Abstract
Background
Patients with uncontrolled type 1 diabetes mellitus may be candidates for pancreatic islet cell transplantation. This report synthesizes qualitative research on how patients with uncontrolled type 1 diabetes perceive their quality of life.
Objective
The objective of this analysis was to examine the perceptions of patients with uncontrolled type 1 diabetes on how it affects their lived experience and quality of life.
Data Sources
This report synthesizes 31 primary qualitative studies to examine quality of life from the perspectives of adult patients with type 1 diabetes mellitus and their families or partners.
Review Methods
We performed a qualitative meta-synthesis to integrate findings across primary research studies.
Results
Long- and short-term negative consequences of uncontrolled type 1 diabetes affect all aspects of patients’ lives: physical, emotional, practical, and social. The effect on each domain is far-reaching, and effects interact across domains. Uncontrolled blood sugar levels lead to substantial psychological distress, negative moods, cognitive difficulties, irritable or aggressive behaviour, and closely associated problems with relationships, self-image, and confidence. Emotional distress is pervasive and under-addressed by health care providers. Patients live in fear of complications from diabetes over the long term. In the shorter term, they are anxious about the personal, social, and professional consequences of hypoglycemic episodes (e.g., injury, humiliation), and may curtail normal activities such as driving or socializing because they are worried about having an episode. The quality of life for patients’ family members is also negatively impacted by uncontrolled type 1 diabetes.
Conclusions
Uncontrolled type 1 diabetes has significant negative impacts on the quality of life of both people with the disease and their families.
PLAIN LANGUAGE SUMMARY
Type 1 diabetes is a chronic condition that starts early in life. People with type 1 diabetes cannot use sugar from food to produce energy without taking insulin, a hormone that helps them process the sugar. Type 1 diabetes has no cure, but many people can manage it with careful diet, exercise, and medication routines.
Some people cannot successfully manage their diabetes through typical techniques. As a result, the level of sugar in their blood can change quickly, sometimes being too low (hypoglycemia) and sometimes being too high (hyperglycemia). If blood sugar is too high for a long time, people with type 1 diabetes can develop a variety of medical conditions and may be at risk of losing their sight or the use of limbs, among other conditions. If blood sugar dips too low, people with type 1 diabetes can lose consciousness or become confused and disoriented. They may feel ill, act aggressively, or not be able to function normally.
People who do not succeed in controlling their blood sugar through medication, diet, and exercise may experience all of these complications of diabetes, and these negatively affect their quality of life. People with uncontrolled diabetes may experience physical impacts on their mood, mental abilities, and health. They may face emotional impacts, feeling irritable or angry when they have low blood sugar; and frustrated, hopeless, and vulnerable because they are not able to control their blood sugar. They may also experience social impacts, having to turn down invitations to social events or feeling different from friends and family members. Uncontrolled diabetes may also mean that people are not able to work at certain types of jobs or to consistently perform to the best of their abilities. Practically, efforts to control diabetes includes sticking to a very strict schedule of testing their blood sugar, taking medication, and eating and exercising, which can also limit their ability to participate in work and social activities. They may rely on family and friends to help them, and this can negatively affect the lives of those people.
Uncontrolled diabetes negatively impacts all aspects of a person's quality of life.
BACKGROUND
Objective of Analysis
The objective of this analysis was to examine how the experience of uncontrolled diabetes impacts the quality of life of people with type 1 diabetes.
Clinical Need and Target Population
Diabetes mellitus is an incurable condition characterized by high blood glucose levels. It currently affects more than 3 million people in Canada. (1) Type 1 diabetes mellitus is a result of autoimmune destruction of the pancreatic beta (β) cells, causing severe insulin deficiency. Type 1 diabetes affects about 10% of patients with diabetes (2); daily intensive management of blood glucose levels, along with a balanced diet and physical activity, is essential for reducing the short- and long-term complications of the disease.
Patients with type 1 diabetes require lifelong insulin therapy to control their blood glucose levels. Insulin can be administered one of two ways:
Via a needle and syringe or an insulin pen that injects insulin under the skin
Through an insulin pump that connects a reservoir of insulin to a catheter inserted under the skin of the abdomen
However, despite optimal insulin treatment, some patients still experience frequent large and unpredictable fluctuations in their blood glucose levels. This rare form of severe diabetes is known as brittle (or labile) diabetes, and it affects about 3 in 1,000 people with type 1 diabetes. (3) Patients experience recurring episodes of hyperglycemia and hypoglycemia, hypoglycemic unawareness (the state when blood glucose levels decrease to dangerously low levels without any warning symptoms), and diabetic ketoacidosis (a potentially life-threatening complication that results in toxic high levels of ketones in the blood). For these patients, the unstable blood glucose levels lower quality of life, potentially lead to recurrent or prolonged hospitalization, and result in more complications that may reduce their life expectancy. (3)
Although improvements have been made in the quality of diabetes care and insulin-delivery systems, they still fail to provide an effective treatment for some patients with type 1 diabetes. As such, efforts to preserve and restore endogenous pancreatic function through β-cell replacement therapy offer an alternative treatment option for these patients.
EVIDENCE-BASED ANALYSIS
Research Question
How does the experience of uncontrolled diabetes impact the quality of life of people with type 1 diabetes?
Methods
Literature Search
We maintain a reference library of qualitative research pertaining to diabetes mellitus. The library was created using a diabetes-specific search strategy in OVID MEDLINE, EBSCO Cumulative Index to Nursing and Allied Health Literature (CINAHL), and ISI Web of Science Social Sciences Citation Index (SSCI), and includes studies published from January 1, 2005, to October 30, 2014. To supplement the current report, we conducted on January 6, 2015, an additional literature search specifically for uncontrolled type 1 diabetes, using the same databases. To identify qualitative research, we developed a qualitative hybrid filter by combining existing published qualitative filters. (4–6) The filters were compared, and redundant search terms were deleted. We added exclusionary terms to the search filter that would be likely to identify quantitative research and reduce the number of false-positives. We applied the qualitative hybrid filter to the diabetes-specific search strategies. Two authors reviewed titles and abstracts to determine eligibility. We obtained full-text articles when a review of titles and abstracts failed to yield enough information to determine eligibility.
Details of the literature search strategy are presented in Appendix 1.
