Abstract
In recent years, three hypotheses have been set forth positing variations on a common question—Has the rate of human aging already been modified? There is no disputing that people now live longer than ever before in history, and considerable variation in duration of life persists as a fundamental attribute of human longevity, but are these events caused by a measurable and verifiable difference in the rate at which people age, or are there other reasons why they occur? In this article, I explore the historical record involving changes in survival and life expectancy at older ages dating back to 1900, and examine what factors will likely contribute to changes in longevity in the United States through 2040. Evidence suggests that despite the absence of verifiable metrics of biological age, delayed aging is unlikely to be a cause of secular increases in life expectancy, but it could explain variation in survival among population subgroups, and it is the most likely explanation for why exceptionally long-lived people experience less disease and live longer than the rest of the population. If genetic heterogeneity explains any significant part of current variation in longevity, this opens the door to the development of therapeutic interventions that confer these advantages to the rest of the population.
Delayed aging may explain why some (but not all) people today experience less disease and live significantly longer than earlier generations. These people may possess “protective genes” that slow the aging process.
The rise in human longevity is one of humanity’s crowning achievements. There has been more survival time manufactured by public health and medical technology in the last 115 years than in all of human history combined. It has been well established that ∼80% of the rise in longevity in the first half of the 20th century in the United States (and most other developed nations) was because of declining early age mortality—mostly from reductions in death rates from communicable diseases. Since 1950, ∼80% of the gain in longevity was because of declining death rates at middle and older ages owing to progress made against chronic fatal diseases such as cardiovascular diseases (CVDs) (Kinsella 1992). Death rates at younger and middle ages have declined dramatically. Now ∼85% of all babies born today in developed nations will survive to at least age 65, and most deaths are concentrated in the 30-yr time period between ages 65 and 95 (see the Human Mortality Database, www.mortality.org).
Although the proximate causes of declining middle and old age mortality are not in dispute (e.g., a combination of advances in public health, improved behavioral and social risk factors, and medical technology), some researchers have speculated that improved mortality statistics alone are sufficient reason to suspect that people in the modern era may be aging more slowly relative to the generations that preceded them. For example, after observing declines in death rates in Sweden from 1900 to 1990, Vaupel and Lundstrom concluded that “… one interpretation of these shifts [declining old age mortality across time] is that the process of aging has been slowed or delayed in Sweden such that elderly Swedish men are effectively three or four years ‘younger’ than they used to be …” (Vaupel and Lundstrom 1994, p. 90). This view was repeated by Vaupel when he stated “… before the discovery that senescence could be postponed [a conclusion based on the observation that death rates at older ages declined], geriatric medicine was viewed as a laudable but rather futile effort to palliate the misery of those in the process of dying” (Vaupel 2010, p. 536). Levine and Crimmins (2014) documented morbidity and mortality differentials and measured biomarkers among Blacks and Whites in the United States using the National Health and Nutrition Examination Survey, concluding that premature declines in health among Blacks observed today may be indicative of an acceleration of the biological processes of aging. The study of centenarians and their offspring has led Atzmon et al. (2005) and Perls et al. (2002) to speculate that this subgroup of the population lives so long, or at least has the potential for exceptionally long lives, because they are biologically aging at a slower pace relative to the rest of the population. That is, for long-lived people, it is hypothesized that 1 yr of clock time is matched by less than 1 yr of biological time.
The preceding paragraph exemplifies the difficulty in understanding the nuances of aging science and how scientists in other disciplines interpret it. One group of researchers observed secular declines in death rates at older ages and concluded from this that more recent cohorts passing through the same age window relative to previous cohorts are “aging more slowly” (referred to here for simplicity as the “secular aging rate hypothesis”). A second set of researchers observed mortality differentials among population subgroups at a single moment in time, and speculated that the shorter-lived subgroup is “aging more rapidly” because of variation in behavioral or environmental risk factors (referred to here as the “comparative aging rate hypothesis”). The third set of researchers focused on the genetics of long-lived people and their offspring, and concluded that these people live so long because they possess “protective genes” that enable them to escape or delay the ravages of time and “age more slowly” than the rest of the population (referred to here as the “heterogeneity aging rate hypothesis”). Can all three of these variations in aging rate be operating?
Let us begin by defining terms, because it is important to know what is meant by “rate of aging” and what it does not mean. According to Olshansky et al. (2008), a defensible definition of aging is:
… the accumulation of random damage to the building blocks of life—especially to DNA, certain proteins, carbohydrates, and lipids (fats)—that begins early in life and eventually exceeds the body’s self-repair capabilities. This damage gradually impairs the functioning of cells, tissues, organs, and organ systems, thereby increasing vulnerability to disease and giving rise to the characteristic manifestations of aging, such as a loss of muscle and bone mass, a decline in reaction time, compromised hearing and vision, and reduced elasticity of the skin. This accretion of molecular damage comes from many sources, including, ironically, the life-sustaining processes involved in converting the food we eat into usable energy… . Aging, in our view, makes us ever more susceptible to such ills as heart disease, Alzheimer’s disease, stroke and cancer, but these age-related conditions are superimposed on aging, not equivalent to it. Therefore, even if science could eliminate today’s leading killers of older individuals, aging would continue to occur, ensuring that different maladies would take their place. In addition, it would guarantee that one crucial body component or another—say, the cardiovascular system—would eventually experience a catastrophic failure. It is an inescapable biological reality that once the engine of life switches on, the body inevitably sows the seeds of its own destruction.
Aging is not defined by the diseases that kill us or which make us more frail and disabled, because most (but not all) of these conditions are heritable on the one hand and, more importantly, inherently modifiable through risk factor modification. It was suggested long ago that biological age can be measured by actuarial analysis of large populations, through assessment of overall morbidity, or observation of chronic degenerative changes (Ludwig and Smoke 1980). But this confusion of biological aging with measurable health and mortality outcomes expressed at later ages is perhaps the source of the problem. The fact is, biological aging itself cannot as yet be reliably measured by any single or multiple “biomarkers of aging” (Baker and Sprott 1988; Kirkwood and Austad 2000), although there may come a time in the future when trustworthy biomarkers of aging are discovered. So, if we cannot measure or directly observe biological aging, let us begin by exploring the documented reasons behind the rise in longevity in the 20th century, with a particular focus on later ages, and what factors what might influence these trends going forward. By revealing what is known about mortality and survival across time and between population subgroups, it is then possible to assess whether any of the three hypotheses set forth are plausible.
DEMOGRAPHIC COMPARISON OF THREE OLDER COHORTS (1965, 2015, and 2040)
Let us begin with some basic historical longevity statistics. In 1965, the life expectancy of the U.S. population was 70.2 yr. In 1900, life expectancy was 47.7 yr. The probability of a baby born in 1965 reaching the age of 65 was 71.3%. In 1900, it was only 39.1%. Among those that had already celebrated their 65th birthday in 1965, 28.1% would survive to their 85th birthday. In 1900, only 14% of those reaching age 65 survived to age 85 (see Life Tables for the United States, www.ssa.gov/oact/NOTES/as120/LifeTables_Tbl_6.html). Statistics like these appear repeatedly throughout the literature describing historical trends in longevity in the United States.
