The transverse rectus abdominus musculocutaneous (TRAM) and deep inferior epigastric perforator (DIEP) flaps share the same fundamental vascular structure and have become preferred methods in autologous breast reconstruction. Despite their utility, however, venous congestion still occurs in a small percentage of flaps during and after surgery. Although strategies exist for salvaging DIEP flaps with intraoperative congestion, it is not always recognized nor has its incidence been extensively investigated. This literature review aimed to raise awareness of intraoperative congestion of TRAM and DIEP flaps, and to discuss clinical incidence and preventive and salvage strategies.
Keywords: DIEP flap, TRAM flap, Venous congestion
Abstract
BACKGROUND:
Even with patent deep inferior epigastric vein anastomoses, venous congestion can occur during free transverse rectus abdominis musculocutaneous (TRAM) or deep inferior epigastric artery perforator (DIEP) flap surgery and lead to flap compromise if not recognized and managed.
OBJECTIVES:
To identify the incidence of intraoperative venous congestion and describe the best available prevention and treatment methods.
METHODS:
Systematic electronic searches of the PubMed database including Medline were performed to identify studies published until 2014. The following keywords were used: “DIEP” or “free TRAM” and “venous insufficiency” or “venous congestion”. Supplemental searches were conducted to identify referenced studies. Statistical analysis using the χ2 test was performed.
RESULTS:
Nine studies representing 4747 free abdominal flaps cases were included and demonstrated an overall incidence of intraoperative venous congestion of 2.8%. The incidence in DIEP flaps (3.3%) was significantly higher than that in the free TRAM flaps (1.0%). All nine articles reported using the superficial inferior epigastric vein to treat venous insufficiency.
CONCLUSION:
The risk for developing intraoperative venous congestion following free abdominal flap breast reconstruction is influenced by inadequate perforator selection and persistent dominance in the superficial venous system. The solution is establishing another venous draining route using the superficial inferior epigastric vein.
Abstract
HISTORIQUE :
Malgré des anastomoses de la veine épigastrique inférieure profonde perméable, une congestion veineuse peut survenir pendant une chirurgie par lambeau libre musculocutané du grand droit transverse (MGDT) ou par lambeau perforant de l’artère épigastrique inférieure profonde (AEIP) et compromettre le lambeau si elle n’est pas décelée et prise en charge.
OBJECTIFS :
Déterminer l’incidence de congestion veineuse peropératoire et décrire les meilleures méthodes préventives et thérapeutiques en place.
MÉTHODOLOGIE :
Les chercheurs ont effectué des recherches virtuelles systématiques dans la base de données PubMed, y compris dans Medline, pour extraire les études publiées jusqu’en 2014. Ils ont utilisé les mots-clés suivants : DIEP ou free TRAM et venous insufficiency ou venous congestion. Ils ont mené d’autres recherches pour extraire les études des références. Ils ont effectué une analyse statistique au moyen du test du chi carré.
RÉSULTATS :
Neuf études représentant 4 747 cas de lambeaux abdominaux libres ont été incluses, pour démontrer une incidence globale de congestion veineuse peropératoire de 2,8 %. L’incidence de lambeaux AEIP (3,3 %) était considérablement plus élevée que celle de lambeaux libres MGDT (1,0 %). Dans les neuf articles, la veine épigastrique inférieure profonde était utilisée pour traiter l’insuffisance veineuse.
CONCLUSION :
Le risque de congestion veineuse peropératoire après une reconstruction mammaire par lambeaux abdominaux libres est influencé par une mauvaise sélection du lambeau perforant et une dominance persistante du système veineux superficiel. La solution consiste à établir une autre voie de drainage veineux au moyen de la veine épigastrique inférieure superficielle.
One of the preferred methods for autologous breast reconstruction is microsurgical reconstruction using abdominal tissue, including the free transverse rectus abdominis musculocutaneous (TRAM) and deep inferior epigastric perforator (DIEP) flaps because these result in the most natural-looking breast (1–3). Free TRAM flap reconstruction is the standard method; DIEP flap reconstruction was developed from TRAM and demonstrates less postoperative pain and morbidity at the donor site (1,3–5). Importantly, these two flaps share the same fundamental vascular structure.