Inclusion Criteria
English-language full reports
Studies published online between January 1, 2005, and January 6, 2015
Primary qualitative empirical research (using any descriptive or interpretive qualitative methodology, including the qualitative component of mixed-methods studies) and secondary syntheses of primary qualitative empirical research
Studies involving adult patients (≥ 18 years of age) with type 1 diabetes mellitus; articles involving participants with types 1 and 2 diabetes were included, as were articles that did not specify a particular type of diabetes
Research conducted in Canada, the United States, Europe, Australia, and New Zealand (i.e., comparable to the Ontario context)
Published research work (no theses)
Studies addressing the experience of uncontrolled diabetes from the patients’ perspective
Exclusion Criteria
Studies addressing topics other than uncontrolled diabetes
Studies that did not include patients with type 1 diabetes
Studies labelled “qualitative” but that did not use a qualitative descriptive or interpretive methodology (e.g., case studies, experiments, or observational analyses using qualitative categorical variables)
Quantitative research (i.e., research using statistical hypothesis testing, using primarily quantitative data or analyses, or expressing results in quantitative or statistical terms)
Studies that did not pose an empirical research objective or question, or involve primary or secondary analysis of empirical data
Qualitative Analysis
We analyzed published qualitative research using techniques of integrative qualitative meta-synthesis, (7–9) also known as qualitative research integration. Qualitative meta-synthesis summarizes research over a number of studies with the intent of combining findings from multiple articles. The objective of qualitative meta-synthesis is twofold: first, the aggregate of a result reflects the range of findings while retaining the original meaning; second, by comparing and contrasting findings across studies, a new integrative interpretation is produced. (10)
A predefined topic and research question about the impact of uncontrolled type 1 diabetes on patient quality of life guided the research collection, data extraction, and analysis. Topics were defined in stages as relevant literature was identified, and corresponding evidence-based analyses proceeded. First, all qualitative research relevant to the condition under analysis was retrieved. Next, a specific research question regarding the impact of uncontrolled type 1 diabetes on patient quality of life was chosen, and a final search was performed to retrieve articles relevant to this question. The current analysis includes articles that addressed the issue of how uncontrolled type 1 diabetes impacts a patient's life.
Data extraction focused on, and was limited to, findings that were relevant to this research topic. Qualitative findings are the “data-driven and integrated discoveries, judgments, and/or pronouncements researchers offer about the phenomena, events, or cases under investigation.” (8) In addition to the researchers’ findings, original data excerpts (participant quotes, stories, or incidents) were also extracted to illustrate or communicate specific findings.
Using a staged coding process similar to that of grounded theory, (11, 12) findings were broken into their component parts (key themes, categories, concepts) and then regrouped across studies and related to each other thematically. This allowed for organization and reflection on the full range of interpretative insights across the body of research. (8, 13) These categorical groupings provided the foundation from which interpretations were synthesized of the social and personal phenomena relevant to quality of life with uncontrolled type 1 diabetes. We used a “constant comparative” and iterative approach, in which preliminary categories were repeatedly compared with the research findings, raw data excerpts, and co-investigators’ interpretations of the studies.
Quality of Evidence
For valid epistemological reasons, the field of qualitative research lacks consensus on the importance of (and methods/standards for) critical appraisal of research quality. (14) Qualitative health researchers conventionally under-report procedural details, and the quality of findings tends to rest more on the conceptual prowess of the researchers than on methodological processes. (9, 14) Theoretically sophisticated findings are promoted as a marker of study quality because they make valuable theoretical contributions to social science academic disciplines. (15) However, theoretical sophistication is not necessary to contribute potentially valuable information to a synthesis of multiple studies, or to inform questions posed by the interdisciplinary and interprofessional field of health technology assessment. Qualitative meta-synthesis researchers typically do not exclude qualitative research on the basis of independently appraised “quality.” This approach is common to multiple types of interpretive 7, 8, 10, 15–19)
For this review, we presumed the academic peer review and publication processes eliminated scientifically unsound studies, according to current standards. Beyond this, we included all topically relevant, accessible, and published research using any qualitative interpretive or descriptive methodology. We appraised the value of the research findings solely in terms of their relevance to the research question and the presence of data that supported the authors’ findings.
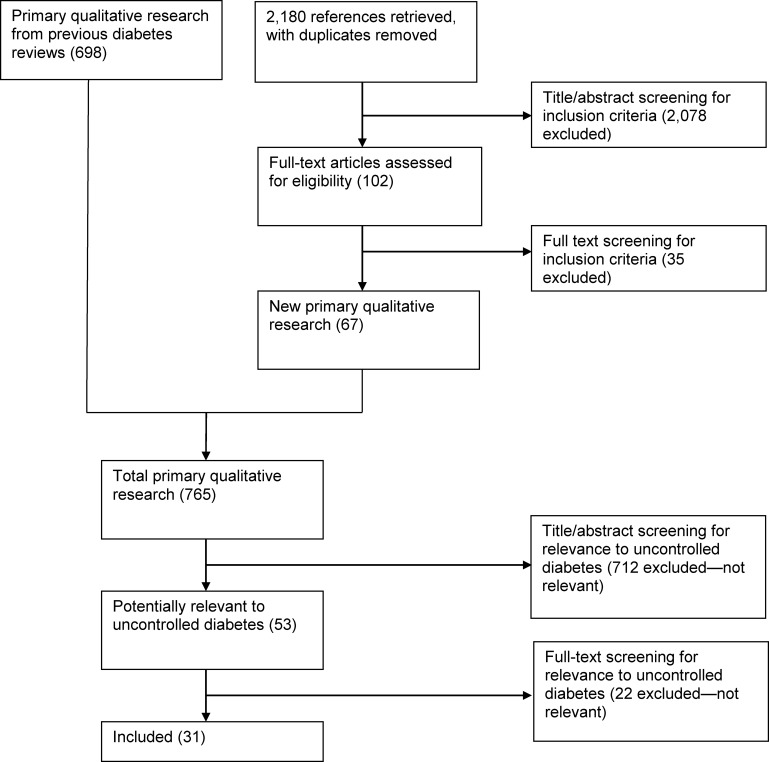
Results of Literature Search
The bibliographic database search yielded 2,180 citations published between January 1, 2005, and January 6, 2015 (with duplicates removed). Articles were excluded based on information in the title and abstract; two reviewers reviewed all titles and abstracts to confine the database to primary qualitative research articles eligible according to the criteria listed in the previous section. These articles were combined with an existing library of 698 primary qualitative research studies on diabetes. The whole library was sorted by two reviewers to identify qualitative research relevant to the quality of life with uncontrolled type 1 diabetes. Figure 1 shows the breakdown of when and for what reason citations were excluded from the analysis.
