Abstract
Background
Little is known about the opinions of primary care clinicians regarding the newly released 2013 ACC/AHA (American College of Cardiology/American Heart Association) Guidelines for the Prevention of Primary and Secondary Atherosclerotic Disease. This survey was created to assess the awareness, attitudes and practices of primary care clinicians on adoption of the new guidelines and to explore obstacles to implementation and suggestions for improved shared decision making.
Methods
600 practicing clinicians within the San Francisco Bay Area Collaborative Research Network were invited to participate in this cross-sectional, internet-based pilot survey of primary care clinicians. These survey data were collected in March 2014, approximately four months after the release of the new guidelines and one month after the release of the ACC/AHA risk estimator application.
Results
183 clinicians responded to the survey. Of those respondents, 176 (96%) were aware of the guidelines. The majority (64%) reported implementing the new guidelines with at least some of their patients, while a minority (25%) reported adopting the guidelines for many of their patients. Disagreeing with the guidelines was the main hindrance to adoption.
Conclusions
While many primary care clinicians are aware of the new guidelines, a substantial proportion has yet to implement them into their clinical practice and obstacles remain for full adoption. Further understanding of clinicians’ views, opinions and needs is necessary to optimize the approach to lipid management and ensure integration into current practice.
Keywords: AHA/ACC Guidelines, Primary Care Providers, cholesterol
Introduction
The American College of Cardiology (ACC) and American Heart Association (AHA) released updated guidelines for prevention of primary and secondary atherosclerotic disease in late 2013.1 The new guidelines emphasized treatment decisions based on risk stratification for atherosclerotic cardiovascular disease rather than lipid targets for cholesterol management, and lowered the threshold for consideration of drug therapy for primary prevention of vascular events. These changes have attracted controversy – ranging from concerns regarding the accuracy of the published 10-year risk calculator for atherosclerotic cardiovascular disease, to the absence of lipid treatment targets, to the anticipated expansion of statin usage in the general population. In response, subsequent publications have reported reassuring performance characteristics for the risk calculator and emphasized the importance of shared decision making and ensuring the effectiveness of treatment with statin or non-statin agents, as outlined in the guidelines.2–10
Outside of academic discourse regarding the changes, limited information is available on the overall reception to the new guidelines by primary care clinicians. The perspective of primary care physicians and their evolving adoption of the new guidelines are important as these clinicians are on the forefront of lipid management. The purpose of this pilot study was to gauge awareness, practices and attitudes of primary care clinicians participating in the San Francisco Bay Area Collaborative Research Network on the implementation of the new guidelines in clinical practice. This study is a first step in the broader understanding of the reception of the new guidelines by primary care clinicians.
Methods
The San Francisco Bay Area Collaborative Research Network is a University of California, San Francisco supported practice-based research network that includes over 1,500 researchers, clinicians, and healthcare organization leaders working in more than 200 public, private, and academic settings across the greater San Francisco Bay Area and Northern California. The network’s mission is to facilitate practice based research partnerships between academic researchers and community based clinical teams that can lead to improved primary care clinical outcomes.11
Six hundred actively practicing adult primary care clinicians within this network were invited via email to participate in an anonymous online survey in March of 2014, approximately four months after the debut of the cholesterol guidelines. Survey questions assessed respondents’ familiarity with the guidelines, their current or future plans for implementation, and barriers to adoption in clinical practice. Additional questions gauged respondents’ views on the online risk calculator and tools for shared decision making. Response options were categorical and included multiple choices; one qualitative, explanatory question inviting free text responses was also included. Age and gender were collected from all respondents. The study was approved by the Committee of Human Research at the University of California, San Francisco and the survey instrument is included in the appendix.
Categorical responses were analyzed using chi-square as appropriate. Categorical responses by age were further analyzed by chi-square for the trend. To explore age and gender differences in the reception of the new guidelines further, responders were stratified into 3 age groups (21–39, 40–55, and ≥56 years of age) and also by gender. A p-value of less than 0.05 was considered significant for all tests. Qualitative responses were thematically coded based on themes that emerged from the data. Representative quotations from respondents that illustrate the main themes identified are included in the results section.
