Synopsis
The care of wounds in exotic animal species can be a challenging endeavor. Special considerations must be made in regards to the animal’s temperament and behavior, unique anatomy and small size, and tendency towards secondary stress-related health problems. It is important to assess the entire patient with adequate systemic evaluation and consideration of proper nutrition and husbandry, which could ultimately impact wound healing. This article summarizes the general phases of wound healing, factors that impact healing, and principles of wound management. Emphasis is placed on novel methods of treating wounds and species differences in wound management and healing.
Keywords: Wound healing, wound management, topical wound therapy, wound products, wound dressings
INTRODUCTION
Open wounds often must be managed for several days, weeks, or even months until they can be closed or they heal by second intention. Most wounds heal without complications; however, the care of wounds in exotic animal species can be a challenging endeavor. Special considerations must be made in regards to the animal’s temperament and behavior, unique anatomy and small size, and tendency towards secondary stress-related health problems. Basic wound care incorporates principles of aseptic technique and gentle tissue handling and is similar across veterinary species. In addition, many wound care products are available that will potentially debride the wound without damaging healthy tissue, reduce infection, and increase the rate of wound healing. This article summarizes the phases of wound healing, factors that impact healing, and general principles of wound management. Emphasis is placed on novel modalities of treating wounds and species differences in wound management and healing.
PHASES OF WOUND HEALING
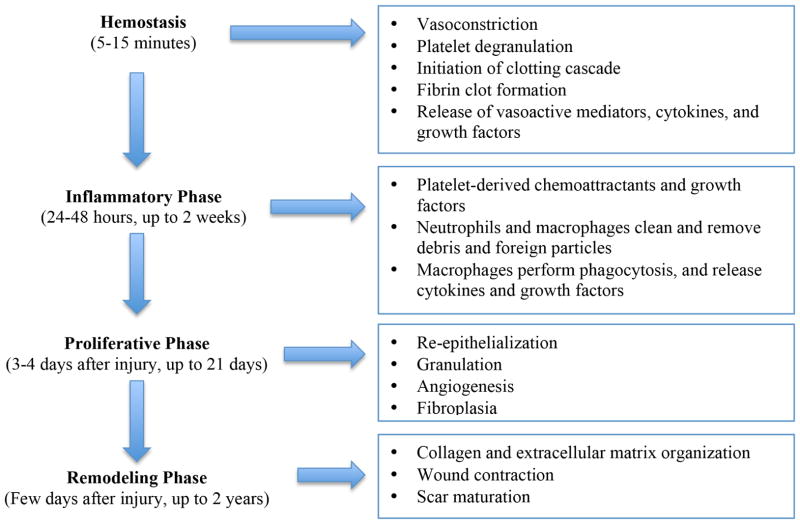
A wound is a physical injury disrupting the normal continuity of anatomic structures, and the wound healing process consists of restoring continuity. Wound healing is typically a well-organized process divided into 3–5 overlapping phases, depending on the classification system: Hemostasis (or coagulation) phase, inflammatory phase, debridement phase (often combined with the inflammatory phase), repair (proliferative) phase, and maturation (remodeling) phase (Figure 1). Chronic or non-healing wounds do not proceed through the normal phases of wound healing, often unable to make the transition from the inflammatory to the repair phase.1, 2 Knowledge of normal wound-healing physiology provides a framework for understanding factors that impair wound healing and for implementing effective wound management strategies.
Figure 1.
Stages of wound healing. (Adapted from Ozturk F, Ermertcan AT. Wound healing: a new approach to the topical wound care. Cutan Ocul Toxicol 2011;30:92–99, with permission.)
Hemostasis (Coagulation) Phase
Immediately following injury to the skin, hemostasis is achieved through vasoconstriction and platelet-mediated activation of the intrinsic clotting cascade, ending in formation of a fibrin clot. Release of proinflammatory cytokines from damaged tissue and the newly formed clot act as potent chemotactic signals to recruit neutrophils, endothelial cells, and fibroblasts to the wound. Formation of the fibrin clot is therefore an important step in promoting onset of the inflammatory and repair phases.1, 2
Inflammatory and Debridement Phase
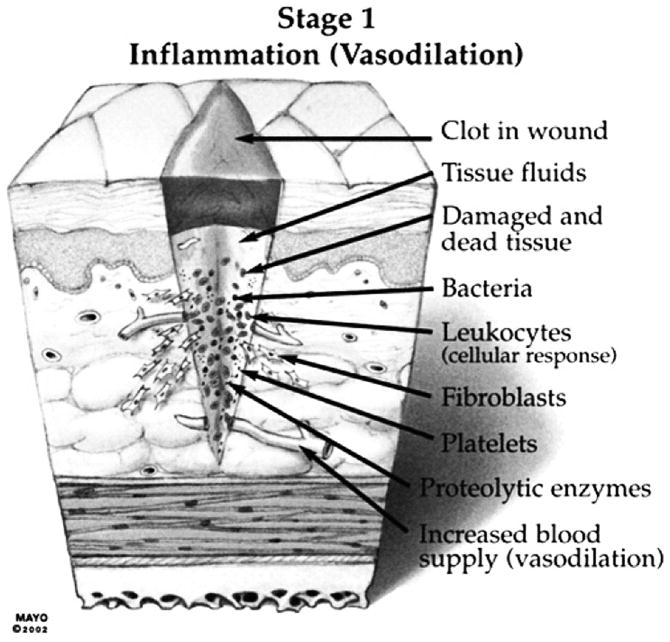
The inflammatory phase is characterized by increased capillary permeability and infiltration of neutrophils, macrophages, and lymphocytes into the wound (Figure 2). Most modern wound classification schemes include the debridement phase within the inflammatory phase due to overlapping time and function of leukocytes within the wound.1–3 Following initial vasoconstriction during hemostasis, vasodilation and increased vascular permeability ensue. Increased blood flow and fluid extravasation combined with blockage of lymphatic drainage cause the classic signs of inflammation, including heat, redness, and swelling. This acute inflammatory response usually lasts for 1–2 days but may persist in a poor wound environment.1, 2
Figure 2.
Stage 1 of wound healing: Inflammation (vasodilation) (From Sherris DA, Kern EB. Essential surgical skills. 2nd edition. Philadelphia: WB Saunders; 2004. p. 13. By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
Wound debridement begins with migration of white blood cells into the wound. Platelets within the fibrin plug release growth factors and cytokines, which recruit inflammatory cells to the wound.2 Circulating neutrophils begin entering the wound within minutes of injury, peaking within the first 24 hours, and are primarily responsible for bacterial phagocytosis.
Monocytes accumulate within 12 hours after injury and undergo differentiation to mature wound macrophages under the influence of local cytokines. Macrophages are the dominant inflammatory cell within three to five days of injury and play a pivotal role in transitioning from inflammation to repair. Macrophages are responsible for phagocytosis of apoptotic cells, tissue debris, and microbial organisms. In addition, they release proinflammatory cytokines that propagate the inflammatory response and growth factors that stimulate conversion of mesenchymal cells to fibroblasts and promote collagen synthesis and angiogenesis.1, 3
Lymphocytes appear later, peaking at approximately seven days. Though the exact role of lymphocytes in wound healing is unknown, it is thought that lymphocytes produce growth factors, interferons, interleukins, and TNF, which recruit fibroblasts and promote wound healing.1, 3
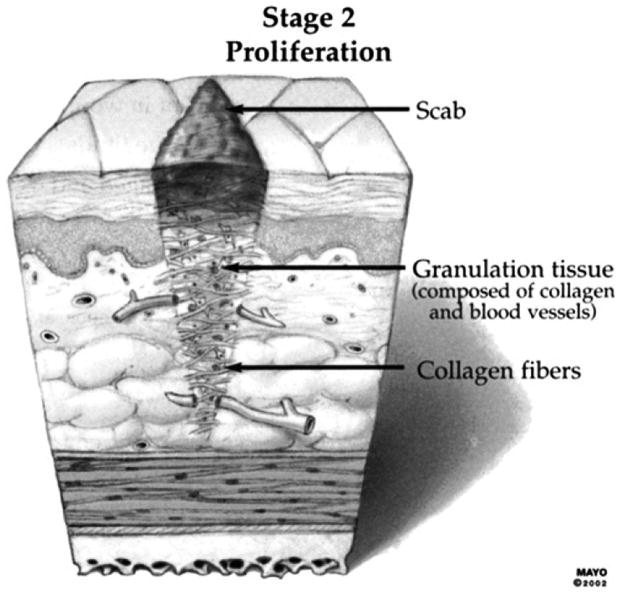
Proliferative (Repair) Phase
The proliferative or repair phase begins approximately 3–4 days after injury and is characterized by fibroplasia, angiogenesis, and epithelialization (Figure 3). Under the influence of growth factors (predominantly PDGF), dermal fibroblasts proliferate, migrate, and differentiate into contractile myofibroblasts. Fibroblasts are critical for the production of extracellular matrix (ECM), comprised of collagen, glycosaminoglycans, proteoglycans, fibronectin, and elastin. TGF-β is one of the most important mediators of collagen matrix formation. It stimulates fibroblasts to produce fibronectin, which is critical to facilitate cell binding and fibroblast movement..2
Figure 3.
