Abstract
Background:
Pregnant female patients with vaginal bleeding in the first trimester are seen commonly in the Emergency Department (ED) at the University Hospital of the West Indies (UHWI), Kingston, Jamaica. The protocol for the management of these patients requires that they have a sonographic evaluation performed for the purpose of localizing the pregnancy where possible, to assist with determining the risk for an ectopic pregnancy. The ultrasound examinations are performed in the radiology department.
Objective:
This retrospective study was conducted to evaluate how long patients wait for a pelvic ultrasound. We also sought to establish how many patients had ultrasound findings that would have allowed safe discharge home.
Methods:
The records of 150 patients seen in the six-month period from January 1 to July 30, 2008 were examined. Data were extracted pertaining to age, time to see an emergency room doctor, time taken for ultrasound examination to be obtained from the radiology department and the ultrasound findings.
Result:
Fifty-four per cent presented to the Emergency Department with a complaint of vaginal bleeding and abdominal pain, 29% with bleeding only, 16% with abdominal pain only and one with syncope. One hundred and sixteen of the patients enrolled had an ultrasound performed at UHWI. The average waiting time for an ultrasound was 3.8 ± 2.5 hours. The majority (66/116) of the patients had an intrauterine pregnancy (IUP) demonstrated on ultrasound. Twenty-nine had no IUP, free fluid or adnexal mass. These 95 patients would likely have been discharged home. Ten patients had an adnexal mass with or without free fluid, and ten had free fluid only on ultrasound. One patient was found to have a definite ectopic pregnancy. These 21 patients would have been referred for evaluation by the obstetrician on call for further management.
Conclusion:
The majority of patients had sonographic findings that would have allowed safe and timely discharge from the Emergency Department had ultrasound been available at the point of care.
Keywords: Pelvic sonography, vaginal bleed, waiting times
Abstract
Antecedentes:
Las pacientes embarazadas con sangrado vaginal en el primer trimestre son atendidas comúnmente en el Departamento de Emergencia (DE) del Hospital Universitario de West Indies (HUWI), Kingston, Jamaica. El protocolo para el tratamiento de estas pacientes requiere que se hagan una evaluación ecográfica con el fin de localizar el embarazo donde quiera que esté, y ayudar a determinar el riesgo de un embarazo ectópico. Los exámenes de ultrasonido se realizan en el Departamento de Radiología.
Objetivo:
Este estudio retrospectivo se realizó con el propósito de evaluar cuánto tiempo las pacientes esperan por un ultrasonido pélvico. También intentamos determinar cuántas pacientes tuvieron resultados ecográficos que habrían permitido que se les diera de alta para regresar seguras a su casa.
Métodos:
Se examinaron las historias de 150 pacientes atendidas en el período de seis meses desde el 1ero de enero al 30 de julio de 2008. Se extrajeron datos en relación con la edad, el tiempo para ver a un médico de emergencia, el tiempo necesario para hacerse un examen en el Departamento de Radiología y obtener los resultados del ultrasonido.
Resultado:
El cincuenta y cuatro por ciento acudió al Departamento de Emergencia aquejadas de sangramiento vaginal y dolor abdominal, el 29% con sangramiento vaginal solamente, 16% con dolor abdominal solamente, y una con un síncope. A ciento dieciséis de las pacientes inscritas se les hizo un ultrasonido en UHWI. El tiempo de espera promedio para un ultrasonido fue 3.8 ± 2.5 horas. La mayoría (66/116) de las pacientes tuvo un embarazo intrauterino (EIU) comprobado por ultrasonido. Veintinueve no tuvieron EIU, ni líquido libre o masa anexial. A estas 95 pacientes probablemente se les hubiera dado de alta. Diez pacientes tuvieron una masa anexial con o sin líquido libre, y diez tuvieron líquido libre sólo en el ultrasonido. Se halló que una paciente tenía un embarazo ectópico definido. Estas 21 pacientes habrían sido remitidas para evaluación por el obstetra de guardia a fin de que recibieran tratamiento ulterior.
