Abstract
Objective
To assess the accuracy of anterior tooth movement using clear aligners in integrated three-dimensional digital models.
Methods
Cone-beam computed tomography was performed before and after treatment with clear aligners in 32 patients. Plaster casts were laser-scanned for virtual setup and aligner fabrication. Differences in predicted and achieved root and crown positions of anterior teeth were compared on superimposed maxillofacial digital images and virtual models and analyzed by Student's t-test.
Results
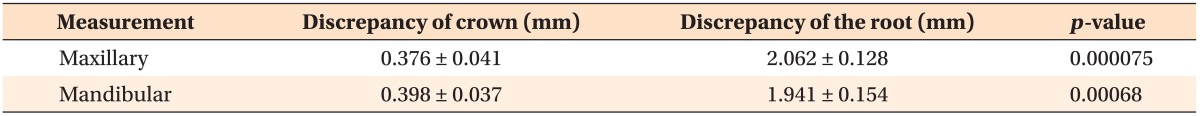
The mean discrepancies in maxillary and mandibular crown positions were 0.376 ± 0.041 mm and 0.398 ± 0.037 mm, respectively. Maxillary and mandibular root positions differed by 2.062 ± 0.128 mm and 1.941 ± 0.154 mm, respectively.
Conclusions
Crowns but not roots of anterior teeth can be moved to designated positions using clear aligners, because these appliances cause tooth movement by tilting motion.
Keywords: Clear aligners, Registration, Cone-beam computed tomography
INTRODUCTION
Clear aligners are widely used in clinical practice. They are considered suitable for complete orthodontic treatment of nonextraction or simple cases.1,2 However, whether they can replace fixed appliances is controversial.1,2,3,4 The ability of fixed appliances to apply root torque is the key to successful treatment,5 while the ability of clear aligners to move roots to designated positions has not been confirmed.
Clear aligners are usually fabricated by scanning plaster casts for virtual setup. The conventional virtual setup displays moving crowns but not roots and the jaws. On the other hand, three-dimensional (3D) digital models with roots6 enable observation of root positions in the jaws, ensuring root parallelism and avoiding fenestration and dehiscence. This study aimed to assess the accuracy of tooth movement using clear aligners in integrated 3D digital models.
MATERIALS AND METHODS
Thirty-two patients (28 men and four women; mean age, 26.7 years; range, 13-44 years) undergoing treatment with clear aligners at the Department of Orthodontics, Capital Medical University School of Stomatology were selected for the study. The duration of treatment was from July 2010 to November 2013. The inclusion criteria were as follows: complete permanent dentition, without lesions or dental prostheses, no requirement for extraction, and completion of treatment using clear aligners alone; less than 2 mm of strip in the whole arch and less than 0.25 mm of strip in a single teeth; Angle Class I malocclusion or no requirement to change the posterior relationship, no requirement for arch expansion or molar distalization, and use of a rectangular attachment for teeth requiring root-controlling torque. The exclusion criteria were as follows: unclear cone-beam computed tomography (CBCT) images of teeth with the jaws, unwillingness of the patient to undergo CBCT, presence of systemic disease, overjet of more than 5 mm or Class III overbite, change in the external morphology of teeth during treatment, and incomplete treatment using clear aligners or a switch to other treatment methods. This study was conducted in accordance with the amended Declaration of Helsinki and was approved by the Ethics Committee of Capital Medical University School of Stomatology. Written informed consent was obtained from all participants.