Stage 2 of wound healing: Proliferation. (From Sherris DA, Kern EB. Essential surgical skills. 2nd edition. Philadelphia: WB Saunders; 2004. p. 13. By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
Angiogenesis refers to new vessel growth by the sprouting of preexisting vessels adjacent to the wound.2 Angiogenesis occurs as dermal endothelial cells migrate into the new ECM under the influence of macrophage derived angiogenic factor and VEGF.1 The combination of fibroblasts, new capillaries, and fibrous tissue forms bright red granulation tissue.
Epithelialization involves proliferation and migration of epidermal keratinocytes from the wound edges, differentiation of epithelial progenitor cells into a stratified epidermis, and restoration of the basement membrane connecting the epidermis to the underlying dermis.2,3 Epithelial cells move to the wound center by sliding over the fibrin deposits or basal lamina. The epithelial cells migrate under the wound clot and over granulation tissue causing the scab to separate from the wound via secretion of proteolytic enzymes. As cells have migrated further from the wound edge, migration slows down and the initial layer formed is only one cell layer thick. Contraction typically occurs five to nine days after initial injury. The existing tissue at the wound edges is pulled inward by contraction, and surrounding skin stretches, decreasing the overall size of the wound. The process continues until the wound edges meet (contact inhibition), tension is high, or myofibroblasts are inadequate.,4, 5
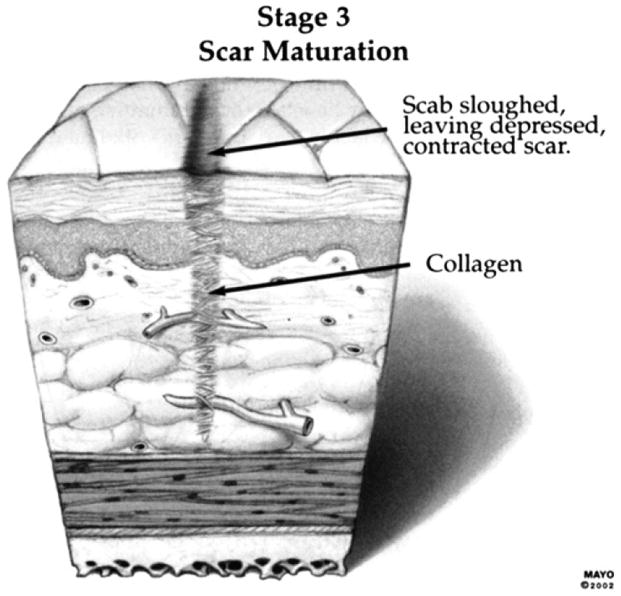
Maturation (Remodeling) Phase
Maturation typically begins one week after injury following collagen deposition in the wound and is the longest phase of wound healing, continuing for weeks to months after injury (Figure 4). The main activity happening during this phase is strengthening and remodeling of the newly formed collagen. There is reduced proliferation and inflammation and regression of the newly formed capillaries in the wound bed. Type III collagen is replaced by type I collagen. Collagen fibers remodel by aligning with tension lines of the body and gain strength through cross-linking. The scar eventually becomes less cellular, flattens, and softens. Normal tissue strength is never regained, with approximately 80% of the original strength acquired at best.1, 2
Figure 4.
Stage 3 of wound healing: Scar maturation. (From Sherris DA, Kern EB. Essential surgical skills. 2nd edition. Philadelphia: WB Saunders; 2004. p. 13. By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
FACTORS IMPACTING WOUND HEALING
Both systemic (host) and local factors serve as potential impediments to wound healing. Host factors include age, body condition, nutritional intake, and concurrent disease. Large wounds place animals in a catabolic state, and thus calorie and protein intake should be increased to ensure that nutritional requirements are met. Hypoproteinemia (< 2.0g/dL) and diets deficient in protein have delay wound healing and decrease wound strength. Underlying metabolic disease, such as diabetes mellitus, hyperadrenocorticism, and uremia, delay wound healing as well.4, 6 Many medications are associated with impaired wound healing and reduced wound strength, including corticosteroids and chemotherapeutic agents.6, 7 Chemotherapeutic drugs further delay healing as they specifically target rapidly dividing cells, affecting fibroblast proliferation and wound strength.8 Nonsteroidal anti-inflammatory drugs have been investigated with regard to their effects on wound healing; however, these medications have not been found to alter the rate of wound healing significantly.6
Local wound factors known to impact healing include tissue perfusion, tissue viability, infection, presence of hematoma and/or seroma, and mechanical factors (tension, motion, wound debris, etc.). The presence of debris, dirt, hair, suture, and necrotic or devitalized tissue act as foreign material, leading to an intense inflammatory reaction that prolongs the inflammatory phase and delays the repair phase. Accumulation of fluid in the wound bed, as with a hematoma or seroma, inhibits fibroblast migration, encourages infection, and leads to wound ischemia, delaying wound healing and strength formation.4, 5 Infection of the wound negatively impacts the process of wound healing as well. It is generally recommended that a wound contaminated with greater than 105 organisms per gram of tissue not be primarily closed, as the incidence of infection is increased.9 Other mechanical factors that impede normal healing include tight bandage placement, tension, and motion, all of which may lead to impaired blood supply, tissue ischemia and necrosis, increased risk of infection, and dehiscence.6 Following Halsted’s surgical principles (gentle tissue handling, strict aseptic technique, sharp anatomic dissection, meticulous hemostasis, obliteration of dead space, avoidance of tension, preserved vascularity, and careful approximation of tissues) will reduce negative local factors in wound healing.
WOUND CLASSIFICATION
Wounds are classified in many ways, based upon whether they are open or closed, duration since injury, underlying etiology, degree of contamination, and degree of skin disruption. Class I wounds (clean) show no signs of inflammation and do not involve a hollow viscous (respiratory, gastrointestinal, or genitourinary tracts). Only skin microflora potentially contaminate the wound, and they generally have only been present for only for 0–6 hours (Figure 5). Class II wounds (clean/contaminated) are clean wounds with a higher risk of infection, such as those in which a hollow viscus has been opened under controlled circumstances without significant spillage of contents. Class III wounds (contaminated) include open accident wounds encountered relative early after injury, those with extensive introduction of bacteria into a normally sterile area due to a major break in sterile technique (Figure 6). Any inflamed tissue around a surgical wound is considered contaminated. Class IV wounds (dirty/infected) include traumatic wounds in which a significant treatment delay has occurred, wounds in which a foreign object is lodged in the wound, or a wound in which necrotic tissue, pus, or fecal matter is present. Bite wounds are considered to be contaminated unless there is purulent exudate, in which case they are considered dirty. When in doubt, the worst category should be presumed for classification in order to provide optimal therapy and reduce the chance for complications. The classification of the wound, in addition to local wound factors, can help guide the type of management approach that should be taken for any given wound. 10, 11
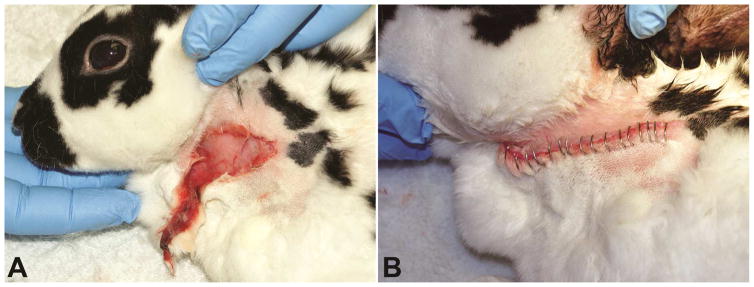
Figure 5.
