Abstract
Background
The objective of the present study was to determine the prevalence and severity of dental fluorosis and to evaluate exposure to fluoridated products in students in the southwest part of the Federal District (Mexico City).
Material/Methods
Students between 10 and 12 years of age who were born and raised in the study zone were evaluated. The level of dental fluorosis was determined using the modified Dean index (DI) using criteria recommended by the World Health Organization (WHO). A bivariate analysis was performed with the χ2 test, and odds ratios (OR) and 95% confidence intervals (CI) are presented. Logistic regression was performed to evaluate the association between dental fluorosis and the independent variables.
Results
A total of 239 students were evaluated. Their mean age was 11±0.82 years, and there were 122 (51%) males. Overall, dental fluorosis was found in 59% of participants; 29.3% had very mild fluorosis, 20.9% had mild fluorosis, 6.7% had moderate fluorosis, and 2.1% had severe fluorosis. The mean fluorosis score was 0.887±0.956. In the final logistic regression model, dental fluorosis was significantly associated with frequency of brushing (OR: 0.444; 95% CI: 0.297–0.666) and with the absence of parental supervision (OR: 0.636; 95% CI: 0.525–0.771).
Conclusions
The association found with frequency of brushing and lack of parental supervision may be contributing to the prevalence and severity of dental fluorosis.
MeSH Keywords: Fluorosis, Dental; Mexico; Toothbrushing
Background
In recent decades, with the objective of preventing dental cavities, multiple topical and systemic fluorides have been incorporated into different diet products. The administration or ingestion of excessive fluorides leads to toxicity and causes the secondary effect of dental fluorosis [1]. Dental fluorosis is a disorder that begins in the odontogenesis stage when the teeth are forming, and the clinical manifestations of this disease are more evident in permanent dentition [2].
Clinically, dental fluorosis is characterized by stains that are white, opaque, and do not have the shine of enamel; the teeth can be striated or spotted, and extrinsic stains may be between yellow and dark brown. The affected dental organs can present greatly accentuated perikymata. More severe cases show disconnected pits and zones of hypoplasia in the enamel, which can cause the tooth to lose its normal morphology [3].
The frequency and severity of the lesion increase as the ingestion of fluoride in the water increases above 0.7 ppm; in Mexico, this level is recommended to achieve a beneficial effect in the prevention of dental cavities due to the warm climate in Mexico, which leads the population to ingest a greater quantity of liquids [3].
In 1993, the fluoridation of salt was incorporated at the national level; the Federal District and all of its delegations were considered for the consumption of fluoridated salt. Other municipalities in Mexico with natural concentrations of water fluoride above 0.7 ppm were not given fluoridated salt, with the goal of protecting the population from dental fluorosis [3,4].
In addition to fluoridated salt, the majority of toothpastes contain fluorides in various formulations, and it is also found in commercial mouthwashes and other fluoridated products to which the population has free access. The use of fluoridated toothpastes in stages of dental formation increases the risk of dental fluorosis, especially when excessive quantities of toothpaste are used on the brush and the concentration of the toothpaste is above the recommended pediatric dose (500 ppm). Studies have identified toothpaste as an important source of fluoride for children [6,7].
For the past 10 years, there have been reports of dental fluorosis in areas of the Federal District despite the low natural concentrations of fluoride in the water [8,9].
Due to the lack of knowledge of the possible causes of the prevalence and severity of dental fluorosis in an area with low fluoride concentration in the water, this study was performed to identify risk factors in addition to fluoridated salt among students who live in a zone in the southwest part of the Federal District.
Material and Methods
Study design
An observational, cross-sectional, descriptive study was performed among students in the municipality of Tláhuac in southeast Mexico City. The investigation was conducted among students between 10 and 12 years of age because they have nearly completed their permanent dentition and are in primary school.
This study was approved by the research commission of the Division of Biological Sciences and Health of the Autonomous Metropolitan University, Xochimilco Campus.
The study zone is characterized by families of low socioeconomic status, regular and irregular settlements, and a population of more than 23 280 inhabitants, of which 8% are illiterate. In the municipality, more than 3.4% of the children do not go to primary school, according to data from the National Institute of Statistics and Geography (INEGI) [10]. Tláhuac is located at 2235 meters above sea level and has a mean annual temperature of 15.7°C, with a minimum of 8.3°C and a maximum of 22.8°C in December and January; in April and May the temperature can be over 30°C.
