Abstract
Background
There is limited information on the validity of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) alcohol use disorders (AUD) symptom criteria among adolescents in the general population. The purpose of the present study is to assess the DSM-IV AUD symptom criteria as reported by adolescent and adult drinkers in a single representative sample of the U.S. population ages 12 years and older. This design avoids potential confounding due to differences in survey methodology when comparing adolescents and adults from different surveys.
Methods
A total of 133,231 current drinkers (had at least one drink in the past year) ages 12 years and older were drawn from respondents to the 2002–2005 National Surveys on Drug Use and Health. DSM-IV AUD criteria were assessed by questions related to specific symptoms occurring during the past 12 months. Factor analytic (FA) and item response theory (IRT) models were applied to the 11 AUD symptom criteria to assess the probabilities of symptom item endorsements across different values of the underlying trait.
Results
A one-factor model provided an adequate and parsimonious interpretation for the 11 AUD criteria for the total sample and for each of the gender-age groups. The MIMIC model exhibited significant indication for item bias among some criteria by gender, age, and race/ethnicity. Symptom criteria for “tolerance,” “time spent,” and “hazardous use” had lower item thresholds (i.e., lower severity) and low item discrimination, and they were well separated from the other symptoms, especially in the two younger age groups (12–17 and 18–25). “Larger amounts,” “cut down,” “withdrawal,” and “legal problems” had higher item thresholds but generally lower item discrimination, and they tend to exhibit greater dispersion at higher AUD severity, particularly in the youngest age group (12–17).
Conclusions
Findings from the present study do not provide support for the two separate DSM-IV diagnoses of alcohol abuse and dependence among either adolescents or adults. Variations in criteria severity for both abuse and dependence offer support for a dimensional approach to diagnosis which should be considered in the ongoing development of DSM-V.
Keywords: Adolescents, Adults, DSM-IV Alcohol Use Disorders, Item Response Theory, Symptom Patterns
INTRODUCTION
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for alcohol abuse and dependence serve as the basis for diagnosis in clinical work, prevalence estimation in epidemiology, and much of the etiological research reported in the literature. The alcohol dependence criteria in DSM-IV are based on the concept of the Alcohol Dependence Syndrome (ADS) (Edwards and Gross, 1976), in which dependence was considered to be a combination of physiological and psychological processes leading to increasingly impaired control over alcohol use even in the face of negative consequences. In their paper, Edwards and Gross (1976) introduced a bi-axial notion of alcohol-related problems in which the ADS forms one dimension or axis and alcohol-related consequences forms another dimension or axis. This bi-axial concept influenced the DSM-IV distinction between abuse criteria (mainly social, role functioning, or legal problems, or hazardous use, most commonly driving while intoxicated) and dependence criteria (tolerance, withdrawal, and numerous indicators of impaired control over use).
Previous studies have shown that there is considerable diagnostic overlap between the DSM-IV criteria for abuse and dependence (Langenbucher and Chung, 1995; Langenbucher et al., 1995). Even factor analytic (FA) studies that report a 2-factor model do not yield complete differentiation between abuse and dependence criteria (Grant et al., 2007; Harford and Muthén, 2001; Muthén, 1995). Multiple-factor models consistently yield one large factor and one or two minor factors that are highly correlated with the first factor, confirming that 2-factor models do not replicate the DSM-IV distinction between dependence and abuse criteria. Clinical studies report evidence for both 1- and 2-factor models, but in view of the high correlation between abuse and dependence, many clinicians favor a single factor as more appropriate in treatment samples (Feingold and Rounsaville, 1995; Langenbucher, 2004). More recent applications of item response theory (IRT) indicate that abuse and dependence criteria each tap into both mild and more severe symptom pathology in adults (Kahler et al., 2006; Krueger et al., 2006; Langenbucher et al., 2004; Saha et al., 2006; Saha et al., 2007) as well as in clinical samples of adolescents (Martin et al., 2006).
There have been few studies on the prevalence of DSM-IV alcohol abuse and dependence among adolescents in the general population (Kessler et al., 1994; Kilpatrick et al., 2000). Harford and colleagues (2005) reported the prevalence of DSM-IV alcohol abuse and dependence and associated diagnostic criteria among adolescents and adults ages 12–65 years based on the 2001 National Household Survey on Drug Abuse (NHSDA). In this analysis, among current drinkers, the prevalence of alcohol dependence was highest among respondents ages 18–23 years (males, 8.5 percent; females, 5.2 percent), followed by respondents ages 12–17 years (males, 4.6 percent; females, 4.5 percent). Similar patterns, though higher in prevalence, were present for alcohol abuse. The study noted the high prevalence among these young age groups of the DSM-IV criterion of tolerance (12–17: males, 21.5 percent; females, 20.6 percent; 18–23: males, 31.5 percent; females, 20.0 percent) and time spent getting alcohol or recovering from its effects (12–17: males, 16.5 percent; females, 17.2 percent; 18–23: males, 30.6 percent; females, 20.3 percent), estimates which research has shown may lead to misclassification and overestimation of alcohol dependence in this younger population.
A number of studies (Harford et al., 2005; Kahler and Strong, 2006) indicate variation in symptom prevalence due to wording and interpretation. Studies have noted difficulties in the assessment of tolerance in population surveys, particularly in younger populations (Chung et al., 2001; Martin et al., 2006). Chung and colleagues (2001) have argued that the assessment of tolerance among adolescents and younger adults reflects low to moderate levels of tolerance rather than a pathological process indicative of alcohol dependence. Harford and colleagues (2005) further note that the endorsement of the criterion much time spent obtaining alcohol, drinking, or getting over its effects in adolescents is more reflective of time spent rather than of getting over its effects (5.2 percent versus 0.4 percent among males and 5.2 percent versus 0.8 percent among females) and, therefore, may reflect problems in obtaining alcohol rather than indicating a clinically relevant aspect of alcohol dependence. A further example is found for the criterion drink more/longer; one that yields high prevalence in most studies. In contrast, Harford and colleagues (2005) report lower prevalence for this criterion based on the symptom wording in the NHSDA. This criterion as defined in the NHSDA is based on the subset of respondents who tried to set limits on drinking amounts (see Appendix in this study1), which departs from the usual assessment in the literature. This wording may be more conservative than the typical wording (using alcohol more or longer than intended) used in other studies. As pointed by Chung and Martin (2005), it is problematic to embed the assumption that a limit on use has been set by the individual in assessing drinking more or longer than intended among adolescents. In this respect, it may be preferable to have set limits as a prerequisite for the symptom criterion larger amounts.
There is limited information on the validity of DSM-IV alcohol use disorders (AUDs) symptom criteria during the developmental period spanning ages 12–23 years (Martin and Winters, 1998). One way to examine the validity of the diagnostic criteria for substance use disorders is to investigate the factor structure of the diagnostic criteria. Several studies have investigated the factor structure of AUD symptom criteria in clinical populations and epidemiological samples. All of these studies used samples of adult populations ages 18 years and older. Regardless of whether DSM-III-R or DSM-IV criteria were used, those studies consistently indicated the presence of two correlated but distinct factors (Grant et al., 2007; Harford and Muthén, 2001; Muthén, 1995). By contrast, more recent FA studies with adolescents and adults (Langenbucher et al., 2004; Martin et al., 2006) failed to support the DSM-IV conceptions of abuse and dependence, favoring instead findings derived from IRT analyses of the more parsimonious single-factor model.
