Abstract
Objectives:
The aim of this survey was to establish the pain management approaches to acute painful crisis (APC) in sickle cell patients at two healthcare facilities and to compare with available guidelines.
Methods:
A multi-centre observational survey of the management of APC in sickle cell patients was conducted. Data were collected at the Sickle Cell Unit (SCU), Tropical Medicine Research Institute (TMRI) and Accident and Emergency Department (A&E), University Hospital of the West Indies.
Results:
One hundred episodes of uncomplicated APC involving 81 patients managed at the SCU clinic and 64 episodes at the A&E in a total of 28 patients were included in the data set. Drugs used at the SCU included oral morphine, codeine and paracetamol and intramuscular diclofenac. At the A&E, parenteral morphine and pethidine were most commonly used. At the SCU, the mean time to initiation of analgesics was 38 minutes (IQR 25 to 50 minutes); at the A&E, this was 111 minutes (IQR 50 to 150 minutes). At the SCU, the mean duration of stay (DOS) was 2.9 hours (IQR 1.9 to 3.8 hours) with 94% of the patients being discharged home. At the A&E, the mean DOS was 13.0 hours (IQR 8.3 to 16.9 hours) with 93% of the patients being discharged home. The A&E patient group contained multiple high frequency presenters. Documentation of pain severity scores was inconsistent.
Conclusion
The findings of the survey indicate that the management of APC at the two centres is substantially different. Further study is required to investigate patient satisfaction, centre preference and analgesic therapy efficacy.
Keywords: Acute painful crisis, sickle cell disease
Abstract
Objetivos:
El objetivo de este estudio fue establecer los enfoques para el tratamiento del dolor en las crisis de dolor agudas (CDA) en pacientes con anemia falciforme en dos centros de salud, y compararlos con las pautas disponibles.
Métodos:
Se realizó un estudio observacional multicéntrico del tratamiento de CDA en pacientes con anemia falciforme. Se recopilaron datos de la Unidad de Células Falciformes (UCF), el Instituto de Investigación de Medicina Tropical (IIMT), el Departamento de Accidentes y Emergencias (A&E), y el Hospital Universitario de West Indies.
Resultados:
Cien episodios de CDA sin complicaciones en 81 pacientes tratados en la Clínica de la UCF, y 64 episodios en el A&E en un total de 28 pacientes, fueron incluidos en el conjunto de datos. Los fármacos utilizados en la UCF incluyeron morfina oral, codeína y paracetamol, y diclofenaco intramuscular. En el A&E, petidina y morfina parenteral fueron los fármacos más comúnmente utilizados. En la UCF, el tiempo promedio de iniciación de los analgésicos fue 38 minutos (RIC 25 a 50 minutos); en el A&E, fue 111 minutos (RIC 50 a 150 minutos). En la UCF, la duración promedio de estancia (DDE) fue 2.9 horas (RIC 1.9 a 3.8 horas) con un 94% de los pacientes dados de alta. En el A&E, la DDE promedio fue 13.0 horas (RIC 8.3 a 16.9 horas) con el 93% de los pacientes dados de alta. El grupo de pacientes de A&E contenía varios presentadores de alta frecuencia. La documentación de las puntuaciones de severidad del dolor fue inconsistente.
Conclusión:
Los resultados de la encuesta indican que el tratamiento de la CDA en los dos centros es sustancialmente diferente. Se necesitan estudios adicionales para investigar la satisfacción del paciente, la preferencia del centro, y la eficacia de la terapia analgésica.
INTRODUCTION
Jamaica has a population of approximately 2.7 million, with a birth rate of 17.6 per 1000 (1). Sickle cell disease (SCD) in Jamaica occurs in 1:150 births [approximately 300 new cases per year] (2). Sickle cell disease is a congenital haemoglobinopathy in which there is a mutation of the b-globulin gene on chromosome 11 resulting in the production of haemoglobin S instead of A. The haemoglobin S molecule crystallizes when exposed to low oxygen tension resulting in a “sickling” of the erythrocyte. The clinical presentation is that of haemolytic anaemia and vascular occlusion associated with ischaemia, infarction and pain (3). There is an inflammatory component to the disease that is the result of damage to the endothelium from reperfusion injury, adherence of erythrocytes to the endothelium and activation of the stress response (4–6).
