Abstract
Bronchial artery embolization is the treatment of choice for the management of life-threatening massive hemoptysis. Chronic pulmonary thromboembolism (PTE) is one of the rare causes of hemoptysis. Management of hemoptysis in chronic PTE is a point of debate. In this article, we have reported one case of hemoptysis in chronic PTE managed successfully with bronchial artery embolization.
KEY WORDS: Bronchial artery embolization, hemoptysis, pulmonary thromboembolism
INTRODUCTION
Massive hemoptysis is a life-threatening medical emergency with mortality rates ranging as high as 75%.[1] Transcatheter embolization of bronchial arteries has been regarded as an effective and safe method for the management of massive hemoptysis.[2] Hemoptysis can occur due to a variety of underlying causes. Chronic pulmonary thromboembolism (PTE) is one of these causes, though its exact incidence remains unknown. Compensatory hypertrophy of bronchial arteries is known to occur in chronic PTE and pulmonary hypertension. However, the exact mechanism of hemoptysis in these patients is unclear. Bleeding due to the rupture of smaller vessels or bleeding from hypertrophied bronchial arteries are the proposed mechanisms.[3,4] Though bronchial artery embolization has been proposed to be effective in the management of hemoptysis,[5] the ideal treatment for hemoptysis in patients with chronic PTE remains uncertain. We report one case of hemoptysis in chronic PTE with pulmonary arterial hypertension (PAH) treated successfully with bronchial artery embolization.
CASE REPORT
A 30-year-old male patient presented to the emergency department of our institute with recurrent bouts of hemoptysis for 1 week, along with shortness of breath. The patient had expectoration of ~100 mL of fresh blood/day. On examination, he was found to have tachycardia (pulse rate: 100 bpm) and tachypnea (respiratory rate: 30 breaths/min) with decreased oxygen saturation (85% in room air). The patient underwent computed tomography (CT) and bronchial angiography that showed two bronchial arteries on the right side, which were hypertrophied and tortuous (measuring ~2.6 mm and 2.4 mm, respectively, in maximum caliber) [Figure 1a]. The left bronchial artery was normal. No significant nonbronchial systemic collateral was seen. In addition, there was a thrombus in the right pulmonary artery, extending from its origin till the subsegmental branches [Figure 1b]. The right pulmonary artery was reduced in caliber with the dilated main and left pulmonary arteries. Patchy areas of mosaic attenuation were also seen in bilateral lungs. Two-dimensional echocardiogram (2D ECHO) was done for the patient that showed severe PAH with dilated right atrium and ventricle. On bronchoscopy, active bleeding with clots was seen in the segmental bronchus of the right lower lobe.
Figure 1.
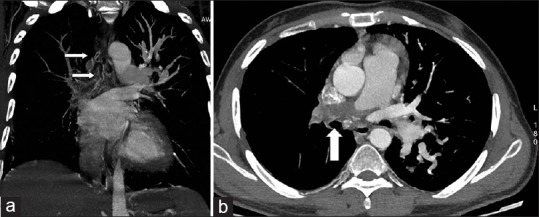
(a, b) Coronal maximum intensity projection (MIP) images of CT bronchial angiography showing hypertrophied right bronchial arteries (arrows in a). One of the bronchial arteries was arising from the intercostobronchial trunk from the descending aorta (not shown here). Origin of the second right bronchial artery was, however, not clear on CT angiography. A thrombus was seen in the right pulmonary artery (arrow in b) extending till the subsegmental branches
The patient was taken up for bronchial angiography. Selective run showed hypertrophied and tortuous right intercostobronchial trunk [Figure 2]. The second bronchial artery was being reconstituted by the internal mammary artery and was hypertrophied [Figure 3]. Both the bronchial arteries were embolized with polyvinyl alcohol (PVA) (500-700 μm) and gelfoam slurry. No other significant systemic collateral was identified on diagnostic runs of the bilateral subclavian arteries. The procedure was uneventful. Postprocedure improvement in oxygen saturation was seen with a decrease in oxygen requirement. No fresh episode of hemoptysis occurred. The patient was started on anticoagulation for chronic PTE and was discharged.
Figure 2.
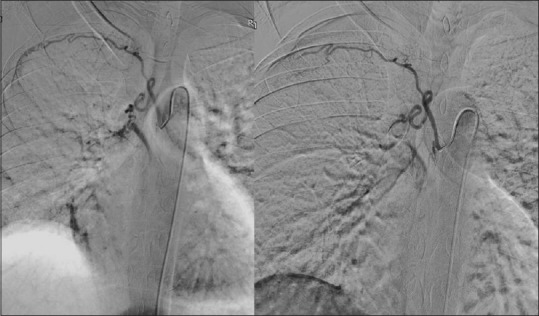
Digital subtraction angiogram of the right intercostobronchial trunk (anteroposterior projection) showing hypertrophied and tortuous bronchial artery. Embolization was done using PVA- gelfoam slurry. Postembolization angiogram showed no opacification of the distal bronchial artery (image on the right side)
Figure 3.

