Abstract
Pulmonary myiasis is an unusual form of myiasis in humans and has been recently identified as a cause of eosinophilic pneumonia. We report the case of a 13-year-old Omani boy who presented to the Royal Hospital, Muscat, Oman, in October 2014 with respiratory distress. Bronchial aspirates revealed features of eosinophilic pneumonia. Possible larvae identified in the cytology report, a high immunoglobulin E level and the patient history all indicated bronchial myiasis. The patient was treated with steroids and ventilation and has since been disease-free with no long-term side-effects. To the best of the authors’ knowledge, this is the first case of bronchial myiasis in Oman.
Keywords: Myiasis, Eosinophilic Pneumonia, Case Report, Oman
Myiasis is the infestation of the vertebrate tissues with fly larvae. Most human cases of myiasis in Oman are ophthalmomyiasis caused by Oestrus ovis (sheep bot fly) of the Oestridae family.1,2 Tracheopulmonary myiasis is very rare with only a few cases reported worldwide.3–9 This case report presents a 13-year-old Omani boy with an unusual case of bronchial myiasis resulting from the inhalation of mature larvae which caused a severe pulmonary reaction. A literature review of all reported cases of tracheopulmonary myiasis is also presented. Myiasis due to O. ovis remains a rare cause of pulmonary disease and is a newly described cause of eosinophilic pneumonia in humans.9
Case Report
In October 2014, a previously healthy 13-year-old boy from a mountainous area of interior Oman reported inhaling a fly and experiencing a subsequent sudden coughing fit. Upon inspection by a relative, all that could be seen was some white thready material at the back of his throat. He presented to the local health centre with a progressive cough and breathing difficulty. The patient was hypoxic with an oxygen (O2) saturation level of 90% when breathing room air. He was wheezy and in severe respiratory distress. He received salbutamol nebulisation without noticeable improvement. He was transferred to a regional hospital on the same day where he was adequately managed for wheezing. However, the patient remained hypoxic, requiring 3 L of O2 to maintain an O2 saturation level above 92%. As the patient was not improving, he was referred the next day to the Paediatric Emergency Department at the Royal Hospital, a tertiary centre in Muscat, Oman, for an urgent bronchoscopy. On examination, he was found to be in severe respiratory distress, with wheezes on the right side of his upper chest and minimal air entry. He was subsequently moved to the Paediatric Intensive Care Unit (PICU).
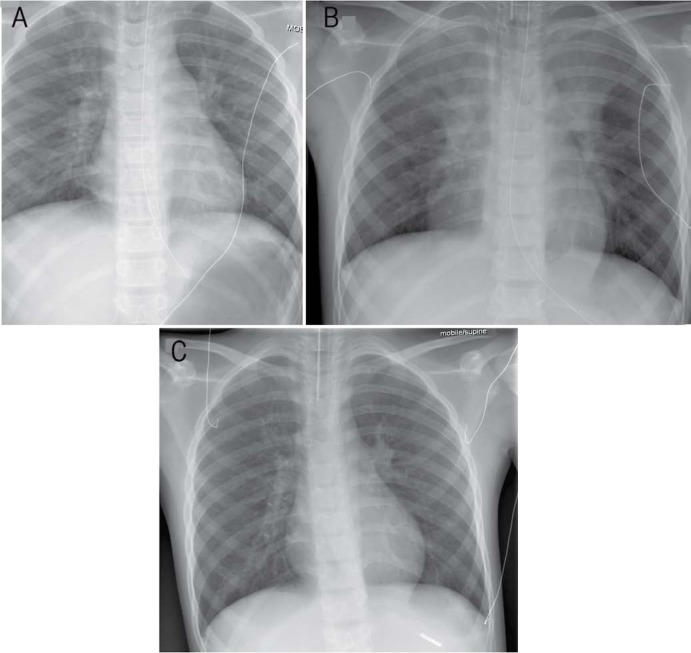
In the PICU, the patient was alert and conscious but still struggling to breathe; he needed 5 L of O2 administered via a face mask and could only maintain an O2 saturation level of 90%. Due to persistent hypoxia, the patient was intubated with a 6.5 size cuffed tube and mechanically ventilated for 10 days with synchronised intermittent mandatory ventilation with volume control. A direct laryngoscopy did not reveal any obvious vocal cord oedema. Flexible bronchoscopy showed oedema and thick secretions in the right upper lobe and superior segment of the right lower lobe. However, no obvious foreign body was isolated. The patient developed anaphylactic shock and was treated with a 12-hour adrenaline infusion with good response. A repeat flexible bronchoscopy after two days revealed thick whitish mucous casts but no foreign body. This time, involvement of the left side was also noted. X-rays showed an initial worsening of the pneumonia followed by gradual improvement after four days of high-frequency oscillatory ventilation (HFOV) [Figure 1]. Post-extubation, he did not require any further O2.