The school authorities and the parents or guardians of the children were informed of the objectives of the study and the procedures to follow. A note was sent to the children’s’ guardians requesting permission for their children to participate in the study; in addition, each of these families completed a survey regarding the child’s place of birth, place of residence, hygiene habits, use of fluoridated toothpaste, frequency of brushing, supervision by parents or guardians during brushing, the use of other fluoridated products in the home or at a professional level, and preventive measures applied at school or at the dentist’s office.
Children age 10 to 12 years, who were born in the municipality and had lived there since birth, who agreed to participate, and who completed the questionnaire were included. We excluded children with fixed orthodontics, who presented a condition that would make the oral examination difficult, and/or who were not present on the days of the study.
Diagnosis of dental fluorosis
International standards for controlling infection were used during the oral examination. The dental examination was performed during the day in natural light using a periodontal probe and mirror after prior removal of dentobacterial plaque via brushing, or failing that, cleaning with gauze.
An experienced and trained examiner measured the index of dental fluorosis in the permanent dentition by applying the WHO criteria [11]. Ten percent of examinations were duplicated, and the resulting Kappa values were greater than 0.92.
The diagnosis of fluorosis was determined using the modified Dean index criteria [11,12] with a range of 0 (normal), 1 (very mild), 2 (mild), 3 (moderate), and 4 (severe). Cases with a questionable index were incorporated into the normal category.
Statistical analysis
Based on data from previous studies, a sample size calculation was performed using a proportional population model with an interval of 95% and an error of 7%. Of 263 initially approached students, 99% agreed to participate and provided informed consent, and 239 children completed the questionnaire to meet all of the inclusion criteria.
Measures of central tendency and dispersion were calculated for each variable. Frequencies and percentages were calculated for each categorical variable. Bivariate analysis was performed to evaluate the associations between the prevalence of dental fluorosis and the independent variables. The χ2 test was used to evaluate associations between the prevalence of dental fluorosis and the independent variables. Finally, logistic regression analysis was performed to evaluate the possible association between dental fluorosis and risk factors.
Results
The study consisted of 239 students between 10 and 12 years of age. The mean age was 11.09±0.82 years. There were 122 male and 117 female students; 81 (33.9%) students were 10 years old, 78 (32.64%) were 11 years old, and 80 (33.47%) were 12 years old (Table 1).
Table 1.
Severity of dental fluorosis using the modified dean index according to age.
| Age | Modified Dean Index | Mean ±SD | |||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||
| 10 | 81 | 49.4 | 30.9 | 13.6 | 4.9 | 1.2 | 0.78±0.949 |
| 11 | 78 | 39.7 | 41.0 | 12.8 | 3.8 | 2.6 | 0.88±0.953 |
| 12 | 80 | 35.0 | 42.5 | 15.0 | 5.0 | 2.5 | 0.98±0.968 |
0 – without dental fluorosis; dental fluorosis = grades 1 to 4; 1 – very mild; 2 – mild; 3 – moderate; 4 – severe; SD – standard deviation.
Using the modified DI, 58.6% (n=140) of students had dental fluorosis and 41.4% (n=99) did not. When these were classified according to the level of severity, 41.4% (n=99) were healthy, 38.1% (n=91) had very mild disease, 13.8% (n=33) had mild disease, 4.6% (n=11) had moderate disease, and 2.09% (n=5) had severe disease. The distribution of severity by age is shown in Table 1 and shows that the severity of dental fluorosis increases with increasing age. There was no association between age and dental fluorosis (p>0.05), which could be because there was little variation in age in this study.
Of the 10-year-olds, the mean dental fluorosis index was 0.78 (CI 95%: 0.57–0.99). Of these children, 50.6% had fluorosis, 44.5% had very mild or mild levels, and only 6.2% had moderate and severe levels. Thus, fluorosis increased with age. Among the 12-year-olds, the mean index was 0.98 (CI 95%: 0.76–1.19), with a 14.4% increase in the prevalence to 65%; 57.5% showed very mild or mild and 7.5% in moderate and severe levels (Figure 1).
Figure 1.