Conclusión:
La mayoría de las pacientes tuvieron resultados ecográficos que habrían permitido que se les diera de alta del Departamento de Emergencias de manera segura y oportuna, si hubiera habido servicio de ultrasonido en el lugar donde se les atendió.
INTRODUCTION
Women in the first trimester frequently visit the Emergency Department (ED) with abdominal pain, vaginal bleeding or both. The current protocol at the University Hospital of the West Indies (UHWI) mandates sonographic evaluation for all females with vaginal bleeding in the first trimester. The aim is to aid early detection of ectopic pregnancy prior to tubal rupture, and prevent life-threatening haemorrhage. It is estimated that 8% of all pregnant ED patients have an ectopic pregnancy (1–4). Another concern with patients who present with lower abdominal pain or vaginal bleeding in early pregnancy is fetal viability. The history and physical examination are often not sufficiently sensitive to allow clear differentiation between normal or abnormal intrauterine pregnancies (IUPs) and ectopic gestations, reinforcing the value of imaging in this category of patients. The early identification of a normal gestation by sonography also provides a great deal of reassurance especially to patients with a bad obstetric history. Fifteen per cent of patients with an IUP and cardiac activity seen on ED ultrasound will go on to have an abortion (5). Efficient sonography can improve the speed and accuracy of diagnosis of ectopic pregnancy and allow for early definitive therapeutic measures. The rate of ectopic pregnancy in Jamaica is one in 28 pregnancies and it is the third leading cause of maternal mortality in our population, accounting for 10% of maternal deaths (6). A study done at the Radiology Department of the UHWI showed that 69% of patients with suspected ectopic pregnancy had positive findings on ultrasound (7). Many emergency physicians now perform limited pelvic sonography in the Emergency Department (4, 8). The use of ED ultrasound for screening purposes has led to improved patient satisfaction, and reduced time to diagnosis and definitive treatment (9).
Many residency programmes in the United States of America (USA) include ED sonography training; this has been incorporated into the guidelines of the American College of Emergency Physicians (8). There is strong evidence that with appropriate training, ED sonography performed by emergency physicians can safely allow rapid therapeutic decisions and identify patients in need of operative intervention (10). The sensitivity of emergency physician-performed pelvic ultrasonography for the detection of ectopic pregnancy is high (94-99%) when the presence of a viable IUP is used to rule out an ectopic pregnancy (4, 11).
It was postulated that the availability of portable ultrasound in the ED at UHWI would shorten the waiting times for pelvic sonography in women presenting with first trimester abdominal pain and/or vaginal bleeding, allowing for safe and rapid disposition. The objectives of this study were to examine women with first trimester bleeding and/or abdominal pain to evaluate:
the waiting times for consultation with the emergency physician
time taken to obtain an ultrasonographic report from the Radiology Department
the spectrum as it relates to final diagnosis
the proportion of patients who could have been discharged early and safely had the modality been available in the ED
SUBJECTS AND METHODS
A retrospective analysis was conducted of all consecutive pregnant patients presenting to the ED with first trimester vaginal bleeding, abdominal pain or syncope between January 1 and June 30, 2008. The list of patients was retrieved from the Emergency Department logbook. The dockets were then obtained from the medical records library. Data regarding patients' presenting symptoms, last menstrual period, gestational age, time taken to see the ED physician, time taken to obtain radiology department sonography as well as the sonographic findings, final clinical diagnosis in the ED and the patients' disposition were all obtained from the dockets and review of ultrasound records.
