Abstract
Context:
For the follow-up of patients with idiopathic interstitial pneumonias (IIP), it is unclear which parameters of pulmonary function tests (PFT) and exercise testing would correlate best with high-resolution computed tomography (HRCT)..
Aim:
To find out the correlation of symptom scores, PFTs and exercise testing with HRCT scoring in patients diagnosed as idiopathic interstitial pneumonia.
Settings and Design:
Cross-sectional study done in pulmonary medicine outpatients department of a tertiary care hospital in South India.
Materials and Methods:
Consecutive patients who were diagnosed as IIP by a standard algorithm were included into the study. Cough and dyspnea were graded for severity and duration. Pulmonary function tests and exercise testing parameters were noted. HRCT was scored based on an alveolar score, an interstitial score and a total score. The HRCT was correlated with each of the clinical and physiologic parameters. Pearson's/Spearman's correlation coefficient was used for the correlation of symptoms and parameters of ABG, PFT and 6MWT with the HRCT scores.
Results:
A total of 94 patients were included in the study. Cough and dyspnea severity (r = 0.336 and 0.299), FVC (r = −0.48), TLC (r = −0.439) and DLCO and distance saturation product (DSP) (r = −0.368) and lowest saturation (r = −0.324) had significant correlation with total HRCT score. Among these, DLCO, particularly DLCO corrected % of predicted, correlated best with HRCT score (r = −0.721)..
Conclusion:
Symptoms, PFT and exercise testing had good correlation with HRCT. DLCO corrected % of predicted correlated best with HRCT.
KEY WORDS: Correlation, high-resolution computed tomography, idiopathic interstitial pneumonia, idiopathic pulmonary fibrosis, interstitial lung disease, pulmonary function tests
INTRODUCTION
Idiopathic interstitial pneumonias (IIP) are a heterogeneous group of diffuse parenchymal lung diseases (DPLD) characterized by lung parenchymal damage with varying patterns of inflammation and fibrosis. Idiopathic pulmonary fibrosis (IPF), earlier known as cryptogenic fibrosing alveolitis (CFA), is the most common form of IIP.[1,2]
Characteristic physiological aberrations in IPF include reductions in lung volumes, impaired single-breath diffusing capacity for carbon monoxide (DLCO) and impaired oxygenation (at rest or with exercise).[3,4] The DLCO is the most sensitive of the static pulmonary functional parameters, and may be reduced even when lung volumes are preserved. The diffusion capacity can be normalized to alveolar volume ventilated (VA) yielding the DLCO/VA ratio. Exercise testing provides a reproducible and objective marker of the extent of impairment.[4,5] Despite its limitations, due to its ease of performance, 6-minutes walk (6 MWT) test may be accepted as a quantitative method for the same.
Although HRCT is the best non-invasive method for assessing the pattern (fibrosis versus inflammation) and quantifying the extent of the disease in IIP patients at diagnosis, its frequent repetition is ill-advised because of the radiation burden and its high cost. Conventional pulmonary function tests are routinely performed in the evaluation of patients with IIP, but their correlation with the extent and progression of the disease has not been very well demonstrated.
Although there are few case series on IPF from India, these have not compared HRCT scores with PFT or symptomatology or 6 MWT. This study aims to find out the correlation between symptoms, PFT and 6 MWT with HRCT scores in patients with IIP.
MATERIALS AND METHODS
This is a cross-sectional study performed from January 2007 to May 2008 in the Pulmonary Medicine outpatients department of a tertiary care hospital in South India. The study was approved by the Institutional Review Board. The sample size was calculated based on a previous study,[6] where the correlation between HRCT score and DLCO has been found to be −0.4. Anticipating a -0.1 correlation between HRCT score and DLCO at 5% level of significance and 80% power of the study, the required sample size was found to be 80 subjects.