CBCT imaging, laser scanning, and integrated 3D registration
CBCT scans were acquired using a NewTom VGi scanner (QR s.r.l., Verona, Italy) with the following operating and reconstruction parameters: 110 kV; 1.2 mA; volume, 15 cm × 15 cm; scanning time, 3.6 s; axial slice thickness, 0.25 mm; and radiation (dose-area product), 33 µy/m2. The participants assumed a natural head position, and a wax occlusal splint was used to avoid interference of the opposing cusps in the CBCT images CBCT data were exported in DICOM format and converted to stereolithographic format using Mimics 10.0 software (Materialise, Leuven, Belgium). The 3D models were segmented by thresholding and separately reconstructed using the CBCT data.4,5
A two-phase polyvinyl siloxane impression of each arch was recorded and poured with dental plaster. The casts were scanned at a resolution of 0.02 mm using a 3D Shaderlight scanner (Breuckmann GmbH, Meersburg, Germany) and the resulting images were outputted in stereolithographic format.4,5
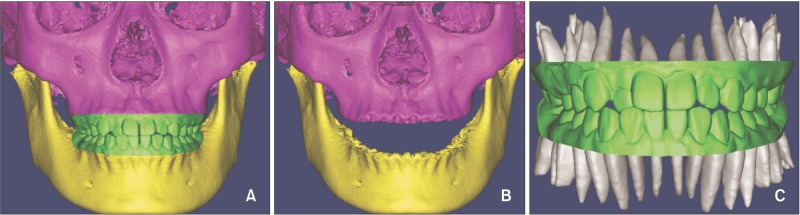
The CBCT and laser-scanned images were inputted into Rapidform 2006 software (Rapidform, Inc., Sunnyvale, CA, USA). After initial registration, surface characteristic-based automated registration of the CBCT and laser-scanned models was performed using the buccal and lingual sides of the jaws as areas of optimal overlap. The overlapping portion of the CBCT-imaged crowns was removed using Magics 9.51 software (Materialise). Each final digital model included accurate crown positions determined by laser scanning and root and jaw positions derived by CBCT imaging (Figure 1). Integrated models were inputted into OrthoDS 4.6 software (EA, Inc., Shanghai, China) for virtual setup according to Andrews' six keys to normal occlusion, without dehiscence, fenestration, and root unparallelism.
Figure 1. Construction of the integrated three-dimensional digital model. A, The integrated model; B, images of the maxilla and mandible; C, images of the complete dentition.
Virtual setup and treatment
Each tooth in the virtual setup was separated to enable individual movement using OrthoDS 4.6 software. The resulting 3D setup enabled simultaneous representation of the jaws, teeth, and occlusion, so that both bone mass and root parallelism could be ascertained. According to the extent of tooth movement in the setup, the virtual treatment was divided into 10-30 steps. Finally, the digitized roots and jaws in each virtual treatment step were removed, retaining only the crowns. Acrylic models were constructed by laser rapid prototyping technology. Clear aligners (EA, Inc.) were finally fabricated on the acrylic models by an air-compressed pressing machine with an 0.8-mm laminated sheet (Biolog Inc., Hayward, CA, USA).
Before insertion, an attachment was adhered according to the first correctional appliance. The patient wore the appliances for more than 20 h a day. The appliance was replaced every 2 weeks until the end of treatment, during which stripping was performed according to the specifications. After the treatment was completed, CBCT images were obtained as already described.
Statistical analysis
Changes in crown and root positions of anterior teeth (canine to canine) and jaw positions were compared on pretreatment and post-treatment CBCT images. Tooth positions predicted by the virtual setup and actual positions determined from the post-treatment CBCT images were also compared. Mean discrepancies (all 3D distances of the overlapping points) in predicted and achieved positions of anterior crowns and roots were analyzed using Student t-test (PASW Statistics software ver. 17.0; IBM Co., Armonk, NY, USA).