Acute painful crisis (APC), also known as vasoocclusive crisis (VOC) is a common complication of SCD. It varies in severity from debilitating to tolerable, and in frequency from constant to hardly ever. Variation in presentation is due to both intrinsic (genotype/phenotype) and extrinsic (infection, exposure to cold, stress) factors (3). Management is complex, may be difficult and must be tailored to the individual's needs.
A number of guidelines have been published which vary in their specific recommendations to manage APC and there is presently no consensus on one single best management protocol (7–9). Ware et al in 1999 published a prospective study investigating outcomes of SCD patients with APC enrolled as day care patients at the Sickle Cell Unit (SCU) clinic of the Tropical Medicine Research Institute (TMRI), a dedicated centre for SCD management and research. They concluded that persons with uncomplicated APC could be safely managed as outpatients. In Jamaica, outpatient care is available at the SCU and in casualty departments of hospitals around the island.
Located on the same campus of The University of the West Indies (UWI), within walking distance, are the SCU and the Accident and Emergency Department (A&E), University Hospital of the West Indies (UHWI). The UHWI is a 540-bed hospital with an annual A&E census of 54 000 visits. Persons with SCD present to the A&E on their own or are referred from healthcare facilities island-wide, including the SCU.
The aim of this survey was to establish what pain management approaches were being used to treat sickle cell patients presenting with APC at these two centres and to compare the management methods with available guidelines.
SUBJECTS AND METHODS
This was a multi-centre observational survey, conducted at two healthcare facilities that manage sickle cell patients who present in painful crisis: the SCU, TMRI and A&E, UHWI. Approval was obtained from the University Hospital of the West Indies/University of the West Indies/Faculty of Medical Sciences Ethics Committee.
Data were collected during the period of April 1 to May 31, 2010. The persons included in the study were SCD patients aged 18 years and older presenting with uncomplicated APC whose pain was severe enough to require admission to an observation ward for extended analgesia care and monitoring. Each presentation was counted separately once the patient was discharged from the facility; this meant that one person could have had multiple presentations during the study period. Patients were excluded if they presented with APC complicated by infection or sequestration.
Data were collected from treatment charts and patient notes for all eligible patients. Data abstracted from the patient notes included demographics (age, gender, phenotype), date of presentation, date and times of triage and of discharge, pain scores (tool used and rating), times, dose and route of medication given, medication taken before presentation and the prescription given at discharge, contraindications to medications and any complications to treatment. The duration of the APC and the number of presentations with APC during the study period were also noted. Time of triage was taken as the initial contact time for calculating times to analgesic treatment and time to discharge.
Data were stored and collated in Epidata and analysed with Stata v 10.0 statistical programme. Descriptive statistics were used to summarize variables such as patient demographics, duration of stay and drug usage. To allow for comparison, all opioid doses were converted to oral morphine equivalents using the conversion calculator at the GlobalRPh website (10).
RESULTS
One hundred episodes of uncomplicated APC involving 81 patients at the SCU clinic and 64 episodes at the A&E involving 28 patients were included in the data set. Five episodes were excluded from some of the analysis because of incomplete available data, four from the SCU clinic group and one from the A&E group. Data collected showed no overlap between the patient groups seen at each centre.
Patient demographic profile
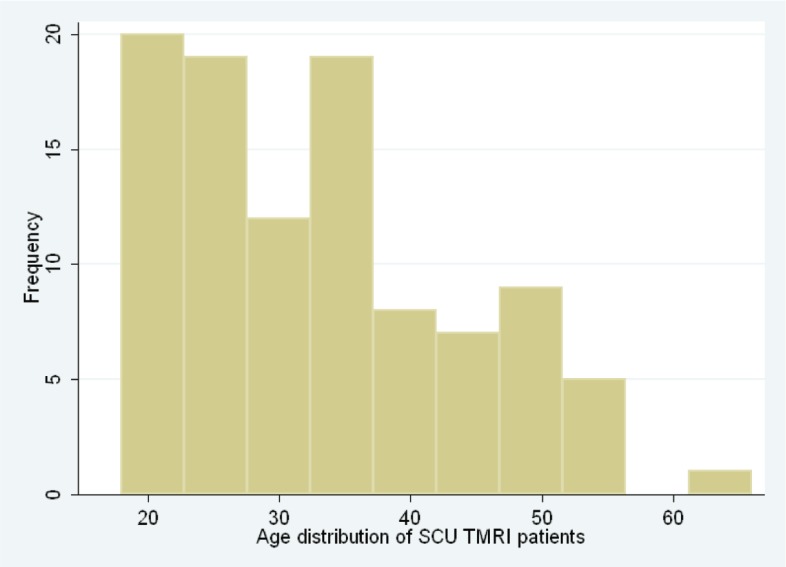
Female patients presented to the SCU most frequently (55%). Mean age was 33 years and ranged from 18 to 66 years (IQR 24–39). Age distribution by centre is shown in Figs. 1 and 2.