Skin laceration in a rabbit. A) Initial presentation of the wound, within one hour after infliction due to con-specific trauma. B) The wound was lavaged the skin edges trimmed and skin staples were used to perform primary wound closure. The wound healed without complications.
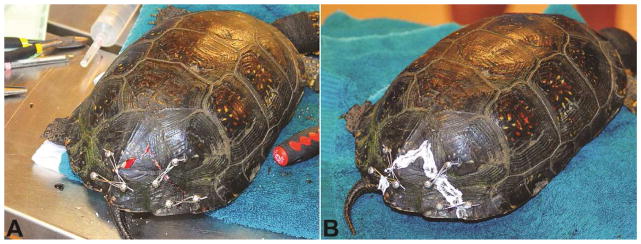
Figure 6.
Chronic wound dorsal to the tail base in a pained turtle (Chrysemys picta) secondary to marginal scute malformation allowing for con-specific trauma in an overcrowded enclosure. A) Initial presentation. B) The same wound following surgical debridement. Note the healthy granulation tissue
INITIAL WOUND CARE AND MANAGEMENT
The goal of wound care is to prevent further contamination and convert contaminated or infected wounds into clean wounds for either surgical closure or second intention healing. In order to fully assess an open wound, sedation or general anesthesia may be indicated. Wounds should be lavaged and debrided immediately, after which samples from the deep aspects of the wound are collected for culture and susceptibility. A biopsy should be considered for all chronic or non-healing wounds. Aseptic technique should be utilized when treating wounds, including the use of sterile gloves, instruments, and bandage materials.11 It should be noted that wound healing is faster under moist and wet conditions. Excessive wetness, however, can be problematic, and thus the ideal wound dressing should absorb exudate without excessively drying the wound.
DECONTAMINATION (LAVAGE)
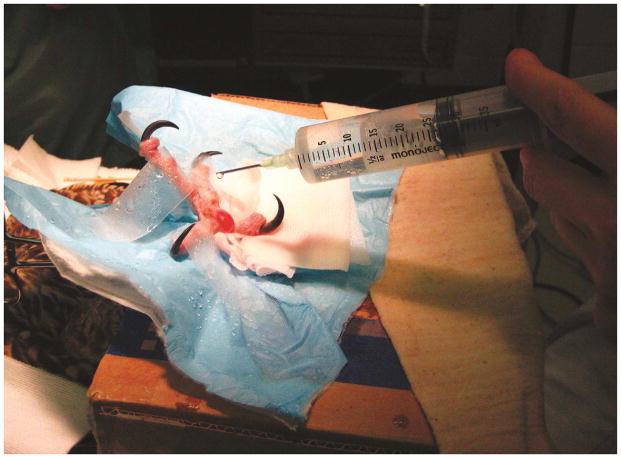
The primary aim of decontamination is to remove bacteria and debris from the wound bed. Following the initial assessment, the wound should be covered with sterile water-soluble lubricant in order to prevent further contamination, and the surrounding wound hairs should be clipped. Lavage with copious, warm, sterile isotonic fluids, such as lactated Ringer’s solution (LRS) or phosphate-buffered saline, should be performed as soon as possible (Figure 7). Use of sterile tap water or prolonged exposure to normal saline has been shown to be cytotoxic to fibroblasts in vitro.6 Adequate irrigation pressure can be achieved with the use of a 35- or 60-mL syringe and 18 gauge catheter or needle or with the use of a syringe connected to a 3-way stopcock and bag of fluids.
Figure 7.
Lavage of a pododermatitis wound following surgical debridement in a peregrine falcon (Falco peregrinus).
Use of lavage solutions containing antiseptics has not been shown to enhance the benefits of lavage.6 If antiseptic solutions are chosen, 0.05% chlorhexidine and 0.5 or 1% povidone-iodine would be considered appropriate. Chlorhexidine solution is not impaired by organic material, has broad-spectrum activity with minimal systemic absorption and maintains residual activity up to two days following application. Povidone-iodine has broad-spectrum activity against bacteria, fungi, viruses, and yeast but is inactivated by the presence of organic matter and has little residual activity. Caution should be observed with more concentrated formulations, as they are cytotoxic, may slow granulation tissue formation, and ultimately impair or delay wound healing.5
Tris-ethylenediaminetetraacetic acid (EDTA) increases susceptibility of bacteria, especially gram-negative bacteria, to antibiotics and antiseptics. Alcohol, hydrogen peroxide, Dakin solution, and acetic acid should be avoided, as they are cytotoxic to the normal tissues.11, 12
DEBRIDEMENT
Debridement entails removal of necrotic and devitalized tissue from the wound with the goal of creating a fresh, clean wound bed for primary or delayed closure. Debridement can consist of surgical, enzymatic, autolytic, or mechanical means.
NONSELECTIVE DEBRIDEMENT
Surgical Debridement
Surgical debridement is indicated for removing large amounts of necrotic debris (Figure 6). Foreign debris is removed with thumb forceps, and necrotic tissue is removed by sharp dissection. In small exotic species, surgical debridement can be performed using sharp excision with a scalpel blade. Nonviable or necrotic tissue often appears purple or black in color, or is loose yellow to brown if sloughing. Care should be taken to avoid removal of viable tissue. Tissue with questionable viability should be left for reassessment the next day. Typically the extent of tissue necrosis will be apparent within 24 to 48 hours following tissue injury, and repeat debridement can be done at that time. The subdermal vascular plexus and supply to the skin should be preserved when possible.
Mechanical Debridement
Mechanical debridement is achieved through the use of adherent dry-to-dry or wet-to-dry bandages. The dressings, usually gauze, are allowed to adhere to the wound. Debridement is nonselective, as once dry, the dressings are removed, pulling off debris along with the superficial layers of the wound bed. The removal of adherent dressings can be painful and typically need to be changed multiple times daily for the first few days.5, 11, 13, 14 The use of wet-to-dry bandages is controversial due to the nonselective nature of debridement and pain associated with removal. If selected, debridement with gauze sponges should only be performed during the inflammatory phase of wound healing.6
SELECTIVE DEBRIDEMENT
Enzymatic Debridement
Enzymatic debridement refers to the use of enzymatic agents to selectively destroy necrotic tissue and liquefy coagulum and bacterial biofilm.6 The most common enzymatic agents currently on the market contain either collagenase or papain-urea, and they are typically available as ointments or gels. Advantages of enzymatic agents include that they are not painful and do not require anesthesia. Further, they can be used as an adjunct to surgical debridement when excision could harm healthy tissues that must be preserved.
There are several disadvantages to enzymatic debridement that should be taken into consideration. Enzymatic debridement is slow, which is not practical for large wounds, and the products may be cost prohibitive. Further, they cause a local inflammatory and pyogenic reaction and should not be used for long-term management. Enzymes can damage or dehydrate normal tissue and if in contact with adjacent healthy tissue surrounding the wound bed, may cause maceration. These ointments or gels are typically applied to the wound bed, covered with a non-adherent dressing, and changed every 12 to 24 hours.15 2, 13
Autolytic Debridement
Autolytic debridement is the natural process that occurs in a moist wound environment in which the enzymes present in the wound fluid debride necrotic tissue. The process is facilitated by placement of hydrophilic, occlusive, or semi-occlusive bandages to maintain wound moisture and allow wound exudate to remain in contact with the wound (Figure 8). Wound exudate contains endogenous enzymes, cytokines, and growth factors that digest necrotic debris while stimulating granulation tissue formation, angiogenesis, and epithelialization. This mechanism is often preferred in wounds with questionable tissue viability, but should be avoided in infected wounds.
