.Yen C.L., Nelson D.W., Yen M.I. Intestinal triacylglycerol synthesis in fat absorption and systemic energy metabolism. J. Lipid Res. 2015;56:489–501. doi: 10.1194/jlr.R052902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Perry R.J., Samuel V.T., Petersen K.F., Shulman G.I. The role of hepatic lipids in hepatic insulin resistance and type 2 diabetes. Nature. 2014;510:84–91. doi: 10.1038/nature13478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adiels M., Taskinen M.R., Packard C., Caslake M.J., Soro-Paavonen A., Westerbacka J., Vehkavaara S., Hakkinen A., Olofsson S.O., Yki-Jarvinen H., et al. Overproduction of large vldl particles is driven by increased liver fat content in man. Diabetologia. 2006;49:755–765. doi: 10.1007/s00125-005-0125-z. [DOI] [PubMed] [Google Scholar]
- 44.Fabbrini E., Mohammed B.S., Magkos F., Korenblat K.M., Patterson B.W., Klein S. Alterations in adipose tissue and hepatic lipid kinetics in obese men and women with nonalcoholic fatty liver disease. Gastroenterology. 2008;134:424–431. doi: 10.1053/j.gastro.2007.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wree A., Schlattjan M., Bechmann L.P., Claudel T., Sowa J.P., Stojakovic T., Scharnagl H., Kofeler H., Baba H.A., Gerken G., et al. Adipocyte cell size, free fatty acids and apolipoproteins are associated with non-alcoholic liver injury progression in severely obese patients. Metabolism. 2014;63:1542–1552. doi: 10.1016/j.metabol.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 46.Mahdessian H., Taxiarchis A., Popov S., Silveira A., Franco-Cereceda A., Hamsten A., Eriksson P., van’t Hooft F. TM6SF2 is a regulator of liver fat metabolism influencing triglyceride secretion and hepatic lipid droplet content. Proc. Natl. Acad. Sci. USA. 2014;111:8913–8918. doi: 10.1073/pnas.1323785111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dongiovanni P., Petta S., Maglio C., Fracanzani A.L., Pipitone R., Mozzi E., Motta B.M., Kaminska D., Rametta R., Grimaudo S., et al. Transmembrane 6 superfamily member 2 gene variant disentangles nonalcoholic steatohepatitis from cardiovascular disease. Hepatology. 2015;61:506–514. doi: 10.1002/hep.27490. [DOI] [PubMed] [Google Scholar]
- 48.Mittendorfer B., Magkos F., Fabbrini E., Mohammed B.S., Klein S. Relationship between body fat mass and free fatty acid kinetics in men and women. Obesity. 2009;17:1872–1877. doi: 10.1038/oby.2009.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smirnova E., Goldberg E.B., Makarova K.S., Lin L., Brown W.J., Jackson C.L. ATGL has a key role in lipid droplet/adiposome degradation in mammalian cells. EMBO Rep. 2006;7:106–113. doi: 10.1038/sj.embor.7400559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haemmerle G., Lass A., Zimmermann R., Gorkiewicz G., Meyer C., Rozman J., Heldmaier G., Maier R., Theussl C., Eder S., et al. Defective lipolysis and altered energy metabolism in mice lacking adipose triglyceride lipase. Science. 2006;312:734–737. doi: 10.1126/science.1123965. [DOI] [PubMed] [Google Scholar]
- 51.Shaw C.S., Clark J.A., Shepherd S.O. HSL and ATGL: The movers and shakers of muscle lipolysis. J. Physiol. 2013;591:6137–6138. doi: 10.1113/jphysiol.2013.265199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huijsman E., van de Par C., Economou C., van der Poel C., Lynch G.S., Schoiswohl G., Haemmerle G., Zechner R., Watt M.J. Adipose triacylglycerol lipase deletion alters whole body energy metabolism and impairs exercise performance in mice. Am. J. Physiol. Endocrinol. Metab. 2009;297:E505–E513. doi: 10.1152/ajpendo.00190.2009. [DOI] [PubMed] [Google Scholar]
- 53.Brown J.M., Betters J.L., Lord C., Ma Y., Han X., Yang K., Alger H.M., Melchior J., Sawyer J., Shah R., et al. CGI-58 knockdown in mice causes hepatic steatosis but prevents diet-induced obesity and glucose intolerance. J. Lipid Res. 2010;51:3306–3315. doi: 10.1194/jlr.M010256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ong K.T., Mashek M.T., Bu S.Y., Greenberg A.S., Mashek D.G. Adipose triglyceride lipase is a major hepatic lipase that regulates triacylglycerol turnover and fatty acid signaling and partitioning. Hepatology. 2010;53:116–126. doi: 10.1002/hep.24006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu J.W., Wang S.P., Alvarez F., Casavant S., Gauthier N., Abed L., Soni K.G., Yang G., Mitchell G.A. Deficiency of liver adipose triglyceride lipase in mice causes progressive hepatic steatosis. Hepatology. 2011;54:122–132. doi: 10.1002/hep.24338. [DOI] [PubMed] [Google Scholar]