Despite improvements in microsurgical techniques, venous congestion still occurs in up to 5% of flaps and remains an important cause of flap loss if not recognized and managed (2,6,7). While most venous complications are associated with microsurgical problems, some cases of venous congestion develop without microsurgical errors, which can be apparent immediately after flap elevation (Video 1) or successful deep inferior epigastric vein (DIEV) anastomoses. The entire flap is typically involved, and the perforators and main vessels show no signs of venous outflow problems such as dilated veins filled with dark-coloured blood. This is mostly accompanied by an engorged superficial inferior epigastric vein (SIEV). This type of venous congestion in the TRAM or DIEP flap can be termed ‘intraoperative venous congestion’, which is assumed to be associated with an ineffective venous structure of the flap. Recent studies report that intraoperative venous congestion without microsurgical failure could be due to inappropriate perforator selection or poor connection between the DIEV and SIEV systems, which is believed to predominate in venous drainage of the lower abdominal integument (7–10). Several studies describe various strategies for salvage of the DIEP flap with intraoperative venous congestion, including the use of secondary alternate pathways or supercharging the venous drainage of the congested flaps (5,6,11–17). However, intraoperative venous congestion is not always recognized and its incidence has not been investigated.
Herein, we review the current literature regarding intraoperative venous congestion in the free TRAM and DIEP flaps, with a particular focus on clinical incidence, preventable findings and salvage strategies. We believe our efforts provide awareness of intraoperative venous congestion and comprehensive information to improve flap success.
METHODS
An electronic search of PubMed, including Medline, Scopus, Embase and Web of Science, and a manual search of references were conducted to identify studies published until 2014 that reported intraoperative venous congestion or venous insufficiency despite patent DIEV anastomosis in free DIEP or TRAM flaps breast reconstruction. The following keywords were used: “DIEP” or “free TRAM” and “venous insufficiency” or “venous congestion”. Articles were considered to be relevant if they described intraoperative venous congestion or widespread venous insufficiency without pedicle compromise. Each article had to report the incidence of intraoperative venous congestion. Our search was limited to studies on humans that were published in English. Case reports, isolated abstracts, reviews, editorials, communications, correspondence, discussions and letters were excluded. The reference lists of relevant studies were evaluated to identify studies that were missed during the initial database search. A single reviewer performed the initial article search and subsequent selection. After deletion of duplicates, each abstract was reviewed for inclusion criteria. If the abstract did not provide clear inclusion or exclusion criteria, the full text was reviewed before final categorization.
The full text of each relevant article was obtained; the ready accessibility of the full-text articles made immediate evaluation possible. Only studies that successfully passed both levels of screening were included (Figure 1). To be included, cases had to meet the following conditions: whole flap congestion was recognized by the authors during the operation, either after flap elevation or vessel anastomosis; and an additional procedure was performed to augment venous outflow. Collected data included the following: lead author, year of publication, type of reconstruction, total number of reconstructions and total number of identified cases of intraoperative venous congestion.
Figure 1).
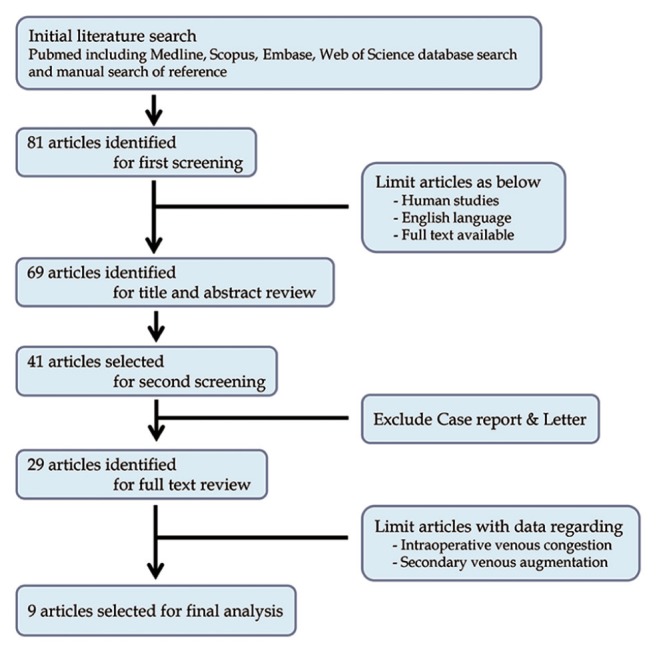
Identification of relevant articles included in the present review
RESULTS
Nine retrospective comparative studies were included (7,11,18–24). Table 1 compares the identified series of cases with free DIEP or TRAM flaps. In total, 3696 DIEP flap cases and 1051 free TRAM flap cases were pooled for further study; 122 DIEP flaps and 10 free TRAM flaps were reported to develop intraoperative venous congestion. The overall mean rate of intraoperative venous congestion was 2.8% (3.3% in DIEP flap cases and 1.0% in free TRAM flap cases). The venous congestion rates of the individual studies were variable and ranged from 0% to 9.3%. Statistical analysis using the Pearson’s χ2 test confirmed that intraoperative venous congestion occured more frequently in the DIEP flap (P<0.001).