There is no doubt that, based on these simple statistics alone, longevity and the enriched health conditions required to generate such increases in survival, improved dramatically in the 20th century. Many more Americans now survive to ages 65+ than at any time in history. We survive longer once having reached this age, and based on an inevitable rapid shift in America’s age structure, it is certain that the prevalence of people surviving up to and beyond age 65 will rise dramatically by midcentury. However, the picture these statistics convey is only part of the story of our past and present (perhaps not even the most important elements). There is a unique history behind secular trends in mortality and survival statistics that, once understood, will provide a full three-dimensional view of the forces that influenced past and current health and longevity attributes of the U.S. population aged 65+, and the factors most likely to influence this age cohort in the future. More importantly, they provide important insights regarding speculation that people are living longer today because they are aging more slowly relative to their age-matched counterparts who lived years earlier.
Population Distribution by Race
In 1965, about 84% of the total population was White, Blacks comprised 12%, Hispanics 3.5%, and all other races represented the remaining 0.5% (Table 1). The United States experienced a rapid transformation in its racial composition to the present day, where Whites now comprise 62.6%, Blacks 12.4%, Hispanics 17.1%, and all other races 7.9% of the total. The most notable change in the U.S. population distribution by race in the year 2040 will be the rise of the Hispanic population—which is expected to comprise 28% of the total population, Blacks will be 14%, Whites 49%, and all other races will be 9% of the total. Hispanics will also occupy an increasing share of the 65+ population in 2040. The relative distribution of the Hispanic population into first-, second-, and third-generational components will be important in understanding their impact on the health and longevity of the 65+ population in 2040.
Table 1.
Demographic and health characteristics of the total United States and 65+ populations
| 1965 | 2010 | 2040 | |
|---|---|---|---|
| Birth era (aged 65–110)a | 1855–1900 | 1905–1950 | 1930–1975 |
| Total U.S. population (in millions)b | 194.3 | 316.1 | 380.0 |
| Population distribution by racec | B 12.0% | B 12.4% | B 14.0% |
| W 84.0% | W 62.6% | W 49.0% | |
| H 3.6% | H 17.1% | H 28.0% | |
| O 0.5% | O 7.9% | O 9.0% | |
| Population aged 65+ (in millions)d | 18.5 | 47.7 | 79.7 |
| Population aged 85+ (in millions) | 1.1 | 6.3 | 14.1 |
| Population aged 100+ | 4000 | 78,000 | 230,000 |
| Proportion of population aged 65+ | 9.5% | 14.8% | 21.0% |
| Proportion of population aged 85+ | 0.6% | 2.0% | 3.7% |
aThese are the years during which members of the 65 and older cohort were born. The entire cohort is contained within the age group 65–110, but the majority of these cohorts were born during the last two decades of each era.
bSource of population statistics for 2014/15 and 2040: U.S. Census Bureau, Table 6, Percent of the Population by Race and Hispanic Origin for the United States: 2015 to 2060, 2012 National Population Projections (U.S. Census Bureau, Population Division, Washington, DC, 2012); www.census.gov/population/projections/data/national/2012.html (accessed October 15, 2014); www.census.gov/population/estimates/nation/popclockest.txt.
cThe “White” population is defined as the “non-Hispanic White” population. Percentages may not add to 100 because of rounding error. The data for 1965 and 2040 are interpolated from the following source that provided estimates only for 1960 and 2050—the percentages are not expected to change much in this short time frame (see thesocietypages.org/socimages/2012/11/14/u-s-racialethnic-demographics-1960-today-and-2050).
d1965 estimated from www.census.gov/prod/99pubs/p23-199.pdf; current and projected from www.census.gov/prod/1/pop/p23-190/p23-190.pdf. 1965, Past; 2010, present; and 2040, future. B, Black; W, White; H, Hispanic; O, other.
Population Distribution by Age
One of the most notable demographic changes in the history of the United States and other developed nations is the absolute increase in the size of the older population. The population aged 65+ in 1965 was 18.5 million, increasing to 47.7 million today, and its projected to rise dramatically to about 80 million by 2040. The primary factor influencing the rise in the population aged 65+ is a shift in the age distribution—that is, larger birth cohorts moving through the age structure. Once the age distribution settles down and the historical blips pass through, the size of the older population is likely to stabilize or slightly increase past 2040. There will also be notable increases in the population aged 85+, rising from 1.1 million in 1965, to 6.3 million today, with a projection of 14.1 million by 2040. The number of centenarians increased from 4000 in 1965 to 78,000 today (Table 1), and the Census Bureau projects there will be about 230,000 centenarians in 2040. All of these estimates for 2040 could rise more rapidly than projected if death rates decline faster than predicted and the reverse is also true—if health conditions worsen for these cohorts, these estimates could be too high.
Life Expectancy
In 1965, life expectancy at birth was only 70.2 yr (Table 2). It rose to 78.8 today, and is projected by the Social Security Administration to rise to 80.5 by 2040. This means the annual rate of change was +0.17 yr annually between 1965 and 2015, and the projected rate of change is expected to decelerate to less than half of that to a +0.07 annual increase between now and 2040. The rise in life expectancy at age 65 is more relevant for this discussion, and here we saw a rise from 14.7 yr in 1965 to 19.3 yr today. The projection for 2040 is only 19.6 yr, which means the U.S. Social Security Administration does not anticipate much of an improvement in duration of life lived at older ages over the next 25 yr.
Table 2.
Life expectancy (in years) at birth and at age 65, and conditional survival to ages 65 and from ages 65 to 85 (United States: 1965, 2010, 2040)
| 1965a | 2010a | 2040b | |
|---|---|---|---|
| Life expectancy at birth | 70.2 | 78.8 | 80.5 |
| Males | 66.8 | 76.4 | 78.5 |
| Females | 73.9 | 81.2 | 82.5 |
| Life expectancy at age 65 | 14.7 | 19.3 | 19.6 |
| Males | 12.9 | 17.9 | 18.4 |
| Females | 16.4 | 20.5 | 20.9 |
| Probability of surviving to age 65 from birth | 71.3% | 84.4% | 87.5% |
| Males | 73.9 | 80.7 | 85.4 |
| Females | 78.9 | 88.1 | 90.2 |
| Probability of surviving to age 85 conditional on survival to age 65 | 28.1% | 50.1% | 50.9 |
| Males | 20.0 | 43.4 | 46.0 |
| Females | 35.1 | 55.7 | 57.6 |
Survival
The story of survival up to and beyond age 65 is similar to that of life expectancy. In 1965, about 71% of all babies born in that year were expected to reach age 65; by 2015, this rose dramatically to over 84% (Table 2). The primary reason for this improvement is a large reduction in death rates at younger ages. By 2040, survival to age 65 is expected to rise to 87.5%, which means the rate of improvement in survival is expected to decelerate rapidly. The reason is the phenomena known as entropy in the life table and competing risks (Olshansky et al. 1990) (discussed in more detail below). Perhaps, more importantly, survival between the ages of 65 and 85 did in fact increase dramatically from 28% in 1965 to 50% today. The marginal expected improvement in survival to age 85 projected for 2040 indicates that, just like life expectancy, the U.S. Social Security Administration does not anticipate much further improvement in survival for the population aged 65+ beyond that already achieved.