Results
Of the 600 primary care clinicians invited, 183 (31%) completed the survey. Based on available data of those invited to participate, 52% were female. The majority (79%) of invited clinicians practiced in non-academic centers such as community health centers or private practice. Additionally, approximately 13% were nurse practitioners or physician assistants, with 60% of physicians practicing family medicine and the remainder general internal medicine. Of the 183 respondents, most were female (n=108, 59%) and 40 to 55 years of age (n=74, 40%) [Table 1]. The remainder were equally divided into younger (21–39 years; n=52, 28%) or older (≥56 years; n=51, 28%) age groups.
Table 1.
Demographics
| Number: 183 (%) | |
|---|---|
| Age | |
| 21–39 | 52 (28.4) |
| 40–55 | 74 (40.4) |
| 56–70 | 49 (26.8) |
| 71+ | 2 (1.1) |
| No Age Specified | 6 (3.3) |
| Gender | |
| Male | 70 (38.3) |
| Female | 108 (59.0) |
| No Gender Specified | 5 (2.7) |
Familiarity with the updated guidelines
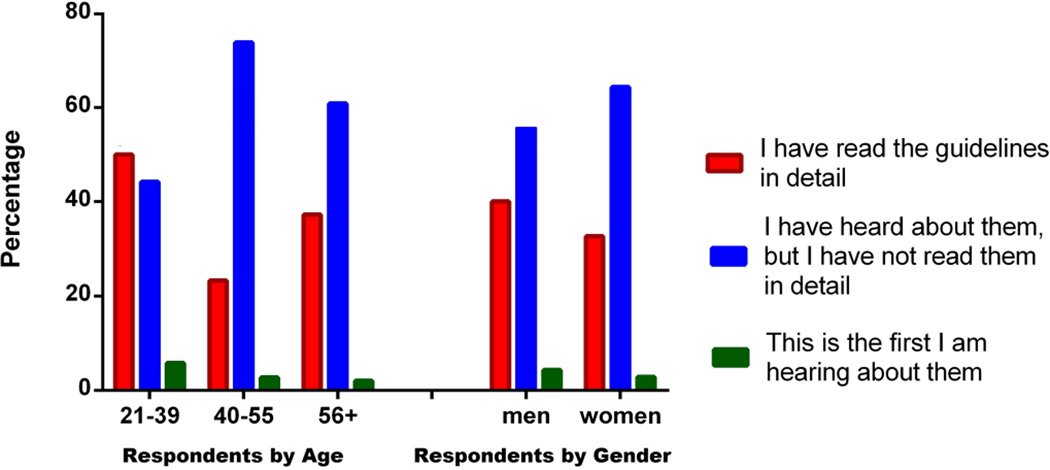
The majority of respondents (n= 176, 96%) reported being aware of the 2013 ACC/AHA cholesterol guidelines and their main tenets, either by reading them in detail or by hearing about them in other venues. Guideline familiarity did not vary by the age or gender of clinicians [Figure 1] [Table 2a].
Figure 1.
Clinicians’ Reported Familiarity with the New 2013 AHA/ACC Guidelines – by age and gender
Table 2.
