Abstract
Objectives:
This study aimed to show the impact of a multidisciplinary quality improvement project on adherence to antimicrobial prophylaxis guidelines in oncological surgery.
Methods:
This pre- and post-intervention prospective observational study was carried out at the King Hussein Cancer Centre (KHCC) in Amman, Jordan, between August 2009 and February 2012. The quality improvement project consisted of revising the institutional guidelines for surgical antimicrobial prophylaxis, assigning a clinical pharmacist to the surgical department, establishing an operating room satellite pharmacy and providing education regarding the appropriate utilisation of antibiotics. The medical records of adult cancer patients who underwent surgery were evaluated one month before and one month after the project was implemented to assess adherence to the guidelines with regards to antibiotics prescribed, drug doses and timing and treatment duration.
Results:
A total of 70 patients were evaluated before and 97 patients were evaluated after the intervention, of which 57 (81.4%) and 95 (97.9%) patients received antibiotics, respectively. In comparing the pre- and post-intervention groups, an improvement was observed in the proportion of patients who received antibiotics at the appropriate time (n = 12 versus n = 79; 21.1% versus 83.2%; P <0.01), for the appropriate duration of time (n = 22 versus n = 94; 38.6% versus 99.0%; P <0.01) and in the appropriate dose (n = 9 versus n = 87; 56.3% versus 98.9%; P <0.01).
Conclusion:
Adherence to the antimicrobial prophylaxis guidelines at KHCC improved significantly after the implementation of a quality improvement project.
Keywords: Antibiotic Prophylaxis, Surgery, Operative Surgical Procedures, Quality Improvement, Pharmacists, Education, Jordan
Advances in Knowledge
- The current study indicated that the implementation of a multidisciplinary quality improvement programme at the King Hussein Cancer Centre in Amman, Jordan, significantly improved compliance with surgical antimicrobial prophylaxis guidelines.
- The programme consisted of revising institutional guidelines for surgical antimicrobial prophylaxis, assigning a clinical pharmacist to the surgical service, establishing an operating room satellite pharmacy and providing educational sessions and tools to aid in the appropriate utilisation of antibiotics.
Application to Patient Care
- Surgical antimicrobial prophylaxis is necessary to reduce the incidence of potential surgical infections. This study demonstrated that adherence to a set of antimicrobial prophylaxis guidelines can be significantly improved with the implementation of a multi-disciplinary project.
Surgical site infections (SSIs) are considered the most common type of nosocomial infections in surgical patients and are associated with high morbidity and mortality as well as increased costs.1–4 Therefore, antimicrobial prophylaxis is recommended in a wide range of surgical procedures for the prevention of SSIs.5 Guidelines are available to provide clinicians with a standardised approach to the rational, safe and effective use of antimicrobial agents.6 However, despite the presence of evidence-based guidelines, poor adherence to guidelines has been reported internationally.7–13
The King Hussein Cancer Centre (KHCC) in Amman, Jordan, is a 170-bed comprehensive teaching cancer centre with a surgical service consisting of nine teams with various specialties. Among these teams, an average of 25 patients are seen and five major elective surgeries are performed per day. A quality improvement initiative was planned at KHCC to improve adherence to surgical prophylaxis guidelines. This study aimed to evaluate the impact of this multidisciplinary quality improvement project on adherence to surgical antimicrobial prophylaxis guidelines.
Methods
This pre- and post-intervention prospective observational study was conducted between August 2009 and February 2012 in the surgical department of KHCC. The pre-intervention phase was carried out in August 2009, one month prior to implementing a quality improvement project, and the post-intervention phase was carried out in February 2012, one month after the full implementation of all elements in the quality improvement project. The intervention itself consisted of four initiatives: revising the institutional guidelines for surgical antimicrobial prophylaxis; assigning a full-time clinical pharmacist to the surgical service; establishing an operating room satellite pharmacy (ORSP); and offering various educational sessions and tools for the medical, nursing and pharmacy staff to aid in the appropriate utilisation of antibiotics.