Health
Crimmins and Saito (2001) have shown that, from 1970 through 1990, there were varying patterns of healthy life expectancy (HLE) as a function of race and level of completed education. Overall patterns of HLE improved consistently only for those with 13+ years of education; there were some improvements for those who completed 9–12 years of schooling, but among the least educated there was a decline in HLE. More importantly, for the population aged 65 and older, there were vast differences in HLE as a function of completed education—with the most highly educated living several more healthy years relative to the least educated.
LIFE HISTORY OF THE POPULATION AGED 65+ IN 1965
Perhaps the most important thing to keep in mind when discussing the population aged 65+ in different eras is that the people who occupied this age window in the past, those in this age window now, and the people reaching that age window by 2040, are each a by-product of a very unique set of life history characteristics (e.g., cohort events). For example, almost the entire population aged 65 and older in 1965, was born in the 19th century, and most of them were born between 1880 and 1900. When they were children, they had scarce access to anything resembling a vaccination, and most vaccines designed to prevent fatal and disabling diseases, as we know them today, did not exist. Antibiotics had not yet been invented, malnutrition and undernutrition were common, infant mortality rates were as high as 35% in some parts of the country, the primary causes of death were communicable diseases (CVD and cancer were common among only the few who were fortunate enough to survive to older ages), some behavioral risk factors now known to be harmful (e.g., smoking) were considered by some in the medical community as “healthy,” and the foundations of public health (clean water, sanitation, refrigeration, etc.) were just beginning to emerge, and they were inequitably distributed where they did exist (Riley 2001).
For those fortunate enough to survive childhood, the early 20th century brought the hazards of World War I and the 1918 influenza pandemic, and for the survivors of these harsh events, malnutrition and difficult living and working environments plagued this cohort in their adult years. The bottom line is that unforgiving environmental conditions led to early deaths for many children born before 1900 (the oldest members of the population aged 65+ in 1965 were the survivors), and extremely harsh environmental, living and working conditions persisted for this cohort in their first few decades of life.
What are the health and longevity implications of these harsh early life developmental events on the 65 and older population in 1965? The irony is that the relatively few members of the late 19th century birth cohorts fortunate to be alive in 1965 represented the hardiest members of their era. This does not mean they did not get sick, nor does it mean they lived a particularly long life after reaching age 65, it just means that they faced harsh living conditions throughout their lives and they were lucky to have survived. Time and the environment acted as a sieve through which members of their birth cohort passed, so although the population aged 65+ in 1965 still died out at rates that are faster than observed today, that generation should be thought of as a very unique population, the likes of which will probably never be seen again.
LIFE HISTORY OF THE POPULATION AGED 65+ TODAY
The current population aged 65+ was born between 1905 and 1950, with the vast majority born during the decades of the 1930s and 1940s into an entirely different set of environmental and health conditions relative to the 1965 cohort of people aged 65+. They carried with them the advantage of major public health advances developed in the early 20th century, but they were also accompanied by harmful behavioral health practices that elevated their risk of chronic fatal and disabling conditions (e.g., the increased use of tobacco). The rise of Alzheimer’s disease along with cancer, CVD, and sensory impairments, was the price that recent older generations had to pay for their extended survival. However, some subgroups of the current population aged 65+ are also showing signs of improved health in the form of declining frailty and disability.
Almost the entire population aged 65+ today was born between the milestone events of World War I and the first few years of the post-World War II baby boom. On the positive side of the health and longevity equation, these were the first U.S. generations to have broad access to vaccines for yellow fever, typhus, influenza, and polio (among others). Shortly thereafter, younger members of this generation were vaccinated against measles, mumps, and rubella, although it is certain that many among this generation exhibited these diseases before the vaccinations became available. Death and disability often resulted from many of these communicable diseases throughout human history, but in the modern era, survival rates after acquiring some of these diseases improved dramatically. It is unclear at this point whether exhibiting these full-blown communicable diseases early in life conferred any protection from chronic/fatal conditions later in life, or whether they raised the risk of these conditions when older. In the cases of yellow fever, polio, and typhus, we now know that vaccines for these diseases saved millions of lives of people who otherwise would not have lived to ages 65 and older (World Health Organization 2009). It is most certainly the case that a substantial proportion of today’s population aged 65+ would not even be alive had they been raised in the same environmental conditions present during the lives of the 1965 cohort aged 65+.
The infant mortality rate for this generation declined dramatically across the United States relative to previous cohorts as most births occurred in a hospital. After the depression there was widespread availability of food. The education of children spread rapidly and those acquiring a college education increased and the basic principles of public health had already become common, enabling most members of this generation access to clean water, sanitation, refrigeration, and indoor living and working environments. Medical technology advanced rapidly, and, by midcentury, maternal mortality was low as most births took place in the far safer environment of a hospital. The bottom line is that life expectancy rose rapidly during this era as the high force of extrinsic mortality (primarily from communicable diseases) waned in the face of advances in public health and medicine.
However, there were also distinctively harmful conditions that arose during this era that set this generation apart from their predecessors. The 1918 influenza pandemic had a profound (albeit short-term, 2-yr) negative effect on the entire U.S. population, essentially wiping out large segments of both the young and old. Few human generations throughout recorded history went through such a lethal pandemic of this magnitude. A handful of survivors from this pandemic are still alive today (they are now 96+ yr of age).
The current population aged 65+ was also characterized by a high and rapidly growing prevalence of some hazardous behavioral risk factors (e.g., smoking). Although women entering the labor force opened up opportunities for half of this generation, it did not come without risks. The rising prevalence of CVD hit both younger men and women alike among the older members of this cohort, as did the rising prevalence of cancer. However, the younger members of this cohort benefitted from a number of advances in medical diagnosis and care for CVD and cancer that occurred during the last quarter of the 20th century (when CVD mortality declined dramatically and cancer case fatality rates improved).
Overall, today’s population aged 65+ faced a much milder set of environmental conditions throughout their lives relative to the 1965 cohort, and they benefitted from advances in public health and the revolution in medicine in the 20th century. This was the first generation in human history to live through and benefit from the first longevity revolution brought forth by public health and modern medical technology.
The good news in this message is that people 65 and older today live longer than any generation in history, and they experience more healthy years than ever before. The bad news is that this is also the first generation to participate in a dangerous Faustian trade—added years of life (decades for many) in exchange for an increase in the amount of survival time spent in a state of frail health accompanied by a suite of chronic fatal and disabling conditions (Alzheimer’s disease, cancer, CVD, sensory impairments, osteoporosis, osteoarthritis, etc.). Older Americans are most certainly living longer today relative to any time in history, and the absolute number of years spent in a state of good health has expanded with it, but the Faustian trade of an extension of the period of old age must be acknowledged as a by-product of our success in extending life.