Figure 1: Citation Flow Chart.
Source: Adapted from Moher et al. (20)
Thirty-one studies met the inclusion criteria. Most studies were conducted in Europe (n = 21) or the United States (n = 7); none were conducted in Canada. Methodologies varied, with a significant number of studies using unspecified methods beyond a generic description of thematic analysis (n = 11). The 31 included studies incorporated data from 865 participants: 752 patients, 103 caregivers, and 10 clinicians.
For each included study (n = 31), the study design, location, and the type and number of participants were identified. This information is summarized below in Tables 1, 2, and 3, respectively.
Table 1:
Body of Evidence Examined According to Study Design
| Study Design | No. of Eligible Studies |
|---|---|
| Content analysis | 5 |
| Grounded theory/constant comparative analysis | 7 |
| Other (framework analysis, hermeneutic approach) | 4 |
| Phenomenology | 4 |
| Qualitative (otherwise unspecified)/thematic analysis | 11 |
| Total | 31 |
Table 2:
Body of Evidence Examined According to Study Location
| Study Location | No. of Eligible Studies |
|---|---|
| Australia/New Zealand | 3 |
| Canada (not Ontario) | 0 |
| Europe | 21 |
| Ontario | 0 |
| United States | 7 |
| Total | 31 |
Table 3:
Body of Evidence Examined According to Type and Number of Participants
| Type of Participant | No. of Participants |
|---|---|
| Patient | 752 |
| Caregiver or family member | 103 |
| Clinicians | 10 |
| Total | 865 |
Results of Evidence-Based Analysis
Uncontrolled type 1 diabetes—both immediate hypoglycemic episodes and longer-term hyperglycemia complications—adversely affects all domains of a patient's life: physical, emotional, practical, and social. The effects of uncontrolled type 1 diabetes on each domain of a person's life are interconnected. After describing how uncontrolled type 1 diabetes may affect each domain, we provide an example of a hypoglycemic episode to demonstrate the holistic nature of the negative effects of uncontrolled diabetes on a patient's quality of life, as well as on the quality of life of the patient's significant others.
Physical Domain
Patients in most studies described that the physical or biological effects of uncontrolled diabetes negatively impacted their quality of life. (21–39) This included general feelings of illness when blood sugar levels were uncontrolled, (26) difficulty maintaining weight at the desired level, (21, 26, 29, 34, 36–38) sexual dysfunction, (29, 37, 38) and fluctuating mood and impaired cognitive function when sugar levels ran high or low. (21, 23–25, 27, 28, 32, 33, 37, 39) Participants attributed the impact of uncontrolled blood sugar on mood to the biological effect of high or low blood sugar (21, 25, 28, 33, 37) as well as to the psychological frustration of poor control. (21, 32) Typically, participants described irritable and aggressive behaviour, (21, 25, 28, 33, 37) which sometimes left family members feeling unsafe and vulnerable to attack from the person with type 1 diabetes. (25, 28) Patients expressed that the cognitive dysfunction associated with impending or actual hypoglycemia or ketoacidosis was dangerous, distressing, and humiliating. (23, 24, 27, 28, 37, 39) They described experiencing panic, disorientation, confusion, decreased consciousness, and loss of control when blood sugars ran too high or low. (23, 24, 27, 28, 37, 39)
Negative impacts on quality of life caused by the biological effects of diabetes were particularly acute for women who were pregnant, breast-feeding, or considering pregnancy. (21, 26, 30, 31, 35, 37) Women with uncontrolled diabetes worried about miscarrying or having large babies; they were also concerned that their children might inherit type 1 diabetes. (21, 26, 30, 31) Pregnant women reported that pregnancy-associated nausea and vomiting disrupted diet management, and that maintaining stable blood sugar levels through labour and delivery was particularly challenging. (21, 26, 30, 31) After giving birth, the transition to motherhood was described as difficult because of the new caloric demands of breast-feeding. Also, there was a lack of time for diabetes self-management routines, as well as hormonal changes. (30, 31, 35, 37)
Emotional Domain
Living with uncontrolled diabetes had many negative effects on the emotional lives of both patients and their families. Nearly all studies mentioned this theme.(21, 22, 24–48) Despite the significant impact on emotions, patients reported that their distress was rarely addressed by health care practitioners. (21)
One of the most common emotions experienced was fear or anxiety. Many patients described living in fear of the long-term complications of diabetes, which inspired anxiety even in patients who had not experienced these effects. While many patients mentioned a general fear of “complications,” (21, 25, 26, 30, 33, 37, 41, 46) specific conditions that patients were afraid of included amputation, (21, 37, 41) death, (21, 33, 38, 41) blindness, (21, 30, 37, 38, 41, 43) necrobiosis, (21) organ failure, (37) and erectile dysfunction. (29, 38) However, more prevalent than fear of long-term complications was the fear of hypoglycemic episodes. (22, 25, 27–31, 33–37, 41, 43–48) Patients expressed anticipatory fear of hypoglycemia, due to the physical effects during and after an episode, the potential for social or professional humiliation, and the possibility of dangerous consequences and injury to self or others. (22, 25, 27–31, 33–37, 41, 43–48) Some patients described that fear of hypoglycemia caused them to avoid participating in normal activities, such as work, driving, and social activities, (43) resulting in a significant sacrifice of quality of life.