Figure 8.
Dressing of a carapacial wound in a common snapping turtle (Chelydra serpentina). A hydrogel sheet is applied to the wound and secured in place by a waterproof transparent film dressing. The animal was allowed full access to water, because the dressing was waterproof.
TOPICAL PRODUCTS
The majority of wounds will heal well utilizing basic wound management techniques and proper bandage application; however, for chronic, non-healing wounds, topical products may be considered as an adjunct. Non-healing wounds are arrested in one of the phases of healing, typically the inflammatory phase.2 Thus, novel wound care products promote transition from the inflammatory to the proliferative phase. It is important to acknowledge, however, that there is little information about the efficacy of topical wound products in veterinary medicine, and even less so in exotic animal species.
Topical Antimicrobials
Topical antimicrobials include antiseptics, silver-based dressings, hyperosmotic dressings and other dressings. These products reduce the number of microorganisms present in the wound bed and promote autolytic debridement. They do have cytotoxic effects, and thus their potential benefits should outweigh the risks, and they should thus be discontinued once a granulation bed is present. Topical antimicrobials are often narrower in spectrum and may promote the creation of “super infections” or nosocomial infections with continued usage.
Triple antibiotic ointment containing bacitracin zinc, neomycin sulfate, polymyxin B sulfate, has broad-spectrum antimicrobial activity and is one of the most commonly used topical antimicrobials. It is not cytotoxic, and is thought to actually enhance epithelialization though it may inhibit wound contraction.5, 11, 12, 15, 16 Bacitracin is not recommended for use in rodents or rabbits due to the risk of dysbacteriosis of the enteric flora.
Gentamicin sulfate ointment is particularly active against gram-negative bacteria, including Pseudomonas and Staphylococcus species. It is also available as a solution, which promotes epithelialization and does not inhibit contraction as seen with use of the cream-based ointments. 5, 11, 12, 15, 16
Silver is an important and widely adopted antimicrobial agent that has been shown to have effects against methicillin-resistant Staphylococcus aureus, fungi, and a variety of other bacteria and does not lead to antibiotic resistance.17 The most common topical silver formulation is silver sulfadiazine cream (SSD) (1%) (Figure 9), which can penetrate necrotic tissue and enhance wound epithelialization; however SSD cream has been shown to impede wound contraction and cause bone marrow suppression if used in larger wounds. SSD has historically been the topical wound treatment of choice in human burn patients. 5, 11, 12, 15, 16 Newer products combining a biologic dressing or polymeric nanofilms with silver to immobilize silver at the wound bed show promise in reducing bacterial burden in full thickness wounds without impeding wound contraction (Figure 8, Figure 10-A).17, 18
Figure 9.
A) Carapacial fracture repair followed by application silver sulfadiazine cream (B) to the fracture site following reduction, in order to prevent contamination in a Blanding’s turtle (Emys blandingii).
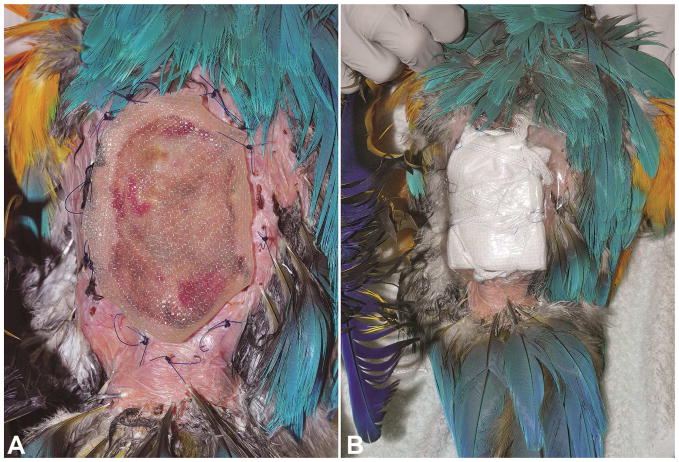
Figure 10.
Large full-thickness wound over the dorsum in a blue and gold macaw (Ara ararauna). A) A hydrogel sheet is placed on the wound as the primary dressing. Note the loose suture loops placed in the periphery of the wound in order to facilitate the tie-over-bandage. B) Gauze has been used as the secondary bandage layer. Umbilical tape is used to create a tie-over bandage. For additional support a waterproof transparent film dressing was applied.
Nitrofurazone has broad-spectrum activity and is hydrophilic in nature, drawing fluid from the wound and decreasing edema in highly exudative wounds. It is known to delay epithelialization, however, and is a known carcinogen. Further, it has reduced antibacterial activity in the presence of organic matter. 5, 12, 15, 16
Aloe Vera
Aloe vera gel has antiprostaglandin, antithromboxane, and antibacterial properties, allowing it to prevent dermal ischemia. Allantoin, a component of aloe vera, promotes epithelial growth and stimulates tissue repair. Acemannan, available as a hydrogel or freeze-dried form (e.g. Carravet, Veterinary Products Labs, Phoenix, Arizona; Carrasorb, Carrington Labs, Irving, Texas), is another component of aloe vera that stimulates macrophages to increase cytokine production, increasing fibroblast proliferation, epidermal growth, and collagen deposition. This is best applied in the early inflammatory phase of wound healing. It can cause excess granulation tissue formation, especially in the freeze-dried form, which inhibits wound contraction.5, 12, 15, 16 It was shown to stimulate fibroblast replication in an experimental study with guinea pig burn wounds.19 The gel enhanced wound healing at 7 days compared to triple-antibiotic and control groups in dogs with pad wounds.20
Tripeptide-Copper Complex
Tripeptide-copper complex (TCC) gel (e.g. Iamin-Vet Skin Care Gel, Covington, Georgia) serves as a chemoattractant for macrophages and mast cells, which stimulates debridement, angiogenesis, collagen deposition, and wound contraction. Copper is utilized for collagen cross-linking, and is thus best utilized in the late inflammatory and early repair phases of wound healing.5, 15, 16 TCC was shown to significantly decrease overall wound healing time in ischemic wounds of rats when compared to controls.21
Maltodextrin NF
Maltodextrin NF, a D-glucose polysaccharide with 1% ascorbic acid (e.g. Intracell, Techni-Vet, Albuquerque, New Mexico), is a hydrophilic powder or gel that provides glucose for cell metabolism, draws fluids from the wound, acts as a chemoattractant, and has antibacterial and bacteriostatic properties. It can be utilized in the early inflammatory phase to reduce exudate, swelling, and infection in the wound bed.5, 15, 16, 20
Honey
Honey has historically been used in wound management, with the benefits of decreasing inflammatory edema, enhancing wound debridement via stimulation of macrophage migration and acceleration of tissue slough, providing a protective layer of protein to the wound bed along with improving wound nutrition, and promoting granulation tissue formation. In addition to these benefits, it is reported to have antibacterial properties due to its high osmolarity, low pH, and enzymatic production of hydrogen peroxide from glucose. While honey is readily available, it is recommended to use medical grade honey. 5, 11, 15, 16, 22 Honey is widely used in wound management of exotic animals, in particular chelonians and birds (Figures 11, 12).
Figure 11.
A) Full-thickness wound of the distal tarsometatarsus of a wattled crane (Bugeranus carunculatus). B) Application of a commercial honey dressing sheet to the same wound. A waterproof transparent film dressing is applied as the secondary layer in order to secure the honey dressing in place. An elastic bandage was applied as the tertiary layer (not shown).
Figure 12.
Multiple Carapacial fractures and bone loss in a common snapping turtle (Chelydra serpentine). A) Initial presentation. B) Following surgical debridement and stabilization of the fractures, sterile gauze strips soaked in raw honey were applied to the soft tissue wounds. C) A waterproof transparent film dressing is applied as the outer layer and the edges are secured with medical tape.