The bottom line is that the generation now passing into the age window of 65+ is, overall, much less “selected” out for early death by harsh environmental conditions relative to the generation that preceded them in 1965. Although known for acquiring harmful behavioral risk factors early on, they are also known for abandoning them in favor of improved lifestyles. Today’s generation of people aged 65+ is the most diverse of all older cohorts ever seen in the United States, and this diversity includes not just ethnic diversity and its unique impact on health and duration of life, but, more importantly, the positive extremes of healthy life brought forth by favorable behavioral risk factors (e.g., reductions in the prevalence of smoking and increased education), and the negative extremes of unhealthy life brought forth by harmful behavioral risk factors (e.g., obesity and drug use) and the ability of modern medical technology to postpone death and prolong the period of life at the end where frailty, disability, and health care costs are the highest. It is safe to say that a population of people like this, all of whom have been influenced by a unique set of historical environmental hazards and cohort-specific risk factors that cannot be repeated for cohorts reaching aged 65+ in the future, will never be seen again.
LIFE HISTORY OF THE POPULATION AGED 65+ IN 2040
The characteristics of the populations aged 65+ in 1965 and today each offer unique birth era and lifetime experiences (e.g., cohort effects) that set them apart from any previous generation. As far apart as these generations are, the differences between their birth and life experiences will pale in comparison to how far different the population aged 65+ in 2040 is likely to be relative to today. The discussion will begin with an examination of how the population aged 65+ in 2040 started their lives, but the majority of the discussion to follow will address what conditions could be like in 2040.1
The population aged 65+ in 2040 was born at the dawn of the depression era. They lived through World War II, the Korean War, and the Vietnam War, and the vast majority was born between 1955 and 1975. Most of this cohort (excluding the centenarians and supercentenarians of 2040 born in the 1930s and 1940s), was vaccinated early in life against all major communicable diseases. They benefitted in midlife from unprecedented reductions in CVD in the last quarter of the 20th century brought forth by advances in medical technology; they benefitted in midlife from reductions in cancer case fatality rates; each successive cohort was more highly educated than the last, making them the most highly educated birth cohort in American history; and a sizeable proportion of the original cohort adhered to improvements in some behavioral risk factors (e.g., although the older members of the cohort picked up smoking early in life, later members of the cohort took up smoking with a lower frequency and many decided to quit smoking once the scientific evidence on its harm became compelling). There will be a sizable number of “former smokers” among the population aged 65+ of 2040, and the largest group (both in terms of numbers and percentages) of nonsmokers and people rarely exposed to second-hand tobacco, in history (the latter a by-product of progressive public health efforts across many parts of the nation to ban smoking from indoor environments). This is a very powerful health advantage to this cohort, as it will significantly reduce their risk of lung cancer and related complications associated with exposure to tobacco.
The one major health blemish in the birth cohort that will reach ages 65+ in 2040 is that this generation of adults succumbed to the many forces that contributed to the rise of adult-onset obesity. Unlike smoking, where quitting the habit is possible, obesity is a far more challenging public health problem because people cannot stop eating—we have to form a new relationship with food to successfully combat obesity. This is the reason why most behavioral efforts to combat obesity do not work. Unless this problem is fixed, there is a high probability that levels of frailty and disability associated with obesity and its many complications (especially diabetes, CVD, cancer, joint problems, and depression) will dominate up to 50% or more of older cohorts in 2040 and for many subsequent years. Because medical technology is also likely to become increasingly more efficient in treating diabetes and its complications over the next quarter century (Flegal et al. 2010), the magnitude and duration of frailty and disability among future cohorts of people aged 65+ (in 2040 and beyond) are likely to skyrocket.
Finally, there is one critical demographic fact to keep in mind. Everyone who will fall within the age range of 65+ in 2040 is already alive, and existing survival data (see the Human Mortality Database, www.mortality.org) indicate that most people born in that historical era will survive to at least age 65 (i.e., ∼85% survival). This means the combination of life extension brought forth by declining middle and old age mortality and a rapidly shifting and much older age structure, will produce a dramatic increase in the absolute size of the population aged 65+ in 2040 (to at least 80 million people relative to the estimated 48 million people of that age in the United States today). As a result, genetic heterogeneity will increase among cohorts reaching older ages in the coming decades.
WILL THE POPULATION AGED 65+ IN 2040 LIVE MUCH LONGER THAN TODAY’S GENERATION?
The question of how high life expectancy in the United States can rise (at birth and at older ages) has been the subject of debate for decades. To get a sense of what life expectancy and survival past age 65 will be like in 2040 in the United States, it is important to place our current longevity within the context of history. The rapid increase in life expectancy in the early 20th century was initially because of advances in public health that saved the lives of the young. When the lives of young people are extended, life expectancy rises rapidly because a large number of person-years of life are added to the population—a phenomenon that can only occur once. Once reductions in early age mortality were achieved, future gains in life expectancy must then be a product of reductions in death rates in other (middle and older) regions of the life span. That is exactly what happened.
The United States is now in a position where the only way to significantly increase life expectancy in the future is to generate large reductions in death rates at the oldest ages, and simultaneously push out the envelope of survival into outer regions of the life span (ages 120+) in which only a handful of people have ever lived. That is, large increases in life expectancy at birth in the future require not only large declines in death rates for people aged 65 and older that would have to occur faster and be of a larger magnitude than what was observed in the past for young and middle aged populations (Carnes et al. 2012). It also requires that most people either routinely live past the age of 120, or that a significant segment of the population begin surviving well past the age of 130. Some researchers contend this is exactly what will happen. Vaupel (2010) suggests that advances in biomedical technology yet to be identified or developed, will continue to yield gains in life expectancy in the future on par with patterns of change observed in the past—thus, the rationale for using linear extrapolation to project the future course of mortality and life expectancy.
Other researchers have suggested that there are two reasons why linear extrapolation of life expectancy is inappropriate in long-lived populations. First, it is critical to acknowledge that the biological processes of aging represent the most important risk factor for fatal diseases expressed at older ages (Harman 1991). Although declines in death rates at older ages are possible and even likely in the coming decades, it has been suggested that this approach will yield diminishing returns with regard to gains in life expectancy—a product of competing risks at older ages that accumulate in aging bodies as life expectancy increases. Because it is not yet possible to alter the biological processes of aging, nor is there evidence to suggest that aging has ever been modified in the past, there is no reason to suspect that dramatic declines in death rates among the extreme elderly are plausible. The U.S. Social Security Administration acknowledges this both implicitly and explicitly by forecasting decelerating rates of increase in life expectancy by midcentury (see www.ssa.gov/oact/NOTES/as120/LifeTables_Tbl_6.html).
Second, the age distribution of death in long-lived populations like the United States has already shifted to later ages, but this shift has been characterized by a compression of death into a fairly narrow region between the ages of 65 and 95. There is no evidence that the prospects for surviving past the age of 120 are improving. There is no reason to expect people will routinely live beyond the age of 130 where no human has been documented to live in history; nor is there reason to believe that, in a genetically heterogeneous population, everyone has the potential to live as long as the longest-lived member of the population.