- 56.Fuchs C.D., Claudel T., Kumari P., Haemmerle G., Pollheimer M.J., Stojakovic T., Scharnagl H., Halilbasic E., Gumhold J., Silbert D., et al. Absence of adipose triglyceride lipase protects from hepatic endoplasmic reticulum stress in mice. Hepatology. 2012;56:270–280. doi: 10.1002/hep.25601. [DOI] [PubMed] [Google Scholar]
- 57.Pulinilkunnil T., Kienesberger P.C., Nagendran J., Sharma N., Young M.E., Dyck J.R. Cardiac-specific adipose triglyceride lipase overexpression protects from cardiac steatosis and dilated cardiomyopathy following diet-induced obesity. Int. J. Obes. 2013;38:205–215. doi: 10.1038/ijo.2013.103. [DOI] [PubMed] [Google Scholar]
- 58.Kraemer F.B., Shen W.J. Hormone-sensitive lipase: Control of intracellular tri-(di-)acylglycerol and cholesteryl ester hydrolysis. J. Lipid. Res. 2002;43:1585–1594. doi: 10.1194/jlr.R200009-JLR200. [DOI] [PubMed] [Google Scholar]
- 59.Osuga J., Ishibashi S., Oka T., Yagyu H., Tozawa R., Fujimoto A., Shionoiri F., Yahagi N., Kraemer F.B., Tsutsumi O., et al. Targeted disruption of hormone-sensitive lipase results in male sterility and adipocyte hypertrophy, but not in obesity. Proc. Natl. Acad. Sci. USA. 2000;97:787–792. doi: 10.1073/pnas.97.2.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Haemmerle G., Zimmermann R., Hayn M., Theussl C., Waeg G., Wagner E., Sattler W., Magin T.M., Wagner E.F., Zechner R. Hormone-sensitive lipase deficiency in mice causes diglyceride accumulation in adipose tissue, muscle, and testis. J. Biol. Chem. 2002;277:4806–4815. doi: 10.1074/jbc.M110355200. [DOI] [PubMed] [Google Scholar]
- 61.Gastaldelli A., Coggan A.R., Wolfe R.R. Assessment of methods for improving tracer estimation of non-steady-state rate of appearance. J. Appl. Physiol. 1999;87:1813–1822. doi: 10.1152/jappl.1999.87.5.1813. [DOI] [PubMed] [Google Scholar]
- 62.Natali A., Gastaldelli A., Galvan A.Q., Sironi A.M., Ciociaro D., Sanna G., Rosenzweig P., Ferrannini E. Effects of acute alpha 2-blockade on insulin action and secretion in humans. Am. J. Physiol. 1998;274:E57–E64. doi: 10.1152/ajpendo.1998.274.1.E57. [DOI] [PubMed] [Google Scholar]
- 63.Karpe F., Dickmann J.R., Frayn K.N. Fatty acids, obesity, and insulin resistance: Time for a reevaluation. Diabetes. 2011;60:2441–2449. doi: 10.2337/db11-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gastaldelli A. Role of beta-cell dysfunction, ectopic fat accumulation and insulin resistance in the pathogenesis of type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2011;93(Suppl. 1):S60–S65. doi: 10.1016/S0168-8227(11)70015-8. [DOI] [PubMed] [Google Scholar]
- 65.Groop L.C., Bonadonna R.C., DelPrato S., Ratheiser K., Zyck K., Ferrannini E., DeFronzo R.A. Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus. Evidence for multiple sites of insulin resistance. J. Clin. Investig. 1989;84:205–213. doi: 10.1172/JCI114142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Brehm A., Krssak M., Schmid A.I., Nowotny P., Waldhausl W., Roden M. Increased lipid availability impairs insulin-stimulated ATP synthesis in human skeletal muscle. Diabetes. 2006;55:136–140. doi: 10.2337/diabetes.55.01.06.db05-1286. [DOI] [PubMed] [Google Scholar]
- 67.Wang X.L., Zhang L., Youker K., Zhang M.X., Wang J., LeMaire S.A., Coselli J.S., Shen Y.H. Free fatty acids inhibit insulin signaling-stimulated endothelial nitric oxide synthase activation through upregulating Pten or inhibiting Akt kinase. Diabetes. 2006;55:2301–2310. doi: 10.2337/db05-1574. [DOI] [PubMed] [Google Scholar]
- 68.Itani S.I., Ruderman N.B., Schmieder F., Boden G. Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IκB-α. Diabetes. 2002;51:2005–2011. doi: 10.2337/diabetes.51.7.2005. [DOI] [PubMed] [Google Scholar]