Sugar
Sugar has a high osmolality which reduces wound edema, attracts macrophages, accelerates sloughing of devitalized tissue, provides an energy source for cells, promotes formation of a protective protein layer over the wound, and enhances granulation tissue formation. Granulated sugar should be applied at least 1 cm thick over the wound and covered with an absorbent bandage.5, 15, 16, 23 When utilizing sugar and honey, caution should be taken to ensure the patient maintains normal hydration, electrolytes, and protein levels given the hydrophilic nature of the two topical therapies. Both honey and sugar can be applied throughout the inflammatory phase of wound healing, but should be discontinued once granulation tissue is present.
Hypertonic saline
Hypertonic saline soaked dressings composed of 20% sodium chloride can be used for their osmotic effect, which draws fluid from the wound into the dressing, desiccating necrotic tissue and bacteria in the process.11 They are only recommended for infected, heavily exudative, and necrotic wounds that require aggressive debridement, as debridement is nonselective. These dressings are only appropriate in the initial few days of the inflammatory phase and should be changed at least every 3 days. Following initial treatment with hypertonic saline, the wound bed can be further treated with an alginate, hydrogel, or foam dressing.5, 24
Growth Factors
Growth Factors regulate many of the key cellular activities involved in the normal wound healing process, including cell division and migration, angiogenesis, and synthesis of the extracellular matrix. Applying a single growth factor is likely not efficacious without knowing which specific growth factors are deficient at the time. Recombinant human-derived PDGF (Regranex Gel, Ortho-McNeil Pharmaceutical, South Raritan, New Jersey) is available and is thought to promote chemotactic recruitment and proliferation of cells for wound repair, accelerate wound healing via promotion of granulation tissue formation, wound contraction and remodeling, stimulation of angiogenesis and recruitment of macrophages, neutrophils, and fibroblasts.5, 12, 15 It has been shown to accelerate wound healing in humans with diabetic and neurotropic ulcers.25
Platelet-derived products are available as a source of growth factors. Platelets can be harvested and concentrated to produce platelet-rich plasma (PRP), which can be used to enhance fibroblast proliferation and epithelialization. Gel derived from PRP has been shown to speed healing of chronic decubital ulcers in dogs compared to controls with paraffin-impregnated gauze.26
Chitosan
Chitosan is a polysaccharide derived from chitin, a component of the exoskeleton in shellfish, which contains the active ingredient glucosamine. It accelerates wound healing via enhancing the function of inflammatory cells, growth factors, and fibroblasts. A reported side effect in dogs is fatal hemorrhagic pneumonia at doses greater than 50mg/kg subcutaneously.11, 12, 15, 16, 27
WOUND CLOSURE TECHNIQUE
Factors considered when deciding how to close a wound include the degree of contamination present, the time from injury, presence of devitalized tissue, amount of tissue tension and extent of dead space, the amount of soft tissue loss and adjacent tissue available for closure, the blood supply and status of the wound vasculature, hemostasis, location and ability to close, and overall patient stability for general anesthesia.
Primary Wound Closure
Primary wound closure (first-intention healing) is considered appositional healing in which closure is achieved by fixing the edges of the wound in contact with one another. Class I wounds and those that can be completely excised and converted to a surgical wound are managed by primary closure. Primary closure is often recommended in cases where the wound is clean, has minimal trauma and contamination, and is less than 6 to 8 hours old following lavage and debridement.5, 11
Secondary Wound Closure
Secondary wound closure (second-intention healing) is used for large skin defects in which the wound edges cannot be approximated or wounds with extensive tissue devitalization. Secondary closure requires formation of a granulation tissue matrix, wound contracture, and epithelialization. Disadvantages of this technique include an increased length to healing or incomplete healing, significant time and energy in wound management, formation of a fragile epithelial scar, and creation of scar tissue.5, 11
Delayed Primary Wound Closure
Delayed primary closure (tertiary-intention healing) is a combination of primary and secondary closure. This type of closure is preferred when a wound is heavily contaminated to reduce the risk of the wound becoming infected. The wound is cleansed and watched for several days to ensure no infection is apparent. When the wound appears to be clean and on it’s way to healing, it is closed surgically. Closure may be elected before or after the presence of granulation tissue. The granulation bed offers the benefit of microbial resistance and increased vascularity once closure is elected.6,5, 11 Certain types of injuries almost always become infected (e.g. bite wounds); these types of injuries are frequently left open and closed only if the infection is controlled.
BANDAGING
The purpose of bandage application is multifactorial, including protection of the wound from contamination and mechanical forces exerted by the external environment or the patient, management of wound exudate, elimination of dead space, immobilization to injured tissue, support and comfort, prevention of wound contamination, minimization of scar tissue, and promotion of healthy wound environment that ultimately promotes healing.5, 12, 24, 28 Bandages are a very important adjunct when considering open wound management. A bandage typically consists of three main layers: the contact, intermediate, and outer layers, with each layer serving a specific purpose. As mentioned previously, keeping the wound bed moist has been shown to accelerate both the inflammatory and proliferative phases of wound healing.
Primary Contact Bandage Layer (Wound Dressings)
Potential functions of the primary contact layer of a bandage include debridement of necrotic debris, delivery of medications, absorption of wound exudate, or formation of an occlusive seal that maintains a moist wound environment. The choice of dressing depends on the condition of the wound (cause, size, location, degree of exudate, and level of contamination), stage of healing, and the activity level or special needs of the patient. (Figure 13)2 Considerations in choosing the contact layer include whether it’s adherent or non-adherent, the permeability, and the absorptive capacity of the material. Adherent dressings are those that adhere to the wound surface, leading to nonselective debridement of necrotic tissue, bacteria, and some normal tissue from the wound. Non-adherent dressings serve to maintain a moist wound environment and encourage epithelialization once a granulation bed is present. Non-adherent dressings are typically semiocclusive (allowing permeability of fluid and air) or occlusive (impermeable to fluid and air, keeping wound humidified during the repair phase) and include films, foams, hydrogels, hydrocolloids, and alginates (Figure 10-A). Contrary to previous belief, occlusive dressings are associated with faster wound healing and better cosmetic outcomes.2, 6
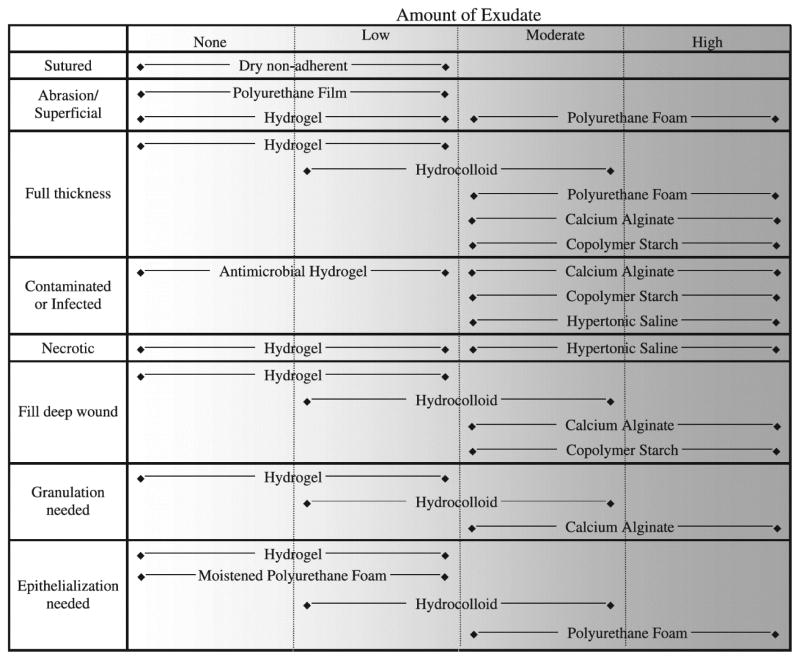
Figure 13.