Currently, life expectancy at age 65 in the United States is 17.9 yr for men and 20.5 yr for women (Table 2). The current probability of surviving to age 85 (conditional on having survived to age 65) in 2010 is 43.4% for men and 55.7% for women. According to middle-range forecasts made by the U.S. Social Security Administration, by 2040, life expectancy at age 65 will be 18.4 for men and 20.9 for women. These represent fairly optimistic improvements because it requires large reductions in death rates at older ages to generate just a 1-yr increase in life expectancy at age 65. Conditional survival to age 85 from age 65 in 2040 is expected to rise to 46.0% for men and 57.6% for women (see www.ssa.gov/oact/NOTES/as120/LifeTables_Tbl_6.html)—a very small improvement over the 2010 cohort. Thus, for every 100 people aged 65 in the United States today, about 50 will live to age 85; for every 100 people aged 65 in the United States in 2040, about 51 are expected to live to age 85.
Overall, there is reason to expect that life expectancy and conditional survival in the United States will rise marginally in the coming decades; the rise will be at a much slower pace than that observed in previous decades, and there is no evidence to support any radical increase in life expectancy or survival in the population aged 65+ in the next quarter century. The implications of these observations are straightforward—mortality compression is the most likely scenario going forward, and this, in turn, is expected to be accompanied by a decelerating increase in life expectancy.
Thus, with regard to the “secular aging rate hypothesis,” there are decades worth of definitive research documenting the fact that reductions in death rates at middle and older ages are a direct by-product of improved behavioral risk factors, increasingly more favorable environmental conditions that reduced death rates at older ages, and advances in medical technology that “manufactured” survival time by diagnosing and treating fatal conditions with greater efficiency. There is no direct or indirect evidence favoring the hypothesis that death rates have declined across time because more recent cohorts are aging at a slower pace.
THE ROLE OF DISPARITIES
At one level, there is reason to be optimistic about the future of health and longevity in the United States during the next 25 years. After all, advances in medicine and biomedical technology are occurring rapidly. Genetic engineering offers the promise of curing or controlling some inherited diseases, the prevalence of smoking has declined, educational attainment is increasing, aging science offers the prospect of an extension of youthful vigor—but this is not yet possible, and recent efforts to attack childhood and adult obesity are encouraging. Having said that, it is not possible to ignore some worrisome and potentially disastrous trends in health that have emerged in recent years, such as the rise of childhood obesity, diabetes, and their complications. The latent effects of these trends will not be seen for decades, which means that by 2040 we could very well witness the long-term negative effect of these trends on the population reaching older ages of the acquisition of harmful behavioral risk factors that were acquired in childhood. Childhood and adult-onset obesity represent the most worrisome health trends at the moment.
There is a tendency in medicine and public health to focus only on what is happening at the national level, and this is understandable given the need to summarize health statistics in a succinct way. However, beneath the surface of national vital statistics is an alarming persistent divide among subgroups within the United States that has been known for decades (Kitagawa and Hauser 1973), and which are invisible when the focus is just on life expectancy, survival, and health for the nation as a whole. These disparities persist even when some major causes of differential survival among the subgroups are eliminated (Lantz et al. 1998; Link and Phelan 2005). Health disparities reflect racial and ethnic differences in addition to variation in education and income that are linked directly and indirectly to behavioral risk factors (Adler et al. 1999), and it has even been proposed that social conditions can be “fundamental causes” of health inequalities, which is why interventions based exclusively on modifying biomedical risk factors have not been, and are not likely to be, successful in substantially reducing health disparities (Link and Phelan 2005). This concept of “fundamental causes” can be interpreted, in part, as variations in the rate at which biological aging is experienced, but in the absence of reliable biomarkers of aging, it is not yet possible to know with certainty whether variation in biological aging causes disparities.
Measures of health disparities as we gauge them today, did not exist in 1965, but Kitagawa and Hauser (1973) documented shortly thereafter that income, education, and occupation (among other socioeconomic status variables) modulate the dramatic variation in longevity and health that existed within the United States at that time. To understand the magnitude and importance of disparities, consider the fact that, in 2008, a White female that acquired a college education could expect to live 10 yr longer than a White female with less than 12 yr of education. To gain an understanding of the magnitude of this difference, relative to someone without a high school degree, a college education is equivalent to taking a pill that cures all CVD and cancer (Beltrán-Sánchez et al. 2008).
A difference in life expectancy of 1 yr is large; a difference of 10 yr means the person with the lower life expectancy is living in the equivalent of the early 20th century. This does not mean people in the modern era are aging more slowly, it just means that in 1900 there were many more risk factors for fatal diseases. Data from the MacArthur Research Network on an Aging Society has shown that these disparities in longevity also apply to the population aged 65 and older (Olshansky et al. 2012)—a particularly notable finding that has important implications for cohorts reaching older ages in the future. This means close attention should be paid to the physical and mental health status and racial composition of younger generations now moving through the age structure because it is these generations that will enter the 65+ age window by 2040.
Furthermore, it is worth noting that, in 2008, the effect of education on the proportion of the population that survived to age 65 (conditional on having survived to age 25) was dramatic for all race–sex groups with the exception of Hispanic females (Table 3). For example, note that among White males with <12 yr of education, only 61.3% of those reaching the age of 25 are expected to survive to age 65. By comparison, 91% of White males with a college education are expected to reach age 65. Education currently has less of an effect on Hispanic men and woman (the longest-lived subgroup in the United States today) because of a phenomenon known as the Hispanic paradox (discussed below).
Table 3.
Proportion surviving to age 65 conditional on having survived to age 25 by sex, race, and level of completed education in the United States in 2008
| Years of school completed | ||||
|---|---|---|---|---|
| <12 | 12 | 13–15 | 16+ | |
| White males | 61.3 | 73.2 | 86.4 | 91.0 |
| White females | 72.8 | 84.1 | 91.9 | 93.8 |
| Black males | 59.8 | 63.6 | 80.5 | 84.5 |
| Black females | 73.1 | 76.9 | 86.6 | 88.4 |
| Hispanic males | 83.5 | 81.8 | 89.6 | 92.2 |
| Hispanic females | 90.6 | 90.2 | 94.0 | 95.0 |
Unpublished data from research conducted for the MacArthur Research Network on an Aging Society. (Related data from the same life tables were published in Olshansky et al. 2012 and reprinted here, with permission, from the author.)
SHIFTING DEMOGRAPHICS—THE HISPANIC PARADOX AND OLD AGE MORTALITY IN THE FUTURE
When rapid increases in longevity combined with declining fertility in the latter part of the 20th century, the U.S. age structure began shifting to a more rectilinear form. By 2040, the age structure of the United States and all other developed nations will be in the shape of a square or nearly so, with at least as many people alive at older ages as there are at younger ages. This new shape to the U.S. age structure is likely to be a permanent feature of our population for the foreseeable future. However, beneath the surface of a visibly shifting age structure are forthcoming changes to our demographics that will alter the course of American health and longevity by 2040, especially among future cohorts of older people. Three major events are unfolding now.
First, there is evidence to suggest that subgroups of the U.S. population are experiencing significantly different health trajectories (Olshansky et al. 2012). Although the least educated among us are a slowly shrinking segment of the population, being less educated today is far more lethal now than it was just two decades ago. This trend will not have a profound influence on national vital statistics because the proportion of the total population that falls into this category is relatively small and shrinking, but it will be a health challenge nonetheless for a number of people reaching older ages in the years 2040 and beyond.