- 69.Bugianesi E., Gastaldelli A., Vanni E., Gambino R., Cassader M., Baldi S., Ponti V., Pagano G., Ferrannini E., Rizzetto M. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: Sites and mechanisms. Diabetologia. 2005;48:634–642. doi: 10.1007/s00125-005-1682-x. [DOI] [PubMed] [Google Scholar]
- 70.Fabbrini E., Magkos F., Conte C., Mittendorfer B., Patterson B.W., Okunade A.L., Klein S. Validation of a novel index to assess insulin resistance of adipose tissue lipolytic activity in obese subjects. J. Lipid Res. 2012;53:321–324. doi: 10.1194/jlr.D020321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fabbrini E., Yoshino J., Yoshino M., Magkos F., Luecking C.T., Samovski D., Fraterrigo G., Okunade A.L., Patterson B.W., Klein S. Metabolically normal obese people are protected from adverse effects following weight gain. J. Clin. Investig. 2015;125:787–795. doi: 10.1172/JCI78425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kashyap S., Belfort R., Gastaldelli A., Pratipanawatr T., Berria R., Pratipanawatr W., Bajaj M., Mandarino L., DeFronzo R., Cusi K. A sustained increase in plasma free fatty acids impairs insulin secretion in nondiabetic subjects genetically predisposed to develop type 2 diabetes. Diabetes. 2003;52:2461–2474. doi: 10.2337/diabetes.52.10.2461. [DOI] [PubMed] [Google Scholar]
- 73.Lupi R., Dotta F., Marselli L., Del Guerra S., Masini M., Santangelo C., Patane G., Boggi U., Piro S., Anello M., et al. Prolonged exposure to free fatty acids has cytostatic and pro-apoptotic effects on human pancreatic islets: Evidence that beta-cell death is caspase mediated, partially dependent on ceramide pathway, and Bcl-2 regulated. Diabetes. 2002;51:1437–1442. doi: 10.2337/diabetes.51.5.1437. [DOI] [PubMed] [Google Scholar]
- 74.Marques B.G., Hausman D.B., Martin R.J. Association of fat cell size and paracrine growth factors in development of hyperplastic obesity. Am. J. Physiol. 1998;275:R1898–R1908. doi: 10.1152/ajpregu.1998.275.6.R1898. [DOI] [PubMed] [Google Scholar]
- 75.Thorne A., Lofgren P., Hoffstedt J. Increased visceral adipocyte lipolysis—A pathogenic role in nonalcoholic fatty liver disease? J. Clin. Endocrinol. Metab. 2010;95:E209–E213. doi: 10.1210/jc.2010-0520. [DOI] [PubMed] [Google Scholar]
- 76.Jensen M.D., Haymond M.W., Rizza R.A., Cryer P.E., Miles J.M. Influence of body fat distribution on free fatty acid metabolism in obesity. J. Clin. Investig. 1989;83:1168–1173. doi: 10.1172/JCI113997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Spalding K.L., Arner E., Westermark P.O., Bernard S., Buchholz B.A., Bergmann O., Blomqvist L., Hoffstedt J., Naslund E., Britton T., et al. Dynamics of fat cell turnover in humans. Nature. 2008;453:783–787. doi: 10.1038/nature06902. [DOI] [PubMed] [Google Scholar]
- 78.Ye R., Scherer P.E. Adiponectin, driver or passenger on the road to insulin sensitivity? Mol. Metab. 2013;2:133–141. doi: 10.1016/j.molmet.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Arner E., Westermark P.O., Spalding K.L., Britton T., Ryden M., Frisen J., Bernard S., Arner P. Adipocyte turnover: Relevance to human adipose tissue morphology. Diabetes. 2010;59:105–109. doi: 10.2337/db09-0942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sainz N., Barrenetxe J., Moreno-Aliaga M.J., Martinez J.A. Leptin resistance and diet-induced obesity: Central and peripheral actions of leptin. Metabolism. 2015;64:35–46. doi: 10.1016/j.metabol.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 81.Skurk T., Alberti-Huber C., Herder C., Hauner H. Relationship between adipocyte size and adipokine expression and secretion. J. Clin. Endocrinol. Metab. 2007;92:1023–1033. doi: 10.1210/jc.2006-1055. [DOI] [PubMed] [Google Scholar]
- 82.Vargas G., Chandalia M., Jiang Y., Davila H., Motamedi M., Abate N. Heterogeneity in subcutaneous adipose tissue morphology and metabolic complications in overweight and obese women. Metab. Syndr. Relat. Disord. 2013;11:276–282. doi: 10.1089/met.2013.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alligier M., Gabert L., Meugnier E., Lambert-Porcheron S., Chanseaume E., Pilleul F., Debard C., Sauvinet V., Morio B., Vidal-Puig A., et al. Visceral fat accumulation during lipid overfeeding is related to subcutaneous adipose tissue characteristics in healthy men. J. Clin. Endocrinol. Metab. 2013;98:802–810. doi: 10.1210/jc.2012-3289. [DOI] [PubMed] [Google Scholar]