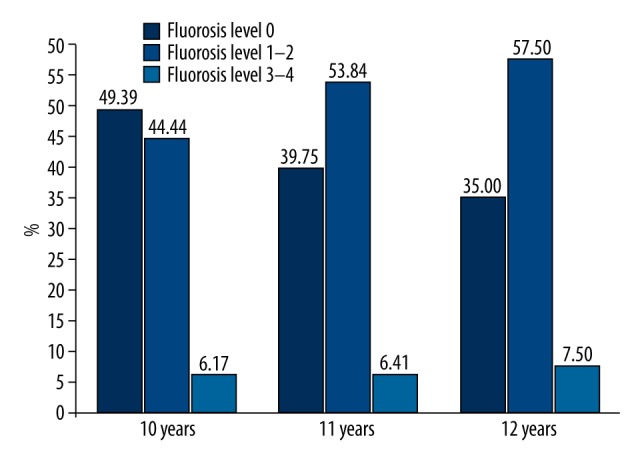
Severity of dental fluorosis using the DI, with level 0 being healthy, level 1–2 being very mild/mild and levels 3–4 being moderate/severe.
There was no difference in fluorosis by gender (p>0.05); 59.8% of males and 57.2% of females had fluorosis.
All children used toothpastes with fluoride concentrations above 1000 ppm for oral hygiene, and 216 (90.4%) did not use other forms of fluoride. With regards to brushing frequency, 147 (61%) participants brushed 1 or 2 times per day and 92 (38.5%) brushed 3 times per day. The age of first tooth-brushing was not considered, as more than 78% of participants reported not remembering. Most parents or guardians (n=174, 72.8%) did not supervise their children’s brushing, with few parents (n=65, 27.2%) supervising brushing. Only 9.6% of children had access to other forms of fluoride, such as mouthwashes or fluoride application in the dentist’s office.
Of the children who brushed 1–2 times per day, 52.4% were free of fluorosis, while of those who brushed 3 times per day, only 23.9% were free of dental fluorosis (p=0.000). The children who brushed the most had a greater prevalence of dental fluorosis, and of those children whose parents or guardians supervised their brushing, the proportion of teeth with fluorosis was less than 30.8% (p=0.000). There were few students exposed to other fluoride products, and of those, 73.9% had dental fluorosis; there were no differences between these students and those who were not exposed (Table 2).
Table 2.
Prevalence of dental fluorosis and relation with independent variables.
| With fluorosis | Without fluorosis | χ2 | p | |||
|---|---|---|---|---|---|---|
| # | % | # | % | |||
| Age | ||||||
| 10 | 41 | 45.7 | 40 | 54.3 | ||
| 11 | 47 | 58.8 | 31 | 41.2 | ||
| 12 | 53 | 65.0 | 27 | 35.0 | 3.436 | 0.064 |
| Sex | ||||||
| Male | 73 | 59.8 | 49 | 40.2 | ||
| Female | 67 | 57.3 | 50 | 42.7 | 0.163 | 0.687 |
| Brushing | ||||||
| 1–2 times | 70 | 47.6 | 77 | 52.4** | ||
| 3 times | 70 | 76.1** | 22 | 23.9 | 18.900 | 0.000 |
| Parental supervision | ||||||
| Yes | 20 | 30.8 | 45 | 69.2** | ||
| No | 120 | 68.9** | 54 | 31.1 | 28.454 | 0.000 |
| Other products with fluoride | ||||||
| Yes | 17 | 73.9 | 6 | 26.1 | ||
| No | 123 | 56.9 | 93 | 43.1 | 2.467 | 0.116 |
Significance at level 0.01 between brushing frequency and fluorosis;
significance at level 0.01 between parental supervision and fluorosis.
Tables 3 and 4 show the results of the bivariate analysis and the logistic regression model; relations between dental fluorosis and the independent variables are shown. The Wald test shows that the frequency of brushing and parental supervision were significant (p<0.05); use of mouthwashes was not significant, as few children used mouthwashes, and the model was mildly significant for the inclusion of this variable.
Table 3.
Bivariate analysis between dental fluorosis and independent variables.
| Variables | OR | CI 95% | p value |
|---|---|---|---|
| Age | |||
| 10–12 years | 0.120 | 0.006–0.252 | 0.064 |
| Gender | |||
| Male | 0.949 | 0.736–1.224 | |
| Female | 1.055 | 0.813–1.370 | 0.687 |
| Brushing | |||
| 1 and 2 times | 1.556 | 1.278–1.893 | |
| 3 times | 0.444 | 0.297–0.666 | 0.000 |
| Parental supervision | |||
| Yes | 3.182 | 2.010–5.038 | |
| No | 0.636 | 0.525–0.771 | 0.000 |
| Mouthwashes | |||
| Yes | 0.499 | 0.204–1.239 | |
| No | 1.069 | 0.988–1.158 | 0.116 |
OR – odds ratio; CI – confidence interval.