A second factor that will influence the age structure in this century are advances in public health and the biomedical sciences that are likely to yield improvements in health and longevity. Included among them are continued efforts to reduce smoking prevalence, greater success in the treatment of complications associated with obesity, traction beginning in the battle against the rise of childhood obesity, and anticipated advances in aging science that could yield an extension of healthy life by 2040. It is unclear exactly how these positive developments will manifest over the next 25 years, but the most likely scenario is that the one subgroup likely to benefit first will be those with the highest education, highest income, and overall highest socioeconomic status.
Finally, one of the more interesting developments in shifting American demographics is the anticipated dramatic increase in the Hispanic population, and the unique impact this will have on health and longevity over the next few decades (Table 1). Details of this event are addressed by Hummer and Hayward (2015), but for now it is important to recognize that the proportion of the total U.S. population that is Hispanic will rise from 17.1% today to 28% by 2040. More important, Hispanics now represent only 7% of the population aged 65+, but this will rise to 18% by 2040. Neither of these demographic events would ordinarily be notable, except for the fact that Hispanics represent perhaps one of the more interesting anomalies in American demographics.
Hispanics currently have the highest life expectancy among the main population subgroups in the United States today. Hummer and Hayward (2015) have shown that this is because of the fact that the Hispanic population in the United States today is currently dominated by first-generation immigrants who are known to have healthier lifestyles than either their country of origin or the general U.S. population. This has led to what is commonly known as the Hispanic paradox (Markides et al. 2015)—the unexpected observation that Hispanic immigrants currently live longer than the resident population.
What makes the Hispanic impact on American demographics even more interesting is the likelihood that the health and longevity of this subgroup is on a trajectory to worsen in the coming decades. Why? Because evidence has emerged to indicate that second- and third-generation Hispanics are experiencing notable declines in health caused by the acquisition of increasingly more harmful behavioral risk factors such as smoking and obesity (Hayward et al. 2014). Thus, because Hispanics are about to noticeably increase their presence as part of American demographics, and their future health and longevity trajectory is spiraling downward, there is reason to believe that this will have a notable negative impact on the life and health expectancy of all Medicare-eligible cohorts between now and 2040.
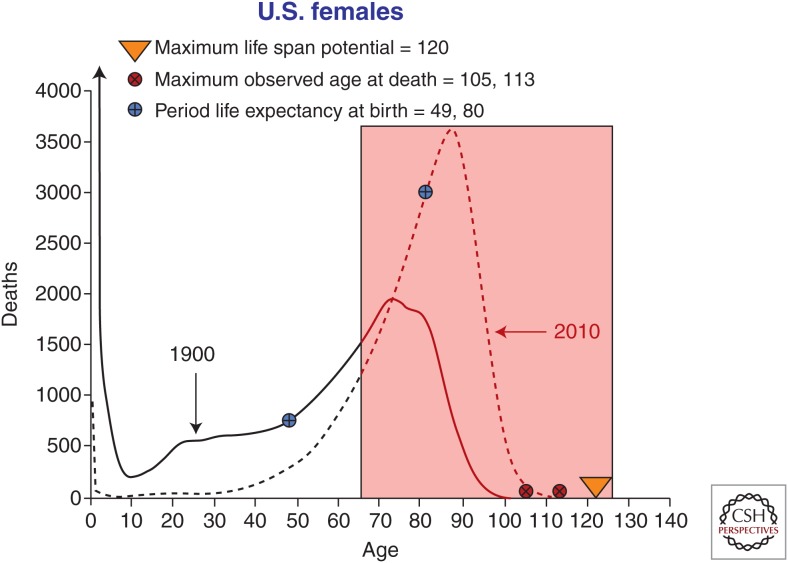
COMPETING RISKS
One of the most important concepts in the field of aging science, which is also either unknown or misunderstood by many, is referred to as “competing risks,” and it will have a profound influence on the prospects for both life expectancy and healthy life span for the older population in this century (current and future cohorts). Imagine a cohort of 100,000 female babies born in selected years in the United States, say, in 1900 and 2010. If one applied the observed death rates in those years to these hypothetical babies and plotted out the ages they would all die based on those death rates, one would observe the “age distribution of death” (see Fig. 1).
Figure 1.
Age distribution of death, period life expectancy at birth, maximum observed age at death, and maximum life span potential for U.S. females in 1900 and 2010. The red shaded box is the “red zone”—an age window in which it becomes increasingly more difficult to influence both length and quality of life. (Image prepared by author based on survival data from the d(x) column of life tables kindly provided to the author by Dr. Steven Goss, Chief Actuary of the U.S. Social Security Administration.)
Note that, in 1900, the death distribution was skewed toward younger ages—this reflects the high infant, child, and maternal mortality observed in that year. However, even in 1900, once individuals survived past the first few years of life, most deaths were then distributed between the ages of 50 and 85 (solid black line). During the course of the 20th century, death rates declined dramatically at younger ages, enabling people who in 1900 would ordinarily have died early in life, an opportunity to survive up to and beyond the age of 65 with regularity. The dashed line illustrates what the distribution of death looks like today. Based on past, current, and projected period life tables, we now know that a female baby born in 1965 had a 78.9% chance of reaching their 65th birthday; today that probability is over 88%, and by 2040 it has been estimated by the U.S. Social Security Administration that >90% will survive to their 65th birthday. However, because death rates are now so low in the United States before age 65, there is not much room left for improvement in survival to this age. This is why the rise in the proportion of the population expected to reach older ages in the future is not going to be far different from what is observed today—it is difficult to improve on a mortality profile that is already so favorable before age 65.
So what exactly are competing risks and why are they important? When death occurred at younger ages in the early 20th century, it was largely a product of communicable diseases. Now that most deaths have been redistributed to the 65+ age window, the price to be paid for extended survival is a dramatic rise in the prevalence of diseases of aging—CVD, cancer, Alzheimer’s disease, dementia, and a suite of nonfatal disabling conditions (sensory impairments, osteoporosis, osteoarthritis, etc.). No one would dispute that the trade-off of chronic aging-related diseases for a longer life was worth it, but nonetheless, it was a Faustian trade that people in the modern era have to live with from now on.
Here is the dilemma. Now that most deaths occur past the age of 65, and given that it is not currently possible to modulate or even measure the rate of biological aging, what is happening in the United States and in other long-lived populations is that older people are now routinely accumulating a broad range of fatal and disabling diseases in their bodies. The longer we live, the more diseases we accumulate. It is as if fatal aging-related diseases are “competing” for our lives in some sort of perverse death battle. If medical technology heroically saves the life of an older person, which happens with regularity, that person lives a bit longer, only to face the next cause of death that is competing for their life.