The quality improvement project was implemented as follows. The surgical antimicrobial prophylaxis guidelines were revised and updated based on the most recent international clinical practice guidelines available at that time.6 In the pre-intervention phase, the institutional guidelines were very limited and did not include recommendations for certain types of oncological surgeries, such as breast cancer or orthopaedic surgeries; as a result, the revised guidelines were made more comprehensive by including recommended antimicrobial therapy for all surgeries commonly performed at KHCC. The revised KHCC guidelines for surgical antimicrobial prophylaxis outlined the recommended antibiotics for each type of surgery along with the appropriate dose and duration. The most recommended antibiotic in the revised guidelines was cefazolin which treats the most common SSIs caused by Gram-negative and -positive pathogens (bacteria of the Staphylococcus and Streptococcus genera and Escherichia coli).5 Metronidazole was also included to treat anaerobic infections common after certain operations (e.g. gastrointestinal surgeries). An assigned clinical pharmacist was available at KHCC during weekdays to review and evaluate all prescribed medications. In addition, a clinical pharmacist was available at all times via mobile phone for any pharmacotherapy-related consultations and was responsible for medication reconciliation and discharge counselling for surgery patients.
Prior to the implementation of the ORSP at KHCC, antibiotics were stored in the operating room and were dispensed and prepared by surgical nurses. This meant that the antibiotic orders were not reviewed by a pharmacist prior to administration to a patient. Due to the potential risk and errors associated with such practice, the pharmacy and surgery departments agreed to create an ORSP adjacent to the operating room as part of the quality improvement project. An ORSP was established and was open from 8 a.m. to 5 p.m. every day. The pharmacy was staffed by a pharmacist and a pharmacy technician, who were responsible for processing all orders and preparing and dispensing the necessary medications. The pharmacist at the ORSP had full access to patient electronic records to ensure that each prescription was in compliance with the guidelines. All orders from the operating room were thus reviewed by a pharmacist and prepared in the ORSP using aseptic techniques. Several educational sessions were also conducted by the clinical pharmacist, the physicians and the head nurse of surgery for the medical, nursing and pharmacy staff. The aim was to increase awareness about the revised institutional guidelines and to promote evidence-based practice. In addition, e-mail reminders were sent to the staff regarding the new guidelines and one-to-one educational sessions were continuously offered to all members of staff.
The study group included all eligible patients admitted to KHCC during the pre- and post-intervention phases. All cancer patients who were assigned to the surgery service and who underwent an elective surgery during their admission were included in the study. Patients admitted and/or discharged on a weekend were excluded since the pharmacist conducting the profile review was not available on those days and therefore a full assessment of the condition would be difficult to conduct. In addition, those who were prescribed antibiotics for the treatment of a suspected or proven infection were excluded. The medical records of the eligible patients were reviewed to assess the type of prophylactic antibiotic prescribed, the dose administered and the timing and duration of the antibiotic administration. The appropriateness of the antibiotic prescribed and the administered dose were evaluated according to either the revised or initial antimicrobial prophylaxis guidelines, depending on the phase of the study. The timing of the antibiotic was considered appropriate if the antibiotic was administered at least 60 minutes prior to surgical incision and the duration of the antibiotic was deemed appropriate if it did not exceed 24 hours following the surgery. These details were recorded for both the pre- and post-intervention patient groups; the data between the two groups was then compared accordingly in order to determine any changes in the compliance to antimicrobial prophylaxis guidelines.
All analyses were performed using the Statistical Analysis System (SAS), Version 9.1 (SAS Institute Inc, Cary, North Carolina, USA). Categorical data were reported as counts and percentages, while continuous data were reported as means with standard deviations. Adherence to the guidelines in the pre- and post-intervention phases was compared using Chi-squared and Fisher’s exact tests. A significance criterion of P <0.05 was used.
This study received ethical approval from the Institutional Review Board at KHCC for both the pre- and post-intervention phases of the study (IRB# 12-KHCC-12).
Results
During the study period, a total of 70 patients were evaluated in the pre-intervention phase and 97 patients were evaluated in the post-intervention phase [Table 1]. In the pre- and post-intervention groups, 57 (81.4%) and 95 (97.9%) patients received antibiotics, respectively. The most common types of surgeries during both phases were breast surgeries (modified radical and skin-sparing mastectomies), gastrointestinal surgeries (hemicolectomies and ileostomy closures) and genitourinary surgeries (transurethral resections of bladder tumours).