RESULTS
Changes in jaw, crown, and root positions
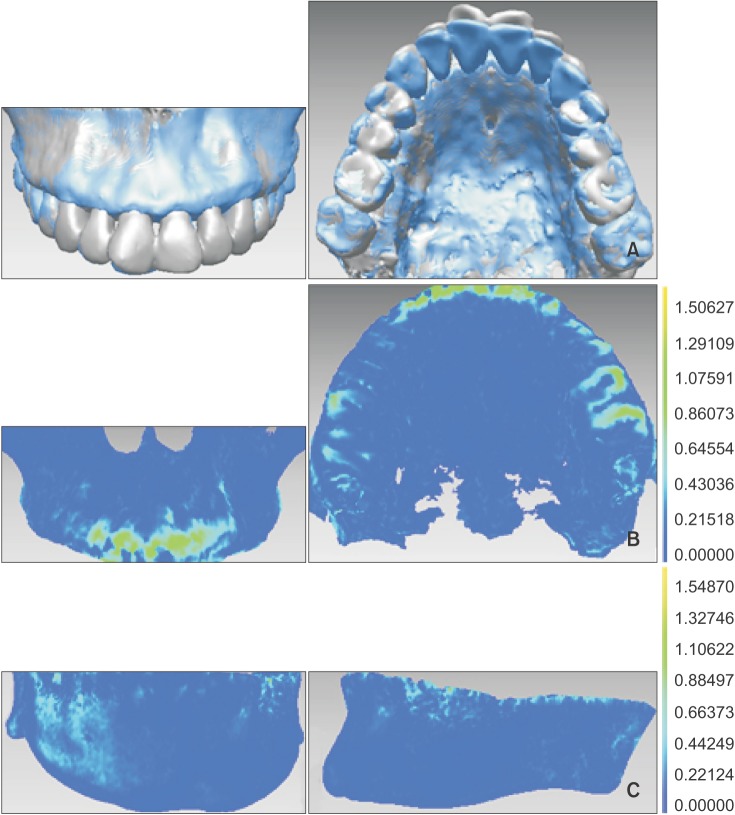
The mean change was 0.226 ± 0.032 mm in the maxilla and 0.211 ± 0.026 mm in the mandible (Figure 2B and 2C). The mean differences in the positions of the maxillary and mandibular crowns were 2.526 ± 0.415 and 2.478 ± 0.372 mm, respectively (Figure 2A). Therefore, the average tooth movement was approximately 2.5 mm. The mean change in the maxillary root positions was 0.418 ± 0.059 mm and that of the mandibular root positions was 0.375 ± 0.066 mm. The amount of movement in the apical region was minimum (Figure 3).
Figure 2. Pretreatment and post-treatment registration of the jaws. A, Maxillary registration. B, Mandibular registration. Blue indicates post-treatment and silver indicates pretreatment. C, Detection map after registration. Dark blue is visible (registration accuracy ≤ 0.15 mm).
Figure 3. Cone-beam computed tomography-based registration of crown and root positions. A, Comparison of pretreatment (yellow) and post-treatment (pink) root positions. A small amount of movement is visible in the apical part while the coronal part appears to have moved to a great extent. B, Detection map after registration. The crown and most of the apical part appear dark blue (registration accuracy ≤ 0.15 mm), while the anterior crown is red.
Discrepancies in predicted and achieved crown and root positions
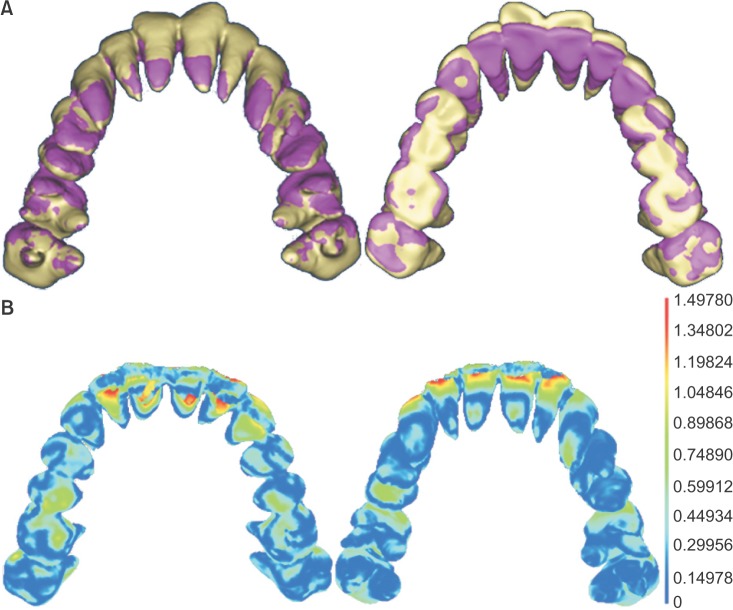
The mean discrepancy in the maxillary crown positions was 0.376 ± 0.041 mm, while that of the mandibular anterior teeth was 0.398 ± 0.037 mm (Table 1); only a small difference between the predicted and the achieved crown positions was observed (Figure 4).