Because death is a zero sum game, when any one cause of death declines (for whatever reason, including either advances in medical technology or improved behavioral risk factors, such as reductions in smoking or the adoption of a healthy lifestyle), the risk of some other fatal condition must eventually rise! Although there is variability in the severity of fatal and disabling conditions across all older cohorts, the population aged 65+ share one important attribute—they have all experienced at least 65 years of the ravages of biological aging on their bodies. This is the reason why some researchers in the field of aging have suggested that long-lived populations like the United States have reached a point of diminishing returns regarding the rise in life expectancy, the probability of reaching the age of 65, and the probability of reaching older ages conditional on having reached the age of 65 (Olshansky et al. 1990). There just is not much room for significant additional improvement in survival until and unless it becomes possible to alter the biological processes of aging and successfully disseminate a therapeutic intervention that accomplishes this. Using a running analogy, although a number of people have broken the 4-minute mile since this record was first breached in 1954, improvements in running speed have decelerated dramatically since then because of limitations imposed by body design—in the absence of genetically fixed programs that could preclude faster running times.
Thus, there are two reasons why the concept of competing causes is so important to the future of survival and the prospect that the aging rate has already been modified. First and foremost, there is no reason to expect any dramatic improvement in survival to the population aged 65+ between now and 2040. Even the Social Security Administration anticipates no more than a 3.1% improvement in survival to age 65 between now and 2040, and that is with a fairly optimistic set of assumptions about anticipated future declines in death rates before age 65 over the next 25 years. Conditional survival to age 85 from age 65 is also not expected to change much by 2040 for the same reason. This does not mean the absolute number of people reaching ages 65 and 85 will not rise rapidly—that is an inevitable by-product of a shifting age structure.
Once one understands the basic demographics of population shifts and entropy in the life table, you can put to rest the idea that any dramatic improvement in life expectancy or survival is forthcoming. Although some in the field of aging would disagree with this (Vaupel 2010), it is suggested here that these views are overly optimistic (unrealistic to some) because they fail to take into account anything more than the extrapolation of historical trends into the future, including our basic biology—which precludes extended survival for most people (Carnes et al. 2012; Olshansky 2013).
The second reason why competing causes is so important is perhaps even more intriguing. Note the red shaded box in the age window of 65+ in Figure 1. This is referred to as the “red zone”—an age window in which it becomes increasingly more difficult to influence both length and quality of life. Importantly, the longer we live, the more difficult it becomes to intervene in any positive way. In fact, to the contrary, I contend that if we continue with current efforts to extend life (even marginally) by combatting only major fatal diseases (consider CVD and cancer as our primary targets), we will probably achieve some additional measure of success in reducing case fatality rates for these competing causes, but the price to be paid for success may very well be an expansion of morbidity and a rise in other competing causes that yield more years of frailty and disability. In other words, the current medical model that is designed to forestall death from fatal conditions may yield marginal additional survival time, but it is distinctly possible that the trade-off will be an increase in the number and severity of unhealthy years. Why? Because treatments for major fatal diseases leave unaltered the basic biological processes of aging that give rise to most diseases competing for our lives in the red zone.
To be clear, biological aging gives rise to an increased risk of fatal diseases because aging is the primary risk factor for competing causes, but medicine and current medical technology does not “treat” aging, it addresses only its consequences. This is the reason why a large number of researchers in the field of aging are now suggesting that the time has arrived to attack biological aging itself rather than just its disease manifestations (Miller 2002; Olshansky et al. 2006; Butler et al. 2008; Sierra et al. 2009; Goldman et al. 2013; Kirkland 2013). Unless successful in this effort, the United States and other long-lived populations run the risk that, by midcentury, the population reaching ages 65+ in the coming decades could (overall) experience higher levels of frailty and disability associated with Alzheimer’s disease and nonfatal disabling conditions associated with aging. The irony is that this unwelcome scenario would be a product of success, not failure, in combatting major fatal diseases.
CONCLUSIONS
Is there empirical evidence to support the “secular aging rate hypothesis”? That is, have successive generations passing through the same age window experienced declining mortality and extended lives because they are aging more slowly? The absence of definitive biomarkers of aging makes it impossible to empirically test this hypothesis. But evidence presented here shows that death rates have been declining and life expectancy has been rising among older people because of a combination of improved behavioral risk factors (e.g., declines in smoking), advances in medical technology that detect and postpone the onset and age progression of major fatal diseases more efficiently, and because of vastly improved environmental conditions under which people were born and lived their lives. There is no empirical evidence anywhere in the scientific literature to suggest or even intimate that the cause of secular declines in death rates (and rising life expectancy) at middle and older ages are a product of improvements in the rate of biological aging among successive generations across time. It is important to emphasize again that the observed death rate in a population is not a measure of biological aging.
Is there empirical evidence to support the “comparative aging rate hypothesis,” suggesting that subgroups of the population age at different rates in a single time period? This is somewhat more complicated. In the absence of a definitive measure of the rate at which biological aging is occurring in individuals, despite alleged biomarkers of aging being measured from National Health and Nutrition Examination Survey (NHANES) data, this is currently unknowable. However, there is evidence to suggest that the lifelong accumulation of stress associated with social disadvantage, leads to a measurable accelerated shortening of telomeres (Epel et al. 2004)—one of the potential biomarkers of human aging that may be associated with rate of biological aging. Given that survival rates and the risk of major fatal conditions occur routinely at younger ages for disadvantaged subgroups of the population, the hypothesis by Levine and Crimmins (2014) that shorter-lived subgroups may experience higher death rates because they are aging more rapidly is plausible but currently immeasurable. It is important to recognize that such a hypothesis does not mean that population subgroups are destined to die earlier or live longer than others, it just means that it appears likely that behavioral and environmental risk factors have the potential to accelerate biological aging at the individual level. There are no documented methods of decelerating biological aging as yet, although researchers may be closing in on therapeutic interventions that will do just this (Kirkland 2013), but there are likely to be a large number of aging accelerators (exposure to ionizing radiation, pollutants, possible obesity, etc.). This is the reason why the “comparative aging rate hypothesis” seems plausible, whereas the “secular aging rate hypothesis” does not.
Is there empirical evidence to support the “heterogeneity aging rate hypothesis” that long-lived people and their offspring experience lower mortality and greater longevity because they possess “protective genes” that enable them to escape or delay the ravages of time more efficiently than the rest of the population? Once again, it is not yet possible for anyone to measure the rate of biological aging in individuals, but evidence from empirical research has documented the powerful effect of genetics on survival and mortality (Kirkwood and Austad 2000; Perls 2003). Given the often harmful behavioral habits practiced by many documented centenarians and supercentenarians (Perls and Silver 2008), there is reason to believe that something is protecting them from harmful risk factors that kill most other people at younger ages. It would be difficult to posit anything other than a strong genetic influence on mortality risk, so the “heterogeneity aging rate hypothesis” seems likely.
To summarize, empirical evidence shows that, during the last 115 years, people in general are living longer and healthier lives than at any time in history. The majority of the rise in longevity in the last century is a by-product of declining early age mortality brought forth by public health advances that reduced the risk of death from communicable diseases—a by-product of forces that were external to human bodies. Declines in death rates at middle and older ages since 1965 are largely a product of improved behavior risk factors and advances in medical technology that successfully manufactured survival time that would not otherwise have been possible. There is no evidence to support the hypothesis that people are living longer today because they are aging more slowly than earlier generations. The fact that genetic heterogeneity influences variation in human longevity lends credence to the “comparative aging rate hypothesis” and the “heterogeneity aging rate hypothesis” because their premise is that genetic variation drives mortality risk differentials—a fact well documented in the literature. This conclusion also opens up the door to promising therapeutic interventions designed to slow aging because such interventions would be fundamentally based on leveraging the genetic advantages for health and longevity that already exist among population subgroups.