Representative Quotations from Survey Respondents
| 2a | “Moving away from strict cut point targets makes sense…” |
| 2b | “I am still hearing some valid criticisms of the guidelines so I am not implementing them wholesale.” |
| 2c | “My patients have very low literacy and many do not speak English. An online risk calculator can help the discussion but often it does not.” |
| 2d | “I think online risk calculators that can show graphically risk reduction for behavioral change would be the most useful for getting patients to make a decision that works for them.” |
Implementation of the guidelines
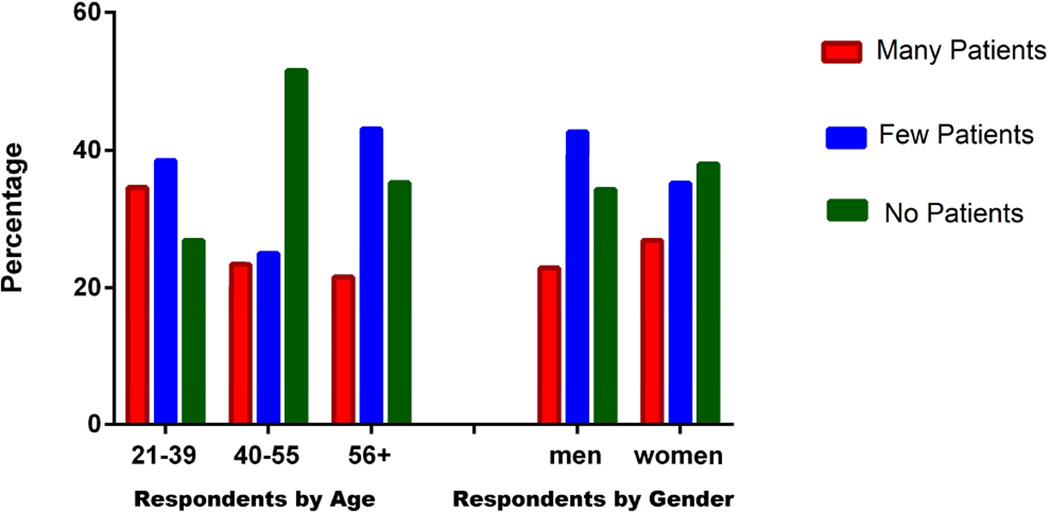
The majority of respondents (63%) reported implementing the new guidelines with at least some of their patients; 46 (25%) reported implementing the guidelines for many patients while 69 (38%) reported implementing the guidelines for a few. Only 68 (37%) reported they had not yet done so with any of their patients. Younger clinicians reported the highest rate of implementation of the new guidelines with many of their adult patients (35%) in comparison to middle aged (23%) and older (22%) respondents. All trends noted by age were not statistically significant. Similarly, there was no observed difference in the rate of implementation by gender [Figure 2].
Figure 2.
Clinicians’ Reported Extent of Implementation of the New 2013 AHA/ACC Guidelines – by age and gender
Of those who had implemented the new guidelines with only some of their patients or none at all (n=133), 62 (47%) planned to implement them in future while 63 (47%) remained unsure. Only 8 (6%) respondents were not planning to implement the new guidelines at all.
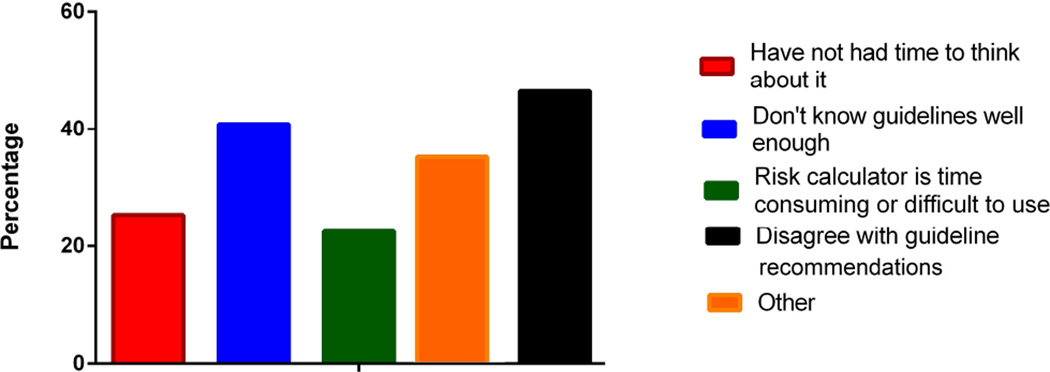
Of those who were not sure or were not planning to implement the new guidelines for many of their adult patients (n=71), 33 (47%) cited disagreeing with the guidelines as at least one of their concerns [Table 2b]. Twenty-nine (41%) noted they did not know the guidelines well enough, while 18 (25%) had not had time to think about the new guidelines. Finally, 23% cited difficulty using the risk calculator as a barrier to implementation [Figure 3]. Free text responses provided by respondents identified concerns related to overtreatment, especially related to the validity of the current risk calculator, lack of applicability to all populations, particularly racial and ethnic minorities, and the controversy surrounding the guidelines [Table 2c]. Others noted that the current risk calculator was too cumbersome to use in clinical practice.
Figure 3.