Table 1. Discrepancies in predicted and achieved crown and root positions.
Values are presented as mean±standard deviation.
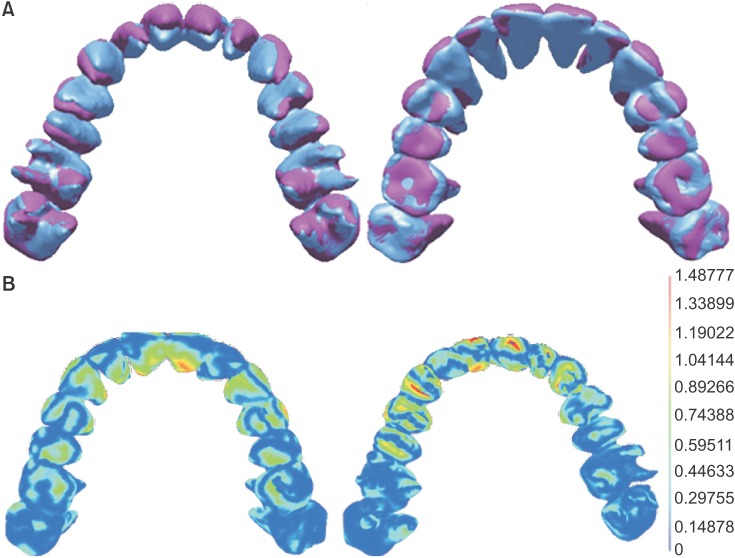
Figure 4. Discrepancies in crown and root positions after treatment with clear aligners. A, Comparison of achieved (blue) and predicted (pink) crown and root positions. Only the crown reached the predicted position. B, Detection map after registration. The immovable and moved parts of molar teeth appear dark blue (registration accuracy ≤ 0.15 mm), while the crown appears red.
The mean discrepancy in the predicted and achieved maxillary root positions was 2.062 ± 0.128 mm and that of the mandibular root positions was 1.941 ± 0.154 mm (Table 1). The difference was maximum in the apical portion of the tooth (Figure 4). Student's t-test based on equality of variances showed that the discrepancy in root position was significantly greater than that in crown position (Table 1).
DISCUSSION
Clear aligners alone can complete orthodontic treatment in many patients, but some studies have shown that 20-80% of the patients require subsequent fixed appliance therapy.7,8 The incidence of relapse is higher with clear aligners than with fixed appliances.9 Considering these disadvantages, the effectiveness of clear aligners should be reassessed.
Kravitz et al.2 showed that the accuracy of overall tooth movement with clear aligners is 41% but that of maxillary incisor intrusion is only 18.3%; however, the accuracy can exceed 70% in 25% of the cases. Nguyen and Chen10 reported that the mean accuracy of anterior intrusion can be as high as 79%. In the current study, the overall movement error was approximately 0.4 mm when the average tooth movement was 2.5 mm.
Many studies have compared virtual and actual crown positions by designing virtual clear aligners, but differences in root position have not been reported. Kim et al.11 superimposed separate OrthoCAD-scanned crowns over CBCT skeletal data. Macchi et al.12 integrated entire laser-scanned models with computed tomography (CT) images. Kim et al.13 fused CT and digital surface data of a plaster cast by sequential point- and surface-based markerless registration: they noted mean errors of 0.12 ± 0.14 mm in the maxillary superimposed models and 0.13 ± 0.11 mm in the mandibular ones. In the present study, 3D digital models with roots constructed by superimposing CBCT-based digital maxillofacial models and digitized plaster casts were used to design clear aligners. The mean errors of such integrated models were found to be 0.159 ± 0.0265 mm in the maxilla and 0.151 ± 0.0337 mm in the mandible.6,14 Therefore, integrated 3D models adequately represent the positional relationships of roots and jaws in the virtual setup.