The primary objective of the present study is to assess the usefulness and characteristics of the DSM-IV AUD symptom criteria as reported by adolescent and adult drinkers in a single representative sample of the U.S. population ages 12 years and older. This design avoids potential confounding due to differences in survey methodology when comparing adolescents and adults from different surveys. It also allows the examination of the continuity of AUD symptom criteria within a broad developmental framework. A secondary objective is to determine symptom patterns related to gender, age, and race/ethnicity.
METHODS
Study Sample
The data are from the 2002 through 2005 National Surveys on Drug Use and Health. NSDUH is an annual survey conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA) through a contract with RTI International. NSDUH is the largest national epidemiologic survey in the United States containing information on DSM-IV AUD symptoms and diagnostic criteria in both adults and adolescents. In addition, NSDUH oversamples youths and young adults, so that the sample is approximately equally distributed among three major age groups: 12 to 17 years, 18 to 25 years, and 26 years or older. To increase reliability of the estimates in the present study, we combined data from four years of the surveys: 2002 to 2005. Although NSDUH selects a multistage area probability sample each year for each of the 50 states and District of Columbia, the sampling design for 2005 is slightly different from that for 2002–2004. First, the 2005 NSDUH is the first survey in a coordinated five-year sampling design that spans 2005 to 2009, so unlike prior year surveys that have a 50-percent overlap in primary sampling units (PSUs) between successive survey years, there is no such overlap between the 2005 and 2004 NSDUH. Second, the PSUs in 2005 are census tracts as opposed to clusters of census blocks in the 2002–2004 surveys. The 2005 NSDUH also applied Small Area Estimation methodology that divided the states (the first level of stratification) into equally-sized state sampling regions (the second level of stratification). Nonetheless, the sampling designs in 2005 and 2002–2004 are sufficiently similar to allow pooling survey data across these four years. With the help of an incentive payment of $30, NSDUH maintained a fairly high response rate for computer-assisted interviews (CAIs)—79 percent in 2002, 77 percent in 2003 and 2004, and 76 percent in 2005. However, the present study was based on public use data, which did not include all the original respondents due to a subsampling step used in the disclosure protection procedures. The pooled data across the four surveys resulted in a total of 220,816 respondents. Of these, 136,163 were current drinkers (had at least one drink in the past year) ages 12 and over. Excluding 2,932 current drinkers who had missing data for the DSM-IV symptom criteria questions (2.2 percent) yielded a final study sample of 133,231 current drinkers (64,900 males and 68,331 females; 16,526 Hispanics; 94,519 non-Hispanic Whites; 13,475 non-Hispanic Blacks; 1,698 non-Hispanic Natives/Alaskans; 516 non-Hispanic Hawaiian/Pacific Islanders [PIs]; 3,415 Non-Hispanic Asians; and 3,082 non-Hispanic others).
Measures
Among respondents who reported alcohol use in the past year, the DSM-IV criteria for alcohol abuse (4 criteria) and dependence (7 criteria) were assessed by questions related to the occurrence of specific symptoms during the past 12 months. These symptom questions are shown in the appendix and are organized by the DSM-IV criteria for alcohol abuse and dependence based on algorithms provided in the NSDUH public use data documentation (Substance Abuse and Mental Health Services Administration, 2006)
Demographic variables included gender (male, with female as referent), age category (12–17, 18–25, with 26 and older as referent) and race/ethnicity (non-Hispanic Black, Native American/Alaskan Native, Hawaiian/PI, Asian, non-Hispanic more than one race, Hispanic, with non-Hispanic White as referent). We retained the age categories conventionally used in the NSDUH reports in view of the study focus on adolescents and younger adults. While the boundary between ages 25 and 26 are somewhat arbitrary, age-specific symptom distributions in a previous NSDUH survey (Harford et al., 2005) provide some justification for these categories.
Analytic Plan
As a preliminary step before pooling the data, the frequency distributions of the 11 DSM-IV criteria and the prevalence of DSM-IV AUDs were examined separately for each survey year. Factor analytic (FA) models were used to test for the presence of a unidimensional trait of alcohol problem severity underlying the 11 DSM-IV AUD symptom criteria for each year of data. Exploratory factor analysis (EFA) was conducted by gender and age group for each survey year. The EFA results were then used to specify the factor structure in a multiple causes and multiple indicators (MIMIC) model (Joreskog and Sorbom, 1979) generalized to dichotomous outcomes (Muthén, 1979; Muthén, Tam, Muthén, et al., 1993). The MIMIC model used in this study is a special case of structural equation modeling, in which one or more latent variables intervene between a set of observed background variables (covariates) predicting a set of observed response variables (i.e., DSM-IV AUD symptom criteria). The MIMIC model includes three sets of relationships: those between the symptom criteria and the latent factors (the measurement model), those between the latent factors and the covariates (the structural regression equations), and those between the symptom criteria and the covariates (the direct effects). The presence of direct effects implies that there are differences in the measurement parameters of the factor model due to certain background characteristics (e.g., the factor models may differ for different subgroups in the population). Such effects indicate measurement non-invariance. The non-invariance of specific symptom criteria is an indication that individuals with a same level of latent trait respond differentially to the same measurement items if they belong to different subpopulation groups. For example, these groups may have different interpretations regarding the meaning of the symptom criteria or may have reasons not to respond truthfully to symptom criteria. Consequently, measurement non-invariance has the potential to distort the results of what is being measured. In this study, the MIMIC models involve only one latent factor representing the unidimensional trait of alcohol use disorder severity. Without covariates, MIMIC models are equivalent to IRT models, as both of these models can be represented mathematically as factor analytic models. The link between IRT models and confirmatory factor analysis for dichotomous variables has been discussed elsewhere (Glockner-Rist and Hoijtink, 2003; MacIntosh and Hashim, 2003). Similar to factor analysis, IRT modeling establishes the relationship between some latent traits and their manifest indicators. By applying two-parameter logistic IRT models to the 11 AUD symptom criteria, we were able to assess the probabilities of symptom item endorsements across different values of the latent factor and to evaluate the psychometric properties of the symptom criteria. Hays and colleagues (2000) gave a detailed overview of IRT and a discussion of the related methodological issues and practical challenges. Briefly, IRT postulates that a person’s performance on a test item is determined by the underlying trait of that person and by the characteristics of the test item, which includes two key parameters, item threshold and item discrimination. Item threshold is the level at which the underlying trait corresponds to a 50 percent chance of endorsing the item. Higher item thresholds indicate greater severity. Item discrimination (illustrated by slopes) indicates the accuracy of an item in distinguishing individuals with different levels of severity along the underlying trait continuum. These parameters are presented graphically with an item response curve (IRC) for each of the AUD symptom criteria. In addition, item information curves that correspond to these IRCs were summed to produce test information curves (TIC), which are also presented graphically. TICs embody the overall precision of these criteria in assessing a given level of the AUD severity (latent trait).
The analyses were conducted using the statistical modeling program Mplus (Muthén and Muthén, 1998; 2005). The default estimator for the MIMIC models was a robust, weighted, least-squares estimator. Model fit indices included chi-square, comparative fit index (CFI), root mean square residuals (RMSR), and root mean square error approximation (RMSEA). We used the following cutoff values as indicators of good fit: CFI > 0.95; RMSR <0.05; RMSEA < 0.06, as suggested by Muthén and Muthén (2005). Sampling weights and design effects of the NSDUH were taken into account for parameter estimation as well as standard error and model fit calculations.
