ABSTRACT
A survey was conducted at a private general hospital, exploring the reasons why children with measles had missed opportunities for vaccination during the local measles epidemics that occurred in Japan between 1999 and 2003. The responses from parents/guardians of confirmed measles patients (n = 120) indicated the following: more than half of the parents/guardians were too busy or forgot to have their children immunized and 32% refrained from immunization due to anti-vaccine views. Healthcare workers should consider that parents/guardians who are willing to immunize their children may miss opportunities to do so because they are busy, and not because of anti-vaccine attitudes. Healthcare workers should keep in mind that it is important to provide honest information on the potential risks and benefits of the vaccine, while informing parents/guardians of the vaccination schedule.
Keywords: Anti-vaccine attitudes, measles, non-vaccination, vaccine
RESUMEN
Se realizó una encuesta en un hospital general privado, explorando las razones de por las cuales los niños con sarampión habían perdido las oportunidades de vacunación durante las epidemias locales de sarampión, ocurridas en Japón entre 1999 y 2003. Las respuestas de los padres y tutores de los pacientes confirmados con sarampión (n = 120) indicaron lo siguiente: más de la mitad de los padres y tutores estaban demasiado ocupados u olvidaron hacer inmunizar a sus hijos, en tanto que el 32% se abstuvo de permitir la inmunización debido a sus puntos de vistas contrarios a las vacunas. Los trabajadores de la salud deben tener en cuenta que los padres y tutores que están dispuestos a vacunar a sus hijos, pueden perder la oportunidad de hacerlo porque están ocupados y no por actitudes contra las vacunas. Los trabajadores de la salud no deben olvidar que es importante proporcionar información honesta sobre los potenciales riesgos y beneficios de la vacuna, cuando se informa el programa de vacunación a los padres y tutores.
INTRODUCTION
In 2005, the World Health Organization (WHO) Regional Office for the Western Pacific (WPRO) established a target date of 2012 for regional measles elimination, following its declaration in 2003 of its goal of measles elimination (1). Due to one of the four criteria that were ratified by members of the WPRO, the WHO confirmed that measles incidence in Japan was 1.8 per 100 000 population and beyond the WPRO standard of < 1.0 per 100 000.
Before 2006, Japan's progress with regard to its measles vaccine policy was rather slow, and vaccine coverage has remained < 80% nationwide since the introduction of the measles containing vaccine (MCV). Following the 1966 introduction and adoption of measles vaccination in the national regular immunization programme of Japan [the Preventive Vaccination Act] (2), the attenuated live vaccine was given once to the children aged 12–90 months. This policy remained in effect until April 2006, when the two-dose measles vaccine was legally approved (3). Between 1999 and 2003, Japan experienced a series of measles epidemics. The number of patients at that time was estimated to be approximately 100 000–200 000 (3). During the same period, we identified more than 190 measles patients in one private general hospital (Chiba-Nishi General Hospital) in Matsudo-city, Chiba prefecture, Japan (3). The majority of the patients were non-immunized children (n = 132, 68.0%), even though vaccines were available (free of charge) during the day on weekdays at hospitals and general practitioners' clinics. In order to determine effective local strategy recommendations, parents/guardians were asked the reasons why their children had not been vaccinated. The results and lessons from the experience of these epidemics are significant and continue to be especially useful for establishing immunization strategies. Here, we examine the reasons for non-vaccination and draw lessons from our findings.
This study was approved by the ethics committee of Chiba-Nishi General Hospital.
SUBJECTS AND RESULTS
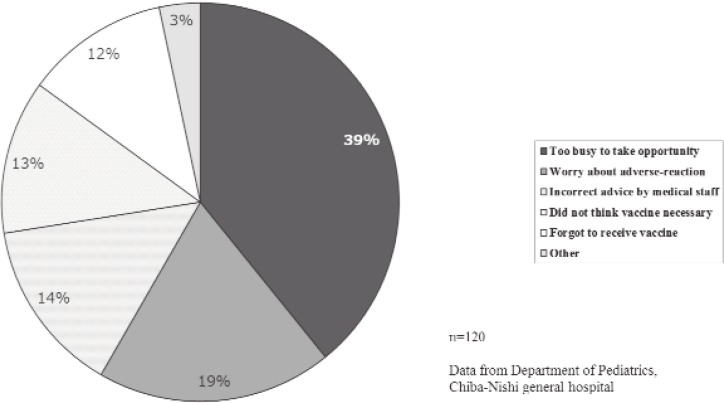
Parents/guardians of confirmed measles patients (n = 120) were asked by the authors, who worked in the paediatrics department of the hospital, to anonymously indicate the reasons why their children had not been vaccinated. The Figure shows all stated reasons for non-vaccination. It is noteworthy that the majority of patients stated reasons that did not reflect anti-vaccine attitudes. The most common reason stated was that they were too busy to take up the opportunity to have their children vaccinated (39%), and a further 12% stated that they had hoped to vaccinate their children but forgot. Reasons that reflected anti-vaccine attitudes such as worry about adverse reactions (19%), and thinking vaccination to be unnecessary (13%), were in the minority.