- 84.Samocha-Bonet D., Dixit V.D., Kahn C.R., Leibel R.L., Lin X., Nieuwdorp M., Pietilainen K.H., Rabasa-Lhoret R., Roden M., Scherer P.E., et al. Metabolically healthy and unhealthy obese—The 2013 stock conference report. Obes. Rev. 2014;15:697–708. doi: 10.1111/obr.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McLaughlin T., Lamendola C., Coghlan N., Liu T.C., Lerner K., Sherman A., Cushman S.W. Subcutaneous adipose cell size and distribution: Relationship to insulin resistance and body fat. Obesity. 2014;22:673–680. doi: 10.1002/oby.20209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Johannsen D.L., Tchoukalova Y., Tam C.S., Covington J.D., Xie W., Schwarz J.M., Bajpeyi S., Ravussin E. Effect of 8 weeks of overfeeding on ectopic fat deposition and insulin sensitivity: Testing the "adipose tissue expandability" hypothesis. Diabetes Care. 2014;37:2789–2797. doi: 10.2337/dc14-0761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.McLaughlin T., Abbasi F., Lamendola C., Reaven G. Heterogeneity in the prevalence of risk factors for cardiovascular disease and type 2 diabetes mellitus in obese individuals: Effect of differences in insulin sensitivity. Arch. Intern. Med. 2007;167:642–648. doi: 10.1001/archinte.167.7.642. [DOI] [PubMed] [Google Scholar]
- 88.Scherer P.E. Adipose tissue: From lipid storage compartment to endocrine organ. Diabetes. 2006;55:1537–1545. doi: 10.2337/db06-0263. [DOI] [PubMed] [Google Scholar]
- 89.Arner P., Arner E., Hammarstedt A., Smith U. Genetic predisposition for type 2 diabetes, but not for overweight/obesity, is associated with a restricted adipogenesis. PLoS ONE. 2011;6:e18284. doi: 10.1371/journal.pone.0018284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arner P. The adipocyte in insulin resistance: Key molecules and the impact of the thiazolidinediones. Trends Endocrinol. Metab. 2003;14:137–145. doi: 10.1016/S1043-2760(03)00024-9. [DOI] [PubMed] [Google Scholar]
- 91.Kanda H., Tateya S., Tamori Y., Kotani K., Hiasa K., Kitazawa R., Kitazawa S., Miyachi H., Maeda S., Egashira K., et al. Mcp-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J. Clin. Investig. 2006;116:1494–1505. doi: 10.1172/JCI26498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bohm A., Halama A., Meile T., Zdichavsky M., Lehmann R., Weigert C., Fritsche A., Stefan N., Konigsrainer A., Haring H.U., et al. Metabolic signatures of cultured human adipocytes from metabolically healthy versus unhealthy obese individuals. PLoS ONE. 2014;9:e93148. doi: 10.1371/journal.pone.0093148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sidossis L.S., Wolfe R.R. Glucose and insulin-induced inhibition of fatty acid oxidation: The glucose-fatty acid cycle reversed. Am. J. Physiol. 1996;270:E733–E738. doi: 10.1152/ajpendo.1996.270.4.E733. [DOI] [PubMed] [Google Scholar]
- 94.Ricchi M., Odoardi M.R., Carulli L., Anzivino C., Ballestri S., Pinetti A., Fantoni L.I., Marra F., Bertolotti M., Banni S., et al. Differential effect of oleic and palmitic acid on lipid accumulation and apoptosis in cultured hepatocytes. J. Gastroenterol Hepatol. 2009;24:830–840. doi: 10.1111/j.1440-1746.2008.05733.x. [DOI] [PubMed] [Google Scholar]
- 95.Siriwardhana N., Kalupahana N.S., Cekanova M., LeMieux M., Greer B., Moustaid-Moussa N. Modulation of adipose tissue inflammation by bioactive food compounds. J. Nutr. Biochem. 2013;24:613–623. doi: 10.1016/j.jnutbio.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 96.Zhao G., Etherton T.D., Martin K.R., Vanden Heuvel J.P., Gillies P.J., West S.G., Kris-Etherton P.M. Anti-inflammatory effects of polyunsaturated fatty acids in THP-1 cells. Biochem. Biophys. Res. Commun. 2005;336:909–917. doi: 10.1016/j.bbrc.2005.08.204. [DOI] [PubMed] [Google Scholar]