RESULTS
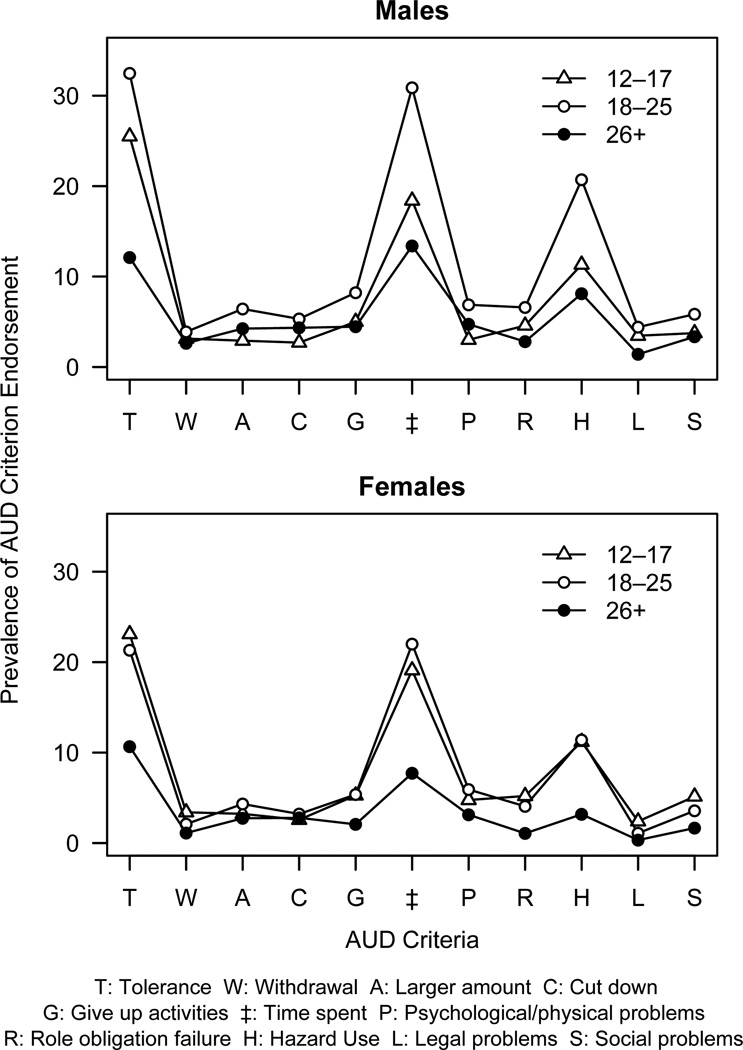
The DSM-IV AUD symptom criteria distributions and AUD prevalence estimates were very similar in each of the four survey years. Taken together, past year prevalence for DSM-IV AUDs among current drinkers is distributed as follows: dependence, 5.15 percent; abuse only, 6.55 percent; no diagnosis, 88.29 percent (among males, 6.37 percent, 8.70 percent, and 84.92 percent, respectively; among females, 3.85 percent, 4.25 percent, and 91.91 percent, respectively). The distributions of DSM-IV AUDs and AUD symptoms among current drinkers by gender and age group are shown in table 1. Within each gender group, the prevalence of alcohol dependence was highest among respondents ages 18–25 years, followed by respondents ages 12–17 years and lowest among respondents ages 26 years and older. Similar patterns were present for alcohol abuse, except among females, the prevalence of alcohol abuse was highest among respondents ages 12–17 years. Approximately 20 percent of adolescents and younger adults were diagnostic orphans (i.e., respondents with 1 or 2 dependence criteria but no DSM-IV AUD diagnosis) with the proportions slightly lower among adults aged 26 years and older. Figure 1 illustrates the distribution of symptom criteria graphically. The prevalence of symptom criteria was notably higher for tolerance, time spent, and hazardous use within each age group. Among female respondents, the prevalence of symptom criteria was similar for ages 12–17 and 18–25 in contrast to that for male respondents.
Table 1.
Prevalence (%) of DSM-IV AUD Symptom Criteria among Current Drinkers by Age Group
| DSM-IV AUD Criteria | Male | Female | ||||
|---|---|---|---|---|---|---|
| Age 12–17 (N=11,651) |
Age 18–25 (N=27,377) |
Age 26+ (N=25,872) |
Age 12–17 (N=12,304) |
Age 18–25 (N=29,331) |
Age 26+ (N=26,696) |
|
| DSM-IV AUD | ||||||
| Dependence | 6.38 (0.31) | 11.05 (0.26)a, g | 5.45 (0.19)a, g | 6.73 (0.30) | 7.26 (0.19)g | 2.96 (0.13)a, g |
| Abuse | 11.58 (0.37) | 17.12 (0.29)a, g | 6.86 (0.20)a, g | 11.02 (0.37) | 9.61 (0.22)a, g | 2.69 (0.12)a, g |
| Diagnostic orphan | 19.76 (0.48) | 24.58 (0.34)a, g | 14.68 (0.29)a, g | 18.59 (0.45) | 20.97 (0.31)a, g | 10.67 (0.26)a, g |
| No symptom | 62.29 (0.58) | 47.26 (0.39)a, g | 73.02 (0.39)a, g | 63.66 (0.60) | 62.16 (0.38)a, g | 83.68 (0.30)a, g |
| DSM-IV Criteria | ||||||
| Tolerance | 25.50 (0.52)g | 32.47 (0.38)a, g | 12.11 (0.28)a, g | 23.10 (0.52)g | 21.32 (0.31)a, g | 7.64 (0.21)a, g |
| Withdrawal | 3.14 (0.21) | 3.89 (0.15)a, g | 2.63 (0.14)a, g | 3.40 (0.21) | 2.10 (0.11)a, g | 1.11 (0.08)a, g |
| Larger amounts | 2.91 (0.20) | 6.42 (0.19)a, g | 4.25 (0.17)a, g | 3.23 (0.20) | 4.32 (0.16)a, g | 2.74 (0.14)a, g |
| Cut down | 2.70 (0.23) | 5.32 (0.18)a, g | 4.34 (0.17)a, g | 2.57 (0.19) | 3.21 (0.13)a, g | 2.79 (0.15)g |
| Give up activities | 5.00 (0.28) | 8.22 (0.23)a, g | 4.46 (0.17)g | 5.26 (0.26) | 5.37 (0.16)g | 2.07 (0.11)a, g |
| Time spent | 18.40 (0.48) | 30.88 (0.38)a, g | 13.39 (0.28)a, g | 19.10 (0.47) | 22.00 (0.33)a, g | 7.72 (0.21)a, g |
| Psychological and physical problems | 3.01 (0.20)g | 6.88 (0.20)a, g | 4.73 (0.17)a, g | 4.76 (0.25)g | 5.92 (0.18)a, g | 3.13 (0.14)a, g |
| Role obligation failure | 4.58 (0.26) | 6.59 (0.20)a, g | 2.81 (0.13)a, g | 5.20 (0.26) | 4.06 (0.15)a, g | 1.07 (0.07)a, g |
| Hazardous use | 11.32 (0.36) | 20.71 (0.31)a, g | 8.11 (0.22)a, g | 11.19 (0.39) | 11.40 (0.24)g | 3.18 (0.13)a, g |
| Legal problems | 3.46 (0.23)g | 4.41 (0.18)a, g | 1.41 (0.09)a, g | 2.40 (0.17)g | 1.09 (0.07)a, g | 0.33 (0.04)a, g |
| Social problems | 3.75 (0.24)g | 5.84 (0.19)a, g | 3.35 (0.14)g | 5.14 (0.28)g | 3.57 (0.14)a, g | 1.66 (0.10)a, g |
Note: Standard error is included in parentheses following each prevalence estimate.