Beyond fear and anxiety, patients also experienced frustration when, despite their best efforts, their blood sugar levels remained unstable. (21, 25, 30, 32, 37, 42, 43) Not being able to achieve target blood sugar levels given by health care practitioners also resulted in feelings of guilt (21, 24, 30, 32, 35, 37, 38) and powerlessness. (25, 26, 30, 32, 35, 37, 40) These constant negative emotions associated with diabetes control and self-management left some patients feeling they had an unfair situation—that they were saddled with an unbearable or impossible burden. (21, 22, 31) Others found themselves feeling stressed from the constant weight of unsuccessful efforts to control their diabetes. (21, 29) Many patients reported feeling estranged from people without diabetes, being outsiders to the “normal” world. (21, 30, 31, 34, 39) For some patients, the cumulative effect of all these negative emotions was depression. (25, 32, 35)
Practical Domain
The effects of uncontrolled type 1 diabetes influenced the way that patients structured their lives. (21–37, 39, 41, 43, 44, 46, 47, 49) Many patients described rigidly adhering to a rigorous routine of testing, eating, and activity as the most reliable way to avoid negative consequences of hypoglycemia or hyperglycemia. (24, 25, 29, 30, 32–34, 41, 43, 47) This routine was simultaneously a way to try to recapture some quality of life and also a limiting factor to quality of life: rigid routines helped to avoid serious complications of uncontrolled diabetes (e.g., hypoglycemic event), but they also severely limited the way patients could engage in social and employment activities. (21–26, 28–30, 32–34, 36, 39, 41, 43, 47) Patients remarked that the careful planning and lack of spontaneity entailed by these routines was limiting or restrictive, often affecting the whole family. (24, 25, 30, 32–34, 41, 43)
Explanations for this limited engagement with employment and leisure activities included the amount of planning and organization required to self-manage uncontrolled diabetes, (21, 23, 25, 30, 31, 39, 41, 47) time lost to illness-related absences including medical appointments, (22, 23, 26, 28, 37, 47) lower levels of function when blood sugar ran too high or low, (22, 28, 39, 41, 47) and the need for time and space to eat, monitor blood sugar, and administer insulin. (21, 23, 26, 30, 39, 47) These challenges were particularly acute for people engaged in activities where suboptimal function (e.g., hypoglycemic event) would result in a danger to self or others, such as driving, operating heavy machinery, or acting as the sole caregiver for an infant or very young child. (23, 25, 27, 28, 35–37, 43, 46, 47) For some, this combination of challenges resulted in a loss of employment opportunities and wages. (22, 23)
One strategy that patients reported using to reclaim their ability to participate in employment and leisure activities was setting their own target blood glucose levels, without input from their health care providers. (25, 29, 35, 39, 41, 43, 44, 47) Many patients described purposefully running their sugar levels high to avoid hypoglycemic episodes, even knowing that this may result in long-term complications. (29, 34, 36, 39, 44, 46, 47) Long-term consequences aside, patients described hyperglycemia as uncomfortable and unpleasant. (46, 48)
Social Domain
Patients reported that uncontrolled diabetes affected their everyday relationships and social experiences, with many patients expressing negative impacts on their social well-being. (21–24, 26, 28–39, 41–43, 45, 46, 50, 51) These included feelings of alienation, (21, 24, 30) embarrassment, (28–30, 39, 46) and stigmatization, (21, 24, 34, 46, 50) and the inability to participate in regular social activities. (21, 29, 43)
Patients felt that their attempts to maintain good glycemic control required sacrificing many aspects of their social lives, as balancing social needs with the demands of diabetes management is challenging, exhausting, and potentially alienating. (25, 31, 36, 38, 39) This need for sacrifice and balance left many patients feeling different from others in their social circles and the public in general; many reported feeling self-conscious about their social identity as a “diabetic.” (24, 26, 30, 31, 39, 43, 46). Self-management processes such as daily insulin injections, blood glucose monitoring, and the use of an insulin pump made patients feel awkward, embarrassed, and alienated. (21, 24, 30, 34, 46, 50) They felt that these visible aspects of their illness marked them as different or an outsider, leading others to believe that they were unable to live a normal life. (21, 26, 30, 31, 39, 43, 46, 50) In public, and among family and friends, many patients reported feeling stigmatized because of diabetes. (21, 24, 45, 46) Fear of stigmatization and of being embarrassed by their condition prevented patients from engaging in normal social activities (21, 39):
Some patients felt that family and friends were unable to relate or unwilling to help (30, 47)
Some felt discouraged about spending time with family and friends as they did not want to experience a hypoglycemic episode in the presence of others, and were afraid that others could become frustrated by their self-management routines (28, 30, 33, 39, 41)
The need to monitor and control both diet and physical activity hindered patients’ ability to experience and enjoy social activities or outings (21, 29, 34, 36, 38)
Family members and loved ones play an important role in the management of uncontrolled diabetes. (22, 24, 28, 30, 31, 33, 35, 37, 44) Although family members do not experience the biological difficulties of diabetes, the chronicity and life-long self-management of this condition affect caregivers’ emotions, daily well-being, and social lives. Parents, friends, and spouses alike faced anxieties about the health of their loved one, expressing fear of potential short- and long-term complications of uncontrolled diabetes. (22, 28, 31, 37, 45, 46, 51) Family and friends reported anxiety about the possibility of hypoglycemia, and were often anxious about their partner or family member missing insulin injections or forgetting to monitor their blood glucose levels. (28, 33, 36, 45, 51)
The emotional distress and complexity of diabetes management had an impact on caregivers’ own daily lives and well-being. Patients’ families and loved ones were frequently required to support diabetes management regimens, and to share the social and practical consequences of uncontrolled diabetes. (22, 24, 28, 30, 31, 33, 37) For example, this support required:
Helping the patient stay on track with management routines (28, 30)
Assisting with insulin therapies and blood glucose monitoring (28, 30, 33, 41)
Losing sleep when the patient experienced nocturnal hypoglycemia (22, 38, 45)
Often the difficulties and stress associated with uncontrolled diabetes can result in antagonism between patients and family members. Fear, anxiety, and disagreement over the processes of diabetes management can cause interpersonal conflict between partners, friends, and family members; (25, 26, 30, 37, 45, 51) many patients stated that they felt like a burden due to their family. (24, 28, 30, 31, 37)
Similar to the ways in which patients can become excluded from social activities when trying to manage uncontrolled diabetes, family members also make sacrifices in their social lives in order to care for and prevent their diabetic family member from experiencing complications; for example, some avoid social activities for fear of abandoning their partner. (28, 30, 33, 37) Furthermore, family members can neglect their own health, work life, and social needs as they become overwhelmingly invested in supporting their loved one. (21, 22, 28, 30, 33, 35, 37–39, 51) Ultimately, the consequences of inter-family or inter-partner distress and the disruption of a comfortable social life can deteriorate the quality of life of both patients with diabetes and their families.
Example: How Hypoglycemia Affects All Aspects of Quality of Life
Hypoglycemic events are one of the most frequently discussed aspects of life with uncontrolled type 1 diabetes. Patients’ discussions of hypoglycemic events illustrate how the domains of impact interact to lower quality of life.
