Abstract
Closed pleural biopsy used to be a popular method of evaluation of pleural effusion. With the advent of thoracoscopy, this valuable method is being neglected. Studies have shown that closed pleural biopsy especially done with image guidance has high yield and low complication rate as compared to thoracoscopy. Given the ease of the procedure and the less cost involved, imaged guided closed pleural biopsy should be considered as the initial diagnostic step in undiagnosed pleural biopsy especially in developing countries with high prevalence of tuberculosis.
KEY WORDS: Closed pleural biopsy, malignant pleural effusion, pleural tuberculosis, thoracoscopy
Closed pleural biopsy (CPB) has been the investigation of choice in the diagnosis of the etiology of pleural effusions for many decades. With the advent of medical thoracoscopy (MT) in the last decade, CPB has taken a beating. The main reason is the increased yield with MT as compared to CPB. Increasingly, fewer pulmonologists are performing CPB and hence, it is becoming a “lost art.” But is the onslaught of MT over CPB justified?
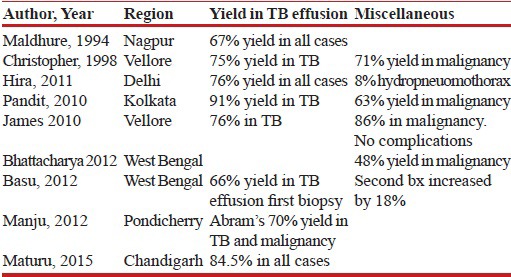
The list of published literature from India [Table 1], though not exhaustive, shows that CPB is widely being performed throughout the length and breadth of India.[1,2,3,4,5,6,7,8,9]
Table 1.
Yield of closed pleural biopsy in various series from India
YIELD
Tuberculosis (TB) continues to be a major cause of pleural effusion in developing countries such as India and the yield of CPB in TB effusion is 66–91% in various series from India.[1,2,3,4,5,6,7,8,9] A second biopsy increases the yield by 18%. In malignancy, the yield of CPB is 63–86%.
Results from a randomized controlled trial from India shows that MT has a diagnostic yield of 86.2% with complication rate of 10.3% compared to the diagnostic yield of 62.1% and complication rate of 17.2% respectively in the CPB group.[10] However, the hospital stay in the MT group was 9 days more than the CPB group.
In this era when the practice of medicine is based on established guidelines, transthoracic ultrasound (US) is suggested routinely for the evaluation of pleural effusion. This facility is ubiquitous and the sonography of pleural effusion is easy to learn. CPB should not be equated to blind pleural biopsy. For optimal safety and increased yield, CPB should be performed under image guidance. Metintas et al. compared MT- and computed tomography (CT)-guided Abrams CPB for the diagnosis of patients with pleural effusions.[11] There was no significant difference in the yield. There was no difference in sensitivities based on the cause of effusion and CT findings of pleural thickening. The complication rates were low in both the arms.
The sensitivities of various procedures for malignant pleural effusion were compared by Koegelenberg et al.[12] The sensitivity of US-guided CPB was 77% as compared to 95% in the case of thoracoscopy. When combined with the pleural fluid analysis, the sensitivities were 83% and 96% in CPB and thoracoscopy, respectively, a difference of only 13%. When we consider CT-guided biopsy, the difference between MT and CPB is only 6%. This shows that the use of image-guided CPB has a comparable yield.
Sensitivity of image-guided CPB for tubercular pleural effusion is 80%.[12] TB is a major cause of pleural effusion in India. If the symptom profile is typical of TB and the analysis shows exudative lymphocytic pleural effusion with high adenosine deaminase (ADA) or interferon, a presumptive diagnosis of tubercular pleural effusion can be made. If the fluid analysis is not typical for TB, then CPB would be a prudent first step.
COST
A major advantage of CPB in a resource-limited country is the cost. Reusable Abram's pleural biopsy costs around  1,700 while the cost of rigid thoracoscope will be
1,700 while the cost of rigid thoracoscope will be  5 lakhs and that of semi-rigid thoracoscope will be approximately
5 lakhs and that of semi-rigid thoracoscope will be approximately  12 lakhs excluding the cost of monitor and processor.