: Age group difference relative to Age 12–17 of the same gender is significant at 0.05 significance level.
: Gender difference is significant at 0.05 significance level.
Figure 1.
Prevalence of DSM-IV AUD Symptom Criteria Among Current Drinkers, by Gender and Age Group.
EFA/MIMIC analysis
The EFA for the total sample yielded one large factor (eigenvalue = 7.25) with eigenvalues dropping below 1.0 for each additional factor (the ratio of first to second eigenvalue was 8.33). The one factor solution was retained for the MIMIC analysis. Summaries of MIMIC models for the total sample and each gender group are shown in table 2. The inclusion of direct effects improved the fit for all models. In the total sample, males had significantly higher estimates for AUD severity than females. When compared to adults ages 26 and older, both adolescents ages 12–17 and younger adults ages 18–25 had significantly higher estimates for AUD severity. Compared with White respondents, all other racial/ethnic groups except Asians had higher estimates for AUD severity. Among males, young adults ages 18–25 had significantly higher estimates for AUD severity, and adolescents did not differ significantly from adults ages 26 and older. Among females, both adolescents and young adults had significantly higher estimates for AUD severity than adults ages 26 and older. In gender-specific models, with the exception of a nonsignificant association for Black, Native Hawaiian/PI, and Hispanic females, the other racial/ethnic comparisons with respect to AUDs were similar to that of the total sample model.
Table 2.
MIMIC Model Estimates for Latent Variable Based on DSM-IV Alcohol Use Disorder Symptom Criteria
| Both Genders | Male | Female | ||||
|---|---|---|---|---|---|---|
| Estimate | S.E. | Estimate | S.E. | Estimate | S.E. | |
| Male gender | 0.25** | .01 | ||||
| Age (referent: 26+) | ||||||
| 12–17 | 0.34** | .02 | 0.02 | .02 | 0.47** | .02 |
| 18–25 | 0.39** | .02 | 0.22** | .02 | 0.42** | .02 |
| Race/ethnicity (referent: Non-Hispanic White) | ||||||
| Non-Hispanic Black | 0.08** | .02 | 0.14** | .03 | −0.02 | .03 |
| Non-Hispanic Native/Alaskan | 0.50** | .04 | 0.44** | .05 | 0.50** | .06 |
| Non-Hispanic Hawaiian/PI | 0.32** | .11 | 0.36* | .15 | 0.12 | .10 |
| Non-Hispanic Asian | −0.16** | .03 | −0.20** | .05 | −0.24** | .05 |
| Non-Hispanic Other | 0.09* | .04 | 0.09 | .07 | 0.13* | .06 |
| Hispanic | 0.14** | .02 | 0.18** | .02 | 0.01 | .02 |
| Direct Effects | ||||||
| Tolerance | ||||||
| Age 12–17 | 0.25** | .02 | 0.48** | .02 | 0.22** | .02 |
| Age 18–25 | 0.25** | .02 | 0.48** | .02 | 0.21** | .02 |
| Non-Hispanic Black | 0.22** | .02 | 0.19** | .02 | 0.29** | .03 |
| Non-Hispanic Asian | NS | NS | 0.25** | .05 | 0.37** | .08 |
| Withdrawal | ||||||
| Age 12–17 | −0.12** | .03 | NS | NS | NS | NS |
| Age 18–25 | −0.23** | .02 | −0.09** | .03 | −0.19** | .03 |
| Non-Hispanic Black | 0.26** | .03 | 0.25** | .04 | 0.28** | .05 |
| Hispanic | 0.23** | .03 | 0.25** | .04 | NS | NS |
| Larger amounts | ||||||
| Age 12–17 | −0.39** | .03 | −0.21** | .04 | −0.40** | .03 |
| Age 18–25 | −0.18* | .02 | NS | NS | −0.21** | .03 |
| Cut down | ||||||
| Age 12–17 | −0.43** | .03 | −0.23** | .04 | −0.46** | .04 |
| Age 18–25 | −0.26** | .02 | −0.09** | .02 | −0.31** | .03 |
| Non-Hispanic Asian | NS | NS | NS | NS | −0.33** | .10 |
| Hispanic | −0.23** | .03 | −0.20** | .04 | −0.22** | .05 |
| Give up activities | ||||||
| Age 18–25 | NS | NS | 0.07** | .02 | NS | NS |
| Hispanic | NS | NS | 0.11** | .03 | NS | NS |
| Time spent | ||||||
| Age 12–17 | NS | NS | 0.17** | .02 | NS | NS |
| Age 18–25 | 0.20** | .02 | 0.36** | .02 | −.20** | .02 |
| Psychological and physical problems | ||||||
| Male | −0.14** | .02 | ||||
| Age 12–17 | −0.39** | .03 | NS | NS | −0.20** | .02 |
| Age 18–25 | −0.21** | .02 | NS | NS | −0.33** | .03 |
| Non-Hispanic Black | −0.10** | .03 | −0.16** | .03 | ||
| Hispanic | −0.22** | .03 | −0.15** | .04 | −0.11* | .03 |
| Role obligation failure | ||||||
| Age 12–17 | NS | NS | NS | NS | 0.17** | .03 |
| Non-Hispanic Asian | NS | NS | 0.26** | .07 | NS | NS |
| Hispanic | NS | NS | 0.13** | .04 | NS | NS |
| Hazardous use | ||||||
| Male | 0.15** | .01 | ||||
| Age 12–17 | NS | NS | 0.16** | .03 | 0.16** | .03 |
| Age 18–25 | 0.21** | .02 | 0.35** | .02 | 0.23** | .02 |
| Non-Hispanic Black | −0.18** | .03 | −0.18** | .03 | −0.20** | .04 |
| Non-Hispanic Asian | NS | NS | −0.22** | .07 | NS | NS |
| Non-Hispanic Other | NS | NS | −0.33** | .08 | NS | NS |
| Hispanic | −0.15** | .02 | −0.14** | .03 | NS | NS |
| Legal problems | ||||||
| Male | 0.24** | .03 | ||||
| Age 12–17 | NS | NS | 0.34** | .04 | 0.25** | .05 |
| Age 18–25 | NS | NS | 0.24** | .03 | 0.35** | .12 |
| Non-Hispanic Black | 0.27** | .04 | 0.28** | .05 | NS | NS |
| Non-Hispanic Native/Alaskan | NS | NS | 0.42** | .09 | NS | NS |
| Hispanic | 0.26** | .04 | 0.29** | .04 | NS | NS |
| Social problems | ||||||
| Age 12–17 | −0.13** | .03 | NS | NS | NS | NS |
| Age 18–25 | −0.16** | .02 | NS | NS | NS | NS |
p < .01;
p < .05;
NS = not significant.
Model fit statistics:
Both genders: Chi square = 1403.99; CFI = .98; RMSEA = .01;
Male: Chi square = 915.19; CFI = .98; RMSEA = .01;
Female: Chi square = 539.04; CFI = .98; RMSEA = .01.