Fig. 1. Age distribution of patients presenting to the Sickle Cell Unit (SCU), at the Tropical Medicine Research Institute (TMRI).
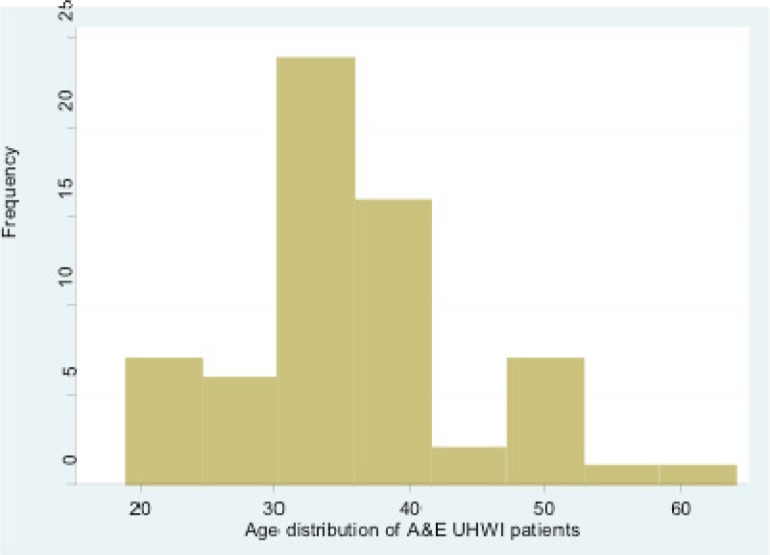
Fig. 2. Age distribution of patients presenting to the Accident and Emergency Department (A&E), University Hospital of the West Indies (UHWI).
Patients with HbSS disease represented 71% of presentations and 17% of patients presenting to the SCU had multiple (at least two) visits.
In 67% of cases, the patient presenting to the A&E was male and in 84% of cases the patient had HbSS disease (Table 1). These numbers are skewed because nine (14%) patients at A&E presented at least three times and one (male with HbSS) presented 13 times (20%) during the study period. Mean age was 35 years and range was 19 to 64 years (IQR 24–39).
Table 1. Patient demographics according to centre where they presented.
| Patient demographics | Centre where patient presented | ||
|---|---|---|---|
| A&E UHWI | SCU clinic | Total | |
| Gender | |||
| Male | 43 | 45 | 88 |
| Female | 21 | 55 | 76 |
| Phenotype | |||
| SS | 54 | 71 | 125 |
| SC | 1 | 13 | 14 |
| Sb+ | 4 | 7 | 11 |
| Sb0 | 4 | 7 | 11 |
| Other | 1 | 2 | 3 |
| Pain assessment at presentation | |||
| Yes | 25 | 67 | 92 |
| No | 39 | 33 | 72 |
A&E UHWI =Accident and Emergency Department, University Hospital of the West Indies, SCU = Sickle Cell Unit
Analgesic medication used prior to presentation
Thirty-three per cent of the presentations to the A&E and 41% at the SCU clinic reported using analgesic medication prior to presentation. The most commonly used medications were paracetamol (42%), diclofenac (32%) and codeine combination drugs such as codeine plus paracetamol (Panadeine) or diclofenac [Voltaren Forte] (14%). Only ten patients (6%) reported using stronger opioids: morphine (two) and pethidine (eight) prior to presentation.
Pain assessment
Pain scores were documented in only 67% of presentations at the SCU and 39% at the A&E (Table 1). The numerical rating score was used to assess pain in the majority of patients. Most presentations at the A&E were with scores of nine to ten (72%), while at SCU, most scores were less severe, between six and eight (72%) [Table 2].