Figure. Reasons given by parents/guardians for not receiving the measles vaccine.
The 17 patients (14%) who refrained from vaccination on the advice of healthcare workers did so because of conditions in the child's medical history, including food allergy, bronchial asthma, atopic dermatitis and febrile convulsion.
DISCUSSION
Several lessons can be gleaned from these results. First, parents/guardians who are willing to vaccinate may miss the opportunity because they are busy. This factor seems to be neglected by health professionals, who are prone to focus only on vaccine refusal. For reducing missed vaccine opportunities, it is necessary to detect unvaccinated children using the vaccine registry and to widely and repeatedly inform the general public of the vaccination schedule (4).
Secondly, advice from medical professionals could cause parents/guardians to take incorrect action. In this survey, the vaccine knowledge of medical advisors for parents/guardians was not scrutinized. However, we can surmise that in some cases parents/guardians misunderstood the advice of their medical practitioners, or that the advice that they were given was incorrect, or not sufficient for them to act correctly. Healthcare workers should keep in mind that their advice may sometimes lead to the misconception that vaccination is unnecessary (5).
Finally, it is inevitable that misinformation will circulate among some of the parents/guardians. In spite of our best efforts to circulate correct information, it is difficult to wipe out the sources of misinformation (6). However, healthcare workers, especially doctors, should honestly inform parents/guardians of what is and is not known about the risks and benefits of the vaccine in question, attempt to understand the parent's concerns about immunization, and try to correct any misperceptions and misinformation (7).
In conclusion, our survey results revealed that more than half of the parents/guardians were too busy or forgot to have their children immunized, and that 32% refrained from immunization due to anti-vaccine views. Healthcare workers should keep in mind that parents/guardians who are willing to immunize may miss opportunities to do so because they are busy, not because they hold anti-vaccine attitudes. It is also important that healthcare workers provide parents and guardians with honest information on the potential risks and benefits of vaccines, while widely and repeatedly informing them of the vaccination schedule.
REFERENCES
- 1.WHO WPRO . Summary record of the eighth meeting. Resolution WPR/RC56.R8. Measles elimination, hepatitis B control, and poliomyelitis eradication. Manila, Philippines: WHO; 2005. Fifty-sixth session of the Regional Committee for the Western Pacific. [Google Scholar]
- 2.Nakatani H, Sano T, Iuchi T. Development of vaccination policy in Japan: current issues and policy directions. Jpn J Infect Dis. 2002;55:101–111. [PubMed] [Google Scholar]
- 3.Takahashi K, Ohkusa Y, Kim JY. The economic disease burden of measles in Japan and a benefit cost analysis of vaccination, a retrospective study. BMC Health Serv Res. 2011;11:254–254. doi: 10.1186/1472-6963-11-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute for Infectious Diseases Efforts toward high measles-rubella (MR) vaccine coverage (> 95%) in preschoolers (6–7 years) in fiscal year 2007–Akita. Infect Dis Wkly Rep Jpn. 2008;10:15–16. [Google Scholar]
- 5.Darden PM, Thompson DM, Roberts JR, Hale JJ, Pope C, Naifeh M, et al. Reasons for not vaccinating adolescents: National Immunization Survey of Teens, 2008–2010. Pediatrics. 2013;131:645–651. doi: 10.1542/peds.2012-2384. [DOI] [PubMed] [Google Scholar]
- 6.Takahashi K, Kanda H, Mizushima S. Growing concerns with the flow of misinformation from electronic books. Interact J Med Res. 2013;2: doi: 10.2196/ijmr.2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diekema DS. Responding to parental refusals of immunization of children. Pediatrics. 2005;115:1428–1431. doi: 10.1542/peds.2005-0316. [DOI] [PubMed] [Google Scholar]