Digital subtraction angiogram of the right internal mammary artery showed hypertrophied second right bronchial artery arising from the internal mammary artery. This bronchial artery was embolized using PVA-gelfoam slurry after selective cannulation
DISCUSSION
Chronic PTE is associated with compensatory hypertrophy of the bronchial arteries and bronchopulmonary collaterals.[6,7] Increased incidence of bronchial artery hypertrophy on CT angiography has been reported in chronic PTE and PAH.[8] Though hemoptysis can occur due to hypertrophied bronchial arteries secondary to any cause, its exact incidence in chronic PTE is unknown. One systemic review of the literature reported chronic PTE as a cause of moderate-to-massive hemoptysis in 0.1% of cases. PAH without PTE was responsible for hemoptysis in 0.2% of cases.[5] Very little is known about the management of hemoptysis in patients with chronic PTE.
We report one case in which bronchial artery embolization was successful in managing hemoptysis in a patient with chronic PTE with PAH. Reesink et al. reported two cases of chronic PTE with massive hemoptysis treated with bronchial artery embolization. One patient was successfully treated while the other patient continued to have active hemoptysis due to collaterals from the subclavian artery. Reembolization was carried out for this patient but the patient died due to right ventricular failure. It was suggested that due to the requirement of anticoagulation for PTE, even mild hemoptysis in these patients should be offered immediate intervention.[5] However, another study reported the failure of bronchial artery embolization to prevent hemoptysis in a patient with chronic thromboembolic PAH.[9]
In chronic PTE, there is a propensity for the formation of thromboemboli. At the same time, these patients have a tendency to bleed from hypertrophied bronchial arteries. The management of hemoptysis in chronic PTE patients poses a therapeutic dilemma. Even mild hemoptysis in these patients should be given prompt treatment due to the underlying risk of progression to massive hemoptysis due to the ongoing anticoagulation therapy.[5] However, very limited literature is available on the management of hemoptysis in chronic PTE. No study has been carried out to evaluate the long-term effect of bronchial artery embolization in preventing hemoptysis. Also, the precise mechanism of hemoptysis in chronic PTE is still not clear. Thus, further studies are required to establish the role of bronchial artery embolization in chronic PTE.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Cahill BC, Ingbar DH. Massive hemoptysis. Assessment and management. Clin Chest Med. 1994;15:147–67. [PubMed] [Google Scholar]
- 2.Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: A comprehensive review. Radiographics. 2002;22:1395–409. doi: 10.1148/rg.226015180. [DOI] [PubMed] [Google Scholar]
- 3.Diller GP, Gatzoulis MA. Pulmonary vascular disease in adults with congenital heart disease. Circulation. 2007;115:1039–50. doi: 10.1161/CIRCULATIONAHA.105.592386. [DOI] [PubMed] [Google Scholar]
- 4.Broberg CS, Ujita M, Prasad S, Li W, Rubens M, Bax BE, et al. Pulmonary arterial thrombosis in Eisenmenger syndrome is associated with ventricular dysfunction, neurohormonal activation, and poorer exercise capacity. Circulation. 2004;110:497. [Google Scholar]
- 5.Reesink HJ, van Delden OM, Kloek JJ, Jansen HM, Reekers JA, Bresser P. Embolization for hemoptysis in chronic thromboembolic pulmonary hypertension: Report of two cases and a review of the literature. Cardiovasc Intervent Radiol. 2007;30:136–9. doi: 10.1007/s00270-005-0382-8. [DOI] [PubMed] [Google Scholar]
- 6.Endrys J, Hayat N, Cherian G. Comparison of bronchopulmonary collaterals and collateral blood flow in patients with chronic thrombo-embolic and primary pulmonary hypertension. Heart. 1997;78:171–6. doi: 10.1136/hrt.78.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orell SR, Hultgren S. Anastomoses between bronchial and pulmonary arteries in pulmonary thromboembolic disease. Acta Pathol Microbiol Scand. 1966;67:322–38. doi: 10.1111/apm.1966.67.3.322. [DOI] [PubMed] [Google Scholar]
- 8.Remy-Jardin M, Duhamel A, Deken V, Bouaziz N, Dumont P, Remy J, et al. Systemic collateral supply in patients with chronic thromboembolic and primary pulmo-nary hypertension: Assessment with multi-detector row helical CT angiography. Radiology. 2005;235:274–81. doi: 10.1148/radiol.2351040335. [DOI] [PubMed] [Google Scholar]
- 9.Petraco R, Dimopoulos K, Rubens M, Gatzoulis MA. Bronchial artery embolization for pulmonary arterial hypertension and recurrent haemoptysis. Am J Cardiol. 2008;101:1064–5. doi: 10.1016/j.amjcard.2007.11.062. [DOI] [PubMed] [Google Scholar]


