Abstract
A 44-year-old woman with a history of dysmenorrhea, obstipation, and low back pain was investigated for gynecological disorder. Physical examination indicated a “frozen pelvis”. Ultrasound examination revealed the ovaries adherent to the uterus, bilateral ovarian cysts, and an intrauterine contraceptive device in situ, which reportedly had been in place for 19 years. Prior to a scheduled laparoscopy, the patient returned with oedema of the lower abdomen and legs, fatigue, and weight loss. Laboratory findings included elevated CA-125, anemia, leucocytosis and high C-reactive protein. Pelvic actinomycosis was subsequently diagnosed. We report the PET/CT appearance of this condition.
Keywords: FDG, PET/CT; intrauterine device; actinomycosis; frozen pelvis
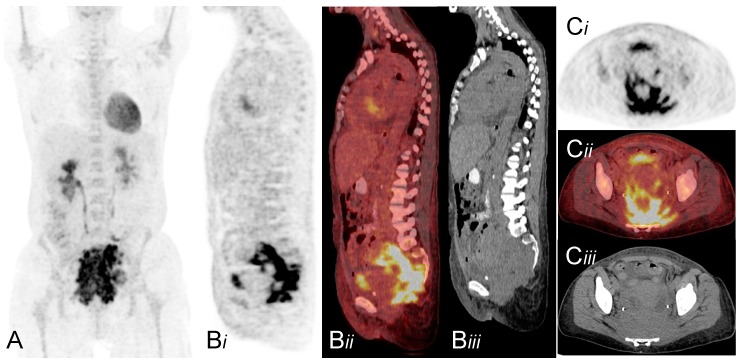
Figure 1.
A 44-year old woman with several months’ history of dysmenorrhea, obstipation, and low back pain was examined. The patient’s history and ultrasonographic findings, with the ovaries adherent to the uterus and possible endometriomas, were suggestive of endometriosis. Additionally, an intrauterine device (IUD) was in place, which had not been replaced in 19 years. Six weeks after the initial consultation, the patient returned with oedema of the lower abdomen and legs, weight loss, and fatigue. The IUD had been removed. Laboratory findings showed erythropenia, leucocytosis, elevated C-reactive protein, and creatinine. Renography showed bilateral urinary tract obstruction and JJ-catheters were implanted. An F-18 fluoro-deoxyglucose (FDG) PET/CT scan with oral but no intravenous contrast, primarily planned to rule out ovarian carcinoma, was performed. PET-CT (A Maximum intensity projection. Bi-iii Sagittal projection; PET, fused and CT scan respectively. Ci-iii Transverse projection; PET, fused and CT scan respectively) revealed a diffusely infiltrative, FDG-avid (SUVmax 18, 0), pelvic mass mainly located in the pre-sacral region extending around the vagina, the intestines and through the greater sciatic foramen intermuscularly on the left side (Ci, Cii, arrow). Subcutaneous oedema of the lower part of the body is seen on CT (Biii, Ciii). The red bone marrow is seen with diffuse high uptake consistent with anemia and infection (A). Based on PET/CT findings alone, no definite diagnosis was possible and malignancy could not be ruled out. Furthermore, the interpretation on the CT scan was compromised due to the absence of intravenous contrast. Actinomycosis was diagnosed by endometrial histology. The patient was treated successfully with high dose intravenous benzylpenicillin and no surgery was required. Actinomyces species are slow-growing, Gram-positive, anaerobic bacteria [1]. Pelvic actinomycosis infection is rare and often associated with IUD in women [2,3,4]. Actinomycosis yields a characteristic granulomatous response with abscess formation, necrosis, and reactive fibrosis with a sub-acute-to-chronic course [3,4,5,6]. Advanced pelvic actinomycosis with formation of solid masses can be difficult to differentiate from pelvic neoplasia, such as ovarian carcinoma, as it can compress nearby structures, as well as invade surrounding tissue [3,5,7,8]. The disease has multiple clinical presentations and non-specific CT findings [4,9] and can lead to extensive surgery before correctly diagnosed [6]. As demonstrated by our F-18 FDG PET/CT scan and previously described cases [4,9], pelvic actinomycosis is an important differential diagnosis in imaging when presented with an infiltrative mass with a tendency to invade across tissue boundaries. This is especially true in women with a history of IUD and signs of infection.
Author Contributions
Conception: Danijela Dejanović; Design: Danijela Dejanović, Jan Anders Ahnlide, Cecilia Nilsson, Anne Kiil Berthelsen, Annika Loft; Analysis and interpretation: Danijela Dejanović, Jan Anders Ahnlide, Cecilia Nilsson, Anne Kiil Berthelsen, Annika Loft; Drafting: Danijela Dejanović; Approval and agreement: Danijela Dejanović, Jan Anders Ahnlide, Cecilia Nilsson, Anne Kiil Berthelsen, Annika Loft.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Garner J.P., Macdonald M., Kumar P.K. Abdominal actinomycosis. Int. J. Surg. 2007;5:441–448. doi: 10.1016/j.ijsu.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Fiorino A.S. Intrauterine contraceptive device-associated actinomycotic abscess and Actinomyces detection on cervical smear. Obstet. Gynecol. 1996;87:142–149. doi: 10.1016/0029-7844(95)00350-9. [DOI] [PubMed] [Google Scholar]
- 3.Kumar N., Das P., Kumar D., Kriplani A., Ray R. Pelvic actinomycosis mimicking: An advanced ovarian cancer. Indian J. Pathol. Microbiol. 2010;53:164–165. doi: 10.4103/0377-4929.59216. [DOI] [PubMed] [Google Scholar]
- 4.Lely R.J., van Es H.W. Case 85: Pelvic actinomycosis in association with an intrauterine device. Radiology. 2005;236:492–494. doi: 10.1148/radiol.2362031034. [DOI] [PubMed] [Google Scholar]
- 5.Akhan S.E., Dogan Y., Akhan S., Iyibozkurt A.C., Topuz S., Yalcin O. Pelvic actinomycosis mimicking ovarian malignancy: Three cases. Eur. J. Gynaecol. Oncol. 2008;29:294–297. [PubMed] [Google Scholar]
- 6.Weese W.C., Smith I.M. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic ‘failure’ with good prognosis after treatment. Arch. Intern. Med. 1975;135:1562–1568. doi: 10.1001/archinte.1975.00330120040006. [DOI] [PubMed] [Google Scholar]
- 7.Hoffman M.S., Roberts W.S., Solomon P., Gunasekarin S., Cavanagh D. Advanced actinomycotic pelvic inflammatory disease simulating gynecologic malignancy. A report of two cases. J. Reprod. Med. 1991;36:543–545. [PubMed] [Google Scholar]
- 8.Koshiyama M., Yoshida M., Fujii H., Nanno H., Hayashi M., Tauchi K., Kaji Y. Ovarian actinomycosis complicated by diabetes mellitus simulating an advanced ovarian carcinoma. Eur. J. Obstet. Gynecol. Reprod. Biol. 1999;87:95–99. doi: 10.1016/S0301-2115(99)00083-4. [DOI] [PubMed] [Google Scholar]
- 9.Ha H.K., Lee H.J., Kim H., Ro H.J., Park Y.H., Cha S.J., Shinn K.S. Abdominal actinomycosis: CT findings in 10 patients. AJR Am. J. Roentgenol. 1993;161:791–794. doi: 10.2214/ajr.161.4.8372760. [DOI] [PubMed] [Google Scholar]