The MIMIC models also yielded many significant direct effects of gender, age, and race/ethnicity on AUD symptom criteria (see table 2). This indicates that not all of the effects of background variables are fully mediated by the latent variable (i.e., AUD severity) and that there is therefore evidence of partial measurement non-invariance. Interpretations of direct effects should be viewed in conjunction with the structural estimates of the factor. For example, in the total sample model, there were three significant direct effects related to gender (continued to drink despite psychological and physical problems [−0.14], hazardous use [0.15], and legal problems [0.24]). The negative direct effect for the criterion, psychological and physical problems among males, implies that for respondents with the same value on this factor (i.e., equally severe with respect to AUD), respondents who are male have a lower probability of reporting this criterion. Factor values being the same, male drinkers have a higher probability for reporting hazardous use and legal problems than female drinkers.
Age showed significant direct effects for both males and females. Among males, there were significant direct effects of age on eight symptom criteria. With the same AUD severity, each of the two younger age groups was more likely than those ages 26 years and older to report tolerance, give up activities (ages 18–25 only), time spent, hazardous use, and legal problems and was less likely to report withdrawal (ages 18–25 only), larger amounts (ages 12–17 only), and cut down. Among females, factor values being the same, each of the two younger age groups was more likely than those ages 26 years and older to report tolerance, role obligation failure (ages 12–17 only), hazardous use, and legal problems and less likely to report withdrawal (ages 18–25 only), larger amounts, cut down, time spent (ages 18–25 only), and continued to drink despite psychological and physical problems.
Race/ethnicity also had significant direct effects for both genders. Compared with their White counterparts with the same AUD severity, Black males were more likely to report tolerance, withdrawal, and legal problems and less likely to report hazardous use, whereas Black females were more likely to report tolerance and withdrawal and less likely to report continued to drink despite psychological/physical problems and hazardous use. Hispanic males were more likely to report withdrawal, give up activities, role obligation failure, and legal problems and less likely to report cut down, continued to drink despite psychological/physical problems, and hazardous use. Hispanic females were less likely to report cut down and continued to drink despite psychological/physical problems. Asian males were more likely to report tolerance and role obligation failure and less likely to report hazardous use. Asian females were more likely to report tolerance and less likely to report cut down. Native/Alaskan males were more likely to report legal problems, and non-Hispanic males with more than one race (i.e., other) were less likely to report hazardous use.
IRT analysis
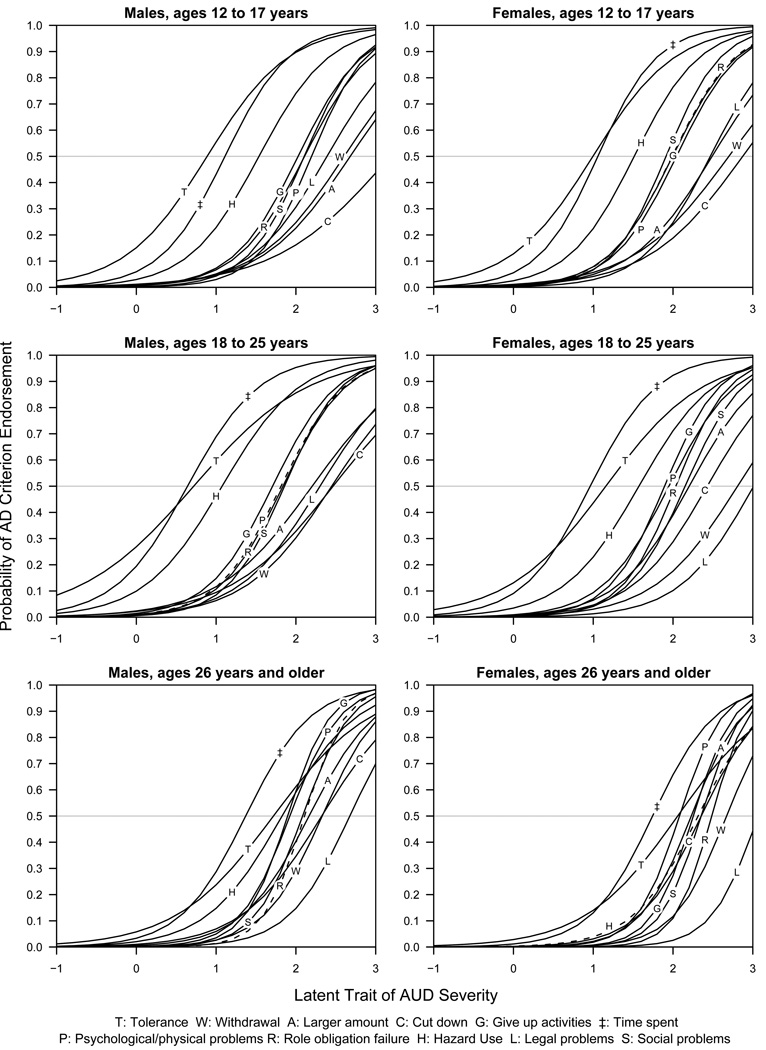
For each gender-age group, item thresholds and item discrimination for the 11 AUD criteria are shown in table 3 and the IRCs are shown in figure 2. Among males in each age group, tolerance, time spent, and hazardous use have relatively lower thresholds, and withdrawal, larger amounts, cut down, and legal problems have relatively higher thresholds. In contrast to the 26 and older age group, which was most likely to endorse time spent and least likely to endorse legal problems, the 12–17 age group was most likely to endorse tolerance and least likely to endorse cut down. The overall IRCs are more spread out in the 12–17 and 18–25 age groups compared to the 26 and older age group. The symptom criteria for tolerance, time spent, and hazardous use tap into the lower end of AUD severity in the 12–17 and 18–25 age groups, and their IRCs are well separated from the rest. In contrast, the symptom criteria give up activities, role obligation, psychological/physical problems, and social problems tend to have their IRCs intertwined with one another in the middle range of the AUD severity. These four symptom criteria have relatively high item discrimination across all age groups, especially among the 26 and older age group.
Table 3.
Item Discrimination and Item Threshold for DSM-IV Alcohol Use Disorder (AUD) Symptom Criteria by Gender and Age Group
| DSM-IV AUD Criteria | Male | Female | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age 12–17 (N=11,651) |
Age 18–25 (N=27,377) |
Age 26+ (N=25,872) |
Age 12–17 (N=12,304) |
Age 18–25 (N=29,331) |
Age 26+ (N=26,696) |
|||||||
| Item Discrim.a |
Item Threshold |
Item Discrim. |
Item Threshold |
Item Discrim. |
Item Threshold |
Item Discrim. |
Item Threshold |
Item Discrim. |
Item Threshold |
Item Discrim. |
Item Threshold |
|
| Tolerance | 1.14 | 0.88 | 0.82 | 0.72 | 0.95 | 1.72 | 1.13 | 0.99 | 0.96 | 1.16 | 0.99 | 2.07 |
| Withdrawal | 1.08 | 2.61 | 1.09 | 2.45 | 1.60 | 2.33 | 0.97 | 2.70 | 1.12 | 2.81 | 1.78 | 2.67 |
| Larger amounts | 1.06 | 2.68 | 0.99 | 2.21 | 1.39 | 2.16 | 1.17 | 2.49 | 1.30 | 2.21 | 1.88 | 2.21 |
| Cut down | 0.82 | 3.19 | 0.91 | 2.47 | 1.15 | 2.32 | 0.98 | 2.88 | 1.24 | 2.43 | 1.53 | 2.34 |
| Give up activities | 1.45 | 2.03 | 1.46 | 1.71 | 2.18 | 1.90 | 1.45 | 1.99 | 1.70 | 1.89 | 2.23 | 2.26 |
| Time spent | 1.46 | 1.11 | 1.30 | 0.64 | 1.44 | 1.37 | 1.57 | 1.06 | 1.41 | 0.96 | 1.48 | 1.75 |
| Psychological and physical problems | 1.71 | 2.20 | 1.48 | 1.81 | 1.85 | 1.93 | 1.48 | 2.04 | 1.41 | 1.95 | 2.16 | 2.08 |
| Role obligation failure | 1.40 | 2.11 | 1.49 | 1.84 | 2.26 | 2.11 | 1.48 | 1.99 | 1.74 | 2.04 | 2.52 | 2.49 |
| Hazardous use | 1.33 | 1.54 | 1.21 | 1.07 | 1.25 | 1.83 | 1.42 | 1.51 | 1.24 | 1.57 | 1.42 | 2.33 |
| Legal problems | 1.23 | 2.39 | 1.16 | 2.30 | 1.53 | 2.68 | 1.40 | 2.47 | 1.27 | 3.01 | 2.02 | 3.06 |
| Social problems | 1.65 | 2.11 | 1.63 | 1.86 | 1.97 | 2.08 | 1.70 | 1.91 | 1.61 | 2.15 | 2.27 | 2.35 |
Discrim.=Discrimination.