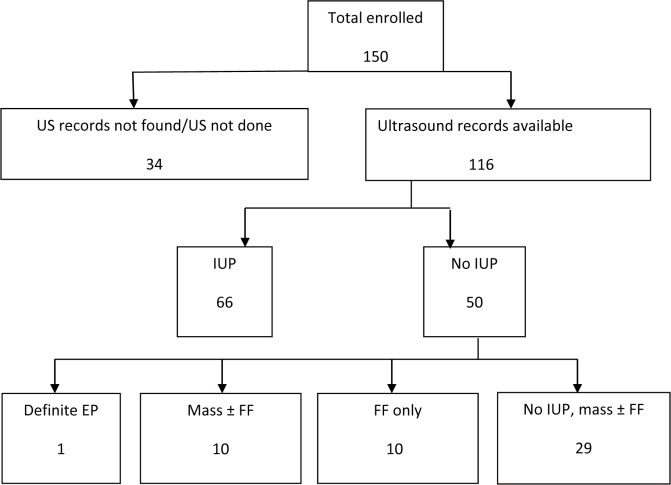
Patients were included if they had a positive ß human chorionic gonadotropin (ßhCG) with a history of syncope, vaginal bleeding and/or abdominal pain. Patients whose gestational age, calculated based on their reported last menstrual period (LMP), was greater than 12 weeks, or having vaginal bleeding as a result of dilatation and curettage were excluded. The study population was investigated with trans-abdominal and/or trans-vaginal ultrasound scans as deemed necessary by the radiologist on duty. Patients were stratified into two groups according to whether or not there was sonographic evidence of an IUP. An IUP was defined as the presence of a gestational sac with fetal pole or yolk sac, or both on ultrasound images. Those with no evidence of an IUP were further divided into four groups: (i) definitive ectopic pregnancy, (ii) adnexal mass ± free fluid, (iii) free fluid only and (iv) no free fluid (Figure). A definite ectopic pregnancy was defined as the presence of an echogenic ring-like structure outside the uterus with an obvious fetal pole or yolk sac.
Figure. Flowchart showing assignment of patients enrolled and ultrasound findings.
US = ultrasound, IUP = intrauterine pregnancy, EP = ectopic pregnancy, FF = free fluid
The waiting time for consultation was calculated as the time between registration and the time that the patient was seen by the emergency room doctor. The waiting time to obtain the ultrasound was the time interval from the time the ED doctor saw the patient to actually getting the ultrasound. The latter was retrieved from the ultrasound reports as the time is recorded on the ultrasound images. Data were analysed using the SPSS version 14 statistical programme.
RESULTS
During the six-month period, a total of 150 patients were enrolled. The age of the patients ranged from 14 to 44 years. The mean age was 28.9 years with 50% of the population being 30 years and over. Approximately 41% of patients were aged 20-29 years, and only 9.3% were less than 20 years old. Fifty-four per cent of patients presented to the ED with a complaint of vaginal bleeding and abdominal pain, 29% with bleeding only and 16% with abdominal pain only. One patient reported syncope, accounting for less than one per cent of those studied.
Data were available for 125 patients with respect to the time taken for the initial consultation with the ED physician. The average waiting time for consultation was 1.7 ± 2.0 hours with a range of 0.95 to 12.6 hours, indicating that some patients were seen and evaluated before being registered.
Of the 150 patients recruited, 116 (77.3%) had an ultrasound performed. Thirty patients had no ultrasound performed, and data were missing for four. Data were available for only 73 patients with respect to waiting time for ultrasound due to incomplete documentation. The average time for patients to obtain an ultrasound was 3.8 ± 2.5 hours, with a range of 0.88 to 16.3 hours. Of those 116 patients who had an ultrasound performed, 66 (56.9%) showed evidence of an IUP. Of the remaining 50 patients with no evidence of IUP, one patient had sonographic evidence of an ectopic pregnancy, 10 patients had an adnexal mass with or without free fluid, 10 showed free fluid only and 29 showed no evidence of an adnexal mass or free fluid (Table).