Consecutive patients who were diagnosed as IIP by a standard diagnostic algorithm [Figure 1] were enrolled in the study. Also, these patients if they underwent an HRCT, pulmonary function tests and 6 MWTs for ongoing assessment at least 3 months later (if within the study period) were re-enrolled into the study. The patients who were unwilling or did not undergo evaluation as stipulated by the algorithm were excluded. The patients who did not have a good quality HRCT which is required for HRCT scoring or if they had an alternate diagnosis on TBLB (trans-bronchial lung biopsy) as per algorithm were excluded from the final analysis.
Figure 1.
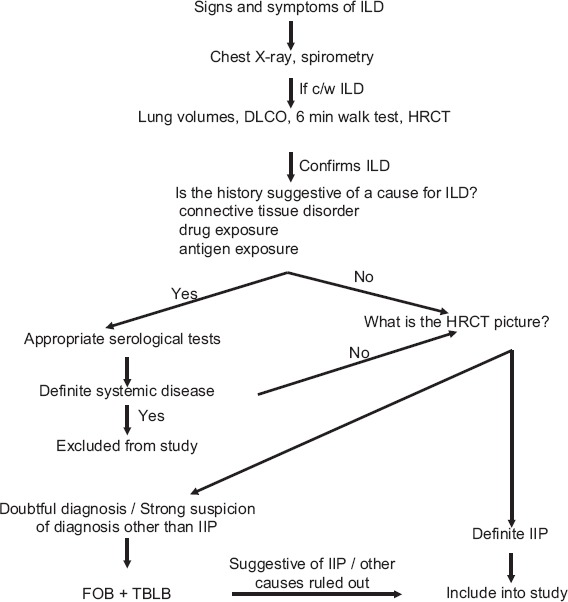
Standard diagnostic algorithm used for the diagnosis of idiopathic interstitial pneumonia
Cough severity was assessed by a visual analogue score (VAS).[7] Cough duration was recorded in months. Dyspnea was recorded in terms of modified medical research council (mMRC) score.[8] The duration was recorded in months. Physical examination was done and relevant signs and symptoms were recorded. An arterial blood gas measurement was done at rest, the PaO2 (partial pressure of oxygen in the arterial blood) was recorded and the P(A-a)O2 (alveolar arterial gradient) was calculated. PFT was standardized and done according to ATS recommendations.[9]
All the following parameters of the pulmonary function test were recorded viz., FEV1 (Forced Expiratory Volume at the end of the first second), FVC (Forced Vital Capacity), FEV1/FVC (Forced Expiratory Volume at the end of the first second as a ratio of the Forced Vital Capacity), TLC (Total Lung Capacity), DLCO (Diffusion capacity measured with Carbon Monoxide), DLCO/VA (Diffusion capacity measured with Carbon Monoxide adjusted for the alveolar volume ventilated). From the 6MWT, the distance walked in meters and lowest saturation were recorded and the distance saturation product (DSP) was calculated in m%, which is the product of the distance walked in meters and the lowest saturation recorded.
All HRCTs were performed with 1-mm thick sections at 10-mm intervals. The HRCT was scored by an experienced chest radiologist using the scoring system recommended by Gay et al.[10] Alveolar score for each lobe ranged from 0 to 5. An average was obtained for the mean total alveolar score. Interstitial score for each lobe also ranged from 0 to 5. An average was taken to be the mean total interstitial score. The total of the mean total alveolar score and the mean total interstitial score gave the mean total HRCT score.
All variables were initially analyzed descriptively. The analysis of continuous variables was carried out through observation of minimum and maximum values, and calculation of means and standard deviations. Absolute and relative frequencies were calculated for categorical variables. Symptoms, ABG, PFT and 6MWT were correlated with the HRCT scores. Pearson correlation coefficient was calculated for those parameters with a normal distribution and those which were continuous. Parameters which had a skewed distribution and those which were ranked had correlation calculated by Spearman's rho correlation coefficient.
RESULTS
The sample size required was 80. Since not all patients managed to perform DLCO successfully, the sample size was exceeded in order to try and achieve sufficient numbers with the result of this test. A total of 105 sets of data were collected from 94 patients. Seven patients had PFT and concurrent HRCT twice during the study period and two patients had these thrice during the study period and hence were included more than once into the study. Only 61 patients completed full PFT including DLCO. One patient among this was excluded as TBLB diagnosed sarcoidosis subsequently. Five patients were excluded due to a suboptimal HRCT due to motion artifacts. Finally, 55 of the 61 patients had a HRCT that was adequate for scoring.