Note: Item response curves are illustrated in Figure 2.
Figure 2.
Item Response Curves for DSM-IV AUD Symptom Criteria, by Gender and Age Group
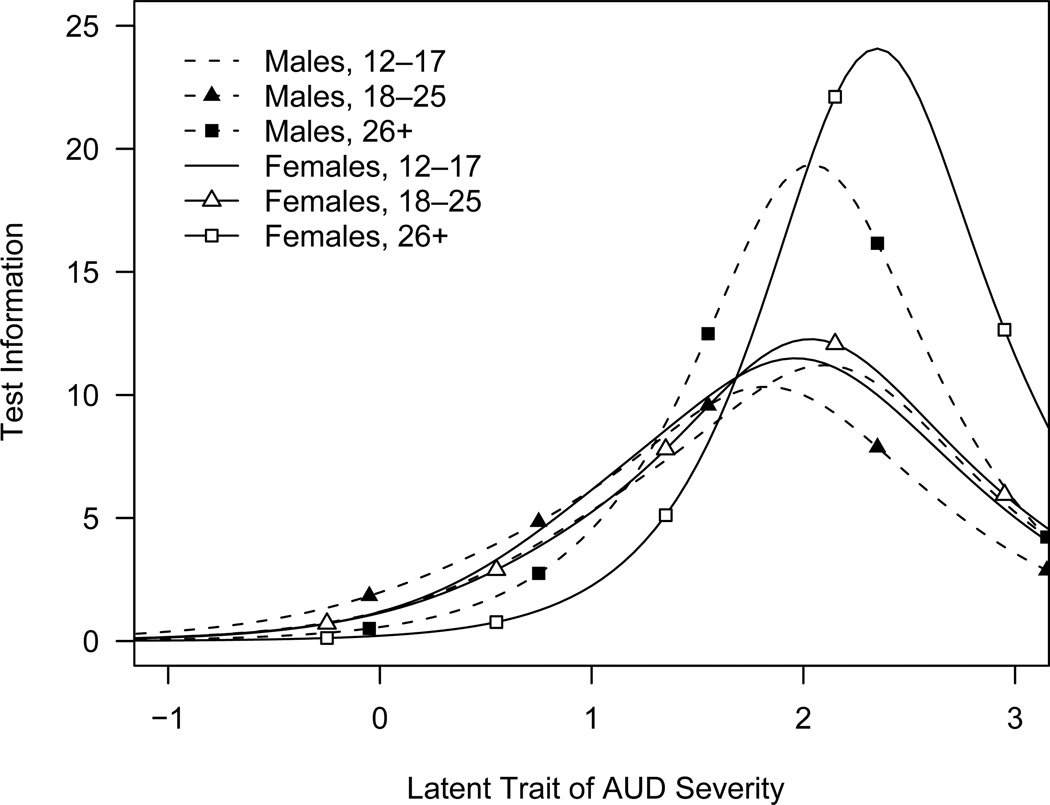
Similarly, among females in each age group, tolerance and time spent have relatively lower item thresholds, and withdrawal, larger amounts, cut down, and legal problems have relatively higher item thresholds. Among 18–25 and 26 and older age groups, the most severe symptom criterion as defined by the item threshold is legal problems; however, it would take higher AUD severity for the 12–17 age group to endorse cut down than to endorse legal problems. The least severe symptom criterion as defined by item threshold is time spent for 18–25 and 26 and older age groups; however, drinkers with very low severity in the 12–17 age group are more likely to endorse tolerance than time spent. Although both tolerance and time spent are the two least severe criteria, time spent has much better discrimination than tolerance, especially among adolescents and young adults. This applies to females as well as to males. As with males, the IRCs are less varied for females ages 26 years and older than the younger age groups. The IRCs for females in this age group are so close together that the IRC of tolerance cuts across those of other symptom criteria, and hazardous use is akin to cut down and larger amount in terms of its psychometric properties. Tolerance has extraordinarily low discrimination relative to other symptom criteria for females ages 26 years and older, although it is generally low across all gender and age groups. As with males, symptom criteria including give up activities, role obligation, psychological/physical problems, and social problems are ranked at the top for their high discrimination, which is good at distinguishing the majority of the drinkers in the middle range of AUD severity. However, because their psychometric properties are very similar, the IRCs intertwine with one another, suggesting redundancy in their functions as diagnostic criteria. For all gender-age groups, the TIC, as shown in figure 3, has a marked peak indicating high measurement precision only within a narrow range of the underlying trait, with lower measurement precision at lower and higher levels of severity. The dispersion, however, is relatively wider in the two younger age groups than the 26 and older age groups for both genders.
Figure 3.
Test Information Curves for DSM-IV AUD Symptom Criteria, by Gender and Age Group
DISCUSSION
The major objective of the present paper was to evaluate the diagnostic utility and characteristics of DSM-IV AUD criteria for assessing severity of AUD disorder by analyzing data from a national sample of adolescents and adult current drinkers pooled over four survey years (2002, 2003, 2004, and 2005). To our knowledge, this is the first study that has examined a large nationally representative sample of adolescents and adults within a comparable measurement model. The comparability of the distributions of DSM-IV AUD diagnoses and symptom criteria across the four survey years provides strong evidence of reliability of these national estimates. Consistent with a previous analysis of the 2001 National Household Survey on Drug Abuse (Harford et al., 2005), the most prevalent AUD criteria included tolerance; time spent obtaining alcohol, drinking, or getting over its effects; and hazardous use. These items were consistently higher in prevalence in each gender by age group, whereas the prevalence of the remaining eight symptom criteria was lower. This disparity in prevalence may introduce bias into DSM-IV AUD assessment and indicate problems with the measurement of these criteria as well as with the criteria themselves. The higher prevalence of these symptoms in younger drinkers (Table 1) may, in part, be due to variations in symptom interpretation by individuals of different ages and may result in over-estimation of diagnosis for younger age groups.
A one-factor model provided an adequate and parsimonious interpretation for the 11 AUD criteria for the total sample and each of the gender-age groups. Findings from the structural equation model indicated that the probability of AUD increased with male gender, younger age, and several racial/ethnic groups. Compared to adults ages 26 years and older, both younger groups (12–17 and 18–25) had significantly higher estimates of AUD. When compared with non-Hispanic Whites, AUD estimates were higher for each racial/ethnic group with the exception of Asian-Americans, who had lower estimates for AUD. Overall, gender-specific models yielded comparable results with a few exceptions. Among males, the AUD estimates among respondents ages 12–17 did not differ from those ages 26 and older. Among females, the AUD estimates for Blacks, Hawaiians/PIs, and Hispanics did not differ from non-Hispanic Whites.