Table 1:
Patient characteristics prior to and following a multidisciplinary quality improvement project on adherence to antimicrobial prophylaxis guidelines at the King Hussein Cancer Centre, Amman, Jordan
| Characteristic | n (%) | P value | |
|---|---|---|---|
| Pre-intervention (n = 70) | Post-intervention (n = 97) | ||
| Mean age in years ± SD | 50.0 ±12.6 | 50.0 ± 15.4 | 0.34 |
| Penicillin and/or cephalosporin allergies | 4 (5.7) | 5 (5.1) | 0.91 |
| Type of surgery | 0.81 | ||
| Breast | 22 (31.4) | 31 (32.0) | |
| Gastrointestinal | 18 (25.7) | 21 (21.7) | |
| Genitourinary | 12 (17.1) | 22 (22.7) | |
| Gynaecological | 8 (11.4) | 6 (6.2) | |
| Head and neck | 5 (7.1) | 7 (7.2) | |
| Other | 5 (7.1) | 10 (10.3) | |
SD = standard deviation.
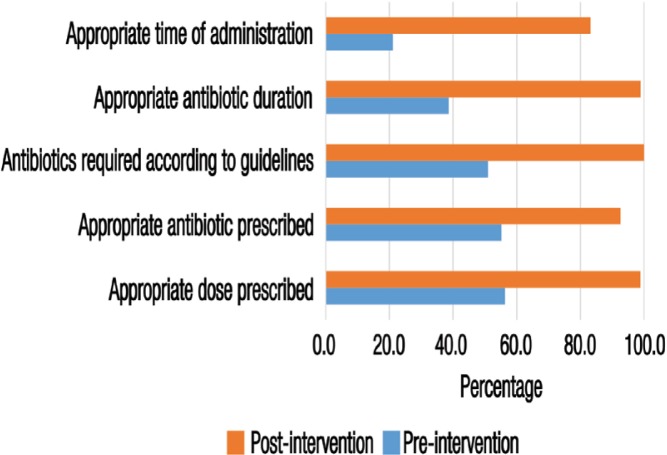
In the post-intervention phase, a significant improvement in adherence to the antimicrobial prophylaxis guidelines was observed. Of the patients in the post-intervention group who received antibiotics, 79 (83.2%) received their antibiotic dose at the appropriate time compared to 12 patients (21.1%) in the pre-intervention group (P <0.01). Furthermore, 94 patients (99.0%) in the post-intervention group were prescribed antibiotics for the appropriate duration of time, in comparison to 22 patients (38.6%) in the pre-intervention group (P <0.01) [Figure 1].
Figure 1:
Proportion of patients whose antibiotic treatment adhered to antimicrobial prophylaxis guidelines prior to (n = 57) and following (n = 97) a multidisciplinary quality improvement project at the King Hussein Cancer Centre, Amman, Jordan. Among the patients, 29 (50.9%) and 95 (100.0%) in the preand post-intervention phase, respectively, were found to require antibiotics according to the guidelines. Use of appropriate antibiotics and appropriate doses were subsequently assessed for the patients who received antibiotics in accordance with the guidelines.
Among patients who were prescribed antibiotics, only 29 patients (50.9%) in the pre-intervention phase were found to require antibiotics according to the guidelines. In comparison, all of the patients who were prescribed antibiotics in the post-intervention phase required antibiotics according to the guidelines (n = 95; 100.0%). Of the patients who received antibiotics in accordance with the guidelines, 16 patients (55.2%) received the appropriate antibiotic in the pre-intervention phase while 88 patients (92.6%) received the appropriate antibiotic in the post-intervention group (P <0.01). Furthermore, among those who were correctly prescribed antibiotics according to the guidelines, the number of patients who received appropriate doses of the appropriate antibiotic was 87 (98.9%) in the post-intervention group compared to nine (56.3%) in the pre-intervention group (P <0.01) [Figure 1].