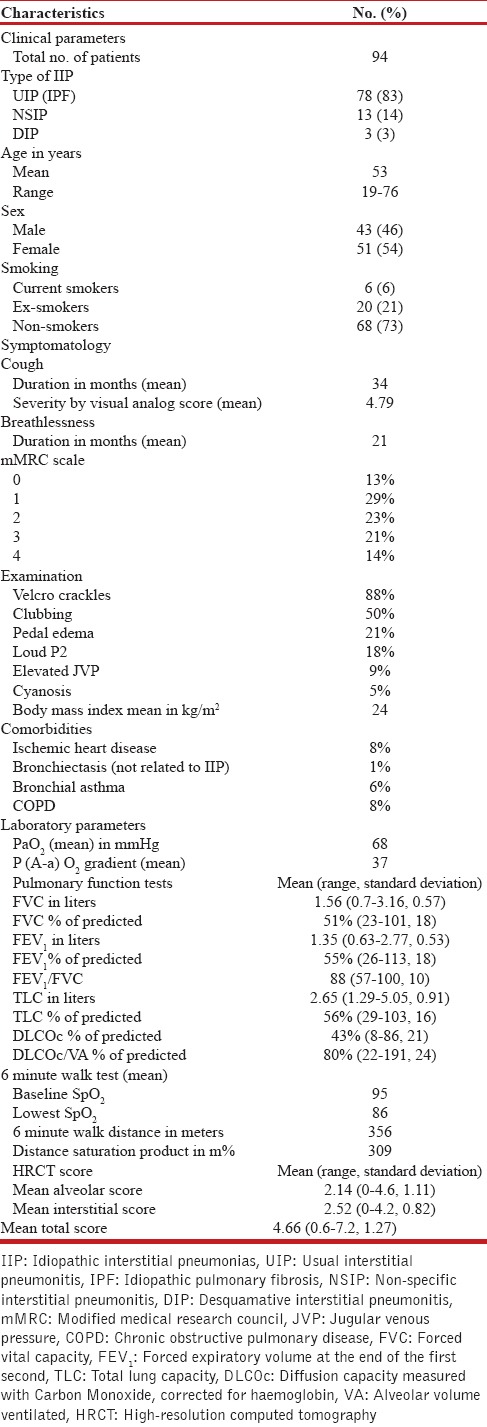
The demographic data and baseline characteristics of the 94 patients are listed in Table 1. The mean age group of our patients was 53 and 68% of them were between 41 and 60 years of age. This is at least a decade younger compared to its prevalence in the western population. There was a slight female preponderance contributed by both IPF and NSIP patients. Among the 11 patients below 41 years of age, there were six females and five males; seven of these patients had IPF, three had NSIP and one had DIP. Among the 20 patients over 60 years of age, all were IPF, except one patient with DIP; there 12 males and eight females in this group. Only 28% of the patients were current or ex-smokers. All of them had presented with cough and breathlessness but the cough seems to have preceded the breathlessness by nearly a year. Crackles were the most common examination finding and clubbing was seen in 50%.
Table 1.
Demographic data and baseline characteristics
The correlations of the symptoms, PaO2, P(A-a)O2, pulmonary function test and the 6 MWT test parameters with the HRCT alveolar scores, interstitial scores and total scores are listed in Table 2. Although the duration of cough did not have any correlation with the total HRCT score, the cough severity as assessed by a visual analog scale had modest but statistically significant correlation. Likewise, the duration of dyspnea did not correlate with the total HRCT score, but the dyspnea severity as assessed by MMRC dyspnea scale showed a statistically significant correlation, although the r value was only 0.299. The PaO2 and the PAO2 - PaO2 at rest did not have any significant correlation with the total HRCT score.
Table 2.