Hypoglycemic events take place when the blood sugar level is low, and they have immediate consequences. Although experiences vary, hypoglycemia typically involves symptoms that include (22–24, 27, 28, 37, 39):
Feeling hot or cold
Dizziness
Trouble walking or with balance
Heart palpitations
Restlessness
Confusion or cognitive dysfunction
Strange dreams
Vision disturbances
Headaches
Weakness or muscle tension
Neuropathy
Anxiety, panic, or anger
Nausea
After hypoglycemic incidents, patients often felt tired, drained, or disoriented. Some of these feelings lasted a couple of days, so patients were not able to work or function well. (22, 37)
The unpleasantness and unpredictability of hypoglycemic incidents caused significant anxiety for patients, who feared that the events would strike at inopportune, embarrassing, or even dangerous times. (22, 25, 27–31, 33–37, 41, 43–48) For instance, many people with uncontrolled type 1 diabetes chose not to drive or operate machinery for fear of injury to self or others in the event of a hypoglycemic event. Some mentioned feeling uncomfortable being the sole caregiver for a young child or infant. (23, 25, 27, 28, 35–37, 43, 46, 47) These anxieties limited employment and leisure activities, as well as causing stress to patients and family.
Beyond physical danger, patients described the social impact of experiencing hypoglycemia in public as “frightening, disabling and deeply embarrassing socially.” (29, 46) The symptoms of hypoglycemic events contributed to a perception of social stigma among people with type 1 diabetes, (21, 23, 24, 30, 34, 43, 47) resulting in some patients withdrawing from social activities; many found it difficult to sufficiently adhere to their self-management routines to avoid hypoglycemic events while still protecting the confidentiality of their diabetic status. (21, 25, 28–31, 36, 38, 39, 43)
Hypoglycemic events also had biological effects on mental function, making patients irritable, aggressive, or confused. (21, 23–25, 27, 28, 32, 33, 37, 39) This was sometimes alarming for family members, who felt vulnerable to patients’ moods and aggressions, exacerbating worry for their loved one's health and safety. (22, 24, 28, 30, 32, 33, 35–38, 41, 45, 51)
The shadow of hypoglycemic events affected patients in other ways, too. Beyond restricting activities and social opportunities, patients often altered their self-management practices to avoid hypoglycemia. The most commonly discussed way was changing their own blood glucose target levels without consulting health care providers. (25, 29, 35, 39, 41, 43, 44, 47) Many patients discussed purposefully maintaining high blood glucose levels to avoid hypoglycemic events. They prioritized the avoidance of hypoglycemia in the short term over potential complications of hyperglycemia in the long term. (29, 34, 36, 39, 44, 46, 47)
LIMITATIONS
Qualitative research provides theoretical and contextual insights into the experiences of limited numbers of people in specific settings. Qualitative research findings are not intended to generalize directly to populations, although meta-synthesis across a number of qualitative studies builds an increasingly robust understanding that is more likely to be transferable. While qualitative insights are robust and often enlightening for understanding experiences and planning services in other settings, the findings of the studies reviewed here—and of this synthesis—do not strictly generalize to the Ontario (or any specific) population. The findings are limited to the conditions included in the body of literature synthesized (i.e., diabetes). This evidence must be interpreted and applied carefully, in light of expertise and the experiences of the relevant community.
CONCLUSIONS
Serious consequences of type 1 diabetes include long-term adverse effects of hyperglycemia and short-term impacts of hypoglycemic events. Whether through the negative consequences of uncontrolled type 1 diabetes or efforts to avoid them, these patients experience impacts to their physical, emotional, practical, and social quality of life. The impacts on each of these domains are connected:
Physically, people with uncontrolled type 1 diabetes often feel ill, experience cognitive dysfunction, have difficulty maintaining their weight at a desired level, and experience fluctuating moods. Women who are pregnant or breast-feeding may find these physical symptoms exacerbated as their blood sugar level fluctuates more dramatically in response to hormone changes, pregnancy-induced nausea and vomiting, and breast-feeding
Emotionally, patients may feel anxious about long-term consequences of hyperglycemia and short-term consequences of hypoglycemia. Patients with uncontrolled diabetes may also experience frustration, guilt, and powerlessness at their inability to control their diabetes. They may feel alienated from the “normal” world, and the cumulative effect of all of these negative emotions can result in depression
Practically, patients may choose to adhere to very rigid self-management regimens in an effort to control their diabetes. The rigidity of these routines may have negative impacts on the employment and social opportunities available. Patients with uncontrolled diabetes may be reluctant to engage in activities, such as driving or operating heavy machinery, where hypoglycemic episodes could have particularly negative consequences. They may not be able to consistently perform to their best level at work due to rigid self-management routines and the negative physical impacts of hypoglycemia and hyperglycemia; this may result in lost wages and professional opportunities
Socially, patients with uncontrolled diabetes experience several negative impacts on their well-being, including alienation, embarrassment, and stigmatization. These experiences, paired with the need for very rigid self-management routines, may result in withdrawal from social activities. The social consequences of uncontrolled diabetes also affect the family members, who report significant amounts of worry and anxiety about their loved ones with diabetes. Many family members describe changing their own routines and social lives in order to support the needs of their loved ones
Even when the serious consequences of type 1 diabetes occur only infrequently, the time and energy spent by patients avoiding these consequences can have negative impacts on their professional, social, and family lives. Also, patients may choose to adjust their own target blood glucose levels, intentionally running high in an effort to prioritize avoiding hypoglycemic events in the short term over avoiding the complications of hyperglycemia in the long term.
ACKNOWLEDGEMENTS
Editorial Staff
Susan Harrison
APPENDICES
Appendix 1: Literature Search Strategies
Hybrid Filter: OVID MEDLINE
-
1.
Interviews+
-
2.
(theme$ or thematic).mp.
-
3.
qualitative.af.
-
4.
Nursing Methodology Research/
-
5.
questionnaire$.mp.
-
6.
ethnological research.mp.
-
7.
ethnograph$.mp.
-
8.
ethnonursing.af.
-
9.
phenomenol$.af.
-
10.
(grounded adj (theor$ or study or studies or research or analys?s)).af.
-
11.
(life stor$ or women* stor$).mp.
-
12.
(emic or etic or hermeneutic$ or heuristic$ or semiotic$).af. or (data adj1 saturat$).tw. or participant observ$.tw.
-
13.
(social construct$ or (postmodern$ or post-structural$) or (post structural$ or poststructural$) or post modern$ or post-modern$ or feminis$ or interpret$).mp.
-
14.
(action research or cooperative inquir$ or co operative inquir$ or co-operative inquir$).mp.