12 lakhs excluding the cost of monitor and processor.
Total cost that the patient will incur for the biopsy will be about  500 for CPB, whereas in thoracoscopy the cost may range from
500 for CPB, whereas in thoracoscopy the cost may range from  15,000 to
15,000 to  70,000 as it requires hospitalization of the patient. MT in some centers is performed in operative theaters under general anesthesia, which further adds to the cost.[13]
70,000 as it requires hospitalization of the patient. MT in some centers is performed in operative theaters under general anesthesia, which further adds to the cost.[13]
PROCEDURE
CPB is an outpatient procedure. It is customary to monitor the patient for 4 h before he/she is sent home. But MT needs hospitalization. The patient can be discharged depending upon the rapidity of lung expansion. It can vary from a few hours to many days. In some patients after introduction of the pneumothorax, the lung does not expand despite giving suction. Such patients with trapped lungs are difficult to manage. If the tube is removed without lung expansion, there is a chance of reaccumulation and secondary infection.
The technique of CPB can be easily learned. Five supervised CPB procedures followed by five biopsy procedures per year are suggested to be adequate for competency,[14] whereas the learning curve of MT is steep, with the recommendation of initial performance of at least 20 supervised procedures.[14]
The procedure per se is much more complicated in MT as compared to CPB. CPB can be performed even if there are pleural adhesions. It can be done even in dyspneic patients in a sitting posture. Adequate pleural effusion or potential pleural space is a prerequirement for MT. The patient must also be stable to lie for at least 30 min in the lateral position. Since one lung is collapsed during MT, the patient should have a stable cardiorespiratory status to withstand unilateral lung ventilation. Hence, MT becomes a risky procedure in those with bilateral lung disease and cardiac failure. Postprocedure care is very important in the case of MT. The chest tube needs to be connected meticulously to an underwater seal and care should be taken to keep the chest tube wound site, tubes, and collecting chamber sterile. Repeated chest x-rays are necessary after MT till the lung expands and then the chest tube needs to be removed in a sterile manner by trained personnel. The patient has to return to the physician for suture removal after a few days. CPB is devoid of all these paraphernalia.
COMPLICATIONS
Complications related to CPB include hydropneumothorax in 8% and bleeding in 2% of the patients.[9,15,16] These are comparable to MT. These complications can be further decreased by using image guidance. It is interesting to remember that the incidence of hydropneumothorax after MT is 100%, although it is intentional! MT is a much more painful procedure and requires more sedatives or analgesics as compared to CPB. In the largest series from India by Maturu et al., MT was associated with mortality rate and complication rate of 0.37% and 5.6%, respectively, whereas the complication rate in case of CPB was 8.3% with no mortality.[9]
CONCLUSIONS
Given the advantages of CPB, MT should be reserved to select cases of exudative pleural effusion where the fluid analysis and CPB are noncontributory. We Indian pulmonologists, especially keeping the economic factors in mind, should not fall for the glamor of MT though it is true that many pulmonologists in India are jumping on the bandwagon of MT and CPB is becoming a skill of the past. CPB has become what one of the authors has called “victim of Western advancement.”[17]
In patients with undiagnosed exudative pleural effusion, performing CPB will provide the diagnosis in nearly 80% of the cases. Only for the remaining 20% in whom CPB is nondiagnostic, the more invasive and costly intervention of MT should be considered. The delay in diagnosis in this small percentage of cases would only be a few days.