TABLE 1.
Incidence of intraoperative venous congestion in deep inferior epigastric artery perforator (DIEP) and free transverse rectus abdominis musculocutaneous (TRAM) flaps
| Author (reference), year | DIEP flap | Free TRAM flap | Free abdominal (TRAM + DIEP) flap | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Total, n | Venous congestion, n (%) | Total, n | Venous congestion, n (%) | Total, n | Venous congestion, n (%) | |
| Ali et al (19), 2010 | 162 | 14 (8.6) | 162 | 14 (8.6) | ||
| Blondeel et al (7), 2000 | 249 | 5 (2.0) | 271 | 0 (0.0) | 520 | 5 (1.0) |
| Figus et al (19), 2006 | 16 | 1 (6.3) | 16 | 1 (6.3) | ||
| Lundberg and Mark (20), 2005 | 50 | 3 (6.0) | 50 | 3 (6.0) | ||
| Ochoa et al (24), 2013 | 2618 | 87 (3.3) | 2618 | 87 (3.3) | ||
| Sbitany et al (21), 2012 | 421 | 1 (0.2) | 780 | 10 (1.3) | 1201 | 11 (0.9) |
| Schaverian et al (22), 2010 | 54 | 5 (9.3) | 54 | 5 (9.3) | ||
| Smit et al (23), 2010 | 26 | 1 (3.8) | 26 | 1 (3.8) | ||
| Tran et al (11), 2007 | 100 | 5 (5.0) | 100 | 5 (5.0) | ||
| Total | 3696 | 122 (3.3)* | 1051 | 10 (1.0)* | 4747 | 132 (2.8) |
Significant difference (P<0.001, Pearson’s χ2 test)
Eight of nine articles reported findings associated with intraoperative venous congestion (Table 2); all reported an engorged SIEV with a diameter >1.5 mm and rapid capillary refill <1 s. Two studies reported preconditions before the diagnosis of intraoperative venous congestion. Ali et al (18) established the diagnosis of intraoperative venous congestion only after conservative treatment for 30 min. Before diagnosis, Tran et al (11) required that there should not be any instance of pedicle torsion, compression or thrombosis.
TABLE 2.
Descriptions of intraoperative venous congestion provided by the included studies
| Author (reference), year | Findings of intraoperative venous congestion |
|---|---|
| Ali et al (18), 2010 | A purplish or plethoric fullness of the flap associated with brisk capillary refill (1 s) |
| Rapid and dark venous bleeding on puncture | |
| No improvement to conservative treatment for 30 min intraoperatively | |
| Engorged (tense and dilated) SIEV | |
| Blondeel et al (7), 2000 | Severe diffuse venous congestion that involved the entire flap |
| Particularly large SIEV (>1.5 mm) | |
| Figus et al (19), 2006 | A turgid superficial vein |
| Lundberg and Mark (20), 2006 | Capillary refill that took <2 s |
| Ochoa et al (24), 2013 | Brisk capillary refill |
| Cutaneous discolouration that improves promptly with release of venous blood through the SIEV | |
| Predominant venous bleeding with peripheral flap incisions | |
| Sbitany et al (21), 2012 | Subjectively engorged SIEV |
| Brisk SIEV bleeding when opened | |
| Positive strip test | |
| Positive venous flow on Doppler ultrasound | |
| Smit et al (23), 2010 | The SIEV is ≥1.5 mm |
| Tran et al (11), 2007 | Intraoperative congestion despite patent deep inferior epigastric venous anastomoses |
| Rapid capillary refill <1 s and a blue flap | |
| No pedicle torsion, compression and thrombosis | |
| The SIEV is ≥1.5 mm |
SIEV Superficial inferior epigastric vein
Various salvage techniques were reported, but they shared common elements. All of the identified studies in the present systematic review report the use of SIEV to provide an additional venous outflow. The differences among them are recipient: the internal mammary vein, DIEV, cephalic vein or chest wall vein. The salvage procedures and outcomes are summarized in Table 3. Four of nine studies report no complications after salvage (19–21,23), and three of these emphasized that the secondary venous outflow should be independent of the DIEV-internal mammary vein drainage (19,20,23). Other studies describe salvage procedures involving DIEV, and reported three cases with partial flap loss and 13 cases with fat necrosis (11,18,22,24).
TABLE 3.