Table 2. Pain assessment scores (NRS) at admission.
| NRS | Centre where patient presented | Total (%) | |
|---|---|---|---|
| A&E UHWI n (%) | SCU clinic n (%) | ||
| 10 | 14 (56) | 4 (7) | 18 (22) |
| 9 | 4 (16) | 7 (12) | 11 (13) |
| 8 | 3 (12) | 13 (23) | 16 (20) |
| 7 | 4 (16) | 20 (35) | 24 (29) |
| 6 | 0 (0) | 8 (14) | 8 (10) |
| 5 | 0 (0) | 5 (9) | 5 (6) |
| Total | 25 (100) | 57 (100) | 82 (100) |
NRS = numeric rating scale, A&E UHWI = Accident and Emergency Department, University Hospital of the West Indies, SCU = Sickle Cell Unit
Time to initiation of analgesic therapy
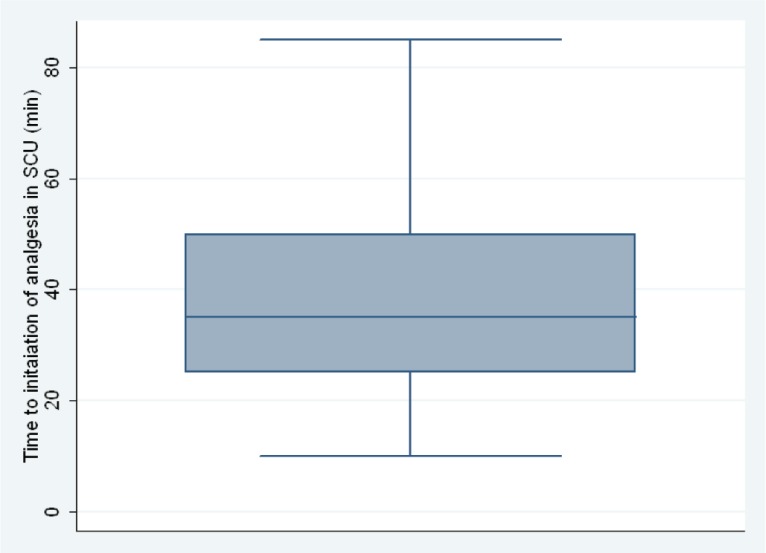
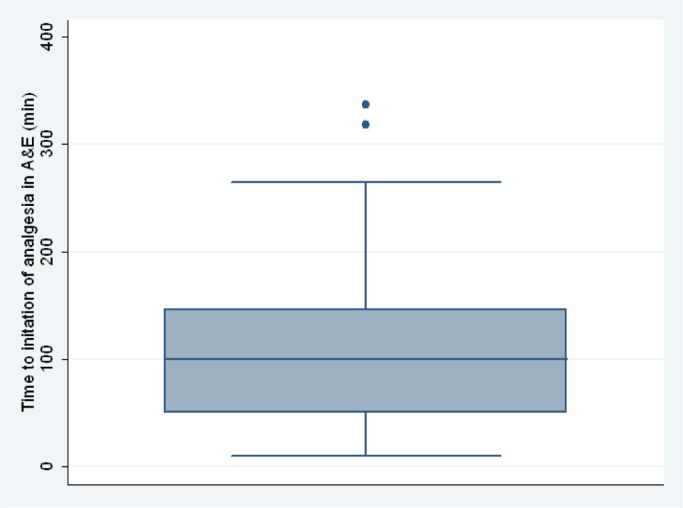
At the SCU, the mean time to initiation of analgesic therapy was 38 minutes (IQR 25 to 50); at the A&E, this was 111 minutes [IQR 50 to 150 minutes] (Figs. 3 and 4).
Fig. 3. Time to initiation of analgesic therapy for patients at the Sickle Cell Unit (SCU) at the Tropical Medicine Research Institute.
Fig. 4. Time to initiation of analgesic therapy for patients at the Accident and Emergency Department (A&E), University Hospital of the West Indies.
Medication dose, routes and timing used
The majority of patients presenting to the SCU received a combination of oral morphine (20 mg), oral codeine (60 mg), intramuscular diclofenac sodium (75 mg) and oral paracetamol (1 g). All patients at the A&E were eventually prescribed parenteral opioids, either morphine (10 mg), or pethidine (100 mg) [intramuscular (IM) or intravenous (IV)] as part of their management. Intramuscular diclofenac sodium (75 mg) and oral paracetamol (1 g) were also used (Table 3).