Discussion
This study revealed poor adherence to the surgical prophylaxis guidelines at KHCC in the pre-intervention phase. This lack of adherence was attributed mainly to the absence of comprehensive institutional guidelines, easy accessibility to several antibiotics that were not included in the guidelines and a lack of awareness about the guidelines. These pre-intervention findings are consistent with those reported by other studies at both local and international hospitals.1–4,7 However, significant improvement was observed in the adherence to surgical prophylaxis guidelines after the implementation of a multidisciplinary quality improvement project in the current study, particularly with regards to the appropriateness, dosage, timing and duration of antibiotic therapy. To the best of the authors’ knowledge, this is the first study to evaluate a comprehensive approach aiming to improve adherence to antimicrobial prophylaxis guidelines.
The implementation of institutional protocols and guidelines for surgical prophylaxis plays a major role in guiding surgeons to use the most appropriate anti- biotic and dose based on evidence-based recommendations. These guidelines should be tailored to the needs of each institution based on the most common types of surgeries performed and the antibiotics available. In a study conducted by Willemsen et al., a standardised, clear and simple protocol for perioperative antibiotic prophylaxis was associated with improvement in antibiotic dosing and timing.14 In the current study, the pre-intervention guidelines did not include recommendations for breast surgery even though it was one of the most common surgeries performed at KHCC. As with any programme, education is essential to promote evidence-based practice. However, educational intervention alone is not sufficient to change practice, as demonstrated by Ozgun et al.15 In their study, the educational intervention resulted in improvements in indications, choice and dosage of surgical antimicrobial prophylaxis but did not result in improved prophylaxis use or total compliance rate. The researchers suggested that educational interventions should be augmented with protocols and guidelines in order to improve overall adherence.15
In the current study, the authors believe that the presence of a clinical pharmacist on the surgery floor was essential in encouraging adherence to the revised antimicrobial prophylaxis guidelines. This clinical pharmacist helped with specific recommendations related to prescribed antibiotics and offered one-to-one and group educational sessions for surgical residents. Unfortunately, the exact number of interventions conducted by the pharmacist during the post-intervention phase was not recorded but anecdotal evidence from surgical and pharmaceutical department staff members indicated that these were numerous. Additionally, the implementation of an ORSP was extremely helpful, as the close proximity of the pharmacy to the operating room ensured the timely delivery of the antibiotics and administration of the medication one hour prior to incision. In a recent study, the presence of a pharmacist in a surgical department was associated with a decrease in the number of patients receiving prophylactic antibiotics without justifiable indications, a decrease in the rate of prolonged duration of prophylaxis and an increase in the number of patients receiving correct antibiotics.16
A significant improvement in the adherence to antimicrobial prophylaxis guidelines was noted in the current study after the implementation of a quality improvement project. The provision of multidisciplinary revised guidelines and educational sessions clearly played a major role in the improved compliance observed in the post-intervention phase. This may have been due to the presence of clear guidelines that outlined the appropriate antibiotics for common surgeries, along with increased knowledge among physicians and surgeons regarding appropriate practices in terms of the appropriate drug, dose and duration. However, there are a few limitations to the study. These limitations include the short duration and relatively small sample size in both the pre- and post-intervention groups. Furthermore, only the total impact of the quality improvement project was measured; the effect of each individual element of the project on the adherence to the guidelines was not determined. Finally, the incidence of post-surgical infections was not evaluated. Future studies are recommended to explore adherence to antimicrobial prophylaxis on the rate of post-surgical infections.