Salvage procedures and outcomes of intraoperative venous congestion.
| Author (reference), year | Salvage procedure | Salvage outcome |
|---|---|---|
| Ali et al (18), 2010 | Additional SIEV outflow to thoracodorsal, IMV or DIEP vena comitantes | 1 partial loss, 1 fat necrosis |
| Blondeel et al (7), 2000 | Additional SIEV outflow to IMV | No information available |
| Figus et al (19), 2006 | Additional SIEV outflow to chest wall perforating vein | 100% survival |
| Lundberg and Mark (20), 2016 | Additional SIEV outflow to cephalic vein | 100% survival |
| Ochoa et al (24), 2013 | Additional SIEV outflow to IMV or DIEP vena comitantes | 11 fat necrosis |
| Sbitany et al (21), 2012 | Additional SIEV outflow to DIEP vena comitantes | 100% survival |
| Schaverien et al (22), 2010 | Additional SIEV outflow to DIEP vena comitantes | 2 partial loss |
| Smit et al (23), 2010 | Additional SIEV outflow to cephalic vein | 100% survival |
| Tran et al (11), 2007 | Additional SIEV outflow to thoracodorsal or DIEP vena comitantes | 1 fat necrosis |
DIEP deep inferior epigastric perforator; IMV Internal mammary vein; SIEV superficial inferior epigastric vein
DISCUSSION
One of the primary purposes of the present study was to heighten awareness of the idiopathic venous congestion of the TRAM or DIEP flaps. Specifically, we intended to investigate flaps that have irreversibly lost the ability to drain the blood effectively; however, the congestion should not be caused by anastomosis failure or vessel damage. Among the many studies reporting the outcome of breast reconstruction using free abdominal flaps, only nine presented data from cases with intraoperative venous congestion. However, it is difficult to confirm that all those cases were true intraoperative idiopathic venous congestion. While two of the studies (11,18) made clear that they distinguished intraoperative venous congestion from the temporary congestion that would recover with time, the other seven did not. Not all studies reported checking patent DIEV anastomoses. Therefore, to obtain consistent data, we only included cases in which an additional venous augmentation procedure was performed. The authors’ decision to perform venous augmentation shows that they must have been convinced that the congestion was not temporary. If the anastomotic problem was the cause of venous congestion, they would easily recognize it and revise the anastomosis. By excluding cases without venous augmentation procedures, we could differentiate from temporary congestion and anastomotic problems.
In several studies reporting the outcome of the breast reconstruction, there is no report of intraoperative venous congestion. If the authors were not aware of the existence of the intraoperative venous congestion, it would be difficult to recognize the problem during the operation. Another explanation may be the rare occurrence of intraoperative venous congestion, which can be found only in reports with a large number of cases. It should be sufficient evidence of the existence of the idiopathic intraoperative venous congestion that nine studies with larger series of free abdominal flap breast reconstruction reported its incidence and management. We systematically reviewed those studies by pooling and analyzing results from different institutions. In total, 4747 free abdominal flaps cases were pooled and demonstrated an overall incidence of intraoperative venous congestion of 2.8%. The incidence in DIEP flaps (3.3%) was significantly different from that in the free TRAM flaps (1.0%).
Although it may be too early to conclude, we believe that the causes of intraoperative venous congestion are the combination of persistent dominance of the superficial venous system and accidental selection of an inadequate perforator. Most cases of intraoperative venous congestion resolved after successful SIEV anastomosis. As reported by Carramenha e Costa et al (25), the SIEV is the largest vein that drains the skin paddle of the DIEP flap or free TRAM flap, suggesting that venous drainage preferentially takes place through this vessel. Retrograde flow from the superficial to deep venous system occurs through the communicating veins that link the two systems, as illustrated by Rozen et al (26). When the DIEP flap is harvested, the SIEV is interrupted and all the venous drainage is redistributed into the deep system by the small venae comitantes that accompany the perforator. In their excellent study, Schaverien et al (22) used magnetic resonance angiography to evaluate numerous perforators in the lower abdomen, and found that not all perforators were directly connected to the superficial venous system. If an abdominal flap is elevated based on perforators that are not connected to the superficial venous system, the flap can develop venous insufficiency even with perfectly patent perforators and main pedicles. Schaverien et al (22) report that perforators with direct communication to the superficial venous system tend to be larger and more frequently located on the medial row. Although there are contrasting opinions regarding the best number of perforators, the decisive factor that prevents venous insufficiency is selection of the perforators with the direct connection to the superficial venous system. The more perforators included, the larger the chance to connect with the superficial venous system. Differences in the incidence of venous congestion between the DIEP flap and the free TRAM flaps can be explained within the same context. By incorporating multiple perforators into the free TRAM flap, there is a higher chance of direct connection to the superficial venous system; in contrast, the DIEP flap often only has a single or fewer than three perforators.