Table 3. Frequency of analgesic drug prescribed and route of administration.
| Analgesic (route) | Centre where patient presented | Total (%) | |
|---|---|---|---|
| A&E UHWI n (%) | SCU clinic n (%) | ||
| Morphine | 13 (20)** | 68 (68)* | 81 (49) |
| Pethidine (parenteral) | 56 (87) | 0 (0)¥ | 56 (13) |
| Codeine (PO) | 0 (0) | 48 (48) | 48 (29) |
| Diclofenac Na (IM) | 41 (64) | 87 (87) | 128 (78) |
| Paracetamol (PO) | 60 (93) | 50 (50) | 110 (67) |
parenteral,
oral,
not available
A&E UHWI = Accident and Emergency Department, University Hospital of the West Indies, SCU = Sickle Cell Unit, PO = parenteral opioid, IM = intramuscular
At the SCU, 64% were prescribed oral morphine as part of the initial analgesic therapy and the mean dose of morphine given orally in the first four hours was 22 mg. The mean time between medication doses was 84 minutes. In 84% of presentation at the A&E, patients received parenteral opioids (pethidine 71% or morphine 12%) as an initial medication. The mean (equivalent oral morphine) dose of opioid given within the first four hours of treatment at the A&E was 41 mg. The mean time between medication doses was 227 minutes.
Side effects
One patient each at the SCU (given dimenhydrinate) and the A&E (given metoclopramide) had nausea and vomiting and one patient at A&E had pruritus requiring intervention (diphenhydramine).
Duration of stay, discharge and discharge medications
At the SCU, mean duration of stay (DOS) was 2.9 hours (IQR 1.9 to 3.8 hours) and 94% of presentations ended with the patient being discharged home. All other patients were referred to the A&E. Only two of these six patients referred were registered and seen at UHWI. Both were admitted but lost to follow-up due to an inability to locate their dockets. At the SCU, 34% were discharged on strong opioid analgesics (pethidine and morphine).
At the A&E, the mean DOS was 13.0 hours (IQR 8.3 to 16.9 hours) and 93% of presentations ended with the patients being discharged home. Sixty per cent of patients were discharged home with prescriptions for strong opioid analgesics (pethidine and morphine).
Patients from both centres were discharged home on a variety of other medications. These included: diclofenac sodium or potassium, codeine, codeine combinations, or paracetamol.
DISCUSSION
The SCU and the A&E represent two different management environments; SCU, the speciality day hospital model and A&E, the non-specialty general emergency model. The specialty model has been shown to reduce admission rates and the associated costs and does not increase morbidity and mortality (11–13). In addition, the available resources (personnel and drugs) differ and this impacts on the therapeutic approach. The literature does not strongly support any singular approach to the analgesic management of APC. The guidelines' recommendations all suggest an acceptance of the use of paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs) and opioids but in varying regimes.
The SCU does not have access to parenteral opioids, only oral morphine and codeine are available. This is due to a lack of facilities for handling parenteral opioids under “The Dangerous Drugs Act” (DDA). The UHWI A&E has both parenteral and oral opioids, including morphine and pethidine. Codeine is not routinely available. Decisions on medications prescribed appear to be determined primarily by what was available and the existence of contraindications such as allergies, peptic ulcer disease and renal impairment.
A lack of consistent documentation of pain scores made it impossible to draw any definite conclusions on the efficacy of the therapy and the patient's state of mind at discharge, these can only be inferred by patient behaviour. It can be argued that patients accept discharge when there has been some reduction in pain and they are comfortable managing their pain (whatever the severity) at home. However, other factors such as wanting to avoid referral to a hospital for admission cannot be excluded.
The published guidelines on management of APC recommended regular assessment of pain severity to quantify the efficacy of therapy, and allow for individualization of the regimen (Table 4). Pain assessment was documented in only 67% of patients at the SCU and 39% at the A&E. The verbal numeric rating scale (NRS) was the most commonly used pain assessment tool in both centres (Table 4). The popularity of the verbal NRS may stem from its ease of use due to a single language in the population, simplicity and no requirement for special charts (which have a cost).