Correlations with HRCT scoring (‘r’ value)
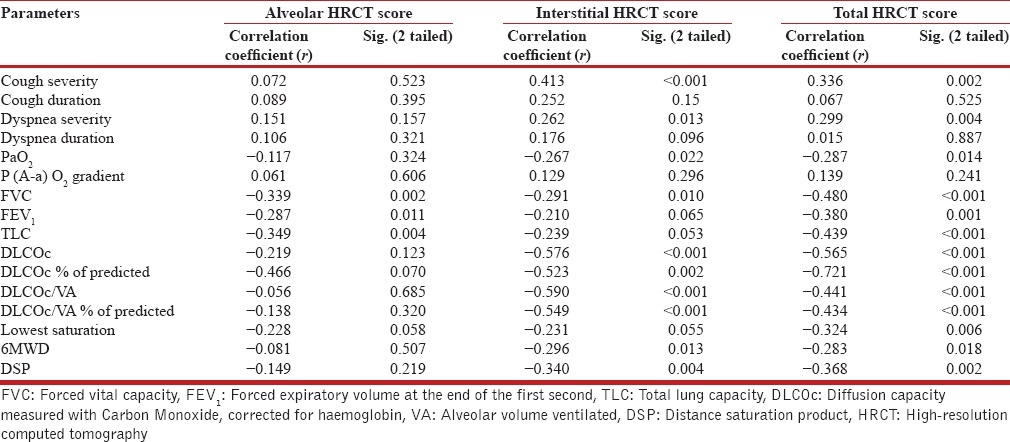
Among 6MWT parameters, the lowest O2 saturation (r = −0.353) and the distance saturation product (DSP) (r = −0.353) had a statistically significant negative correlation with the total HRCT score. Among the PFT parameters FEV1 (r = −0.38) and FVC (r = −0.48), showed statistically significant negative correlation with the total HRCT scores. FEV1/FVC (r = 0.423), a measure of obstruction showed a significant positive correlation. FVC (r = −0.48) showed the best correlation, which was superior to TLC (r = −0.439).
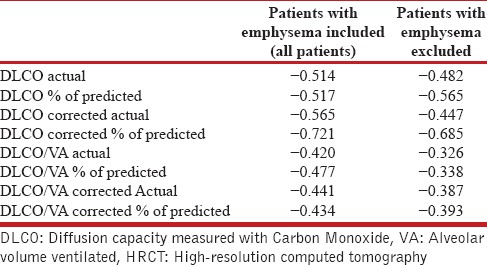
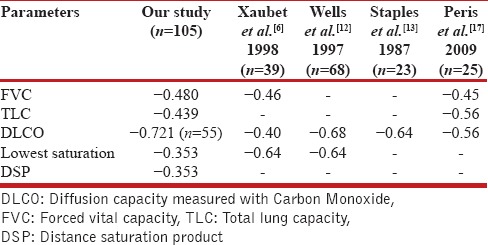
Since DLCO was the parameter that was found to correlate best with HRCT in previous studies, we analyzed this in greater detail and separately looked at correlation of DLCO, DLCO/VA, DLCOc, DLCOc/VA in actual values and as % of predicted. All these showed statistically significant negative correlation with total HRCT score with ‘r’ values above - 0.40 [Table 2]. The best correlation was seen with DLCO corrected % of predicted (r = −0.721). Correlations of DLCO with HRCT were analysed further, to see if emphysema would influence it. After excluding the patients with emphysema the correlations were similar with only modest differences and the comparisons are tabulated in Table 3.
Table 3.