- 97.Calder P.C. Polyunsaturated fatty acids and inflammation. Prostaglandins Leukot. Essent. Fatty Acids. 2006;75:197–202. doi: 10.1016/j.plefa.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 98.Mei S., Ni H.M., Manley S., Bockus A., Kassel K.M., Luyendyk J.P., Copple B.L., Ding W.X. Differential roles of unsaturated and saturated fatty acids on autophagy and apoptosis in hepatocytes. J. Pharmacol. Exp. Ther. 2011;339:487–498. doi: 10.1124/jpet.111.184341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Haus J.M., Kashyap S.R., Kasumov T., Zhang R., Kelly K.R., Defronzo R.A., Kirwan J.P. Plasma ceramides are elevated in obese subjects with type 2 diabetes and correlate with the severity of insulin resistance. Diabetes. 2009;58:337–343. doi: 10.2337/db08-1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kang M.J., Shin M.S., Park J.N., Lee S.S. The effects of polyunsaturated:Saturated fatty acids ratios and peroxidisability index values of dietary fats on serum lipid profiles and hepatic enzyme activities in rats. Br. J. Nutr. 2005;94:526–532. doi: 10.1079/BJN20051523. [DOI] [PubMed] [Google Scholar]
- 101.Liao F.H., Liou T.H., Shieh M.J., Chien Y.W. Effects of different ratios of monounsaturated and polyunsaturated fatty acids to saturated fatty acids on regulating body fat deposition in hamsters. Nutrition. 2010;26:811–817. doi: 10.1016/j.nut.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 102.Summers L.K., Fielding B.A., Bradshaw H.A., Ilic V., Beysen C., Clark M.L., Moore N.R., Frayn K.N. Substituting dietary saturated fat with polyunsaturated fat changes abdominal fat distribution and improves insulin sensitivity. Diabetologia. 2002;45:369–377. doi: 10.1007/s00125-001-0768-3. [DOI] [PubMed] [Google Scholar]
- 103.Hudgins L.C., Hellerstein M., Seidman C., Neese R., Diakun J., Hirsch J. Human fatty acid synthesis is stimulated by a eucaloric low fat, high carbohydrate diet. J. Clin. Investig. 1996;97:2081–2091. doi: 10.1172/JCI118645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chong M.F., Hodson L., Bickerton A.S., Roberts R., Neville M., Karpe F., Frayn K.N., Fielding B.A. Parallel activation of de novo lipogenesis and stearoyl-CoA desaturase activity after 3 d of high-carbohydrate feeding. Am. J. Clin. Nutr. 2008;87:817–823. doi: 10.1093/ajcn/87.4.817. [DOI] [PubMed] [Google Scholar]
- 105.Flowers M.T. The Delta9 fatty acid desaturation index as a predictor of metabolic disease. Clin. Chem. 2009;55:2071–2073. doi: 10.1373/clinchem.2009.135152. [DOI] [PubMed] [Google Scholar]
- 106.Warensjo E., Rosell M., Hellenius M.L., Vessby B., De Faire U., Riserus U. Associations between estimated fatty acid desaturase activities in serum lipids and adipose tissue in humans: Links to obesity and insulin resistance. Lipids Health. Dis. 2009;8:37. doi: 10.1186/1476-511X-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mar-Heyming R., Miyazaki M., Weissglas-Volkov D., Kolaitis N.A., Sadaat N., Plaisier C., Pajukanta P., Cantor R.M., de Bruin T.W., Ntambi J.M., et al. Association of stearoyl-CoA desaturase 1 activity with familial combined hyperlipidemia. Arterioscler. Thromb. Vasc. Biol. 2008;28:1193–1199. doi: 10.1161/ATVBAHA.107.160150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Riserus U., Tan G.D., Fielding B.A., Neville M.J., Currie J., Savage D.B., Chatterjee V.K., Frayn K.N., O’Rahilly S., Karpe F. Rosiglitazone increases indexes of stearoyl-CoA desaturase activity in humans: Link to insulin sensitization and the role of dominant-negative mutation in peroxisome proliferator-activated receptor-gamma. Diabetes. 2005;54:1379–1384. doi: 10.2337/diabetes.54.5.1379. [DOI] [PubMed] [Google Scholar]
- 109.Peter A., Cegan A., Wagner S., Lehmann R., Stefan N., Konigsrainer A., Konigsrainer I., Haring H.U., Schleicher E. Hepatic lipid composition and stearoyl-coenzyme a desaturase 1 mRNA expression can be estimated from plasma VLDL fatty acid ratios. Clin. Chem. 2009;55:2113–2120. doi: 10.1373/clinchem.2009.127274. [DOI] [PubMed] [Google Scholar]
- 110.Attie A.D., Krauss R.M., Gray-Keller M.P., Brownlie A., Miyazaki M., Kastelein J.J., Lusis A.J., Stalenhoef A.F., Stoehr J.P., Hayden M.R., et al. Relationship between stearoyl-CoA desaturase activity and plasma triglycerides in human and mouse hypertriglyceridemia. J. Lipid Res. 2002;43:1899–1907. doi: 10.1194/jlr.M200189-JLR200. [DOI] [PubMed] [Google Scholar]