Table 4.
Logistic regression model between fluorosis and independent variables.
| Variables | B | Wald | p value |
|---|---|---|---|
| Brushing | 2.111 | 26.030 | 0.000 |
| Parental supervision | 2.502 | 31.199 | 0.000 |
| Mouthwashes | −0.650 | 1.323 | 0.250 |
| Constant | −4.699 | 3.675 | 0.055 |
Brushing frequency and parental supervision are significant variables. Final equation model –2 log-likelihood 256.737, r2 Nagelkerke p 0.331.
Discussion
The present study found dental fluorosis in more than half of children studied, which is greater than the prevalence found in studies of students of the same age who lived in other zones in the south of the Federal District [8,13].
The predominant levels were very mild and mild, consisting of 51.9% of students; 6.69% of children had moderate or severe levels, which indicates that these children were exposed to high doses of fluorides. The severity could be due to a difference in overexposure to fluoride or to the individual characteristics of the children.
In a recent 5-year period, an increase in mean dental fluorosis from 0.26 to 0.43 has been reported in a municipality of Mexico City [13].
Various studies have recorded dental fluorosis in many countries [14–16], and in various states of Mexico, the presence of this illness has been considered endemic in several areas, especially in the center and north of the country [17,18], which have high concentrations of natural fluoride in the water [19,20]. The population of this region is characterized by low socioeconomic status, and is a vulnerable group in which fluoridated salt is an efficient measure to improve the deplorable situation of dental cavities. Because they have very little purchasing power, families use the same toothpaste for all members, such that from the moment they begin brushing their teeth, in addition to salt intake, the children can be exposed to high concentrations of fluoride in the toothpaste.
Most children brushed their teeth fewer than 3 times per day; 38.5% brushed 3 times per day. An association was found between fluorosis and more frequent brushing, with the group of children who brushed more often having 28.5% more cases of fluorosis than in children who brushed less frequently, and these results agree with other studies [21,22].
Virtually all brands of toothpaste available in Mexico are fluoridated with fluoride concentrations above 1000 ppm. Studies on children below the age of 6 years show that they generally swallow some of the toothpaste when brushing their teeth; in the first years of life, as revealed by systematic research, this is a fundamental risk factor for the development of dental fluorosis in permanent teeth [23].
Few parents supervised their children when they were brushing their teeth, indicating that the amount of toothpaste used could be greater than required and that children might not be rinsing properly, both of which could increase the prevalence of dental fluorosis. In this study, there was a greater prevalence of fluorosis among children who brushed without parental supervision. At early ages, there is little control of expectoration of the residues of toothpaste during brushing, and studies have reported that small children ingest between 64.3% and 83.9% of toothpaste, and even at 5 years of age, children will ingest up to 30% of the toothpaste they use [24–26].
The exposure to fluorides through tooth-brushing with toothpastes containing a high concentration of fluoride, the lack of supervision by parents during tooth-brushing, and the use of fluoridated salt, which is the only systemic measure implemented at a national level, and which has been used for more than 2 decades through the norm NOM-040-SSAI-1993 [27], which established the limits of exposure to fluoride concentration. The levels of fluorides may be higher than is regulated by the norm, causing overexposure during key periods of susceptibility.
There are studies that show that subjects under the same conditions regarding exposure to fluorides may present different severity in dental fluorosis and may even not be affected by the problem. This may be due to several factors, among which we can mention the difference between absorption and retention of fluorides, duration of the exposure, nutritional state of the individual, diet, and possible genetic susceptibility [28,29].
The results from the present study can be interpreted to show that in addition to fluoridated salt, toothpastes are exacerbating the prevalence of this ailment.
At present, dental fluorosis is not a public health problem in the majority of the studied population. However, it is a public health problem among children with moderate and severe fluorosis, in whom the entire enamel structure is affected and which may lead to the loss of chewing function, esthetic problems, and even tooth breakage.
It is important to identify all of the risk factors involved and all of the sources of fluorides that can lead to this disorder of the enamel, as well as to detect the problem early, chiefly during primary dentition, to avoid the risks of fluorosis in permanent dentition.