Figure 1A–C:
Portable post-intubation supine chest X-rays of a patient with pulmonary myiasis and eosinophilic pneumonia at (A) admission, (B) two days later and (C) four days after high-frequency oscillatory ventilation (HFOV). Note the worsening pneumonia with bilateral involvement and the improvement after HFOV.
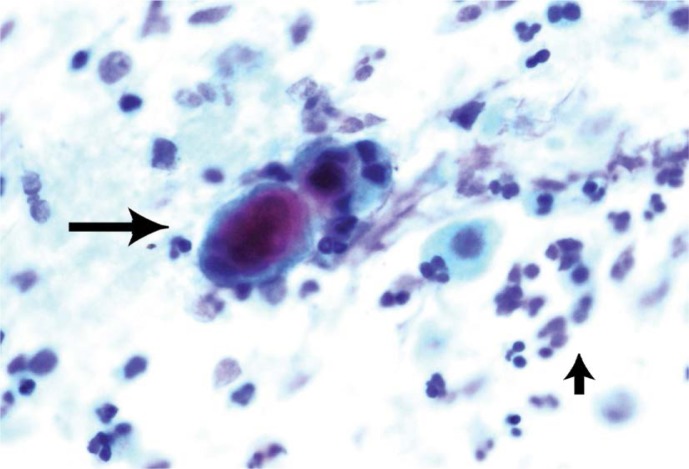
Cytology of the bronchial aspirate revealed eosinophils in scattered clusters. Many neutrophils, macrophages and lymphocytes were also admixed with a thick mucus. Occasional small oval structures (possibly larvae) were identified [Figure 2] along with a few Charcot-Leyden crystals. There were no bacteria or fungi isolated in the culture and a complete blood count did not show any eosinophilia. The presence of the eosinophilic clusters and Charcot-Leyden crystals in the cytology report suggested a diagnosis of eosinophilic pneumonia. The presence of possible larvae in the cytology report, a high immunoglobulin E level (897 IU/mL) and the patient history all pointed towards a parasitic cause. The eosinophilic pneumonia was treated with 14-day courses of intravenous hydrocortisone and ceftriaxone, the former of which was then tapered off over the following seven days.
Figure 2:
Papanicolaou stain at ×400 magnification showing an amphiphilic structure (large arrow) consistent with an Oestrus ovis larva in a patient with pulmonary myiasis and eosinophilic pneumonia. Note the inflammatory infiltrate with a predominance of eosinophils (small arrow).
Discussion
Myiasis is caused by the invasion of human or animal tissues by fly larvae (maggots) and can be classified as accidental, facultative or obligate. Human cases are mostly accidental. In terms of the present case, the responsible organism for the myiasis was likely to be O. ovis, locally known as dis’sa, because the fly is known to lay its larvae during flight and the species is very common in the patient’s home region. The eyes are usually affected in most cases of O. ovis involvement.1,2,10 Many people living in the same area as the patient, including the boy’s father, had had a history of conjunctivitis and coughing.
O. ovis is found worldwide and is known to cause cavitary myiasis. Its hosts are sheep and goats and there is as yet no confirmation that O. ovis is able to complete its life cycle in humans. The female fly is active during the summer and early autumn, when it deposits as many as 500 already hatched first instar larvae. Direct contact between the fly and its host is not necessary for infestation.10 O. ovis is the most common cause of external ophthalmomyiasis and may cause many allergic manifestations, especially when found in the throat.11,12
Tracheopulmonary myiasis is a very rare form of the disease; to date, only seven cases have been reported worldwide [Table 1].3–9 The geographical distribution of cases is varied (including the USA, Brazil, Japan and Korea) and no specific age group or gender is targeted. Causative organisms range from Cuterebra fontinella, Megaselia spicularis, Alouattamyia baeri and the Lucilia and Gasterophilus genera and Cuterebrinae subfamily. Although the likelihood of human infestation is rare, the severe medical complications and the varied worldwide distribution indicates the medical importance of this condition. As with the current patient, those suspected of having tracheopulmonary myiasis (i.e. those with severe respiratory distress and hypoxia and living in fly-prevalent regions) should be urgently treated at a tertiary care centre.
Table 1:
Demographic and entomological characteristics of tracheopulmonary myiasis cases in the literature
| Author and year of report | Patient age in years and gender | Location | Suspected causative organism | Involvement | Confirmatory findings | Larvae stage |
|---|---|---|---|---|---|---|
| Ahmed et al.3 1969 | N/A | USA | Gasterophilus genus | Pulmonary | N/A | N/A |
| Scholten et al.5 1977 | 22 M | Canada | Cuterebra fontinella | Tracheal | Patient coughed up larvae | Instar 2 |
| Komori et al.7 1978 | 19 M | Japan | Megaselia spiracularis | Pulmonary | Larvae on lung biopsy | Instar 3 |
| Baird et al.4 1979 | 22 M | USA | Cuterebra subgenus | Bronchial | Patient coughed up larvae | Instar 2 |
| Fraiha et al.6 1984 | N/A | Brazil | Alouattamyia baeri | N/A | N/A | N/A |
| Choi et al.8 2002 | 84 F | Korea | Lucilia genus | Pulmonary | Larvae crawled out of patient’s nose | N/A |
| Cornet et al.9 2002 | 60 F | USA | Cuterebra subgenus | Tracheal | Patient coughed up larvae | Instar 3 |
| Present case | 13 M | Oman | Oestrus ovis | Bronchial | Bronchial aspirates | N/A |
N/A = not available; M = male; F = female.