- 111.DeFronzo R.A. Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: The missing links. The claude bernard lecture 2009. Diabetologia. 2010;53:1270–1287. doi: 10.1007/s00125-010-1684-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Belfort R., Mandarino L., Kashyap S., Wirfel K., Pratipanawatr T., Berria R., Defronzo R.A., Cusi K. Dose-response effect of elevated plasma free fatty acid on insulin signaling. Diabetes. 2005;54:1640–1648. doi: 10.2337/diabetes.54.6.1640. [DOI] [PubMed] [Google Scholar]
- 113.Chinen I., Shimabukuro M., Yamakawa K., Higa N., Matsuzaki T., Noguchi K., Ueda S., Sakanashi M., Takasu N. Vascular lipotoxicity: Endothelial dysfunction via fatty-acid-induced reactive oxygen species overproduction in obese zucker diabetic fatty rats. Endocrinology. 2007;148:160–165. doi: 10.1210/en.2006-1132. [DOI] [PubMed] [Google Scholar]
- 114.Inoguchi T., Li P., Umeda F., Yu H.Y., Kakimoto M., Imamura M., Aoki T., Etoh T., Hashimoto T., Naruse M., et al. High glucose level and free fatty acid stimulate reactive oxygen species production through protein kinase C—Dependent activation of NAD(P)H oxidase in cultured vascular cells. Diabetes. 2000;49:1939–1945. doi: 10.2337/diabetes.49.11.1939. [DOI] [PubMed] [Google Scholar]
- 115.Watanabe S., Tagawa T., Yamakawa K., Shimabukuro M., Ueda S. Inhibition of the renin-angiotensin system prevents free fatty acid-induced acute endothelial dysfunction in humans. Arterioscler Thromb. Vasc. Biol. 2005;25:2376–2380. doi: 10.1161/01.ATV.0000187465.55507.85. [DOI] [PubMed] [Google Scholar]
- 116.Egan B.M., Hennes M.M., Stepniakowski K.T., O'Shaughnessy I.M., Kissebah A.H., Goodfriend T.L. Obesity hypertension is related more to insulin's fatty acid than glucose action. Hypertension. 1996;27:723–728. doi: 10.1161/01.HYP.27.3.723. [DOI] [PubMed] [Google Scholar]
- 117.DeFronzo R.A., Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009;32(Suppl. 2):S157–S163. doi: 10.2337/dc09-S302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Perseghin G., Scifo P., De Cobelli F., Pagliato E., Battezzati A., Arcelloni C., Vanzulli A., Testolin G., Pozza G., Del Maschio A., et al. Intramyocellular triglyceride content is a determinant of in vivo insulin resistance in humans: A 1H-13C nuclear magnetic resonance spectroscopy assessment in offspring of type 2 diabetic parents. Diabetes. 1999;48:1600–1606. doi: 10.2337/diabetes.48.8.1600. [DOI] [PubMed] [Google Scholar]
- 119.Szendroedi J., Roden M. Mitochondrial fitness and insulin sensitivity in humans. Diabetologia. 2008;51:2155–2167. doi: 10.1007/s00125-008-1153-2. [DOI] [PubMed] [Google Scholar]
- 120.Jensen M.D. Role of body fat distribution and the metabolic complications of obesity. J. Clin. Endocrinol. Metab. 2008;93:S57–S63. doi: 10.1210/jc.2008-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rahman R., Hammoud G.M., Almashhrawi A.A., Ahmed K.T., Ibdah J.A. Primary hepatocellular carcinoma and metabolic syndrome: An update. World J. Gastrointest Oncol. 2013;5:186–194. doi: 10.4251/wjgo.v5.i9.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Marra F., Gastaldelli A., Svegliati Baroni G., Tell G., Tiribelli C. Molecular basis and mechanisms of progression of non-alcoholic steatohepatitis. Trends Mol. Med. 2008;14:72–81. doi: 10.1016/j.molmed.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 123.Park J.W., Chen M., Colombo M., Roberts L.R., Schwartz M., Chen P.J., Kudo M., Johnson P., Wagner S., Orsini L.S., et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: The bridge study. Liver Int. 2015;35:2155–2166. doi: 10.1111/liv.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.De Minicis S., Agostinelli L., Rychlicki C., Sorice G.P., Saccomanno S., Candelaresi C., Giaccari A., Trozzi L., Pierantonelli I., Mingarelli E., et al. HCC development is associated to peripheral insulin resistance in a mouse model of NASH. PLoS ONE. 2014;9:e97136. doi: 10.1371/journal.pone.0097136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chalasani N., Younossi Z., Lavine J.E., Diehl A.M., Brunt E.M., Cusi K., Charlton M., Sanyal A.J. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American association for the study of liver diseases, American college of gastroenterology, and the American gastroenterological association. Hepatology. 2012;55:2005–2023. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 126.Ertle J., Dechene A., Sowa J.P., Penndorf V., Herzer K., Kaiser G., Schlaak J.F., Gerken G., Syn W.K., Canbay A. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int. J. Cancer. 2011;128:2436–2443. doi: 10.1002/ijc.25797. [DOI] [PubMed] [Google Scholar]
- 127.Dongiovanni P., Romeo S., Valenti L. Hepatocellular carcinoma in nonalcoholic fatty liver: Role of environmental and genetic factors. World J. Gastroenterol. 2014;20:12945–12955. doi: 10.3748/wjg.v20.i36.12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wong R.J., Cheung R., Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59:2188–2195. doi: 10.1002/hep.26986. [DOI] [PubMed] [Google Scholar]
- 129.Basta G., Navarra T., De Simone P., Del Turco S., Gastaldelli A., Filipponi F. What is the role of the receptor for advanced glycation end products-ligand axis in liver injury? Liver Transpl. 2011;17:633–640. doi: 10.1002/lt.22306. [DOI] [PubMed] [Google Scholar]
- 130.Kasumov T., Li L., Li M., Gulshan K., Kirwan J.P., Liu X., Previs S., Willard B., Smith J.D., McCullough A. Ceramide as a mediator of non-alcoholic fatty liver disease and associated atherosclerosis. PLoS ONE. 2015;10:e0126910. doi: 10.1371/journal.pone.0126910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lomonaco R., Ortiz-Lopez C., Orsak B., Webb A., Hardies J., Darland C., Finch J., Gastaldelli A., Harrison S., Tio F., et al. Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with non-alcoholic fatty liver disease. Hepatology. 2012;55:1389–1397. doi: 10.1002/hep.25539. [DOI] [PubMed] [Google Scholar]
- 132.Sommerfeld A., Reinehr R., Haussinger D. Free fatty acids shift insulin-induced hepatocyte proliferation towards CD95-dependent apoptosis. J. Biol. Chem. 2015;290:4398–4409. doi: 10.1074/jbc.M114.617035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Clarke J.D., Novak P., Lake A.D., Shipkova P., Aranibar N., Robertson D., Severson P.L., Reily M.D., Futscher B.W., Lehman-McKeeman L.D., et al. Characterization of hepatocellular carcinoma related genes and metabolites in human nonalcoholic fatty liver disease. Dig. Dis. Sci. 2014;59:365–374. doi: 10.1007/s10620-013-2873-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Muir K., Hazim A., He Y., Peyressatre M., Kim D.Y., Song X., Beretta L. Proteomic and lipidomic signatures of lipid metabolism in NASH-associated hepatocellular carcinoma. Cancer Res. 2013;73:4722–4731. doi: 10.1158/0008-5472.CAN-12-3797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sironi A.M., Petz R., De Marchi D., Buzzigoli E., Ciociaro D., Positano V., Lombardi M., Ferrannini E., Gastaldelli A. Impact of increased visceral and cardiac fat on cardiometabolic risk and disease. Diabet Med. 2012;29:622–627. doi: 10.1111/j.1464-5491.2011.03503.x. [DOI] [PubMed] [Google Scholar]
- 136.Djaberi R., Schuijf J.D., van Werkhoven J.M., Nucifora G., Jukema J.W., Bax J.J. Relation of epicardial adipose tissue to coronary atherosclerosis. Am. J. Cardiol. 2008;102:1602–1607. doi: 10.1016/j.amjcard.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 137.Ding J., Kritchevsky S.B., Harris T.B., Burke G.L., Detrano R.C., Szklo M., Jeffrey Carr J., Multi-Ethnic Study of Atherosclerosis The association of pericardial fat with calcified coronary plaque. Obesity. 2008;16:1914–1919. doi: 10.1038/oby.2008.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Floegel A., Stefan N., Yu Z., Muhlenbruch K., Drogan D., Joost H.G., Fritsche A., Haring H.U., Hrabe de Angelis M., Peters A., et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes. 2013;62:639–648. doi: 10.2337/db12-0495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wang-Sattler R., Yu Z., Herder C., Messias A.C., Floegel A., He Y., Heim K., Campillos M., Holzapfel C., Thorand B., et al. Novel biomarkers for pre-diabetes identified by metabolomics. Mol. Syst. Biol. 2012;8:615. doi: 10.1038/msb.