Influence of excluding patients with emphysema on correlations (r value) of DLCO with HRCT
DISCUSSION
Review of the literature revealed that there are eight studies[6,11,12] published so far (the last one unpublished data), which have looked at the correlation of HRCT with pulmonary function tests and only two of these have looked at the correlation between HRCT and symptom scores. Seven of the eight studies[6,12,13,14,15,16,17] have shown good correlation and the other revealed moderate correlation between HRCT and PFT.[11] The latter study[11] has used a histogram of the HRCT to correlate (and it found kurtosis to correlate maximally with the PFT), whereas the others have used the usual HRCT scores. Of the seven studies showing good correlation between PFT parameters and HRCT, two[12,13] have shown only DLCO to correlate significantly and another[6] has shown both DLCO and FVC to correlate significantly. The other four studies[14,15,16,17] have found all the PFT parameters to correlate significantly. Of the two studies that have looked at the correlation of dyspnea with HRCT, one showed limited correlation[14] and the other significant correlation.[13] Two studies had looked at 6 MWT and its correlation with HRCT. When one of them found only modest correlation,[14] the other found good correlation with oxygen de-saturation on exercise.[12]
In a study of 39 patients by Xaubet et al.,[6] the PaO2 at peak exercise was found to correlate with ground glassing and overall HRCT with r values of 0.6 and 0.64 and P values of 0.02 and 0.01, respectively. But in our study neither PaO2 nor PAO2 - PaO2 have any significant correlation with HRCT scores.
FVC has been shown to correlate well with HRCT in two previous studies.[6,14] In the study by Xaubet et al.,[6] FVC correlated better with ground glassing (r = −0.58) than with overall score (r = −0.46) similar to our study [Table 2]. In this same study where the researchers also looked at the follow up of patients with treatment, FVC variation over a period of time significantly correlated with corresponding variations in HRCT (r = −0.51). The study by Mura et al.,[14] also found good negative correlation of both TLC and FVC with HRCT scores. In our study too we found good correlation of both FVC (r = −0.48) and TLC (r = −0.439), the former being better than the latter. Hence FVC is a PFT measure which correlates well with HRCT scores, even better than TLC.
Wells et al.,[12] with the largest sample size so far studied, found DLCO % of predicted to correlate well with HRCT of patients without emphysema (r = −0.68). Staples et al.[13] studied 23 patients and found DLCO to correlate well (r = −0.64) with HRCT (visual analogue scale of 0-100%). Our study has been able to demonstrate a better significance or a larger r value (r = −0.721) for correlation of DLCO % of predicted with HRCT. Since IIP is associated with loss of alveolar volume, correcting for alveolar volume underestimates the lung damage. Hence, DLCO correlates better with HRCT rather than DLCO/VA.
The comparative data of this study with earlier published data is shown in Table 4.
Table 4.
Comparison of the ‘r’ value with previous published data
The first limitation of our study is that it is a cross sectional study. It does not throw light on the correlations of various parameters with changes in HRCT over time. Secondly, the study was under-powered especially for correlations of DLCO with HRCT for reasons mentioned earlier.
CONCLUSIONS
This study shows that cough severity and dyspnea severity among symptoms (smaller r value), FVC, TLC, DLCO among PFT parameters and lowest oxygen saturation and DSP from among the six minute walk test have statistically significant correlation with total HRCT score in patients with idiopathic interstitial pneumonia. DLCO showed the best correlation and among the diffusion capacity measures, DLCO corrected % of predicted correlated the best with HRCT. A study which is adequately powered, also looking at correlation of changes in DLCO with changes in HRCT will be useful in ensuring that this is the best parameter that could be used in the follow-up of patients with idiopathic interstitial pneumonia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Demedts M, Wells AU, Antó JM, Costabel U, Hubbard R, Cullinan P, et al. Interstitial Lung Diseases: An epidemiological overview. Eur Respir J Suppl. 2001;32:2–16s. [PubMed] [Google Scholar]