Untreated teeth, palatal rugae, and dental implants should be selected as overlapping points if pretreatment and post-treatment plaster casts are referenced to calculate errors.2,15 In the current study, the buccal and lingual sides of the jaws were used as benchmarks, with a relatively large overlap, because they are unaffected by tooth surface and occlusal changes during treatment. Given that patients with almost complete growth and development were included, the buccal and lingual jaw anatomy showed little change (registration accuracies of 0.226 ± 0.032 mm for the maxilla and 0.211 ± 0.026 mm for the mandible). Alveolar convexities with larger changes after treatment were eliminated. The registration accuracies of the other parts of the jaws were all under 0.15 mm (Figure 1).
This study showed a relatively large amount of crown movement (~2.5 mm) but a relatively small amount of root movement (~0.4 mm). These results indicate that clear aligners cannot achieve bodily movement, explaining the poorer treatment quality and easier relapse than with fixed appliance therapy. The clear aligners mostly moved the teeth by tilting motion; fixed appliances were subsequently required because relapse was more likely after treatment with clear aligners.
The material properties of clear aligners are probably responsible for their inability to apply torque. Given that the gingival margin of an aligner is elastic, it would clearly have difficulty in controlling forces applied in this region.16,17,18 Castroflorio et al.5 used Power Ridges (Align Technology, Amsterdam, The Netherlands) at the gingival margin of clear aligners to resist twisting movement of roots caused by anti-reaction torque and showed that clear aligners can accurately control root torque according to the crown position in the virtual setup. However, only crown movement was measured in that study.
This study showed that clear aligners mostly moved anterior teeth by tilting motion, increasing stress at the cervical and apical regions. Recent studies have shown that the resorption rate in the apical portion is 54% with clear aligners, which is slightly higher than that with fixed appliances.19 Root resorption after orthodontic treatment is related to excessive concentration of apical stress, and is reportedly caused by anterior root movement within cortical bone.20 Apajalahti and Petola21 reported that apical root resorption of 3 mm is nearly equivalent to 1 mm of marginal bone loss. Therefore, a virtual setup that involves roots is necessary to prevent apical root resorption and periodontal disease.
This study has three limitations. First, no posterior teeth were registered because these teeth were not designed to move or demonstrated only a small amount of movement in the majority of the patients. Moreover, the biomechanical characteristics of molars are very different from those of anterior teeth. Second, only successful cases were included in the statistical analysis, and patients switching from fixed appliances to clear aligners were excluded. Third, Power Ridges were not included in the cervical region of the clear aligners. Further research considering these variables is required.
CONCLUSION
Crowns but not roots can be moved to designated positions using clear aligners, primarily because such appliances cause tooth movement by tilting motion.
ACKNOWLEDGEMENTS
This study was supported by Beijing Science and Technology Committee grants no z121107001012022 and Beijing Natural Science Foundation (grants no 4112023. Experimental Research on Computer-aided Design/Computer-aided Manufacture (CAD/CAM) Individualized Lingual Brackets System).