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ferrannini E., Natali A., Camastra S., Nannipieri M., Mari A., Adam K.P., Milburn M.V., Kastenmuller G., Adamski J., Tuomi T., et al. Early metabolic markers of the development of dysglycemia and type 2 diabetes and their physiological significance. Diabetes. 2013;62:1730–1737. doi: 10.2337/db12-0707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rhee E.P., Cheng S., Larson M.G., Walford G.A., Lewis G.D., McCabe E., Yang E., Farrell L., Fox C.S., O'Donnell C.J., et al. Lipid profiling identifies a triacylglycerol signature of insulin resistance and improves diabetes prediction in humans. J. Clin. Investig. 2011;121:1402–1411. doi: 10.1172/JCI44442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Sala-Vila A., Cofan M., Mateo-Gallego R., Cenarro A., Civeira F., Ortega E., Ros E. Inverse association between serum phospholipid oleic acid and insulin resistance in subjects with primary dyslipidaemia. Clin. Nutr. 2011;30:590–592. doi: 10.1016/j.clnu.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 143.Hodge A.M., English D.R., O’Dea K., Sinclair A.J., Makrides M., Gibson R.A., Giles G.G. Plasma phospholipid and dietary fatty acids as predictors of type 2 diabetes: Interpreting the role of linoleic acid. Am. J. Clin. Nutr. 2007;86:189–197. doi: 10.1093/ajcn/86.1.189. [DOI] [PubMed] [Google Scholar]
- 144.Nestel P.J., Straznicky N., Mellett N.A., Wong G., De Souza D.P., Tull D.L., Barlow C.K., Grima M.T., Meikle P.J. Specific plasma lipid classes and phospholipid fatty acids indicative of dairy food consumption associate with insulin sensitivity. Am. J. Clin. Nutr. 2014;99:46–53. doi: 10.3945/ajcn.113.071712. [DOI] [PubMed] [Google Scholar]
- 145.Fox T.E., Bewley M.C., Unrath K.A., Pedersen M.M., Anderson R.E., Jung D.Y., Jefferson L.S., Kim J.K., Bronson S.K., Flanagan J.M., et al. Circulating sphingolipid biomarkers in models of type 1 diabetes. J. Lipid Res. 2011;52:509–517. doi: 10.1194/jlr.M010595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kang S.C., Kim B.R., Lee S.Y., Park T.S. Sphingolipid metabolism and obesity-induced inflammation. Front. Endocrinol. 2013;4:67. doi: 10.3389/fendo.2013.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Samad F., Hester K.D., Yang G., Hannun Y.A., Bielawski J. Altered adipose and plasma sphingolipid metabolism in obesity: A potential mechanism for cardiovascular and metabolic risk. Diabetes. 2006;55:2579–2587. doi: 10.2337/db06-0330. [DOI] [PubMed] [Google Scholar]
- 148.Jornayvaz F.R., Shulman G.I. Diacylglycerol activation of protein kinase cepsilon and hepatic insulin resistance. Cell Metab. 2012;15:574–584. doi: 10.1016/j.cmet.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kotronen A., Seppanen-Laakso T., Westerbacka J., Kiviluoto T., Arola J., Ruskeepaa A.L., Oresic M., Yki-Jarvinen H. Hepatic stearoyl-CoA desaturase (SCD)-1 activity and diacylglycerol but not ceramide concentrations are increased in the nonalcoholic human fatty liver. Diabetes. 2009;58:203–208. doi: 10.2337/db08-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Magkos F., Su X., Bradley D., Fabbrini E., Conte C., Eagon J.C., Varela J.E., Brunt E.M., Patterson B.W., Klein S. Intrahepatic diacylglycerol content is associated with hepatic insulin resistance in obese subjects. Gastroenterology. 2012;142:1444–1446. doi: 10.1053/j.gastro.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gorden D.L., Ivanova P.T., Myers D.S., McIntyre J.O., VanSaun M.N., Wright J.K., Matrisian L.M., Brown H.A. Increased diacylglycerols characterize hepatic lipid changes in progression of human nonalcoholic fatty liver disease; comparison to a murine model. PLoS ONE. 2011;6:e22775. doi: 10.1371/journal.pone.0022775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Pagadala M., Kasumov T., McCullough A.J., Zein N.N., Kirwan J.P. Role of ceramides in nonalcoholic fatty liver disease. Trends Endocrinol. Metab. 2012;23:365–371. doi: 10.1016/j.tem.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]