Evidence-based practice is the need of the hour. With evidence of CPB being easier and safe with a yield comparable to MT, image-guided CPB should be the first diagnostic intervention of choice. The availability of an modern and costlier instrument does not always justify its use.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Maldhure BR, Bedarkar SP, Kulkarnl HR, Paplnwar SP. Pleural biopsy and adenosine deaminase in pleural fluid for the diagnosis of tubercular pleural effusion. Ind J Tub. 1994;41:161–5. [Google Scholar]
- 2.Christopher DJ, Peter JV, Cherian AM. Blind pleural biopsy using a Tru-cut needle in moderate to large pleural effusion--an experience. Singapore Med J. 1998;39:196–9. [PubMed] [Google Scholar]
- 3.Hira HS, Ranjan R. Role of percutaneous closed needle pleural biopsy among patients of undiagnosed exudative pleural effusion. Lung India. 2011;28:101–4. doi: 10.4103/0970-2113.80319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandit S, Chaudhuri AD, Datta SB, Dey A, Bhanja P. Role of pleural biopsy in etiological diagnosis of pleural effusion. Lung India. 2010;27:202–4. doi: 10.4103/0970-2113.71941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.James P, Gupta R, Christopher DJ, Balamugesh T. Evaluation of the diagnostic yield and safety of closed pleural biopsy in the diagnosis of pleural effusion. Indian J Tuberc. 2010;57:19–24. [PubMed] [Google Scholar]
- 6.Bhattacharya S, Bairagya TD, Das A, Mandal A, Das SK. Closed pleural biopsy is still useful in the evaluation of malignant pleural effusion. J Lab Physicians. 2012;4:35–8. doi: 10.4103/0974-2727.98669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basu A, Chakrabarti I, Ghosh N, Chakraborty S. A clinicopathological study of tuberculous pleural effusion in a tertiary care hospital. Ann Trop Med Public Health. 2012;5:168–72. [Google Scholar]
- 8.Manju R, Venkateswara Babu R, Vinod Kumar S, Badhe BA. Pleural biopsy in exudative effusions-A comparative study using Abram's and Cope Needles. World J Med Sci. 2012;7:68–71. [Google Scholar]
- 9.Maturu VN, Dhooria S, Bal A, Singh N, Aggarwal AN, Gupta D, et al. Role of medical thoracoscopy and closed-blind pleural biopsy in undiagnosed exudative pleural effusions: A single-center experience of 348 patients. J Bronchology Interv Pulmonol. 2015;22:121–9. doi: 10.1097/LBR.0000000000000145. [DOI] [PubMed] [Google Scholar]
- 10.Haridas N, Suraj KP, Rajagopal TP, James PT, Chetambath R. Medical thoracoscopy vs closed pleural biopsy in pleural effusions: A randomized controlled study. J Clin Diagn Res. 2014;8:MC01–4. doi: 10.7860/JCDR/2014/7476.4310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Metintas M, Ak G, Dundar E, Yildirim H, Ozkan R, Kurt E, et al. Medical thoracoscopy vs CT scan-guided Abrams pleural needle biopsy for diagnosis of patients with pleural effusions: A randomized, controlled trial. Chest. 2010;137:1362–8. doi: 10.1378/chest.09-0884. [DOI] [PubMed] [Google Scholar]
- 12.Koegelenberg CF, Diacon AH. Pleural controversy: Close needle pleural biopsy or thoracoscopy-which first? Respirology. 2011;16:738–46. doi: 10.1111/j.1440-1843.2011.01973.x. [DOI] [PubMed] [Google Scholar]
- 13.Prabhu VG, Narasimhan R. The role of pleuroscopy in undiagnosed exudative pleural effusion. Lung India. 2012;29:128–30. doi: 10.4103/0970-2113.95304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ernst A, Silvestri GA, Johnstone D American College of Chest Physicians. Interventional pulmonary procedures: Guidelines from the American College of Chest Physicians. Chest. 2003;123:1693–717. doi: 10.1378/chest.123.5.1693. [DOI] [PubMed] [Google Scholar]
- 15.Hooper C, Lee YC, Maskell N BTS Pleural Guideline Group. Investigation of a unilateral pleural effusion in adults: British thoracic society pleural disease guideline 2010. Thorax. 2010;65(Suppl 2):ii4–17. doi: 10.1136/thx.2010.136978. [DOI] [PubMed] [Google Scholar]
- 16.Pereyra MF, San-José E, Ferreiro L, Golpe A, Antúnez J, González-Barcala FJ, et al. Role of blind closed pleural biopsy in the management of pleural exudates. Can Respir J. 2013;20:362–6. doi: 10.1155/2013/731352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dutt N, Aggarwal D. Closed needle pleural biopsy: A victim of western advancement? Lung India. 2011;28:322. doi: 10.4103/0970-2113.85750. [DOI] [PMC free article] [PubMed] [Google Scholar]