Eosinophilic pneumonia is a condition describing an accumulation of eosinophils in the lungs. Known causes include certain medications, parasitic infections, cancer, environmental triggers and immunogenic factors. The prognosis is very good and patients usually respond well to steroid treatment. Parasites can cause eosinophilic pneumonia in three different ways: either by invading the lung, living in the lung as part of their life cycle or spreading to the lung through the bloodstream. Tapeworms, helminths and Japanese lung flukes are the most common parasites. Fly larvae infestation has recently been reported as a cause of eosinophilic pneumonia and is a very rare entity.9
A few cases of ophthalmomyiasis have been reported in Oman; however, only some of these were caused by O. ovis.1,2 There have been no reported cases of bronchial myiasis in Oman to date. The current case represents the first report of bronchial myiasis in Oman and the Middle East with eosinophilic pneumonia requiring mechanical ventilatory support, including HFOV, despite treatment with steroids.
Conclusion
Bronchial myiasis can be a life-threatening infestation and should be considered in the differential diagnosis of unexplained respiratory distress and hypoxia in individuals from fly-prevalent areas. Patients should be urgently referred to a tertiary centre for effective management and care. To the best of the authors’ knowledge, this is the first case of bronchial myiasis in Oman. The patient presented with eosinophilic pneumonia and the causative organism was likely O. ovis.
References
- 1.Victor R, Bhargva K. Ophthalmomyiasis in Oman: A case report and comments. Wilderness Environ Med. 1998;9:32–5. doi: 10.1580/1080-6032(1998)009[0032:OIOACR]2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Abuelhassan AA. External ophthalmomyiasis due to Oestrus ovis: A case report from Oman. Oman Med J. 2010;25 doi: 10.5001/omj.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed MJ, Miller A. Pulmonary coin lesion containing a horse bot, Gasterophilus; Report of a case of myiasis. Am J Clin Pathol. 1969;52:414–19. doi: 10.1093/ajcp/52.4.414. [DOI] [PubMed] [Google Scholar]
- 4.Baird CR, Podgore JK, Sabrosky CW. Cuterebra myiasis in humans: Six new case reports from the United States with a summary of known cases (Diptera: Cuterebridae) J Med Entomol. 1982;19:263–7. doi: 10.1093/jmedent/19.3.263. [DOI] [PubMed] [Google Scholar]
- 5.Scholten T, Chrom VH. Myiasis due to Cuterebra in humans. Can Med Assoc J. 1979;120:1392–3. [PMC free article] [PubMed] [Google Scholar]
- 6.Fraiha H, Chaves LC, Borges IC, de Freitas RB. [Human myiasis in Amazonia - III: Myiasis of the lung due to Alouattamyia baeri (Shannon & Greene, 1926) (Diptera, Cuterebridae)] Seperata da Revista da Fundaçao Sesp. 1984;29:63–8. [Google Scholar]
- 7.Komori K, Hara K, Smith KG, Oda T, Karamine D. A case of lung myiasis caused by larvae of Megaselia spiracularis Schmitz (Diptera: Phoridae) Trans R Soc Trop Med Hyg. 1978;72:467–70. doi: 10.1016/0035-9203(78)90165-7. [DOI] [PubMed] [Google Scholar]
- 8.Choi E, Lim D, Na M, Yang J, Lee Y, Lee W. A case of internal myiasis of the respiratory system associated with pneumonia. Tuberc Respir Dis. 2002;53:650–5. [Google Scholar]
- 9.Cornet M, Florent M, Lefebvre A, Wertheimer C, Perez-Eid C, Bangs MJ, et al. Tracheopulmonary myiasis caused by a mature third-instar Cuterebra larva: Case report and review. J Clin Microbiol. 2003;41:5810–12. doi: 10.1128/JCM.41.12.5810-5812.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cameron JA, Shoukrey NM, al-Garni AA. Conjunctival ophthalmomyiasis caused by the sheep nasal botfly (Oestrus ovis) Am J Ophthalmol. 1991;112:331–4. doi: 10.1016/S0002-9394(14)76736-4. [DOI] [PubMed] [Google Scholar]
- 11.Francesconi F, Lupi O. Myiasis. Clin Microbiol Rev. 2012;25:79–105. doi: 10.1128/CMR.00010-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Masoodi M, Hosseini K. The respiratory and allergic manifestations of human myiasis caused by larvae of the sheep bot fly (Oestrus ovis): A report of 33 pharyngeal cases from southern Iran. Ann Trop Med Parasitol. 2003;97:75–81. doi: 10.1179/136485913X13789813917706. [DOI] [PubMed] [Google Scholar]