Table 4. Table comparing acute painful crisis management guidelines with management at study centres.
| Source | Pain assessment method | Time to initiation of analgesic (minutes) | Reassessment interval (minutes) |
|---|---|---|---|
| Bortolusso Ali et al(2008) | NRS | No time given | 30 |
| National Institutes of Health (2002) | NRS or VAS | 15–20 | 15–30 |
| Rees et al(2003) | Patient appropriate | ≤30 | ≤30 |
| SCU TMRI data | VNRS and VRS | Mean 38 | Mean 84 |
| A&E UHWI data | VNRS | Mean 111 | Mean 227 |
A&E UHWI = Accident and Emergency Department, University Hospital of the West Indies, SCU TMRI =Sickle Cell Unit, Tropical Medicine Research Institute, NRS = numeric rating scale, VAS = visual analogue scale, VNRS = verbal numeric rating scale
The guidelines suggest that therapy should begin between 15 and 30 minutes after triage (Table 4). Three studies in the United States of America (USA): Benjamin et al (2000), Tanabe et al (2007) and Tanabe et al (2010) reported achieving initiation within 20 minutes, 90 minutes and 74 minutes, respectively (11, 14, 15). The results of this survey showed mean times to initiation of analgesic therapy of 38 minutes and 111 minutes at SCU and A&E, respectively. Possible reasons for delays in the initiation of therapy proffered by Tanabe et al (14, 15) include over-crowding and “under-triage” or the assigning of a lower priority level. Interestingly, negative attitudes toward “frequent attenders” were not cited as a cause for delay by Tanabe et al (14, 15). It could be argued, however, that “under-triage” was the manifestation of the negative perception of SCD patients that abound in the literature (16–19) and can affect perceptions and assessment of priority.
Locally, the delays may be explained by high patient to doctor ratios or delays due to the logistics of accessing opioid drugs from the DDA locker in either centre. There is a need to investigate reasons for the delays and the attitudes of the local healthcare workers to SCD patients in view of anecdotal reports of negative behaviour.
Based on a lack of overlap observed between the patient populations attending both centres, it appears that there are two disparate groups of SCD patients who chose to seek analgesic therapy preferentially in one centre. Location is unlikely to be a cause because of the close proximity of the centres. Preference could be related to the protocol of drugs used, the attitude of the staff, or the accessibility (opening hours) or comfort of the facilities.
Another explanation may lie with a phenotypical variation between patients attending the A&E and those attending SCU (20). This hypothesis is supported by data that show higher pain scores on presentation, longer durations of stay in the department, a larger number of high frequency presenters and preference for parenteral opioids in the A&E population (relative to the SCU patients).
The methodology employed entailed abstraction of data from patient notes, which has the disadvantage of only allowing for the observation of available documented data, creating observer bias.
CONCLUSION
The findings of the survey indicate that the management of APC at the two centres fundamentally differ in their structure. The methodologies applied to SCD patients presenting with APC vary in the specifics of the drug routes and dosages. Regimes at both centres though, are generally consistent with the available evidence in their use of a combination of opioids, NSAIDs and paracetamol/ acetominophen delivered either enterally or parenterally. These observed variations may be due to differences in the availability of drugs.
Initiating analgesic therapy within times recommended by the guidelines has not been widely achieved. The infrequent and inconsistent documentation of pain severity scores suggests informality in patient reassessment that may be detrimental to quality of care and has made assessment of the efficacy of analgesic regimens impossible.
Differences in the characteristics of the centres and/or phenotypical variation in the population may explain the apparent existence of two separate populations differentiated by their preference for one facility over the other for the treatment of APC. Research into the possibility of phenotypical variation affecting patient choices for pain management is also of interest as it may help to explain drug preferences.