-
15.
(humanistic or existential or experiential or paradigm$).mp.
-
16.
(field adj (study or studies or research)).tw.
-
17.
human science.tw.
-
18.
biographical method.tw.
-
19.
theoretical sampl$.af.
-
20.
((purpos$ adj4 sampl$) or (focus adj group$)).af.
-
21.
(account or accounts or unstructured or open-ended or open ended or text$ or narrative$).mp.
-
22.
(life world or life-world or conversation analys?s or personal experience$ or theoretical saturation).mp
-
23.
(lived or life adj experience$.mp
-
24.
cluster sampl$.mp.
-
25.
observational method$.af.
-
26.
content analysis.af.
-
27.
(constant adj (comparative or comparison)).af.
-
28.
((discourse$ or discurs$) adj3 analys?s).tw.
-
29.
narrative analys?s.af.
-
30.
heidegger$.tw.
-
31.
colaizzi$.tw.
-
32.
spiegelberg$.tw.
-
33.
(van adj manen$).tw.
-
34.
(van adj kaam$).tw.
-
35.
(merleau adj ponty$).tw
-
36.
.husserl$.tw
-
37.
foucault$.tw.
-
38.
(corbin$ adj2 strauss$).tw
-
39.
glaser$.tw.
NOT
-
40.
p =.ti,ab.
-
41.
p<.ti,ab.
-
42.
p>.ti,ab.
-
43.
p =.ti,ab.
-
44.
p<.ti,ab.
-
45.
p>.ti,ab.
-
46.
p-value.ti,ab.
-
47.
retrospective.ti,ab.
-
48.
regression.ti,ab.
-
49.
statistical.ti,ab.
Hybrid Filter: EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL)
-
1.
Interviews+
-
2.
MH audiorecording
-
3.
MH Grounded theory
-
4.
MH Qualitative Studies
-
5.
MH Research, Nursing
-
6.
MH Questionnaires+
-
7.
MH Focus Groups (12639)
-
8.
MH Discourse Analysis (1176)
-
9.
MH Content Analysis (11245)
-
10.
MH Ethnographic Research (2958)
-
11.
MH Ethnological Research (1901)
-
12.
MH Ethnonursing Research (123)
-
13.
MH Constant Comparative Method (3633)
-
14.
MH Qualitative Validity+ (850)
-
15.
MH Purposive Sample (10730)
-
16.
MH Observational Methods+ (10164)
-
17.
MH Field Studies (1151)
-
18.
MH theoretical sample (861)
-
19.
MH Phenomenology (1561)
-
20.
MH Phenomenological Research (5751)
-
21.
MH Life Experiences+ (8637)
-
22.
MH Cluster Sample+ (1418)
-
23.
Ethnonursing (179)
-
24.
ethnograph* (4630)
-
25.
phenomenol* (8164)
-
26.
grounded N1 theor* (6532)
-
27.
grounded N1 study (601)
-
28.
grounded N1 studies (22)
-
29.
grounded N1 research (117)
-
30.
grounded N1 analys?s (131)
-
31.
life stor* (349)
-
32.
women's stor* (90)
-
33.
emic or etic or hermeneutic$ or heuristic$ or semiotic$ (2305)
-
34.
data N1 saturat* (96)
-
35.
participant observ* (3417)
-
36.
social construct* or postmodern* or post-structural* or post structural* or poststructural* or post modern* or post-modern* or feminis* or interpret* (25187)
-
37.
action research or cooperative inquir* or co operative inquir* or co-operative inquir* (2381)
-
38.
humanistic or existential or experiential or paradigm* (11017)
-
39.
field N1 stud* (1269)
-
40.
field N1 research (306)
-
41.
human science (132)
-
42.
biographical method (4)
-
43.
theoretical sampl* (983)
-
44.
purpos* N4 sampl* (11299)
-
45.
focus N1 group* (13775)
-
46.
account or accounts or unstructured or open-ended or open ended or text* or narrative* (37137)
-
47.
life world or life-world or conversation analys?s or personal experience* or theoretical saturation (2042)
-
48.
lived experience* (2170)
-
49.
life experience* (6236)
-
50.
cluster sampl* (1411)
-
51.
theme* or thematic (25504)
-
52.
observational method* (6607)
-
53.
questionnaire* (126686)
-
54.
content analysis (12252)
-
55.
discourse* N3 analys?s (1341)
-
56.
discurs* N3 analys?s (35)
-
57.
constant N1 comparative (3904)
-
58.
constant N1 comparison (366)
-
59.
narrative analys?s (312)
-
60.
Heidegger* (387)
-
61.
Colaizzi* (387)
-
62.
Spiegelberg* (0)
-
63.
van N1 manen* (261)
-
64.
van N1 kaam* (34)
-
65.
merleau N1 ponty* (78)
-
66.
husserl* (106)
-
67.
Foucault* (253)
-
68.
Corbin* N2 strauss* (50)
-
69.
strauss* N2 corbin* (88)
-
70.
glaser* (302)
NOT
-
71.
TI statistical OR AB statistical
-
72.
TI regression OR AB regression
-
73.
TI retrospective OR AB retrospective
-
74.
TI p-value OR AB p-value
-
75.
TI p< OR AB p<
-
76.
TI p< OR AB p<
-
77.
TI p= OR AB p=
Hybrid Filter: ISI Web of Science, Social Science Citation Index
-
1.
TS=interview*
-
2.
TS=(theme*)
-
3.
TS=(thematic analysis)
-
4.
TS=qualitative
-
5.
TS=nursing research methodology
-
6.
TS=questionnaire
-
7.
TS=(ethnograph*)
-
8.
TS= (ethnonursing)
-
9.
TS=(ethnological research)
-
10.
TS=(phenomenol*)
-
11.
TS=(grounded theor*) OR TS=(grounded stud*) OR TS=(grounded research) OR TS=(grounded analys?s)
-
12.
TS=(life stor*) OR TS=(women's stor*)
-
13.
TS=(emic) OR TS=(etic) OR TS=(hermeneutic) OR TS=(heuristic) OR TS=(semiotic) OR TS=(data saturat*) OR TS=(participant observ*)
-
14.
TS=(social construct*) OR TS=(postmodern*) OR TS=(post structural*) OR TS=(feminis*) OR TS=(interpret*)
-
15.
TS=(action research) OR TS=(co-operative inquir*)
-
16.