The methodology used in this study differs from conventional risk factor analysis in which a dichotomous diagnostic variable is regressed on a set of covariates or hypothesized antecedents. Instead, a continuous latent variable (AUD) defined by a set of symptom criteria is regressed on the covariates. Despite these methodological differences, the associations between the demographic variables and AUD found in this study are consistent with those from other general population studies (Caetano and Clark, 1998; Dawson, 1998; Grant et al., 2004) and analyses of more recent national surveys using structural equation modeling (Grant et al., 2007; Harford and Muthén, 2001).
One of the strengths of the structural equation modeling approach used here is the ability to detect and compensate for non-invariance of the measurement of criteria across subgroups of individuals in the population, thereby adjusting for distortion of the risk factor assessment. In addition to the demographic effects on the overall AUD factor, there were significant direct effects of gender, age, and race/ethnicity on individual AUD symptom criteria. The positive direct effects for tolerance, time spent, and hazardous use among the younger (12–17 and 18–25) compared to the older age group is consistent with the potential item bias reported in other studies (Langenbucher et al., 2004; Martin et al., 2006; Saha et al., 2006). In addition, the positive direct effects for legal problems among both younger age gender groups may result from perceived sanctions for hazardous behaviors, particularly traffic citations. The negative direct effects related to withdrawal, larger amounts, cut down, and continued drinking despite psychological/physical problems among younger compared to older current drinkers may be related to greater AUD severity. Overall, although the incorporation of direct effects in the model improved model fit somewhat, it did not appreciably change the associations between gender and race/ethnicity, and the AUD factor. Saha and colleagues (2006) also note that despite some variation in symptom/criterion expression, there was little or no differential scale functioning among these groups.
Fewer studies have examined symptom patterns in racial/ethnic groups. The present study found that among Blacks, compared to non-Hispanic Whites, both genders were more likely to report tolerance, withdrawal, and legal problems and less likely to report hazardous use, whereas females were less likely to report continued to drink despite psychological/physical problems. Among Hispanics, compared to non-Hispanic Whites, both genders were less likely to report cut down and continued to drink despite psychological/physical problems, whereas males were more likely to report withdrawal, give up activities, role obligation failure, and legal problems. Two previous studies examined symptom criterion bias in racial/ethnic groups (Grant et al., 2007; Saha et al., 2006), but both were limited to adults 18 years and older. Grant and colleagues (2007) used comparable statistical models and found positive direct effects related to attempts to cut down drinking and negative direct effects for withdrawal symptoms among both Blacks and Hispanics. Inclusion of adolescents and variation in symptom wording in the present study, however, complicate comparisons across studies.
The IRT analysis indicated that the thresholds for the 11 symptom criteria do not align with the DSM-IV conceptualization of AUD, a finding consistent with other FA (Harford and Muthén, 2001) and IRT analyses (Langenbucher et al., 2004; Martin et al., 2006; Saha et al., 2006). Dependence criteria for tolerance and time spent had low item thresholds and discrimination, whereas abuse criteria for legal problems and role obligation failure had higher thresholds and discrimination. Tolerance, time spent, and hazardous use (males only) had lower item thresholds (i.e., higher endorsement) and low item discrimination. They tapped lower levels of AUD severity in the IRCs and were well separated from the other symptoms, especially in the two younger age groups. As reported in the MIMIC analysis, these items also exhibited significant item bias among the younger age groups when compared with adults ages 26 and older.
The IRCs for symptom criteria such as give up activities, continued drinking despite psychological/physical problems, role obligation failure, and social problems have similar shapes that cluster in the middle range of the AUD severity and have relatively higher item thresholds and high item discrimination, especially in the 26 and older age group.
For both gender groups, symptom criteria for larger amounts, cut down, withdrawal, and legal problems have higher item thresholds but generally lower item discrimination and tend to exhibit greater dispersion at higher AUD severity (as measured by the latent factor representing the unidimensional trait of alcohol use disorder), particularly in the youngest age group (12–17). The high threshold and poor discrimination exhibited by some symptom criteria is consistent with the literature, which indicates that adolescents with high levels of alcohol problem severity do not always report attempts to set limits or cut down drinking, whereas some adolescents with low levels of alcohol problem severity do (Chung and Martin, 2002; Harford et al., 2005; Martin et al., 2006). The legal problem criterion has been shown to perform poorly in other IRT analyses (Langenbucher et al., 2004; Martin et al., 2006; Saha et al., 2006). The present findings related to this criterion may be a function of the large samples available for analysis.
To our knowledge, the only other IRT analysis of adolescent drinking is provided in an analysis of 472 clinical adolescents (Martin et al., 2006). Consistent with our study, Martin and colleagues found that the DSM-IV symptom criteria for AUD perform better in the moderate range of severity but are less accurate at mild and more severe ranges, and do not support the DSM-IV abuse–dependence distinction. Although the symptom criteria for tolerance, give up activities, cut down, withdrawal, and legal problems had similar characteristics with respect to item threshold and discrimination, there were considerable differences among the other six symptom criteria. These differences might be a function of illness severity among treatment populations compared with the general population. A recent IRT analysis of DSM-IV symptom criteria in a sample of 22,526 current drinkers age 18 and older from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) provides a better comparison for the present analysis (Saha et al., 2006). In contrast to the present study, the test information function in the NESARC analysis peaked at more severe AUD levels and did not tap the less severe range of AUD. This overall pattern is consistent with present findings for the age 26 and older group but less so for the 18–25 age group.
A number of study limitations should be noted. Despite the large representative samples, estimates are based on self-report and lack the more detailed assessments of symptoms and diagnoses in clinical studies. Among younger samples, particularly adolescents, many individuals have not reached critical ages for dependence symptoms. Numerous other factors that could influence symptom reports were beyond the scope of this study (e.g., differences in comorbid conditions, age at drinking onset, family structure or family intactness, history of alcoholism). Despite the application of standardized DSM-IV criteria for alcohol use disorders, care must be taken when making comparisons with other studies. Aside from differences in sample selection, variations in measurement of the criteria and in the functioning of symptom items may contribute to observed differences with other studies.
In summary, findings from the present study are consistent with the current literature in: their lack of support for the DSM-IV distinctions between abuse and dependence; the presence of a single dimension underlying these criteria; and the fact that the criteria are aligned along a continuum of problem severity. Both MIMIC and IRT analyses indicate that current assessments of tolerance, time spent, and hazard use introduce potential bias in the assessment of AUD, resulting in over-diagnosis for each of the age groups in this study, but particularly among adolescents. As noted earlier, the inclusion of direct effects in the MIMIC model had only a modest effect on model fit and did not appreciably change associations between the demographic factors and AUD. Future studies need to address specific effects of variations in symptom wording on criterion prevalence for age, gender, and race/ethnicity as well as distinctions between developmentally normative changes and pathological symptoms related to tolerance and time spent. As indicated by other investigators (Langenbucher et al., 2004; Martin et al., 2006; Saha et al., 2006), future research should continue to examine the dimensional properties of these symptom criteria to inform future DSM diagnostic conceptualizations. Applications of newer hybrid models (Muthén, 2006), which include both categorical and dimensional representations and external validating criteria, can provide clearer boundary estimates for proposed DSM-V diagnosis and more precise prevalence estimates for AUD among adolescents and adults.