Guidelines for selection of primary wound dressings based on wound type and amount of wound exudate. (From Campbell BG. Dressings, Bandages, and splints for wound management in dogs and cats. Vet Clin Small Anim 2006;36:759–91, with permission.)
Semiocclusive Dressings
Semiocclusive dressings allow penetration of air and exudate from the wound surface due to their porous nature. They are the most common primary layer utilized and are typically used on less exudative wounds to maintain moisture in the early repair phase.5, 11 Traditional choices include cotton non-adherent bandages, such as polyethylene (e.g. Telfa Adhesive Pads, The Kendall Co., Mansfield, Massachusetts), moisture and vapor permeable dressings (e.g. Tegaderm, 3M Animal Care Products, (Figures 8, 12-C), and petroleum-impregnated gauze (e.g. Adaptic, Ethicon, Inc, Arlington, Texas).5, 16, 28 Petroleum can slow wound contraction and epithelialization.28
Films
Films are thin membranes that are also semiocclusive, permitting the exchange of oxygen and water vapor between the wound and the environment while remaining impermeable to liquid and bacteria. These dressings are non-absorbent, in that they manage moisture by vapor transmission only. Films are not ideal for wounds with heavy exudate.2
Foams
Polyurethane foams are composed of synthetic polymers (e.g. Hydrasorb, KenVet Animal Care Group, Ashland, Ohio). These are highly absorptive, hydrophilic, and nonadherent dressings that promote autolytic debridement, stimulate granulation tissue formation, and promote epithelialization.5, 28, 29 Polyurethane foam is recommended for wounds with moderate to heavy levels of exudate and can be used in the case of infected wounds. Dressings should be replaced every 1 to 5 days, avoiding dry out since they can become incorporated into the wound bed, becoming difficult, painful, and traumatic to remove.
Hydrogels
Hydrogels consists of a fibrous network of polymers and humectants combined with 90–95% water, which forms a sheet or gel. They are able to absorb small amounts of fluid, but are capable of donating significant amounts of moisture to the wound bed, rehydrating the wound, facilitating autolytic debridement, and removing a dried eschar. They are useful in the later phases of wound healing that have healthy granulation tissue and initiation of epithelialization. Hydrogels are flexible and can fill dead space, but present similar problems as with hydrocolloids where maceration of surrounding tissue is possible if they are not cut to the size of the open wound bed.5, 12, 24, 28, 30 A hydrogel sheet and get form with sustained release of silver ions (SilvaSorb™ (Medline Industries, Inc) has been used extensively in exotic and wildlife patients. (Figures 8, 10-A) These products provide up to 7 days of antimicrobial control and a moist wound environment. The sustained release of silver, allows for less frequent dressing changes, which results in less handling and restraint-related stress and risk of injury for exotic and wildlife patients.31
Hydrocolloids
Hydrocolloids are composed of hydrophilic polymers, such as carboxymethylcellulose with gelatin or pectin, that interact with wound fluid to form a gel, maintaining a moist wound environment which facilitates autolytic debridement. The dressings are cut to the size and shape of the wound to avoid maceration of the wound edges. They can be pre-warmed in the clinician’s hands prior to application to soften the dressing for improved wound contouring.24 The dressings are typically designed to be changed every 3 to 7 days, depending upon the amount of exudate and the manufacturer guidelines. If used too long, exuberant granulation tissue can form.5, 12, 24, 28, 29 Hydrocolloids are not recommended for wounds with heavy exudate or when infection is present. When compared with hydrogels and polyethylene oxide dressings for open wounds in dogs, they were shown to have no significant difference early on (days 4 and 7) but demonstrated less complete healing on days 21 and 28 compared to the hydrogel group.30
Alginates
Alginates consist of fibers derived from seaweed arranged in sheets or ropes. Sodium ions in the wound fluid exchange with calcium ions in the dressing, converting the material into a gel that is capable of absorbing up to 20 times its own weight.32, 33 The calcium ions released activate prothrombin in the clotting cascade, promoting hemostasis.34 Alginates impregnated with silver are available for its antimicrobial properties. Alginates are best suited for heavily exudative wounds in which they promote autolytic debridement and granulation tissue formation. Sheets are cut to fit the size of the wound bed and ropes can be placed within deep wounds. The dressings are changed when strike through of exudate occurs, which can be up to 7 days. 5, 23, 24, 28, 32 Oftentimes with use of an occlusive dressing that converts to a gel, a mild odor or yellow, purulent appearance is seen at bandage changes, which should not to be confused with infection. 29, 32, 33
Other products
Other products available include bioactive dressings that originate from living tissue, such as those derived from fibroblasts, keratinocytes, amnion, and submucosa of porcine small intestine or urinary bladder. They are thought to accelerate wound repair via provision of an ECM for cellular migration and can thus be used as a scaffold for tissue ingrowth.
Hydrolyzed bovine collagen (e.g. Collamand, BioVet, Inc., Topeka, Kansas) serves as a template of collagen fibers for fibroblasts, epithelial and endothelial cells to enter and migrate across.5, 15, 24 Bovine collagen has been shown to enhance early epithelialization compared to controls in dog wounds, which could be due to its hydrophilic nature.35
Porcine small intestinal submucosa (PSIS) (e.g. VetBioSIST, Cook, West Lafayette, Indiana) consists of collagen, fibronectin, hyaluronic acid, chondroitin sulfate A, heparin, and various growth factors.5, 15, 16, 24 In a study of open wounds with bone exposure in dogs, there was no difference in wound healing, epithelialization, contraction, inflammation or angiogenesis between PSIS applied wounds and control wounds.36 These scaffolds are cut slightly larger than the area of the wound with the edges tucked underneath the wound edges, sutured, and left in place to be incorporated within the host tissues. Over two weeks following placement, neutrophils break down the scaffold, releasing cytokines and growth factors that promote healing and neovascularization.37
Equine amnion has been used as an occlusive dressing that was shown to increase wound contraction and epithelialization compared to hydrogel and polyethylene non-adherent dressings in a canine study.38 Due to cost concerns, these dressings are reserved for chronic, non-healing wounds where granulation tissue is needed.
Secondary (Intermediate) Bandage Layer
The secondary or intermediate layer is often times minimized or avoided in exotic species, in order to limit the bulkiness of the bandage. This layer holds the contact layer in place, and functions in exudate absorption, pressure, support, and reduction of mobility. This layer should be thick enough to collect the amount of exudate that is anticipated and serve as a pad to prevent movement (Figure 10-B). Materials commonly used include cast padding, combine rolls or absorbent bulk roll cotton. The inner, absorbent layer is typically followed by an outer, stabilizing layer. When indicated, a splint or stabilizing rod can be placed between these layers to provide immobilization. The outer stabilizing portion is typically achieved using roll gauze.
Tertiary (Outer) Bandage Layer
The tertiary or outer layer primarily functions to hold the other layers of the bandage in place and protect the wound and underlying bandage from external contamination. Materials most commonly used for this layer include elastic adhesive tapes, stockinette, surgical adhesive tape, or spandex garments.5, 24, 28 Care should be taken that the bandage is not placed too tight when using bandage material with elastic properties. In exotic patients adhesive films (e.g. Tegaderm™) can be effective outer layers and are frequently used, especially in birds and reptiles (Figures 8, 10-B, 12).
Tie-over Bandages
In cases where a circumferential bandage is not possible, a tie-over bandage can be utilized. Several sutures are loosely placed in the skin surrounding the periphery of the primary wound (Figure 10-A). The primary wound is covered with an appropriate dressing over which an absorbent layer with gauze or laparotomy pads is placed. The bandage is secured using umbilical tape or suture threaded through the suture loops in the skin and knotted (Figure 10-B). When bandages are changed, the suture loops remain in place, limiting additional stress placed upon the patient. In order to prevent additional contamination, an adhesive film can be placed over the entire bandage, limiting environmental exposure.5
Bandage Changes
The level of exudate present should determine the timing of bandage changes. The ideal timing of a bandage change may be daily initially; however, in exotic species it is imperative to consider the risks of stress and frequent sedation or anesthesia indicated. Therefore, bandage choices, such as hydrogels, which can potentially be changed less frequently due to their ability to maintain wound moisture, may be better options in these species. Efforts should be made to protect the bandage. Elizabethan collars (E-collars) are the most common method to protect the bandage from patient-induced damage, such as licking or chewing It is imperative that the bandage be kept dry, away from fecal and urinary contamination. This may merit separation of group-housed animals temporarily. Proper selection of bandage materials and topical wound dressings should be catered to the individual patient, and consideration should be taken to the behavior of the species along with the nature of the wound.