REFERENCES
- 1.Pan American Health Organization. II. Jamaica. Washington, DC: PAHO; 2007. Health in the Americas, 2007. Countries. Available from: www.paho.org/HIA/archivosvol2/paisesing/Jamaica%20English.pdf. [Google Scholar]
- 2.King L, Fraser R, Forbes M, Grindley M, Ali S, Reid M. Newborn sickle cell disease screening: the Jamaican experience (1995-2006) J Med Screen. 2007;14:117–122. doi: 10.1258/096914107782066185. [DOI] [PubMed] [Google Scholar]
- 3.Serjeant GR, Serjeant BE. Sickle cell disease. 3rd ed. Oxford University Press; 2001. [Google Scholar]
- 4.Ballas SK. Current issues in sickle cell pain and its management. Hematology. 2007;2007:97–105. doi: 10.1182/asheducation-2007.1.97. [DOI] [PubMed] [Google Scholar]
- 5.Hebbel RP, Osarogiagbon R, Kaul D. The endothelial biology of sickle cell disease: inflammation and a chronic vasculopathy. Microcirculation. 2004;11:129–151. [PubMed] [Google Scholar]
- 6.Hebbel RP, Vercellotti GM. The endothelial biology of sickle cell disease. J Lab Clin Med. 1997;129:288–293. doi: 10.1016/s0022-2143(97)90176-1. [DOI] [PubMed] [Google Scholar]
- 7.Bortolusso-Ali S, editor. Sickle cell disease: the clinical guidelines of the Sickle Cell Unit, TMRI, UWI. 1st ed. Kingston, Jamaica: The University of the West Indies; 2008. [Google Scholar]
- 8.National Institutes of Health The management of sickle cell disease. 2002. NIH publication no 02-2117. Available from: http://www.nhlbi.nih.gov/health/prof/blood/sickle/index.htm#filefor.
- 9.Rees DC, Olujohungbe AD, Parker NE, Stephens AD, Telfer P, Wright J. Guidelines for the management of the acute painful crisis in sickle cell disease. Br J Haematol. 2003;120:744–752. doi: 10.1046/j.1365-2141.2003.04193.x. [DOI] [PubMed] [Google Scholar]
- 10.Opioid analgesic converter. [cited 2010 May 1]. GlobalRPh.com. Available from http://www.globalrph.com/narcoticonv.htm.
- 11.Benjamin LJ, Swinson GI, Nagel RL. Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crises. Blood. 2000;95:1130–1136. [PubMed] [Google Scholar]
- 12.Ware MA, Hambleton I, Ochaya I, Serjeant GR. Day-care management of sickle cell painful crisis in Jamaica: a model applicable elsewhere? Br J Haematol. 1999;104:93–96. doi: 10.1046/j.1365-2141.1999.01160.x. [DOI] [PubMed] [Google Scholar]
- 13.Wright J, Bareford D, Wright C, Augustine G, Olley K, Musamadi L, et al. Day case management of sickle pain: 3 years experience in a UK sickle cell unit. Br J Haematol. 2004;126:878–880. doi: 10.1111/j.1365-2141.2004.05123.x. [DOI] [PubMed] [Google Scholar]
- 14.Tanabe P, Artz N, Mark, Courtney D, Martinovich Z, Weiss KB, Zvirbulis E, et al. Adult emergency department patients with sickle cell pain crisis: a learning collaborative model to improve analgesic management. Acad Emerg Med. 2010;17:399–407. doi: 10.1111/j.1553-2712.2010.00693.x. [DOI] [PubMed] [Google Scholar]
- 15.Tanabe P, Myers R, Zosel A, Brice J, Ansari AH, Evans J, et al. Emergency department management of acute pain episodes in sickle cell disease. Acad Emerg Med. 2007;14:419–425. doi: 10.1197/j.aem.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 16.Lazio MP, Costello HH, Courtney DM, Martinovich Z, Myers R, Zosel A, et al. A comparison of analgesic management for emergency department patients with sickle cell disease and renal colic. Clin J Pain. 2010;26:199–205. doi: 10.1097/AJP.0b013e3181bed10c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shapiro BS, Benjamin LJ, Payne R, Heidrich G. Sickle cell-related pain: perceptions of medical practitioners. J Pain Symptom Manage. 1997;14:168–174. doi: 10.1016/S0885-3924(97)00019-5. [DOI] [PubMed] [Google Scholar]
- 18.Todd KH, Green C, Bonham VL Jr, Haywood C Jr, Ivy E. Sickle cell disease related pain: crisis and conflict. J Pain. 2006;7:453–458. doi: 10.1016/j.jpain.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 19.Zempsky WT. Treatment of sickle cell pain: fostering trust and justice. JAMA. 2009;302:2479–2480. doi: 10.1001/jama.2009.1811. [DOI] [PubMed] [Google Scholar]
- 20.Alexander N, Higgs D, Dover G, Serjeant GR. Are there clinical phenotypes of homozygous sickle cell disease? Br J Haematol. 2004;126:606–611. doi: 10.1111/j.1365-2141.2004.05025.x. [DOI] [PubMed] [Google Scholar]