Supplementary Material
Acknowledgments
This study was conducted for the Alcohol Epidemiologic Data System (AEDS) under Contract No. N0AA32007 for the Division of Epidemiology and Prevention Research, National Institute on Alcohol Abuse and Alcoholism.
Footnotes
The NHSDA was renamed to the National Survey on Drug Use and Health (NSDUH) in 2002, which is the data source used in the current study.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Caetano R, Clark CL. Trends in alcohol-related problems among Whites, Blacks, and Hispanics: 1984–1995. Alcohol Clin Exp Res. 1998;22:534–538. [PubMed] [Google Scholar]
- Chung T, Martin CS. Concurrent and discriminate validity of DSM-IV symptoms of impaired control over alcohol consumption in adolescents. Alcohol Clin Exp Res. 2002;26:485–492. [PubMed] [Google Scholar]
- Chung T, Martin CS. What were they thinking? Adolescents' interpretations of DSM-IV alcohol dependence symptom queries and implications for diagnostic validity. Drug Alcohol Depend. 2005;80(2):191–200. doi: 10.1016/j.drugalcdep.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS, Winters KC, Langenbucher JW. Assessment of alcohol tolerance in adolescents. J Stud Alcohol. 2001;62:687–695. doi: 10.15288/jsa.2001.62.687. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS, Armstrong TD, Labouvie EW. Prevalence of DSM-IV alcohol diagnoses and symptoms in adolescent community and clinical samples. J Am Acad Child Adolesc Psychiatry. 2002;41:546–554. doi: 10.1097/00004583-200205000-00012. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS, Winters KC. Diagnosis, course, and assessment of alcohol abuse and dependence in adolescents. Recent Dev Alcohol. 2005;17:5–27. doi: 10.1007/0-306-48626-1_1. [DOI] [PubMed] [Google Scholar]
- Dawson DA. Beyond black, white and Hispanic: Race, ethnic origin and drinking patterns in the United States. J Substance Abuse. 1998;10(4):321–339. doi: 10.1016/s0899-3289(99)00009-7. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross M. Alcohol dependence: provisional description of a clinical syndrome. Br Med Journal. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A, Rounsaville B. Construct validity of the abuse-dependence distinction as measured by DSM-IV criteria for different psychoactive drugs. Drug Alcohol Depend. 1995;39:99–109. doi: 10.1016/0376-8716(95)01142-l. [DOI] [PubMed] [Google Scholar]
- Glockner-Rist A, Hoijtink H. The Best of Both Worlds: Factor Analysis of Dichotomous Data Using Item Response Theory and Structural Equation Modeling. Structural Equation Modeling: A Multidisciplinary Journal. 2003;10(4):544–565. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Muthén BO, Yi H-y, Hasin DS, Stinson FS. DSM-IV alcohol dependence and abuse: further evidence of validity in a general population. Drug Alcohol Depend. 2007;86(2–3):154–166. doi: 10.1016/j.drugalcdep.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Harford TC, Muthén BO. The dimensionality of alcohol abuse and dependence: a multivariate analysis of DSM-IV symptom items in the National Longitudinal Survey of Youth. J Stud Alcohol. 2001;62:150–157. doi: 10.15288/jsa.2001.62.150. [DOI] [PubMed] [Google Scholar]
- Harford TC, Grant BF, Yi H-y, Chen CM. Patterns of DSM-IV alcohol abuse and dependence criteria among adolescents and adults: results from the 2001 National Household Survey on Drug Abuse. Alcohol Clin Exp Res. 2005;20(5):810–828. doi: 10.1097/01.alc.0000164381.67723.76. [DOI] [PubMed] [Google Scholar]
- Hays RD, Morales LS, Reise SP. Item response theory and health outcomes measurement in the 21st century. Med Care. 2000;38(9 Suppl):II28–II42. doi: 10.1097/00005650-200009002-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joreskog KG, Sorbom D. Advances in Factor Analysis and Structural Equation Models. Cambridge, MA: Abt Books; 1979. [Google Scholar]
- Kahler CW, Strong DR. A Rash model analysis of DSM-IV alcohol abuse and dependence items in the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res. 2006;30(7):1165–1175. doi: 10.1111/j.1530-0277.2006.00140.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnicj HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: data from a national sample. J Consult Clin Psychol. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Nichol PE, Hicks BM, Markon KE, Patrick CJ, Iacono WG, McGue M. Using latent trait modeling to conceptualize an alcohol problems continuum. Psychol Assess. 2004;16(2):107–119. doi: 10.1037/1040-3590.16.2.107. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Chung T. Onset and staging of DSM-IV alcohol dependence using mean age and survival-hazard methods. J Abnorm Psychol. 1995;104:346–354. doi: 10.1037//0021-843x.104.2.346. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Morgenstern J, Miller J. DSM-III, DSM-IV and ICD-10 as severity scales for drug dependence. Alcohol Drug Depend. 1995;39:139–150. doi: 10.1016/0376-8716(95)01152-o. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Labouvie E, Martin C, Sanjuan PM, Bavly L, Kirisci L, Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. J Abnorm Psychol. 2004;113(1):72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- MacIntosh R, Hashim S. Variance Estimation for Converting MIMIC Model Parameters to IRT Parameters in DIF Analysis. Applied Psychological Measurement. 2003;27(5):372–379. [Google Scholar]
- Martin CS, Winters KC. Diagnosis and assessment of alcohol use disorders among adolescents. Alcohol Health Res World. 1998;22:95–105. [PMC free article] [PubMed] [Google Scholar]
- Martin CS, Kaczynski NA, Maisto SA, Bukstein OM, Moss HB. Patterns of DSM-IV alcohol abuse and dependence symptoms in adolescent drinkers. J Stud Alcohol. 1995;56:672–680. doi: 10.15288/jsa.1995.56.672. [DOI] [PubMed] [Google Scholar]
- Martin CS, Chung T, Kirisci L, Langenbucher JW. Item response theory analysis of diagnostic criteria for alcohol and cannabis use disorders in adolescents: implications for DSM-V. J Abnorm Psychol. 2006;115(4):807–814. doi: 10.1037/0021-843X.115.4.807. [DOI] [PubMed] [Google Scholar]
- Muthén BO. A structural model with latent variables. J. Am. Stat. Assn. 1979;74:807–811. [Google Scholar]
- Muthén B, Tam T, Muthén L, et al. Latent variable modeling in the LISCOMP framework: Measurement of attitudes toward career choice. In: Krebs D, Schmidt P, editors. New Direction in Attitude Measurement: Festschrift for Karl Schuessler. New York, NY: W. de Gruyter; 1993. pp. 277–290. [Google Scholar]
- Muthén BO. Factor analysis of alcohol abuse and dependence symptom items in the 1988 National Health Interview survey. Addiction. 1995;90:637–645. doi: 10.1046/j.1360-0443.1995.9056375.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. 4th ed. Los Angeles, CA: Muthén and Muthén; 1998–2005. [Google Scholar]
- Muthén BO. Should substance disorder be considered as categorical or dimensional? Addiction. 2006;101(Suppl 1):6–16. doi: 10.1111/j.1360-0443.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- Saha TD, Chou PS, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classification of alcohol use disorders. Alcohol Drug Depend. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey On Drug Use and Health, 2005. Research Triangle Park, NC: Research Triangle Institute [producer]; Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2006. [2006-11-16]. U.S. Dept. of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies. [Computer file]. ICPSR04596-v1. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.