Table. Ultrasound findings in pregnant patients presenting with vaginal bleeding and/or abdominal pain.
| Ultrasound finding | Number of patients (%) |
|---|---|
| Intrauterine pregnancy (IUP) | 66 (56.9) |
| No IUP, definite ectopic pregnancy | 1 (0.1) |
| No IUP, adnexal mass ± free fluid | 10 (8.6) |
| No IUP, free fluid only | 10 (8.6) |
| No IUP, no free fluid | 29 (25.0) |
Records were found for 148 of the 150 patients studied. Of those 148 patients, 43 (28.7%) had a final clinical diagnosis of threatened abortion, 37 (24.7%) had incomplete abortion, five (3.3%) had a complete abortion, five (3.3%) an inevitable abortion and there was one missed abortion; 11 (7.3%) had findings of an unruptured ectopic pregnancy and nine (6%), that of an ectopic pregnancy. Seventeen patients (11.3%) where assessed as having a normal intrauterine gestation. Other recorded clinical diagnoses included blighted ovum (one), urinary tract infection in pregnancy (two), early pregnancy (eight) and cervicitis (one). Eight records were available but had no recorded clinical diagnosis.
DISCUSSION
Several studies have shown that emergency physicians can perform limited sonographic evaluations that would allow patients to be categorized in a manner similar to this study and facilitate timely treatment decisions. The findings of this study are quite significant. Approximately 56% (66/116) of those who had ultrasound done had IUP diagnosed and would likely have been discharged home. Fifty-eight per cent (n = 29) who had no IUP on ultrasound also had no free fluid and would have likely been discharged home to be followed-up by the gynaecologist in 24-48 hours with serum ßhCG results, in keeping with institutional practice standards. Thus, a total of 95 of the 150 patients studied could have been discharged home safely from the ED with significant reduction in waiting time had sonography been available at the bedside for use during their examination.
Of concern is the long average waiting time for patients with first trimester vaginal bleeding and/or abdominal pain to see an ED physician. The data indicate that some patients were seen before registration. However, some took as long as 12.6 hours to be seen. The long waiting time to obtain ultrasound is also a matter that requires examination. The average waiting time for an ultrasound from the radiology department was 3.8 hours with an upper range of 16.3 hours. The results of this study suggest that significant benefit would accrue from the availability of ultrasound at the bedside in the emergency room. Several studies have shown that emergency physicians can be trained to perform limited sonographic evaluations that would allow the patient to be categorized in a similar manner to this study, and facilitate timely treatment decisions (9, 11). Ultrasound training is now being incorporated into medical school curricula in North America and Europe and it has been shown that with limited training, these skills are retained (12). At present, only one of our consultants is fully trained in sonography. Five others have done ultrasound courses and are capable of performing these scans. The residents in the Emergency Medicine programme perform scans during their radiology rotation. One study estimates that ultrasound is available for use by emergency physicians on a 24-hour basis in only 19% of community EDs in the USA. Fifteen per cent have a machine for use in some capacity and 66% have no access to ED sonography (13). No functional ultrasound machine is available in the emergency room at UHWI. This is a major limiting factor. The acquisition of a suitable ultrasound machine and ongoing training in limited sonography would allow the emergency physicians in training to gain additional expertise so that they can introduce ED ultrasound to emergency departments across the island.
Ultrasounds were not performed in 30 of the 150 patients studied. Unfortunately, the reasons for not doing the ultrasound were not recorded, and no further comment can therefore be made on this group. It would be useful to re-examine this group to determine the reason that these studies were not done. It might be that several of these patients were deemed too unstable and were taken to the operating theatre. Alternatively, some patients might have had recent ultrasounds done prior to presentation at the request of their general practitioner or gynaecologist that eliminated the need for another scan.