Close observation of the SIEV is a reliable way to diagnose intraoperative venous congestion during flap elevation. Six of the nine studies reviewed herein mentioned intraoperative venous congestion in association with SIEV dilation. The size of the SIEV at the beginning of DIEP flap dissection can be an indicator of the predominance of the deep or superficial drainage system, with larger SIEVs demonstrating superficial dominance rather than deep system dominance (27). Therefore, the SIEV should be identified at the beginning of flap elevation and ligated with clips to ensure the easy detection of engorgement. However, SIEV diameter may not be an absolute predictor of venous congestion. A recent study (28) did not show a direct correlation between vessel diameters in the superficial and deep inferior epigastric systems, meaning that the SIEV diameter can be relatively large, but the deep venous system is still large enough to drain the complete flap. Another important clinical finding is a rapid capillary refill in <1 s. In four of the articles we assessed, capillary refill of the flap itself was introduced as an easily assessable way to diagnose venous congestion. Most of all, however, the diagnosis of intraoperative venous congestion is made after confirming the absence of pedicle compromises, as described by Tran et al (11).
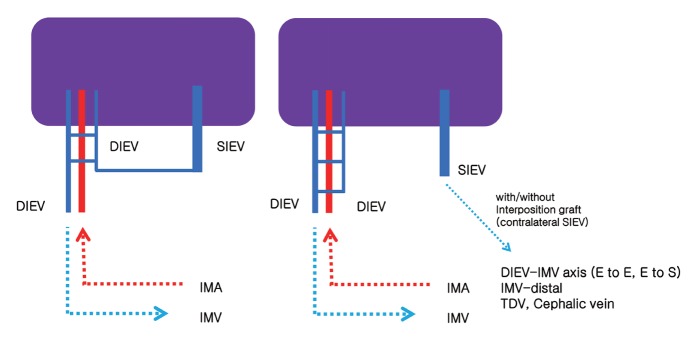
If intraoperative venous congestion is noticed during surgery, venous outflow augmentation is required, rather than revising the original anastomosis. Several successful venous augmentation methods have been introduced (29–31), and all authors prefer using the SIEV as the secondary route for venous drainage. Eight articles in the present study report the outcomes of salvage procedures that used SIEV outflow to treat intraoperative venous congestion. Four of these studies reported excellent results of 100% salvage rate, and minor complications were reported in four articles (11,18,22,24). Using turbo- and supercharging to augment the vascularity of the DIEP flap and the free TRAM flap have been described (Figure 2). Turbocharging requires connecting separate vascular sources within the flap territory using a single recipient pathway, such as bypass between the SIEV and DIEV (29). The concept of connecting the SIEV and DIEV was also proposed by Rohde and Keller (32) and Liu et al (13). However, the effective length of the pedicle is shortened, which can limit flap positioning (33). Supercharging is defined as any vascular augmentation that uses additional recipient vessels, such as the cephalic vein, thoracodorsal vein, lateral thoracic vein or intercostal veins, to provide alternative flow to the flap (6,29,34). The drawbacks of this approach include flap-shaping and inset limitations and the need for an additional recipient vein. Another option for additional venous outflow is to anastomose the SIEV to another internal mammary vein (if available), or to the distal end of the internal mammary vein, to provide anterograde or reverse venous drainage, respectively (7,35). However, our simplest suggestion, which has not been introduced to date, is to dissect one of the venae commitantes of the deep inferior epigastric artery and anastomose the proximal end to the ipsilateral SIEV (Figure 3).
Figure 2).
Intraoperative salvage procedures can be performed utilizing preserved superficial inferior epigastric vein (SIEV). Left Turbocharging technique. To enhance venous drainage for intraoperative venous congestion, a superficial to deep venous loop can be created. Right Supercharging technique. The ipsilateral SIEV is anastomosed directly to deep inferior epigastric vena comitantes-internal mammary vein (DIEV-IMV) axis, distal end of IMV, Thoracodorsal vein (TDV), or cephalic vein with or without interposition vein graft. E to E End-to-end anastomosis; E to S End-to-side anastomosis; IMA Internal mammary artery; IMV-distal Distal end of internal mammary vein
Figure 3).