TS=(humanistic) OR TS=(existential) OR TS=(experiential) OR TS=(paradigm*)
-
17.
TS=(field stud*) OR TS=(field research)
-
18.
TS=(human science)
-
19.
TS=(biographical method*)
-
20.
TS=(theoretical sampl*)
-
21.
TS=(purposive sampl*)
-
22.
TS=(open-ended account*) OR TS=(unstructured account) OR TS=(narrative*) OR TS=(text*)
-
23.
TS=(life world) OR TS=(conversation analys?s) OR TS=(theoretical saturation)
-
24.
TS=(lived experience*) OR TS=(life experience*)
-
25.
TS=(cluster sampl*)
-
26.
TS=observational method*
-
27.
TS=(content analysis)
-
28.
TS=(constant comparative)
-
29.
TS=(discourse analys?s) or TS =(discurs* analys?s)
-
30.
TS=(narrative analys?s)
-
31.
TS=(heidegger*)
-
32.
TS=(colaizzi*)
-
33.
TS=(spiegelberg*)
-
34.
TS=(van manen*)
-
35.
TS=(van kaam*)
-
36.
TS=(merleau ponty*)
-
37.
TS=(husserl*)
-
38.
TS=(foucault*)
-
39.
TS=(corbin*)
-
40.
TS=(strauss*)
-
41.
TS=(glaser*)
NOT
-
42.
TS=(p-value)
-
43.
TS=(retrospective)
-
44.
TS=(regression)
-
45.
TS=(statistical)
REFERENCES
- (1).Canadian Diabetes Association. Diabetes: Canada at the tipping point [Internet]. Toronto (ON): The Association; 2015. [cited 2015 Feb 6]. Available from: http://www.diabetes.ca/CDA/media/documents/publications-and-newsletters/advocacy-reports/canada-at-the-tipping-point-english.pdf [Google Scholar]
- (2).Types of diabetes [Internet]. Toronto (ON): Canadian Diabetes Association; 2015. [cited 2015 Feb 4]. Available from: http://www.diabetes.ca/about-diabetes/types-of-diabetes [Google Scholar]
- (3).Brittle diabetes (labile diabetes) [Internet]. United Kingdom: Diabetes.co.uk; 2015. [cited 2015 Feb 5]. Available from: http://www.diabetes.co.uk/brittle-diabetes.html [Google Scholar]
- (4).Shaw RL, Booth A, Sutton AJ, Miller T, Smith JA, Young B, et al. Finding qualitative research: an evaluation of search strategies. BMC Med Res Methodol. 2004; 4(1): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Wilczynski NL, Marks S, Haynes RB. Search strategies for identifying qualitative studies in CINAHL. Qual Health Res. 2007; 17(5): 705–10. [DOI] [PubMed] [Google Scholar]
- (6).Wong S, Wilczynski NL, Haynes RB. Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Medinfo. 2004; 11(Pt 1): 311–6. [PubMed] [Google Scholar]
- (7).Sandelowski M, Barroso J. Creating metasummaries of qualitative findings. Nurs Res. 2003; 52(4): 226–33. [DOI] [PubMed] [Google Scholar]
- (8).Sandelowski M, Barroso J. Toward a metasynthesis of qualitative findings on motherhood in HIV-positive women. Res Nurs Health. 2003; 26(2): 153–70. [DOI] [PubMed] [Google Scholar]
- (9).Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. New York: Springer Publishing Co.; 2006. [Google Scholar]
- (10).Saini M, Shlonsky A. Systematic synthesis of qualitative research. New York: Oxford University Press; 2012. [Google Scholar]
- (11).Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London, UK: Sage Publications; 2006. [Google Scholar]
- (12).Corbin JM. Basics of qualitative research: techniques and procedures for developing grounded theory. 3rd ed. Los Angeles (CA): Sage Publications Inc.; 2008. [Google Scholar]
- (13).Finfgeld DL. Metasynthesis: the state of the art—so far. Qual Health Res. 2003; 13(7): 893–904. [DOI] [PubMed] [Google Scholar]
- (14).Melia KM. Recognizing quality in qualitative research. In: Bourgeault IL, DeVries R, Dingwall R, editors. SAGE Handbook of Qualitative Health Research. Thousand Oaks (CA): Sage; 2010. p. 559–74. [Google Scholar]
- (15).Sandelowski M, Barroso J. Finding the findings in qualitative studies. J Nurs Scholarsh. 2002; 34(3): 213–9. [DOI] [PubMed] [Google Scholar]
- (16).Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009; 9(1): 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Finfgeld-Connett D. Meta-synthesis of presence in nursing. J Adv Nurs. 2006; 55(6): 708–14. [DOI] [PubMed] [Google Scholar]
- (18).Noblit G, Hare RD. Meta-ethnography: synthesizing qualitative studies. Newbury Park (CA): Sage Publications; 1988. [Google Scholar]
- (19).Paterson BL. Coming out as ill: understanding self-disclosure in chronic illness from a meta-synthesis of qualitative research. In: Webb C, Roe B, editors. Reviewing research evidence for nursing practice. Malden (MA): Blackwell Publishing Inc.; 2007. p. 73–83. [Google Scholar]
- (20).Moher D, Liberati A, Tetzlaff J, Altman DG, the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6(6): e100009. [PMC free article] [PubMed] [Google Scholar]
- (21).Balfe M, Doyle F, Smith D, Sreenan S, Brugha R, Hevey D, et al. What's distressing about having type 1 diabetes? A qualitative study of young adults’ perspectives. BMC Endocr Disord. 2013;13:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Brod M, Pohlman B, Wolden M, Christensen T. Non-severe nocturnal hypoglycemic events: experience and impacts on patient functioning and well-being. Qual Life Res. 2013; 22(5): 997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Burda MHF, van der Horst F, van den Akker M, Stork ADM, Crebolder H, van Attekum T, et al. Identifying experiential expertise to support people with diabetes mellitus in applying for and participating effectively in paid work a qualitative study. J Occup Environ Med. 2012; 54(1): 92–100. [DOI] [PubMed] [Google Scholar]
- (24).Garmo A, Hornsten A, Leksell J. ‘The pump was a saviour for me.’ Patients’ experiences of insulin pump therapy. Diabet Med. 2013; 30(6): 717–23. [DOI] [PubMed] [Google Scholar]