Subgroup analysis of those with no IUP yielded only 50 patients, thus the numbers of patients with definitive ectopic, adnexal mass, free fluid only or no IUP/no free fluid were small. The use of these categories is practical, as assigning the patient with no IUP to one of these groups suggests the safety of discharge or need for admission. Patients with findings of definite ectopic require admission for operative intervention or medical management. Those with an adnexal mass or free fluid only may have unruptured or leaking ectopic pregnancies. These patients are referred to the gynaecologist on duty at our institution. Those with no IUP or free fluid are usually sent home once they are stable with minimal or no pain. They are reviewed within 24-48 hours by the gynaecology service with the results of serum ßhCG testing, with advice to return should their symptoms worsen. Serum ßhCG testing is not available at our institution on an emergency basis and the results of testing done in the ED are not available to the emergency physician to guide clinical decision-making.
Undiagnosed ectopic pregnancy is a leading cause of emergency medicine malpractice claims. Unfortunately, clinical findings alone cannot reliably diagnose or exclude ectopic pregnancy (14). Our study revealed a final clinical diagnosis of ectopic pregnancy (ruptured or unruptured) in 20 (13%) of the 150 patients studied. Ultrasound confirmed the presence of a definite ectopic pregnancy in only one patient, and showed an IUP in 56.9%. The finding of an IUP has been shown to have a high negative predictive value for the exclusion of ectopic pregnancies in patients who are not taking fertility drugs (4, 11). Abortions accounted for the discharge diagnosis in 91 patients. With the exception of inevitable (n = 5) and missed (n = 1) abortions, most of these patients are not admitted at our institution but return in 24-48 hours for dilatation and curettage by the gynaecology service.
There were some clear limitations of this study. Despite our best efforts, there were a lot of missing data, particularly as it related to time for consultation with the ED physician and time that the ultrasound was performed. This speaks to a significant failure to document these times and the difficulty in collecting data retrospectively. This is important as it may have medico-legal implications. Measures must be taken to improve this aspect of documentation. The fact that different radiologists performed the scans might have resulted in inter-observer variability. Direction for future studies includes the following:
Establishment of a registry for pregnant patients in the first trimester to allow closer examination of the factors that impact on waiting times for this group of patients, and to further describe the outcome in specific subgroups, for example in patients with no IUP or free fluid who are discharged home.
Establishment and evaluation of the effectiveness of a formal credentialling programme for local ED physicians to include evaluation of first trimester patients. The American College of Emergency Physicians (ACEP) and the Society for Academic Emergency Medicine (SAEM) have both published guidelines that can be adopted and implanted to make this a reality (4).
Evaluation of the usefulness of initial serum ßhCG and application of the discriminatory zone in refining the management of the group of patients to include a cost benefit analysis.
All patients with first trimester vaginal bleeding or abdominal pain are considered possible ectopic pregnancies until proven otherwise. The diagnosis of a definite ectopic pregnancy is rare based on sonographic findings. In many instances, the diagnosis of ectopic pregnancy is based on sonographic evidence that is highly suggestive. Given the potential for haemodynamic instability in patients with ectopic pregnancies and the emergent nature of the diagnosis, any reductions in the waiting time for investigations and definitive treatment, subsequent diagnosis and disposal are desirable.
Ultrasound performed by emergency physicians can select the safe discharge of patients with vaginal bleeding and/or abdominal pain. Several studies document the ability of emergency physicians to reliably and safely perform limited sonographic evaluations of the pelvis in first trimester patients with vaginal bleeding (2, 4). The reduction in waiting time, reduced time to definitive care and increased availability of ED beds are significant benefits to be had from such an approach.
We therefore conclude that the majority of patients seen at UHWI with vaginal bleeding in the first trimester are not likely to have an ectopic pregnancy. Emergency department ultrasound would select safe discharge of many of these patients in a timely manner. Ultrasound can readily be incorporated in emergency medicine postgraduate and medical student education once the relevant equipment and a dedicated group of trained senior physicians are in place.