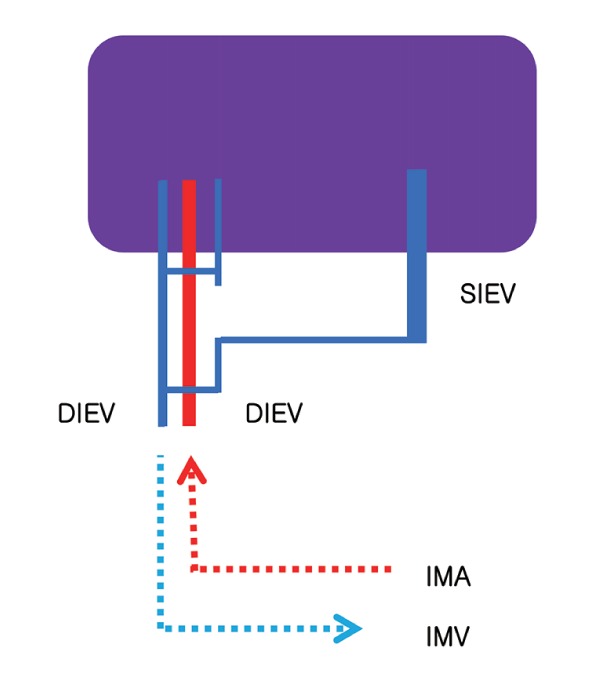
The authors’ method of intraoperative salvage technique using preserved superficial inferior epigastric vein (SIEV). One of the venae commitantes of the deep inferior epigastric artery is dissected toward the flap and its proximal end is connected to SIEV. DIEV Deep inferior epigastric vena comitantes; IMA Internal mammary artery; IMV Internal mammary vein
Venous insufficiency is best addressed by early diagnosis and quick, effective intervention (27). The early establishment of a second route for venous outflow, especially during surgery, leads to the best outcomes. A common necessity of all these techniques, however, is the preservation of an adequately long SIEV, which is worth the extra time and labour. It usually requires <50 min to dissect the SIEVs, prepare the recipient vein and perform microsurgical anastomosis (36). The best timing for additional vein anastomosis is after inset and flap-shaping because the anastomosed SIEV can limit flap mobility.
CONCLUSION
According to the available evidence, intraoperative venous congestion of the free abdominal flap during breast reconstruction demonstrates an incidence of 2.8%. Intraoperative venous congestion is caused by the persistent dominance of the superficial venous system and disconnection between the superficial and deep venous systems, which results from perforators that are not connected to the superficial venous system. The solution is establishing another venous draining route using the SIEV. Thus, dissecting and preserving a long SIEV is crucial for treating intraoperative venous congestion.
Footnotes
DISCLOSURES: None of the authors have financial interests in any of the products, devices or drugs mentioned in this article.
REFERENCES
- 1.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–8. doi: 10.1097/00000637-199401000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Blondeel PN. One hundred free DIEP flap breast reconstructions: A personal experience. Br J Plast Surg. 1999;52:104–11. doi: 10.1054/bjps.1998.3033. [DOI] [PubMed] [Google Scholar]
- 3.Hamdi M, Weiler-Mithoff EM, Webster MH. Deep inferior epigastric perforator flap in breast reconstruction: Experience with the first 50 flaps. Plast Reconstr Surg. 1999;103:86–95. doi: 10.1097/00006534-199901000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Blondeel PN, Boeckx WD. Refinements in free flap breast reconstruction: The free bilateral deep inferior epigastric perforator flap anastomosed to the internal mammary artery. Br J Plast Surg. 1994;47:495–501. doi: 10.1016/0007-1226(94)90033-7. [DOI] [PubMed] [Google Scholar]
- 5.Tutor EG, Auba C, Benito A, Rábago G, Kreutler W. Easy venous superdrainage in DIEP flap breast reconstruction through the intercostal branch. J Reconstr Microsurg. 2002;18:595–8. doi: 10.1055/s-2002-35098. [DOI] [PubMed] [Google Scholar]
- 6.Wechselberger G, Schoeller T, Bauer T, Ninkovic M, Otto A. Venous superdrainage in deep inferior epigastric perforator flap breast reconstruction. Plast Reconstr Surg. 2001;108:162–6. doi: 10.1097/00006534-200107000-00026. [DOI] [PubMed] [Google Scholar]
- 7.Blondeel PN, Arnstein M, Verstraete K, et al. Venous congestion and blood flow in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2000;106:1295–9. doi: 10.1097/00006534-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 8.El-Mrakby HH, Milner RH. The vascular anatomy of the lower anterior abdominal wall: A microdissection study on the deep inferior epigastric vessels and the perforator branches. Plast Reconstr Surg. 2002;109:539–43. doi: 10.1097/00006534-200202000-00020. discussion 544–7. [DOI] [PubMed] [Google Scholar]