The prevalence of fluorosis in areas without high levels of fluoride in the water may be related to the use of fluoridated salt as the only systematic preventative measure for dental cavities. We believe that in Mexico, a fluoride concentration of 0.5 ppm in the water would be sufficient for applying the National Program of Fluoridation of Domestic Salt, in addition to the authorities maintaining strict monitoring of fluoridated substances, toothpastes, drinks, and foods containing fluoride.
Conclusions
In conclusion, the association found with frequency of brushing and lack of parental supervision may be contributing to the prevalence and severity of dental fluorosis.
Acknowledgements
We wish to thank the authorities from Secretary of Education, especially the school principals, teachers, parents, and alumni, for their collaboration in the present study, and who made this study possible.
Footnotes
Source of support: This study was supported by the Department of Health Care, DCBS, Autonomous Metropolitan University, Xochimilco, Projects Number 3450496
Conflicts of interest
The authors declare no conflict of interests.
References
- 1.Burt BA, Keels MA, Heller KE. The effect of a break in water fluoridation no the development on dental fluorosis. J Dent Res. 2000;79:761–69. doi: 10.1177/00220345000790021001. [DOI] [PubMed] [Google Scholar]
- 2.DesBesten PK. Biological mechanisms of dental fluorosis to the use of fluoride supplements. Community Dent Oral Epidemiol. 1999;27:41–47. doi: 10.1111/j.1600-0528.1999.tb01990.x. [DOI] [PubMed] [Google Scholar]
- 3.Secretaría de Salud. Manual para el Uso de Fluoruros Dentales en la República Mexicana. 2006. [in Spanish] [Google Scholar]
- 4.Normatividad Mexicana para la Fluoruración de la Sal. Secretaria de Salud; Norma Oficial Mexicana NOM-013-SSA2-1994 Para la Prevención y Control de Enfermedades Bucales. http://www.amisac.org.mx [in Spanish] [Google Scholar]
- 5.Comisión Nacional del Agua. Monitoreo de las fuentes de abastecimiento de agua. SRH; México: 2000. [in Spanish] [Google Scholar]
- 6.Mascarenhas AK. Risk factors for dental fluorosis: a review of the recent literature. Pediatr Dent. 2000;22:269–77. [PubMed] [Google Scholar]
- 7.Martínez-Mier EA, Soto-Rojas AE, Ureña-Cirett JL, et al. Fluoride intake from foods, beverages and dentifrice by children in Mexico. Community Dent Oral Epidemiol. 2003;31:221–30. doi: 10.1034/j.1600-0528.2003.00043.x. [DOI] [PubMed] [Google Scholar]
- 8.Molina-Frechero N, Castañeda-Castaneira RE, Hernández-Guerrero JC, Robles PG. Prevalencia de fluorosis dental en escolares de una delegación política de la Ciudad de México. Rev Mex Pediatr. 2005;72(1):13–16. [in Spanish] [Google Scholar]
- 9.Juárez-López M, Hernández-Guerrero JC, Jiménez-Farfán D, Ledesma-Montes C. Prevalencia de fluorosis dental y caries en escolares de la ciudad de México. Gac Med Mex. 2003;139(3):221–25. [in Spanish] [PubMed] [Google Scholar]
- 10.Instituto Nacional de Estadística, Geografía e Informática 2011. INEGI; México: [in Spanish] [Google Scholar]
- 11.World Health Organization. Oral health survey-basic methods. 3rd ed. Geneva: WHO; 1997. [Google Scholar]
- 12.Rozier RG. Epidemiologic Indices for Measuring the Clinical Manifestations of Dental Fluorosis. Overview and Critique. Adv Dent Res. 1994;8:39–55. doi: 10.1177/08959374940080010901. [DOI] [PubMed] [Google Scholar]
- 13.Molina-Frechero, Castañeda-Castaneira RE, Robles Pinto G. Incremento de la fluorosis en México. Acta Pediatr Mex. 2007;28:149–53. [in Spanish] [Google Scholar]
- 14.Whelton HP, Ketley CE, McSweeney F, O’Mullane DM. A review of fluorosis in the European Union: prevalence, risk factors and aesthetic issues. Community Dent Oral Epidemiol. 2004;32(Suppl 1):9–18. doi: 10.1111/j.1600-0528.2004.00134.x. [DOI] [PubMed] [Google Scholar]