REFERENCES
- 1.American College of Emergency Physicians Clinical Polices Subcommittee on Early Pregnancy Clinical policy: critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med. 2003;41:123–133. doi: 10.1067/mem.2003.13. [DOI] [PubMed] [Google Scholar]
- 2.Stovall TG, Kellerman AL, Ling FW, Buster JE. Emergency department diagnosis of ectopic pregnancy. Ann Emerg Med. 1990;19:1098–1103. doi: 10.1016/s0196-0644(05)81511-2. [DOI] [PubMed] [Google Scholar]
- 3.Lazarus E. What's new in first trimester ultrasound. Radiol Clin North Am. 2003;41:663–679. doi: 10.1016/s0033-8389(03)00039-3. [DOI] [PubMed] [Google Scholar]
- 4.Stein JC, Wang R, Adler N, Boscardin J, Jacoby VL, Won G, et al. Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann Emerg Med. 2010;56:674–683. doi: 10.1016/j.annemergmed.2010.06.563. [DOI] [PubMed] [Google Scholar]
- 5.Falco P, Milano V, Pilu G, David C, Gisolia G, Rizzo N, et al. Sonography of pregnancies with first trimester vaginal bleeding and a viable embryo: a study of prognostic indicators by logistic regression analysis. Ultrasound Obstet Gynecol. 1996;7:165–169. doi: 10.1046/j.1469-0705.1996.07030165.x. [DOI] [PubMed] [Google Scholar]
- 6.Walker GJ, Ashley DE, McCaw AM, Bernard GW. Maternal mortality in Jamaica. Lancet. 1986;1:486–488. doi: 10.1016/s0140-6736(86)92939-9. [DOI] [PubMed] [Google Scholar]
- 7.Dallas J, West W, Mullings A. Evaluation of trans-abdominal ultra-sonography for ectopic pregnancy. West Indian Med J. 1994;43:20–22. [PubMed] [Google Scholar]
- 8.American College of Emergency Physicians . Policy Statement: emergency ultrasound guidelines. Dallas, TX: American College of Emergency Physicians; 2008. [cited 2012 Jun 23]. Available from http://www.acep.org/clinical-practice-management/emergency-ultrasound-guidelines-2008. [Google Scholar]
- 9.McRae A, Murray H, Edmonds M. Diagnostic accuracy and clinical utility of emergency department targeted ultrasonography in the evaluation of first-trimester pelvic pain and bleeding: a systematic review. CJEM. 2009;11:355–364. doi: 10.1017/s1481803500011416. [DOI] [PubMed] [Google Scholar]
- 10.MacVane CZ, Irish CB, Strout TD, Owens WB. Implementation of transvaginal ultrasound in an emergency department residency program: an analysis of resident interpretation. J Emerg Med. 2012;43:124–128. doi: 10.1016/j.jemermed.2011.05.099. [DOI] [PubMed] [Google Scholar]
- 11.Shih CHY. Effect of emergency physician-performed pelvic sonography on length of stay in the emergency department. Ann Emerg Med. 1997;29:348–352. doi: 10.1016/s0196-0644(97)70346-9. [DOI] [PubMed] [Google Scholar]
- 12.Moore CL, Molina AA, Lin H. Ultrasonography in community emergency departments in the United States: access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006;47:147–153. doi: 10.1016/j.annemergmed.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 13.Fox JC, Cusick S, Scruggs W, Henson TW, Anderson CL, Barajas G, et al. Educational assessment of medical student rotation in emergency ultrasound. West J Emerg Med. 2007;8:84–87. [PMC free article] [PubMed] [Google Scholar]
- 14.Kaplan BL, Dart RG, Moskos M, Kuligowska E, Chun B, Adel Hamid M, et al. Ectopic pregnancy: prospective study with improved diagnostic accuracy. Ann Emerg Med. 1996;28:10–17. doi: 10.1016/s0196-0644(96)70131-2. [DOI] [PubMed] [Google Scholar]