- 2.Thomeer MJ, Costabe U, Rizzato G, Poletti V, Demedts M. Comparison of registries of interstitial lung diseases in three European countries. Eur Respir J Suppl. 2001;32:114–8s. [PubMed] [Google Scholar]
- 3.Chinet T, Jaubert F, Dusser D, Danel C, Chrétien J, Huchon GJ. Effects of inflammation and fibrosis on pulmonary function in diffuse lung fibrosis. Thorax. 1990;45:675–8. doi: 10.1136/thx.45.9.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robertson HT. Clinical application of pulmonary function and exercise tests in the management of patients with interstitial lung disease. Semin Respir Crit Care Med. 1994;15:1–9. [Google Scholar]
- 5.Watters LC, King TE, Schwarz MI, Waldron JA, Stanford RE, Cherniack RM. A clinical, radiographic, and physiologic scoring system for the longitudinal assessment of patients with idiopathic pulmonary fibrosis. Am Rev Respir Dis. 1986;133:97–103. doi: 10.1164/arrd.1986.133.1.97. [DOI] [PubMed] [Google Scholar]
- 6.Xaubet A, Agustí C, Luburich P, Roca J, Montón C, Ayuso MC, et al. Pulmonary function tests and CT scan in the management of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;158:431–6. doi: 10.1164/ajrccm.158.2.9709008. [DOI] [PubMed] [Google Scholar]
- 7.Spinou A, Birring SS. An update on measurement and monitoring of cough: What are the important study endpoints? J Thorac Dis. 2014t;6(Suppl 7):S728–34. doi: 10.3978/j.issn.2072-1439.2014.10.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishiyama O, Taniguchi H, Kondoh Y, Kimura T, Kato K, Kataoka K, et al. A simple assessment of dyspnoea as a prognostic indicator in idiopathic pulmonary fibrosis. Eur Respir J. 2010;36:1067–72. doi: 10.1183/09031936.00152609. [DOI] [PubMed] [Google Scholar]
- 9.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 10.Gay SE, Kazerooni EA, Toews GB, Lynch JP, 3rd, Gross BH, Cascade PN, et al. Idiopathic pulmonary fibrosis: Predicting response to therapy and survival. Am J Respir Crit Care Med. 1998;157:1063–72. doi: 10.1164/ajrccm.157.4.9703022. [DOI] [PubMed] [Google Scholar]
- 11.Best AC, Lynch AM, Bozic CM, Miller D, Grunwald GK, Lynch DA. Quantitative CT indexes in idiopathic pulmonary fibrosis: Relationship with physiologic impairment. Radiology. 2003;228:407–14. doi: 10.1148/radiol.2282020274. [DOI] [PubMed] [Google Scholar]
- 12.Wells AU, King AD, Rubens MB, Cramer D, du Bois RM, Hansell DM. Lone cryptogenic fibrosing alveolitis: A functional-morphologic correlation based on extent of disease on thin-section computed tomography. Am J Respir Crit Care Med. 1997;155:1367–75. doi: 10.1164/ajrccm.155.4.9105081. [DOI] [PubMed] [Google Scholar]
- 13.Staples CA, Müller NL, Vedal S, Abboud R, Ostrow D, Miller RR. Usual interstitial pneumonia: Correlation of CT with clinical, functional, and radiologic findings. Radiology. 1987;162:377–81. doi: 10.1148/radiology.162.2.3797650. [DOI] [PubMed] [Google Scholar]
- 14.Mura M, Ferretti A, Ferro O, Zompatori M, Cavalli A, Schiavina M, et al. Functional predictors of exertional dyspnea, 6-min walking distance and HRCT fibrosis score in idiopathic pulmonary fibrosis. Respiration. 2006;73:495–502. doi: 10.1159/000089656. [DOI] [PubMed] [Google Scholar]
- 15.Battista G, Zompatori M, Fasano L, Pacilli A, Basile B. Progressive worsening of idiopathic pulmonary fibrosis. High resolution computed tomography (HRCT) study with functional correlations. Radiol Med. 2003;105:2–11. [PubMed] [Google Scholar]
- 16.Chen N, Yang ZG, Yu JQ. Idiopathic pulmonary fibrosis: Correlation between helical CT findings and pulmonary function test results. Sichuan Da Xue Xue Bao Yi Xue Ban. 2004;35:94–7. [PubMed] [Google Scholar]
- 17.Peris R, Fernandez-Fabrellas E, Ramirez C, Domingo ML, Catalan P, Martinez A, et al. Correlation of a Semiquantitative HRCT score with pulmonary function tests (PFT) in idiopathic pulmonary fibrosis patients. Am J Respir Crit Care Med. 2009;179:A1117. [Google Scholar]