NEGATIVE PRESSURE WOUND THERAPY
Negative pressure wound therapy (NPWT) is an adjunctive wound management technique that locally applies subatmospheric pressure across a wound in a closed environment. Open-pore polyurethane foam sponges are placed within the wound bed following debridement and semiocclusive adhesive dressing is placed over the foam extending a few centimeters beyond the edge of the wound margin to create a complete seal. A hole is created in the dressing over the center of the foam and the suction port with tubing is attached to the suction pump canister. The unit is set to either continuous or intermittent suction. If no leaks in the system are present, the foam should visibly collapse beneath the adhesive.11, 39
NPWT is proposed to increase wound healing via promoting wound contraction, stimulating granulation tissue formation, increasing tissue perfusion, reducing edema, removing exudate, and decreasing bacterial colonization.40 Large, comprehensive reviews have revealed that insufficient or contradictory evidence currently exists with regards to the mechanisms of action of NPWT.40 However, successful clinical reports have been made in exotic species, including avian, chelonians, and experimentally in rabbits and rats. NPWT should not be utilized when there is potential for the wound to contain neoplastic cells or when there are exposed organs, nerves, or large vessels, where negative pressure could result in hemorrhage or erosion.40 Initially the dressings may need to be changed daily, but can later be changed every 2–3 days.
CONSIDERATIONS FOR WOUND MANAGEMENT IN EXOTIC ANIMAL SPECIES
While the underlying concepts of wound healing as detailed above are similar across the board, variations amongst species exist with regard to healing.
Birds
Avian integument is thinner and more delicate than mammalian skin, while also being dry and inelastic. It is comprised of two layers, the dermis and epidermis. The dermis is the site of feather development from dermal papilla and contains striated muscle that functions to control skin tension. Dense dermal capillary beds contribute to the red coloration of wattles, combs, and appendages in some species. The epidermis contains living and dead cells, with the outer keratinized stratum corneum made of horny dead cells. It is important to consider that wounds of the distal extremities have reduced vascular supply and thus heal more slowly. In avian species, bruising may develop 2–3 days post injury and is characterized by a green discoloration of the skin due to biliverdin pigment accumulation following breakdown of hemoglobin. Caution should be observed with the use of topical therapy due to the thin dermis, which predisposed to increased absorption of topical medications with the potential for systemic effects. Avoid oil-based products in birds, as they can be preened into feathers, affecting thermoregulation. Causes of open wounds are most often traumatic, bite wounds from other animals or self-inflicted wounds, but constriction injuries, infections, and cutaneous neoplasms are also seen. Chronic, non-healing wounds of the medial wings and patagium are difficult to manage primarily due to the dynamic movement of muscles, tendons, and skin of the wings during flight. It is oftentimes necessary to immobilize the limb to allow healing, but care should be made to limit the risks of permanent inability for wing extension and prevention of flight. Pododermatitis, or bumblefoot, is an especially large problem in captive raptors and waterfowl species. Management is best achieved with aggressive surgical debridement with primary closure followed by postoperative protective foot casting in addition to local and systemic antimicrobial therapy.42 Oftentimes, both feet need to be bandaged, due to the risk of weight shifting onto the other limb during healing. The casts should be removed every 7 days to re-evaluate the foot.
Reptiles
Reptiles have dry skin, devoid of glands, with scales of epidermal origin arranged in regular geometric patterns. As reptiles are ectotherms, the wound healing process is highly dependent upon the environmental temperature. Lower temperatures will delay cell migration and thus delay wound healing.43 In addition just like in other species stress has a negative effect on wound healing.44 In snakes antibiotic ointments have been shown to delay wound healing of experimentally induced skin wounds, while occlusive polyurethane film (Op-Site Spray Bandage, Smith and Nephew Inc., Lachine, Quebec, Canada) resulted in more advanced wound healing.45 Consideration should be made for semiaquatic or aquatic reptiles (e.g. turtles), as those open wounds should be close primarily despite common wound healing principles. Causes of open wounds are often abscesses or abrasions secondary to poor husbandry, conspecific trauma (Figure 6), thermal burns from heated rocks or incandescent light bulbs, abnormal shedding (dysecdysis) that allows tearing of the epidermis, or trauma, especially from prey species.
SUMMARY
Wound healing is a complicated process that includes overlapping phases: hemostasis, inflammation, debridement, repair (proliferation), and remodeling. Each phase is affected by various endogenous and exogenous factors. An understanding of normal wound healing, as well as the pathogenesis of impaired or delayed healing, is critical in choosing an appropriate and successful wound management strategy. Finally, considerations of the patient species must me made when determining appropriate wound care to achieve the best possible outcome.
Key points.
General principles of wound healing are similar across species.
Selection of appropriate topical therapies and bandaging is based on the phase of wound healing and amount of exudate produced in addition to patient factors.
When addressing wounds in exotics, it is important to account for individual patient stress levels, behavior, and husbandry when considering wound management techniques and options.
Footnotes
The authors have nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Portou MJ, Baker D, Abraham D, et al. The innate immune system, toll-like receptors and dermal wound healing: A review. Vascul Pharmacol. 2015 doi: 10.1016/j.vph.2015.02.007. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 2.Ozturk F, Ermertcan AT. Wound healing: a new approach to the topical wound care. Cutan Ocul Toxicol. 2011;30:92–99. doi: 10.3109/15569527.2010.539586. [DOI] [PubMed] [Google Scholar]
- 3.Pazyar N, Yaghoobi R, Rafiee E, et al. Skin wound healing and phytomedicine: a review. Skin Pharmacol Physiol. 2014;27:303–310. doi: 10.1159/000357477. [DOI] [PubMed] [Google Scholar]
- 4.Cornell K. Wound Healing. In: Tobias KM, Johnston SA, editors. Veterinary Surgery: Small Animal. 1. Vol. 1. St. Louis: Saunders; 2012. pp. 125–134. [Google Scholar]
- 5.Fossum, Hedlund CS. Small Animal Surgery. 3. St. Louis: Mosby, Inc; 2007. Surgery of the Integumentary System; pp. 159–228. [Google Scholar]
- 6.Balsa IM, Culp WT. Wound Care. Vet Clin North Am Small Anim Pract. 2015 doi: 10.1016/j.cvsm.2015.04.009. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Franz MG, Robson MC, Steed DL, et al. Guidelines to aid in healing of acute wounds by decreasing impediments of healing. Wound Rep Regen. 2008;16:723–48. doi: 10.1111/j.1524-475X.2008.00427.x. [DOI] [PubMed] [Google Scholar]
- 8.Amsellem P. Complications of reconstructive surgery in companion animals. Vet Clin Small Anim. 2011;41:995–1006. doi: 10.1016/j.cvsm.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Tobin GR. Closure of contaminated wounds. Biologic and technical considerations. Surg Clin North Am. 1984;64:639–52. doi: 10.1016/s0039-6109(16)43380-3. [DOI] [PubMed] [Google Scholar]