The difference between a projection and a forecast is that the former is a hypothetical scenario of what might be, and the latter is a scenario that the investigator actually believes will transpire. Because the population aged 65+ in 2040 has already been born and much is known about their early life conditions, the following discussion of health and longevity conditions for this cohort should be viewed as a forecast.
Editors: S. Jay Olshansky, George M. Martin, and James L. Kirkland
Additional Perspectives on Aging available at www.perspectivesinmedicine.org
REFERENCES
- Adler NE, Marmot M, McEwen BS, Stewart J. eds. 1999. Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways. New York Academy of Sciences, New York. [PubMed] [Google Scholar]
- Atzmon G, Rincon M, Rabizadeh P, Barzilai N. 2005. Biological evidence for inheritance of exceptional longevity. Mech Ageing Dev 126: 341–345. [DOI] [PubMed] [Google Scholar]
- Baker GT, Sprott RL. 1988. Biomarkers of aging. Exp Gerontol 23: 223–239. [DOI] [PubMed] [Google Scholar]
- Beltrán-Sánchez H, Preston SH, Canudas-Romo V. 2008. An integrated approach to cause-of-death analysis: Cause-deleted life tables and decompositions of life expectancy. Demogr Res 19: 1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler RN, Miller RA, Perry D, Carnes BA, Williams TF, Cassel C, Brody J, Bernard MA, Partridge L, Kirkwood T, et al. 2008. New model of health promotion and disease prevention for the 21st century. BMJ 337: a399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnes BA, Olshansky SJ, Hayflick L. 2012. Can human biology allow most of us to become centenarians? J Gerontol A Biol Sci Med Sci 68: 136–142. [DOI] [PubMed] [Google Scholar]
- Crimmins E, Saito Y. 2001. Trends in healthy life expectancy in the United States, 1970–1990: Gender, racial, and educational differences. Soc Sci Med 52: 1629–1641. [DOI] [PubMed] [Google Scholar]
- Epel ES, Blackburn EH, Lin J, Dhabhar FS, Adler NA, Morrow JD, Cawthon RM. 2004. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci 101: 17312–17315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Ogden CL, Yanovski JA, Freedman DS, Shepherd JA, Graubard BI, Borrud LG. 2010. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr 91: 1020–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman DP, Cutler D, Rowe JW, Michaud PC, Sullivan J, Peneva D, Olshansky SJ. 2013. Substantial health and economic returns from delayed aging may warrant a new focus for medical research. Health Aff (Millwood) 32: 1698–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harman D. 1991. The aging process: Major risk factor for disease and death. Proc Natl Acad Sci 88: 5360–5363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward MD, Hummer RA, Chiu C, Gonzalez-Gonzalez C, Wong R. 2014. Does the Hispanic paradox in U.S. adult mortality extend to disability? Popul Res Policy Rev 33: 81–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer RA, Hayward MD. 2015. Hispanic older adult health and longevity in the United States: Current patterns and concerns for the future. Daedalus 144: 20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsella KG. 1992. Changes in life expectancy 1900–1990. Am J Clin Nutr 55: 1196S–1202S. [DOI] [PubMed] [Google Scholar]
- Kirkland JL. 2013. Translating advances from the basic biology of aging into clinical application. Exp Gerontol 48: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkwood TB, Austad SN. 2000. Why do we age? Nature 408: 233–238. [DOI] [PubMed] [Google Scholar]
- Kitagawa EM, Hauser PM. 1973. Differential mortality in the United States: A study in socioeconomic epidemiology. Harvard University Press, Cambridge, MA. [Google Scholar]
- Lantz PM, House JS, Lepowski JM, Williams DR, Mero RP, Chen J, 1998. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of US adults. JAMA 279: 1703–1708. [DOI] [PubMed] [Google Scholar]
- Levine ME, Crimmins E. 2014. Evidence of accelerated aging among African Americans and its implications for mortality. Soc Sci Med 118: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan JC. 2005. Fundamental sources of health inequalities. In Policy challenges in modern health care (ed. Mechanic D, et al. ), pp. 71–84. Rutgers University Press, New Brunswick, NJ. [Google Scholar]
- Ludwig FC, Smoke ME. 1980. The measurement of biological age. Exp Aging Res 6: 497–522. [DOI] [PubMed] [Google Scholar]
- Markides KS, Samper-Terment R, Al Snih S. 2015. Aging and health in Mexican Americans: Selected findings from the Hispanic EPESE. In Race and social problems, pp. 171–186. Springer, New York. [Google Scholar]
- Miller RA. 2002. Extending life: Scientific prospects and political obstacles. Milbank Q 80: 155–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky SJ. 2013. Can a lot more people live to one hundred and what if they did? Accid Anal Prev 61: 141–145. [DOI] [PubMed] [Google Scholar]
- Olshansky SJ, Carnes BA, Cassel C. 1990. In search of Methuselah: Estimating the upper limits to human longevity. Science 250: 634–640. [DOI] [PubMed] [Google Scholar]
- Olshansky SJ, Perry D, Miller RA, Butler RN. 2006. In pursuit of the longevity dividend. The Scientist 20: 28–36. [Google Scholar]
- Olshansky SJ, Hayflick L, Carnes BA. 2008. No truth to the fountain of youth. Sci Am 14: 98–102. [DOI] [PubMed] [Google Scholar]
- Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, Carnes BA, Carstensen LL, Fried LP, Goldman DP, et al. 2012. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood) 31: 1803–1813. [DOI] [PubMed] [Google Scholar]
- Perls T. 2003. Genetics of exceptional longevity. Exp Gerontol 38: 725–730. [DOI] [PubMed] [Google Scholar]
- Perls TT, Silver MH. 2008. Living to 100. Basic Books, New York. [Google Scholar]
- Perls TT, Wilmoth J, Levenson R, Drinkwater M, Cohen M, Bogan H, Joyce E, Brewster S, Kunkel L, Puca A. 2002. Life-long sustained mortality advantage of siblings of centenarians. Proc Natl Acad Sci 99: 8442–8447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley JC. 2001. Rising life expectancy: A global history. Cambridge University Press, New York. [Google Scholar]
- Sierra F, Hadley E, Suzman R, Hodes R. 2009. Prospects for life span extension. Annu Rev Med 60: 457–469. [DOI] [PubMed] [Google Scholar]
- Vaupel JW. 2010. Biodemography of human ageing. Nature 464: 536–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaupel J, Lundstrom H. 1994. Longer life expectancy? Evidence from Sweden of reductions in mortality rates at advanced ages. In Studies in the economics of aging (ed. Wise DA), pp. 79–102. University of Chicago Press, Chicago. [Google Scholar]
- World Health Organization. 2009. State of the world’s vaccines and immunization, 3rd ed. World Health Organization, Geneva. [Google Scholar]