Conclusion
A multidisciplinary quality improvement project carried out at KHCC resulted in a significant improvement in adherence to antimicrobial prophylaxis guidelines among surgical staff. In the post-intervention stage, a significant improvement was seen in the correct choice of antibiotic administered as well as the timing, duration and dosage of antibiotics. Surgical antimicrobial prophylaxis is necessary to reduce the incidence of potential SSIs. The results of this study suggest that a focused multidisciplinary intervention can enhance adherence to institutional antimicrobial prophylaxis guidelines.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
References
- 1.de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: Incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–97. doi: 10.1016/j.ajic.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 2.Weber WP, Zwahlen M, Reck S, Feder-Mengus C, Misteli H, Rosenthal R, et al. Economic burden of surgical site infections at a European university hospital. Infect Control Hosp Epidemiol. 2008;29:623–9. doi: 10.1086/589331. [DOI] [PubMed] [Google Scholar]
- 3.Anderson DJ. Surgical site infections. Infect Dis Clin North Am. 2011;25:135–53. doi: 10.1016/j.idc.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: Adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23:183–9. doi: 10.1086/502033. [DOI] [PubMed] [Google Scholar]
- 5.Dhar H, Al-Busaidi I, Rathi B, Nimre EA, Sachdeva V, Hamdi I. A study of post-Caesarean section wound infections in a regional referral hospital, Oman. Sultan Qaboos Univ Med J. 2014;14:e211–17. [PMC free article] [PubMed] [Google Scholar]
- 6.American Society of Health-System Pharmacists ASHP therapeutic guidelines on antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 1999;56:1839–88. doi: 10.1093/ajhp/56.18.1839. [DOI] [PubMed] [Google Scholar]
- 7.Goede WJ, Lovely JK, Thompson RL, Cima RR. Assessment of prophylactic antibiotic use in patients with surgical site infections. Hosp Pharm. 2013;48:560–7. doi: 10.1310/hpj4807-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tourmousoglou CE, Yiannakopoulou EC, Kalapothaki V, Bramis J, St Papadopoulos J. Adherence to guidelines for antibiotic prophylaxis in general surgery: A critical appraisal. J Antimicrob Chemother. 2008;61:214–18. doi: 10.1093/jac/dkm406. [DOI] [PubMed] [Google Scholar]
- 9.Al-Momany NH, Al-Bakri AG, Makahleh ZM, Wazaify MM. Adherence to international antimicrobial prophylaxis guidelines in cardiac surgery: A Jordanian study demonstrates need for quality improvement. J Manag Care Pharm. 2009;15:262–71. doi: 10.18553/jmcp.2009.15.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parulekar L, Soman R, Singhal T, Rodrigues C, Dastur FD, Mehta A. How good is compliance with surgical antibiotic prophylaxis guidelines in a tertiary care private hospital in India? A prospective study. Indian J Surg. 2009;71:15–18. doi: 10.1007/s12262-009-0004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hosoglu S, Sunbul M, Erol S, Altindis M, Caylan R, Demirdag K, et al. A national survey of surgical antibiotic prophylaxis in Turkey. Infect Control Hosp Epidemiol. 2003;24:758–61. doi: 10.1086/502127. [DOI] [PubMed] [Google Scholar]
- 12.Al-Azzam SI, Alzoubi KH, Mhaidat NM, Haddadin RD, Masadeh MM, Tumah HN, et al. Preoperative antibiotic prophylaxis practice and guideline adherence in Jordan: A multi-centre study in Jordanian hospitals. J Infect Dev Ctries. 2012;6:715–20. doi: 10.3855/jidc.1676. [DOI] [PubMed] [Google Scholar]
- 13.Abdel-Aziz A, El-Menyar A, Al-Thani H, Zarour A, Parchani A, Asim M, et al. Adherence of surgeons to antimicrobial prophylaxis guidelines in a tertiary general hospital in a rapidly developing country. Adv Pharmacol Sci. 2013;2013:842593. doi: 10.1155/2013/842593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Willemsen I, van den Broek R, Bijsterveldt T, van Hattum P, Winters M, Andriesse G, et al. A standardized protocol for perioperative antibiotic prophylaxis is associated with improvement of timing and reduction of costs. J Hosp Infect. 2007;67:156–60. doi: 10.1016/j.jhin.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 15.Ozgun H, Ertugrul BM, Soyder A, Ozturk B, Aydemir M. Perioperative antibiotic prophylaxis: Adherence to guidelines and effects of educational intervention. Int J Surg. 2010;8:159–63. doi: 10.1016/j.ijsu.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Zhang HX, Li X, Huo HQ, Liang P, Zhang JP, Ge WH. Pharmacist interventions for prophylactic antibiotic use in urological inpatients undergoing clean or clean-contaminated operations in a Chinese hospital. PLoS One. 2014;9:e88971. doi: 10.1371/journal.pone.0088971. [DOI] [PMC free article] [PubMed] [Google Scholar]