- 9.Imanishi N, Nakajima H, Minabe T, Chang H, Aiso S. Anatomical relationship between arteries and veins in the paraumbilical region. Br J Plast Surg. 2003;56:552–6. doi: 10.1016/s0007-1226(03)00207-8. [DOI] [PubMed] [Google Scholar]
- 10.Schaverien M, Saint-Cyr M, Arbique G, Brown SA. Arterial and venous anatomies of the deep inferior epigastric perforator and superficial inferior epigastric artery flaps. Plast Reconstr Surg. 2008;121:1909–19. doi: 10.1097/PRS.0b013e31817151f8. [DOI] [PubMed] [Google Scholar]
- 11.Tran NV, Buchel EW, Convery PA. Microvascular complications of DIEP flaps. Plast Reconstr Surg. 2007;119:1397–405. doi: 10.1097/01.prs.0000256045.71765.96. discussion 1406–8. [DOI] [PubMed] [Google Scholar]
- 12.Niranjan NS, Khandwala AR, Mackenzie DM. Venous augmentation of the free TRAM flap. Br J Plast Surg. 2001;54:335–7. doi: 10.1054/bjps.2000.3587. [DOI] [PubMed] [Google Scholar]
- 13.Liu TS, Ashjian P, Festekjian J. Salvage of congested deep inferior epigastric perforator flap with a reverse flow venous anastomosis. Ann Plast Surg. 2007;59:214–7. doi: 10.1097/01.sap.0000250853.40099.49. [DOI] [PubMed] [Google Scholar]
- 14.Mehrara BJ, Santoro T, Smith A, et al. Alternative venous outflow vessels in microvascular breast reconstruction. Plast Reconstr Surg. 2003;112:448–55. doi: 10.1097/01.PRS.0000070487.94201.30. [DOI] [PubMed] [Google Scholar]
- 15.Villafane O, Gahankari D, Webster M. Superficial inferior epigastric vein (SIEV): “lifeboat” for DIEP/TRAM flaps. Br J Plast Surg. 1999;52:599. doi: 10.1054/bjps.1999.3209. [DOI] [PubMed] [Google Scholar]
- 16.Cavadas PC. Unusual intraoperative venous complication in a free DIEP flap. Plast Reconstr Surg. 2001;107:1312–3. doi: 10.1097/00006534-200104150-00047. [DOI] [PubMed] [Google Scholar]
- 17.Shamsian N, Sassoon E, Haywood R. Salvage of a congested DIEP flap: A new technique. Plast Reconstr Surg. 2008;122:41e–42e. doi: 10.1097/PRS.0b013e31817745c1. [DOI] [PubMed] [Google Scholar]
- 18.Ali R, Bernier C, Lin Y, Te, et al. Surgical strategies to salvage the venous compromised deep inferior epigastric perforator flap. Ann Plast Surg. 2010;65:398–406. doi: 10.1097/SAP.0b013e3181d9ab27. [DOI] [PubMed] [Google Scholar]
- 19.Figus A, Mosahebi A, Ramakrishnan V. Microcirculation in DIEP flaps: A study of the haemodynamics using laser Doppler flowmetry and lightguide reflectance spectrophotometry. J Plast Reconstr Aesthet Surg. 2006;59:604–12. doi: 10.1016/j.bjps.2005.09.047. discussion 613. [DOI] [PubMed] [Google Scholar]
- 20.Lundberg J, Mark H. Avoidance of complications after the use of deep inferior epigastric perforator flaps for reconstruction of the breast. Scand J Plast Reconstr Surg Hand Surg. 2006;40:79–81. doi: 10.1080/02844310500539332. [DOI] [PubMed] [Google Scholar]
- 21.Sbitany H, Mirzabeigi MN, Kovach SJ, Wu LC, Serletti JM. Strategies for recognizing and managing intraoperative venous congestion in abdominally based autologous breast reconstruction. Plast Reconstr Surg. 2012;129:809–15. doi: 10.1097/PRS.0b013e318244222d. [DOI] [PubMed] [Google Scholar]
- 22.Schaverien MV, Ludman CN, Neil-Dwyer J, et al. Relationship between venous congestion and intraflap venous anatomy in DIEP flaps using contrast-enhanced magnetic resonance angiography. Plast Reconstr Surg. 2010;126:385–92. doi: 10.1097/PRS.0b013e3181de2313. [DOI] [PubMed] [Google Scholar]
- 23.Smit JM, Audolfsson T, Whitaker IS, Werker PM, Acosta R, Liss AG. Measuring the pressure in the superficial inferior epigastric vein to monitor for venous congestion in deep inferior epigastric artery perforator breast reconstructions: A pilot study. J Reconstr Microsurg. 2010;26:103–7. doi: 10.1055/s-0029-1243294. [DOI] [PubMed] [Google Scholar]
