Introduction
Fetal intra-abdominal umbilical vein varix (FIUVV) is a rare fetal malformation, defined as an umbilical vein diameter larger than 9 mm; greater than two standard deviations for gestational age; 1.5 times the diameter of its intrahepatic portion or more than 50 % compared to its non-dilated portion. The prevalence rate is unknown. Recently, it has been estimated at 2.8 per 1000 pregnancies [1]. Several case studies have been published, with a highly variable fetal prognosis [2]. In addition, as it is a rare malformation, there are no clear protocols on its obstetric management. This case study presents the prenatal diagnosis, obstetric management, and neonatal development of a fetus diagnosed with FIUVV.
Case
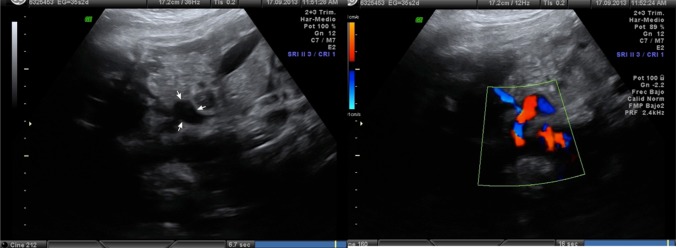
Our patient was a 35-year-old healthy gravida 1 para 0, who achieved pregnancy after IVF. The combined screening for fetal aneuploidy performed at 12 weeks of gestation reported a low risk, and the morphological ultrasound performed at 20 weeks showed a female fetus with a normal anatomical study except for an umbilical vein dilatation of 11 mm in its intra-abdominal portion, leading to the FIUVV diagnosis. Ultrasound follow-up was performed since then every 2 weeks showing no significant increase in dilatation or impact on fetal hemodynamic status. She was referred to our center at the 34th week of gestation, when we confirmed an aneurysmal dilatation of the intra-abdominal umbilical vein of 11 mm, with venous flow as observed by applying color Doppler, without any signs of thrombosis (Fig. 1). Weekly cardiotocography and ultrasound guidance were performed, showing no changes in the image described and ascertaining fetal wellbeing. Labor was induced at 37 weeks of gestation, giving birth, by cesarean section because of failed induction, to a 2620-g female baby with Apgar scores of 9 at 1 min and 10 at 5 min. No abnormalities were evident in the physical examination. Echocardiography, and cerebral and abdominal ultrasound performed on the newborn were normal. A karyotype was requested and yielded normal results (46, XX). Outpatient controls showed adequate development, reaching milestones for her age.
Fig. 1.
Ultrasonographic images of the FIUVV, with and without color Doppler
Discussion
Classically, FIUVV has been considered to imply a high risk of intrauterine fetal demise, especially if it is associated with other malformations; presents turbulent flow; or appears early (<26 weeks). Thrombosis of the aneurysm or heart failure is suggested as possible cause(s) of fetal demise, while the mechanism by which this feared complication takes place is not fully understood.
This has conditioned its obstetric management, with the recommendation being to induce delivery at 34 weeks of gestational age. However, it has recently been proposed that in cases of isolated FIUVV, it would be better to wait until term whenever possible, since it seems that, in these cases, the risk of intrauterine fetal demise does not justify taking the risks of prematurity [3].
Regarding the obstetric management of FIUVV, it is essential to perform a careful anatomical study for its possible association with other malformations. If other malformations are found, a karyotype is recommended. The frequency of associated malformations published to date was around 30 % and almost 10 % for chromosome abnormalities. These data were based on case series collected from different authors. However, the first retrospective study to be published describes a frequency of 9.6 % of associated abnormalities on ultrasound and no chromosomal abnormalities [1]. It is possible that the risk has been falsely magnified by publication bias, and it is actually much more likely to be an isolated finding.
Anyway it is advisable to closely monitor the pregnancy from the time of diagnosis, especially at the end of the third trimester in which some authors recommend weekly or biweekly monitoring until delivery. The last three case series published follow these guidelines. Won Lee reported 121 cases with over 90 % born at term with only one intrauterine fetal death [1]. Navarro-González reported 14 cases, with a mean gestational age at delivery of 38 weeks without perinatal complications [4]. Bass-Lando published 24 cases with a mean gestational age at delivery of 37 weeks, with no intrauterine or perinatal demises. In fact, this author suggests that the isolated finding of FIUVV might be a normal anatomical variant [2].
Conclusion
Usually FIUVV is an isolated finding with favorable evolution, and conservative management is appropriate, as happened in our case. It is advisable to focus on other possible associated malformations or fetal growth delays by ultrasound, and to avoid delivering prematurely if it is an isolated finding.
Compliance with ethical requirements and Conflict of interest
No research involving human and/or animal participants has been done. No informed consent has been obtained because it does not apply. The authors report no declaration of interest.
Loida Pamplona-Bueno
has a degree in Medicine and Surgery from the Universidad Autónoma de Madrid (2012). She is currently undergoing Residency Training Program in Obstetrics and Gynecology at the University Hospital La Fe, Valencia. She holds currently a Master’s Degree in Human Reproduction from the University of Valencia. She is presently the co-principal investigator in the ongoing clinical trial: “Follicle activation in patients with poor ovarian response through fragmentation of the ovarian tissue,” at the University Hospital La Fe, Valencia. Her research interests are focused on Reproductive medicine, especially that of poor ovarian response. .
.
References
- 1.Lee SW, Kim MY, Kim JE, et al. Clinical characteristics and outcomes of antenatal fetal intra-abdominal umbilical vein varix detection. Obstet Gynecol Sci. 2014;57(3):181–186. doi: 10.5468/ogs.2014.57.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bass-Lando M, Rabinowitz R, Samueloff A, et al. The prenatal diagnosis of isolated fetal varix of the intra-abdominal umbilical vein is associated with favorable neonatal outcome at term: a case series. Arch Gynecol Obstet. 2013;288(1):33–39. doi: 10.1007/s00404-013-2743-x. [DOI] [PubMed] [Google Scholar]
- 3.Mankuta D, Nadjari DC, Pomp G. Isolated fetal intra-abdominal umbilical vein varix, clinical importance and recommendations. J Ultrasound Med. 2011;30:273–276. doi: 10.7863/jum.2011.30.2.273. [DOI] [PubMed] [Google Scholar]
- 4.Navarro-González T, Bravo-Arribas C, Fernández-Pacheco RP, et al. Perinatal outcome after prenatal diagnosis of intra-abdominal umbilical vein varix. Ginecol Obstet Mex. 2013;81(3):140–145. [PubMed] [Google Scholar]