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Kassas W, Al-Jewair T, Preston CB, Tabbaa S. Assessment of Invisalign treatment outcomes using the ABO Model Grading System. J World Fed Orthod. 2013;2:e61–e64. [Google Scholar]
- 2.Kravitz ND, Kusnoto B, BeGole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;135:27–35. doi: 10.1016/j.ajodo.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 3.Lund H, Gröndahl K, Hansen K, Gröndahl HG. Apical root resorption during orthodontic treatment. A prospective study using cone beam CT. Angle Orthod. 2012;82:480–487. doi: 10.2319/061311-390.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krieger E, Seiferth J, Marinello I, Jung BA, Wriedt S, Jacobs C, et al. Invisalign® treatment in the anterior region: were the predicted tooth movements achieved? J Orofac Orthop. 2012;73:365–376. doi: 10.1007/s00056-012-0097-9. [DOI] [PubMed] [Google Scholar]
- 5.Castroflorio T, Garino F, Lazzaro A, Debernardi C. Upper-incisor root control with Invisalign appliances. J Clin Orthod. 2013;47:346–351. [PubMed] [Google Scholar]
- 6.Guo H, Zhou J, Bai Y, Li S. A three-dimensional setup model with dental roots. J Clin Orthod. 2011;45:209–216. [PubMed] [Google Scholar]
- 7.Chisari JR, McGorray SP, Nair M, Wheeler TT. Variables affecting orthodontic tooth movement with clear aligners. Am J Orthod Dentofacial Orthop. 2014;145(4 Suppl):S82–S91. doi: 10.1016/j.ajodo.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 8.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015;85:881–889. doi: 10.2319/061614-436.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Djeu G, Shelton C, Maganzini A. Outcome assessment of Invisalign and traditional orthodontic treatment compared with the American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2005;128:292–298. doi: 10.1016/j.ajodo.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen CV, Chen J. Chapter 14. In: Tuncay OC, editor. The invisalign system. London, UK: Quintessence Publishing Company, Ltd.; 2006. pp. 12–32. [Google Scholar]
- 11.Kim DS, Choi SC, Lee SS, Heo MS, Huh KH, Hwang SJ, et al. Principal direction of inertia for 3D trajectories from patient-specific TMJ movement. Comput Biol Med. 2013;43:169–175. doi: 10.1016/j.compbiomed.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Macchi A, Carrafiello G, Cacciafesta V, Norcini A. Three-dimensional digital modeling and setup. Am J Orthod Dentofacial Orthop. 2006;129:605–610. doi: 10.1016/j.ajodo.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Kim BC, Lee CE, Park W, Kang SH, Zhengguo P, Yi CK, et al. Integration accuracy of digital dental models and 3-dimensional computerized tomography images by sequential point- and surface-based markerless registration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:370–378. doi: 10.1016/j.tripleo.2010.03.036. [DOI] [PubMed] [Google Scholar]
- 14.Ye N, Jian F, Xue J, Wang S, Liao L, Huang W, et al. Accuracy of in-vitro tooth volumetric measurements from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2012;142:879–887. doi: 10.1016/j.ajodo.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Miller RJ, Kuo E, Choi W. Validation of Align Technology's Treat III digital model superimposition tool and its case application. Orthod Craniofac Res. 2003;6(Suppl 1):143–149. doi: 10.1034/j.1600-0544.2003.247.x. [DOI] [PubMed] [Google Scholar]
- 16.Hahn W, Zapf A, Dathe H, Fialka-Fricke J, Fricke-Zech S, Gruber R, et al. Torquing an upper central incisor with aligners--acting forces and biomechanical principles. Eur J Orthod. 2010;32:607–613. doi: 10.1093/ejo/cjq007. [DOI] [PubMed] [Google Scholar]
- 17.Brezniak N. The clear plastic appliance: a biomechanical point of view. Angle Orthod. 2008;78:381–382. doi: 10.2319/0003-3219(2008)078[0381:TCPA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Baldwin DK, King G, Ramsay DS, Huang G, Bollen AM. Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: premolar extraction patients. Am J Orthod Dentofacial Orthop. 2008;133:837–845. doi: 10.1016/j.ajodo.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 19.Krieger E, Drechsler T, Schmidtmann I, Jacobs C, Haag S, Wehrbein H. Apical root resorption during orthodontic treatment with aligners? A retrospective radiometric study. Head Face Med. 2013;9:21. doi: 10.1186/1746-160X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 21.Apajalahti S, Peltola JS. Apical root resorption after orthodontic treatment -- a retrospective study. Eur J Orthod. 2007;29:408–412. doi: 10.1093/ejo/cjm016. [DOI] [PubMed] [Google Scholar]