- 24.Ochoa O, Pisano S, Chrysopoulo M, Ledoux P, Arishita G, Nastala C. Salvage of intraoperative deep inferior epigastric perforator flap venous congestion with augmentation of venous outflow: Flap morbidity and review of the literature. Plast Reconstr Surg Glob Open. 2013;1:e52–e61. doi: 10.1097/GOX.0b013e3182aa8736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carramenha e Costa MA, Carriquiry C, Vasconez LO, Grotting JC, Herrera RH, Windle BH. An anatomic study of the venous drainage of the transverse rectus abdominis musculocutaneous flap. Plast Reconstr Surg. 1987;79:208–17. doi: 10.1097/00006534-198702000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Rozen WM, Pan W-R, Le Roux CM, Taylor GI, Ashton MW. The venous anatomy of the anterior abdominal wall: An anatomical and clinical study. Plast Reconstr Surg. 2009;124:848–53. doi: 10.1097/PRS.0b013e3181b037a2. [DOI] [PubMed] [Google Scholar]
- 27.Cheng M-H, Nguyen A. Invited discussion: A case of intra-operative venous congestion of the entire DIEP flap: A novel salvage technique and review of the literature. Microsurgery. 2010;30:447–8. doi: 10.1002/micr.20775. [DOI] [PubMed] [Google Scholar]
- 28.Ayhan S, Oktar SO, Tuncer S, Yucel C, Kandal S, Demirtas Y. Correlation between vessel diameters of superficial and deep inferior epigastric systems: Doppler ultrasound assessment. J Plast Reconstr Aesthet Surg. 2009;62:1140–7. doi: 10.1016/j.bjps.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 29.Cohn AB, Walton RL. Immediate autologous breast reconstruction using muscle-sparing TRAM flaps with superficial epigastric system turbocharging: A salvage option. J Reconstr Microsurg. 2006;22:153–6. doi: 10.1055/s-2006-939960. [DOI] [PubMed] [Google Scholar]
- 30.Xin Q, Luan J, Mu H, Mu L. Augmentation of venous drainage in deep inferior epigastric perforator flap breast reconstruction: Efficacy and advancement. J Reconstr Microsurg. 2012;28:313–8. doi: 10.1055/s-0032-1311688. [DOI] [PubMed] [Google Scholar]
- 31.Tseng CY, Lang PO, Cipriani NA, Song DH. Pedicle preservation technique for arterial and venous turbocharging of free DIEP and muscle-sparing TRAM flaps. Plast Reconstr Surg. 2007;120:851–4. doi: 10.1097/01.prs.0000277663.50061.83. [DOI] [PubMed] [Google Scholar]
- 32.Rohde C, Keller A. Novel technique for venous augmentation in a free deep inferior epigastric perforator flap. Ann Plast Surg. 2005;55:528–30. doi: 10.1097/01.sap.0000181356.86118.c8. [DOI] [PubMed] [Google Scholar]
- 33.Yang SJ, Eom JS, Lee TJ, Ahn SH, Son BH. Recipient vessel selection in immediate breast reconstruction with free abdominal tissue transfer after nipple-sparing mastectomy. Arch Plast Surg. 2012;39:216–21. doi: 10.5999/aps.2012.39.3.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guzzetti T, Thione A. The basilic vein: An alternative drainage of DIEP flap in severe venous congestion. Microsurgery. 2008;28:555–8. doi: 10.1002/micr.20537. [DOI] [PubMed] [Google Scholar]
- 35.Kerr-Valentic MA, Gottlieb LJ, Agarwal JP. The retrograde limb of the internal mammary vein: An additional outflow option in DIEP flap breast reconstruction. Plast Reconstr Surg. 2009;124:717–21. doi: 10.1097/PRS.0b013e3181b179fc. [DOI] [PubMed] [Google Scholar]
- 36.Eom JS, Sun S, Lee TJ. Selection of the recipient veins for additional anastomosis of the superficial inferior epigastric vein in breast reconstruction with free transverse rectus abdominis musculocutaneous or deep inferior epigastric artery perforator flaps. Ann Plast Surg. 2011;67:505–9. doi: 10.1097/SAP.0b013e31820bcd5f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.