- 15.Kumar JV, Swango P. Fluoride exposure and dental fluorosis in Newburgh and Kingston, New York: policy implications. Community Dent Oral Epidemiol. 1999;27:171–80. doi: 10.1111/j.1600-0528.1999.tb02007.x. [DOI] [PubMed] [Google Scholar]
- 16.Angulo M, Bianco P, Cuitiño E, Silveira A. Relevamiento y análisis de caries dental, Fluorosis y gingivitis en adolescentes escolarizados de 12 años de edad en la República Oriental del Uruguay. Facultad de Odontología-Ministerio de Salud Pública; 2015. pp. 46–53. [in Spanish] [Google Scholar]
- 17.Irigoyen Camacho ME, Molina Frechero N, Luengas Aguirre MI. Prevalence and severity of dental fluorosis in a mexican community with above-optimal fluoride concentration in drinking water. Community Dentistry and Oral Epidemiol. 1995;23:243–45. doi: 10.1111/j.1600-0528.1995.tb00239.x. [DOI] [PubMed] [Google Scholar]
- 18.Jarquín Yañez L, Mejia Saavedra JJ, Molina Frechero N, et al. Association between urine fluoride and dental fluorosis as a toxicity factor in a rural community in the State of San Luis Potosí. Scientific World Journal. 2015;2015:647184. doi: 10.1155/2015/647184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franco AM, Martignon S, Saldarriaga A, et al. Total fluoride intake in children aged 22–35 months in four Colombian cities. Community Dent Oral Epidemiol. 2005;33:1–8. doi: 10.1111/j.1600-0528.2004.00164.x. [DOI] [PubMed] [Google Scholar]
- 20.Twetman S, Axelsson S, Dahlgren H, et al. Caries-preventive effect of fluoride toothpaste: a systematic review. Acta Odontol Scand. 2003;6:347–55. doi: 10.1080/00016350310007590. [DOI] [PubMed] [Google Scholar]
- 21.Cochran JA, Ketly CE, Duckworth RM, et al. Development of a standardize method for comparing fluoride ingested from toothpaste by 1,5-3,5 years-old children in seven European countries. Part 2: Ingestion result. Community Dent Oral Epidemiol. 2004;32(Suppl 1):47–53. doi: 10.1111/j.1600-0528.2004.00139.x. [DOI] [PubMed] [Google Scholar]
- 22.Abanto Alvarez J, Rezende KM, Marocho SM, et al. Dental fluorosis: Exposure,prevention and managment. Med Oral Patol Oral Cir Bucal. 2009;14(2):E103–7. [PubMed] [Google Scholar]
- 23.Bårdsen A. “Risk periods” associated with the development of dental fluorosis in maxillary permanent central incisors: a meta-analysis. Acta Odontol Scan. 1999;57(5):247–56. doi: 10.1080/000163599428652. [DOI] [PubMed] [Google Scholar]
- 24.Bottenberg P, Deeclerck D, Ghidey W, et al. Prevalence and determinants of enamel fluorosis in Flemish schoolchildren. Caries Res. 2004;38:20–28. doi: 10.1159/000073916. [DOI] [PubMed] [Google Scholar]
- 25.Zohoori FV, Duckworth RM, Omid N, et al. Fluoridated toothpaste: Usage and ingestion of fluoride by 4-to 6-yr-old children in England. Eur J Oral Sci. 2012;120:415–21. doi: 10.1111/j.1600-0722.2012.00984.x. [DOI] [PubMed] [Google Scholar]
- 26.Browne D, Whelton H, O’Mullane D. Fluoride metabolism and fluorosis. J Dent. 2005;33(3):177–86. doi: 10.1016/j.jdent.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 27.Secretaría de Salud. Especificaciones sanitarias. SSA; 1995. Norma Oficial Mexicana NOM-040-SSA1-1993, Bienes y Servicios. Sal yodatada y sal yodatada fluorurada. [in Spanish] [Google Scholar]
- 28.Mousny M, Banse X, Wise L, et al. The genetic influence on bone susceptibility to fluoride. Bone. 2006;39:1283–89. doi: 10.1016/j.bone.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 29.Vieira AP, Hancock R, Eggertsson H, et al. Tooth quality in dental fluorosis genetic and environmental factors. Calcif Tissue Int. 2005;76:17–25. doi: 10.1007/s00223-004-0075-3. [DOI] [PubMed] [Google Scholar]