Cited Reasons by Clinicians Who Have Not Implemented the New ACC/AHA Guidelines for Many of Their Adult Patients
Use of Online Tools for Shared Decision Making
The majority of all respondents (n=129, 71%) thought there was a need for better evidence-based online tools to help engage adult patients in shared decision making regarding cholesterol treatment. Similarly, the majority of clinician respondents reported they would be very likely (n=90, 51%) or somewhat likely (n=59, 33%) to use such a tool regularly for shared decision making if available. These beliefs were similar across all age groups and genders. Many clinicians also emphasized a need for a patient-focused tool with illustrative outcomes for shared decision making and motivational use in their practice [Table 2d].
Discussion
The controversy surrounding the new AHA/ACC cholesterol guidelines has generated much discussion, but little is known about how the guidelines have actually been received in primary care providers’ clinical practice. Limited information derived from cardiologists and primary care clinicians is consistent with the findings of this survey: many clinicians are aware of the new guidelines, but there are multiple barriers to implementation.12–13
Perhaps in part due to the controversy surrounding the guidelines, the overwhelming majority of clinicians in our sample were aware of the new guidelines, across ages and genders. The controversy has not prevented clinicians from adopting at least portions of the guidelines into their practice: only a small minority of clinicians in our sample has not and does not plan to implement and adopt the new guidelines for any of their patients.
However, substantial barriers to adoption remain. The main obstacles cited by respondents who have not implemented the guidelines were unsurprising. One was disagreement with the recommendations of the guidelines – with some citing the public discourse as a hindrance to full implementation. Notably, many clinicians in this survey echoed the public’s concern for statin overtreatment with the current risk calculator, and some questioned its validity. Additional direct and public approaches to addressing these concerns may be needed by AHA/ACC. Further studies addressing whether physicians’ attitudes towards the new guidelines are influenced directly by the source of their information about the guidelines, including whether or not they used the ACC/AHA risk-estimator calculator, would be helpful. Future studies are also needed to assess primary clinicians’ understanding of the new ACC/AHA guidelines recommendations – especially after the robust response to the original criticism aired in both medical and lay media. Some of the respondents also cited perceived lack of applicability to racial and ethnic minorities as a barrier for guideline adoption, an especially pertinent issue given the ethnic diversity of the patient population in Northern California. Lack of familiarity with the guidelines reported by many clinicians suggests that further efforts to educate primary care clinicians about the lipid guidelines, beyond publication in medical journals may be needed. As suggested by some respondents, integration of the risk calculator into electronic medical records, possibly pre-populated from clinical documentation, may also aid adoption of guidelines in a busy primary care practice.
Lastly, shared decision making is an important element in the primary care clinician and patient relationship. Clinicians appear to endorse the idea of an easy-to-use online patient-centered risk calculator or other illustrative tool to help with patient motivation and education, especially in the face of recent reports regarding statin medication disutility and discontinuation.14–17. Notably, given the complexity of the guidelines and perceived limitations of the current risk calculator, many clinicians expressed a strong interest in having patient-centered resources targeting the low-literacy and multilingual audiences especially prevalent in the San Francisco Bay area.
Study Limitations
The participants of this survey were geographically isolated to Northern California and answers were self-reported. Respondents utilized individual definitions for “many” versus “few” patients in our survey questions as these terms were not specifically defined. Additionally, a minority of invited participants completed the survey and only very limited demographic information on survey non-respondents is available. Given that the responses were collected as a convenience sample, results may not be fully generalizable to the San Francisco Bay Area Collaborative Research Network or other populations and should be replicated with larger, population-based samples. Finally, the specific source(s) of information used by our respondents regarding the new AHA/ACC guidelines is not known.
Conclusion
Nearly all survey respondents were aware of the new AHA/ACC guidelines. Even with the surrounding controversy, many have begun implementing the guidelines but a substantial percentage has not yet done so. Barriers may need to be addressed for a more universal adoption. Further assessment of clinicians’ perspective and evolving adoption of the guidelines may help with optimizing the approach to lipid management and ensure integration into current practice.
Supplementary Material
Clinical Significance.
Little is known about opinions of primary care clinicians regarding the 2013 ACC/AHA Guidelines for the Prevention of Primary and Secondary Atherosclerotic Disease.