- (25).Hortensius J, Kars MC, Wierenga WS, Kleefstra N, Bilo HJ, van der Bijl JJ. Perspectives of patients with type 1 or insulin-treated type 2 diabetes on self-monitoring of blood glucose: a qualitative study. BMC Public Health. 2012; 12:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Kay C, Davies J, Gamsu D, Jarman M. An exploration of the experiences of young women living with type 1 diabetes. J Health Psychol. 2009; 14(2): 242–50. [DOI] [PubMed] [Google Scholar]
- (27).Lawton J, Rankin D, Cooke DD, Elliott J, Amiel S, Heller S, et al. Self-treating hypoglycaemia: a longitudinal qualitative investigation of the experiences and views of people with type 1 diabetes. Diabet Med. 2013; 30(2): 209–15. [DOI] [PubMed] [Google Scholar]
- (28).Lawton J, Rankin D, Elliott J, Heller SR, Rogers HA, De Zoysa N, et al. Experiences, views, and support needs of family members of people with hypoglycemia unawareness: interview study. Diabetes Care. 2014; 37(1): 109–15. [DOI] [PubMed] [Google Scholar]
- (29).Nafees B, Lloyd A, Kennedy-Martin T, Hynd S. How diabetes and insulin therapy affects the lives of people with type 1 diabetes. Eur Diabetes Nurs. 2006; 3(2): 92–7. [Google Scholar]
- (30).Rasmussen B, O'Connell B, Dunning P, Cox H. Young women with type 1 diabetes’ management of turning points and transitions. Qual Health Res. 2007; 17(3): 300–10. [DOI] [PubMed] [Google Scholar]
- (31).Richmond J. Coping with diabetes through pregnancy. Br J Midwifery. 2009; 17(2): 84–91. [Google Scholar]
- (32).Ridge K, Treasure J, Forbes A, Thomas S, Ismail K. Themes elicited during motivational interviewing to improve glycaemic control in adults with type 1 diabetes mellitus. Diabet Med. 2012; 29(1): 148–52. [DOI] [PubMed] [Google Scholar]
- (33).Rintala TM, Paavilainen E, Åstedt-Kurki P. Everyday life of a family with diabetes as described by adults with type 1 diabetes. Eur Diabetes Nurs. 2013; 10(3): 86–90. [Google Scholar]
- (34).Ritholz MD, Smaldone A, Lee J, Castillo A, Wolpert H, Weinger K. Perceptions of psychosocial factors and the insulin pump. Diabetes Care. 2007; 30(3): 549–54. [DOI] [PubMed] [Google Scholar]
- (35).Sparud-Lundin C, Berg M. Extraordinary exposed in early motherhood—a qualitative study exploring experiences of mothers with type 1 diabetes. BMC Womens Health. 2011; 11(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Sutton L, Chapman-Novakofski K. Hypoglycemia education needs. Qual Health Res. 2011; 21(9): 1220–8. [DOI] [PubMed] [Google Scholar]
- (37).Trief PM, Sandberg JG, Dimmock JA, Forken PJ, Weinstock RS. Personal and relationship challenges of adults with type 1 diabetes: a qualitative focus group study. Diabetes Care. 2013; 36(9): 2483–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Watts S, O'Hara L, Trigg R. Living with type 1 diabetes: a by-person qualitative exploration. Psychol Health. 2010; 25(4): 491–506. [DOI] [PubMed] [Google Scholar]
- (39).Wilson V. Students’ experiences of managing type 1 diabetes. Paediatr Nurs. 2010; 22(10): 25–8. [DOI] [PubMed] [Google Scholar]
- (40).Grant L, Lawton J, Hopkins D, Elliott J, Lucas S, Clark M, et al. Type 1 diabetes structured education: what are the core self-management behaviours? Diabet Med. 2013;30(6): 724–30. [DOI] [PubMed] [Google Scholar]
- (41).Lawson VL, Lyne PA, Harvey JN, Bundy CE. Understanding why people with type 1 diabetes do not attend for specialist advice: a qualitative analysis of the views of people with insulin-dependent diabetes who do not attend diabetes clinic. J Health Psychol. 2005; 10(3): 409–23. [DOI] [PubMed] [Google Scholar]
- (42).Mayer DD, Rosenfeld A. Symptom interpretation in women with diabetes and myocardial infarction: a qualitative study. Diabetes Educ. 2006; 32(6): 918–24. [DOI] [PubMed] [Google Scholar]
- (43).Pera PI. Living with diabetes: quality of care and quality of life. Patient Prefer Adherence. 2011; 5:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (44).Rankin D, Cooke DD, Heller S, Elliott J, Amiel S, Lawton J, et al. Experiences of using blood glucose targets when following an intensive insulin regimen: a qualitative longitudinal investigation involving patients with type 1 diabetes. Diabet Med. 2012; 29(8): 1079–84. [DOI] [PubMed] [Google Scholar]
- (45).Ritholz MD, Beste M, Edwards SS, Beverly EA, Atakov-Castillo A, Wolpert HA. Impact of continuous glucose monitoring on diabetes management and marital relationships of adults with type 1 diabetes and their spouses: a qualitative study. Diabet Med. 2014; 31(1): 47–54. [DOI] [PubMed] [Google Scholar]
- (46).Rogers HA, de Zoysa N, Amiel SA. Patient experience of hypoglycaemia unawareness in type 1 diabetes: are patients appropriately concerned? Diabet Med. 2012;29(3): 321–7. [DOI] [PubMed] [Google Scholar]
- (47).Ruston A, Smith A, Fernando B. Diabetes in the workplace—diabetic's perceptions and experiences of managing their disease at work: a qualitative study. BMC Public Health. 2013; 13:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (48).Savage S, Duggan N, Dunning T, Martin P. The experiences and care preferences of people with diabetes at the end of life: a qualitative study. J Hosp Palliat Nurs. 2012; 14(4): 293–302. [Google Scholar]
- (49).Snow R, Fulop N. Understanding issues associated with attending a young adult diabetes clinic: a case study. Diabet Med. 2012; 29(2): 257–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Browne JL, Ventura A, Mosely K, Speight J. ‘I'm not a druggie, I'm just a diabetic': a qualitative study of stigma from the perspective of adults with type 1 diabetes. BMJ Open. 2014; 4(7): 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (51).Sandberg J, Trief PM, Greenberg RP, Graff K, Weinstock RS. “He said, she said”: the impact of gender on spousal support in diabetes management. J Couple Relationship Ther. 2006; 5(2): 23–42. [Google Scholar]