- 10.Brown DC. Wound Infections and Antimicrobial Use. In: Tobias KM, Johnston SA, editors. Veterinary Surgery: Small Animal. 1. Vol. 1. St. Louis: Saunders; 2012. pp. 135–9. [Google Scholar]
- 11.Hosgood G. Open Wounds. In: Tobias KM, Johnston SA, editors. Veterinary Surgery: Small Animal. 1. Vol. 1. St. Louis: Saunders; 2012. pp. 1210–20. [Google Scholar]
- 12.Davidson JR. Current concepts in wound management and wound healing products. Vet Clin Small Anim. 2015:1–28. doi: 10.1016/j.cvsm.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Ayello EA, Cuddigan JE. Debridement: Controlling the necrotic/cellular burden. Adv Skin Wound Care. 2004;17:66–75. doi: 10.1097/00129334-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Kirshen C, Woo K, Ayello EA, et al. Debridement. A vital component of wound bed preparation. Adv Skin Wound Care. 2006;19:506–17. doi: 10.1097/00129334-200611000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Krahwinkel DJ, Boothe HW. Topical and systemic medications for wounds. Vet Clin Small Anim. 2006;36:739–57. doi: 10.1016/j.cvsm.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Fahie MA. Evidence-based wound management: a systematic review of therapeutic agents to enhance granulation and epithelialization. Vet Clin Small Anim. 2007;37:559–77. doi: 10.1016/j.cvsm.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Guthrie KM, Agarwal A, Tackes DS, et al. Antibacterial efficacy of silver-impregnated polyelectrolyte multilayers immobilized on a biological dressing in a murine wound infection model. Ann Surg. 2012;256:371–377. doi: 10.1097/SLA.0b013e318256ff99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herron M, Agarwal A, Kierski P, et al. Reduction in wound bioburden using a silver-loaded dissolvable microfilm construct. Adv Healthc Mater. 2014;3:916–28. doi: 10.1002/adhm.201300537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez-Bigas M, Cruz NI, Suarez A. Comparative evaluation of aloe vera in the management of burn wounds in guinea pigs. Plast Reconstr Surg. 1988;81:386–9. doi: 10.1097/00006534-198803000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Swaim SF, Riddell KP, McGuire JA. Effects of topical medications on the healing of open pad wounds in dogs. J Am Anim Hosp Assoc. 1992;28:499–502. [Google Scholar]
- 21.Canapp SO, Farese JP, Schultz GS, et al. The effect of topical tripeptide-copper complex on healing of ischemic open wounds. Vet Surg. 2003;32:515–23. doi: 10.1111/j.1532-950x.2003.00515.x. [DOI] [PubMed] [Google Scholar]
- 22.Matthews KA, Binnington AG. Wound management using honey. Compend Contin Educ Pract Vet. 2002;24:53–60. [Google Scholar]
- 23.Matthews KA, Binnington AG. Wound management using sugar. Compend Contin Educ Pract Vet. 2002;24:41–52. [Google Scholar]
- 24.Campbell BG. Dressings, Bandages, and splints for wound management in dogs and cats. Vet Clin Small Anim. 2006;36:759–91. doi: 10.1016/j.cvsm.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Knighton, Ciresi K, Fiegel VD, et al. Stimulation of repair in chronic, nonhealing, cutaneous ulcers using platelet-derived wound healing formula. Surg Gynecol Obstet. 1990;170:56–60. [PubMed] [Google Scholar]
- 26.Tambella AM, Attili AR, Dini F, et al. Autologous platelet gel to treat chronic decubital ulcers: a randomized, blind controlled clinical trial in dogs. Vet Surg. 2014;43:726–33. doi: 10.1111/j.1532-950X.2014.12148.x. [DOI] [PubMed] [Google Scholar]
- 27.Uneo H, Mori T, Fujinaga T. Topical formulations and wound healing applications of chitosan. Adv Drug Deliv Rev. 2001;52:105–15. doi: 10.1016/s0169-409x(01)00189-2. [DOI] [PubMed] [Google Scholar]
- 28.Campbell BG. Bandages and Drains. In: Tobias KM, Johnston SA, editors. Veterinary Surgery: Small Animal. 1. Vol. 1. St. Louis: Saunders; 2012. pp. 221–230. [Google Scholar]
- 29.Kannon GA, Garrett AB. Moist wound healing with occlusive dressings. A clinical Review. Dermatol Surg. 1995;21:583–90. doi: 10.1111/j.1524-4725.1995.tb00511.x. [DOI] [PubMed] [Google Scholar]
- 30.Morgan PW, Binnington AG, Miller CW, et al. The effect of occlusive and semi-occlusive dressings on the healing of acute full-thickness skin wounds on the forelimbs of dogs. Vet Surg. 1994;23:494–502. doi: 10.1111/j.1532-950x.1994.tb00511.x. [DOI] [PubMed] [Google Scholar]
- 31.Mans C, Guincho M, Taylor M. Application of a sustained-release silver hydrogel dressing sheet in avian wound management. Exotic DVM. 2007;9:21–4. [Google Scholar]
- 32.Dissemond J, Augustin M, Eming SA, et al. Modern wound care-practical aspects of non-interventional topical treatment of patients with chronic wounds. J Dtsch Dermatol Ges. 2014;12:541–54. doi: 10.1111/ddg.12351. [DOI] [PubMed] [Google Scholar]
- 33.Eaglstein WH. Moist wound healing with occlusive dressings: a clinical focus. Dermatol Surg. 2001;27:175–81. doi: 10.1046/j.1524-4725.2001.00299.x. [DOI] [PubMed] [Google Scholar]
- 34.Segal HC, Hunt BJ, Gilding K. The effects of alginate and non-alginate wound dressings on blood coagulation and platelet activation. J Biomater Appl. 1998;12:249–57. doi: 10.1177/088532829801200305. [DOI] [PubMed] [Google Scholar]
- 35.Swaim SF, Gillette RL, Sartin EA, et al. Effects of a hydrolyzed collagen dressing on the healing of open wounds in dogs. Am J Vet Res. 2000;61:1574–8. doi: 10.2460/ajvr.2000.61.1574. [DOI] [PubMed] [Google Scholar]
- 36.Winkler JT, Swaim SF, Sartin EA, et al. The effect of porcine-derived small intestinal submucosa product on wounds with exposed bone in dogs. Vet Surg. 2002;31:541–51. doi: 10.1053/jvet.2002.34669. [DOI] [PubMed] [Google Scholar]
- 37.Badylak SF. Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol. 2004;12:367–77. doi: 10.1016/j.trim.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 38.Ramsey DT, Pope ER, Wagner-Mann C, et al. Effects of three occlusive dressing materials on healing of full-thickness skin wounds in dogs. Am J Vet Res. 1995;56:941–9. [PubMed] [Google Scholar]
- 39.Howe LM. Current concepts in negative pressure wound therapy. Vet Clin Small Anim. 2015:1–19. doi: 10.1016/j.cvsm.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 40.Moues CM, Heule F, Hovius SE. A review of topical negative pressure therapy in wound healing: sufficient evidence. Am J Surg. 2011;201:544–56. doi: 10.1016/j.amjsurg.2010.04.029. [DOI] [PubMed] [Google Scholar]
- 41.Marin ML, Norton TM, Mettee NS. Vacuum-Assisted Wound Closure in Chelonians. In: Mader DR, Divers SJ, editors. Current Therapy in Reptile Medicine and Surgery. St. Louis: Elsevier Saunders; 2014. pp. 197–204. [Google Scholar]
- 42.Remple JD. A multifaceted approach to the treatment of bumblefoot in raptors. J Exot Pet Med. 2006;15:49–55. [Google Scholar]
- 43.Smith DA, Barker IK, Allen OB. The effect of ambient temperature and type of wound on healing of cutaneous wounds in the common garter snake (Thamnophis sirtalis) Can J Vet Res. 1988;52:120–128. [PMC free article] [PubMed] [Google Scholar]
- 44.French SS, Matt KS, Moore MC. The effects of stress on wound healing in male tree lizards (Urosaurus ornatus) General and Comparative Endocrinology. 2006;145(2):128–132. doi: 10.1016/j.ygcen.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 45.Smith DA, Barker IK, Allen OB. The effect of certain topical medications on healing of cutaneous wounds in the common garter snake (Thamnophis sirtalis) Canadian journal of veterinary research = Revue canadienne de recherche veterinaire. 1988;52(1):129–133. [PMC free article] [PubMed] [Google Scholar]