This survey suggests a majority of primary care clinicians are aware of the new guidelines and many have begun to implement them in their clinical practice.
However, barriers to implementation ranging from disagreement with recommendations to concerns regarding the accompanying risk calculator will need to be addressed.
Acknowledgement
This project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number UL1 TR000004. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest disclosure: None.
References
- 1.Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;11:1524–4539. Risk Calculator: http://tools.cardiosource.org/ASCVD-Risk-Estimator/ [Google Scholar]
- 2.Kavousi M, Leening MJ, Nanchen D, et al. Comparison of Application of the ACC/AHA Guidelines, Adult Treatment Panel III Guidelines, and European Society of Cardiology Guidelines for Cardiovascular Disease Prevention in a European Cohort. JAMA. 2014;311(14):1416–1423. doi: 10.1001/jama.2014.2632. [DOI] [PubMed] [Google Scholar]
- 3.Pencina MJ, Navar-Boggan AM, D’Agostino RB, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370:1422–1431. doi: 10.1056/NEJMoa1315665. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Goff D, Stone NJ. Statins, risk assessment, and the new American prevention guidelines. Lancet. 2014;383(9917):600–602. doi: 10.1016/S0140-6736(13)62348-X. [DOI] [PubMed] [Google Scholar]
- 5.Ioannidis JP. More than a billion people taking statins?: Potential implications of the new cardiovascular guidelines. JAMA. 2014;311:463–464. doi: 10.1001/jama.2013.284657. [DOI] [PubMed] [Google Scholar]
- 6.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2014;382:1762–1765. doi: 10.1016/S0140-6736(13)62388-0. [DOI] [PubMed] [Google Scholar]
- 7.Kolata G. Bumps in the Road to New Cholesterol Guidelines. The New York Times. 2013 Nov 26;:A17. [Google Scholar]
- 8.Kolata G. Risk Calculator for Cholesterol Appears Flawed. The New York Times. 2013 Nov 18;:A1. [Google Scholar]
- 9.Kolata G. New Cholesterol Advice Startles Even Some Doctors. The New York Times. 2013 Nov 13;:A4. [Google Scholar]
- 10.Muntner P, Colantonio LD, Cushman M, et al. Validation of the Atherosclerotic Cardiovascular Disease Pooled Cohort Risk Equations. JAMA. 2014;311:1406–1415. doi: 10.1001/jama.2014.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.San Francisco Bay Area Collaborative Research Network (SF Bay CRN) [Accessed September 4, 2014]; Available at: http://accelerate.ucsf.edu/community/sfbaycrn. [Google Scholar]
- 12.Berry E, Ward T. CV Guidelines, Sex Post-MI, and Barriers to Heart Health: Docs Weigh In. [Accessed September 28, 2014];Medscape. 2014 Mar; Available at: http://www.medscape.com/features/slideshow/heart-health-survey#1. [Google Scholar]
- 13.Silverman Ed. What Doctors are Saying About Those New Cholesterol Meds. [Access September 28, 2014]; Available at: http://blogs.wsj.com/pharmalot/2014/09/02/what-doctors-are-saying-about-those-new-cholesterol-meds. [Google Scholar]
- 14.Lloyd-Jones D, et al. Statins, risk assessment, and the new American prevention guidelines. doi: 10.1016/S0140-6736(13)62348-X. [DOI] [PubMed] [Google Scholar]
- 15.Hensley S. Mixed feelings about side effects from cholesterol pills. [Accessed October 10, 2014]; www.npr.org/blogs/health/2012/08/01/157729714/mixed-picture-on-perceptions-of-cholesterol-pill-side-effects August 2nd, 2012. [Google Scholar]
- 16.Fontana M, Asaria P, Moraldo M, et al. Patient accessible tool for shared decision making in cardiovascular primary prevention: Balancing longevity benefits against medication disutility. Circulation. 2014;129:2539–2546. doi: 10.1161/CIRCULATIONAHA.113.007595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Derose SF, et al. Automated outreach to increase primary adherence to cholesterol lowering medications. JAMA Intern Med. 2013;173:38–43. doi: 10.1001/2013.jamainternmed.717. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.