Abstract
Objectives
Uterine morcellation of presumed leiomyomas inadvertently results in an increase in morcellated uterine leiomyosarcoma (ULMS). Morcellation alters the natural course of ULMS, leading to an increased incidence and earlier recurrences. Recurrences following tumor morcellation are significantly more likely to occur in the peritoneum. Since there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma, the US FDA (Food and Drug Administration) discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy (US Food and Drug Administration, http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm in 2014). In the wake of recent ban on usage of power morcellation by US FDA, we introduce a technique of in-bag morcellation, thus avoiding spillage of tissues in the peritoneal cavity and spread of an undiagnosed disease or cancer or sarcoma.
Methods
We present a study of twenty-one cases of laparoscopic in-bag morcellation of fibroid and uteri done by Total Health Care method.
Results
The in-bag morcellation technique handles the issue of ULMS and makes laparoscopic myomectomy and hysterectomy possible with fair safety.
Conclusions
Further studies should be directed toward identifying patients at high risk of ULMS prior to presumed leiomyoma resection in order to reduce the risk of inadvertent tumor morcellation.
Keywords: Leiomyosarcoma, Morcellation, In-bag, Fibroids, Total Health Care method
Introduction
Tissue retrieval is a unique challenge since long time. Originally, it was for dermoid cyst, doubtful ovarian masses removed in lap sac or endobag reducing the risk of spillage; though if the spillage was from a non-malignant mass, the consequences were not dangerous. However, laparoscopic power morcellation if performed in women with unsuspected uterine sarcoma, there is a risk that the procedure will spread the cancerous tissue within the abdomen and pelvis, significantly worsening the patient’s likelihood of long-term survival. Evaluation by sonography, Doppler or markers is also not completely reliable to diagnose a case of sarcoma. The US FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy [1]. In a recent meta-analysis, the estimated rate of leiomyosarcoma was 0.51 per 1000 procedures or approximately 1 in 2000; restricting the meta-analysis to the 64 prospective studies resulted in a substantially lower estimate of 0.12 leiomyosarcomas per 1000 procedures or approximately 1 leiomyosarcoma per 8300 surgeries [2]. Withdrawing morcellation and not giving the benefits of laparoscopic surgery especially in young infertile women with fibroids or laparoscopic hysterectomy in patients with low risk of ULMS are debatable. To avoid a surprise case though rare of ULMS diagnosed postoperatively, it is better to perform the Total Health Care in-bag morcellation method, described in the study, on a regular basis.
Materials and Methods
Twenty-one cases of laparoscopic in-bag morcellation of uteri and fibroids, of varying sizes and numbers, were performed over a period of 5 months from April 2015 to August 2015 at Total Health Care Centre, a referral center for advanced endoscopy.
Laparoscopic myomectomy is an art of three in one technique:
Removal of fibroid from the uterus
Reconstructing the uterus with very efficient methods of laparoscopic suturing
Removing the separated fibroid from the abdominal cavity either by vaginally or by morcellation.
Similarly, laparoscopic hysterectomy in difficult cases of large uterus with previous cesareans or previous abdominal surgeries in addition to obesity and high-risk patients is an equally skilled procedure, especially when very large uteri are removed by morcellation.
Fourteen cases of laparoscopic hysterectomy with varying sizes and weight—largest being 1.4 kg—and seven cases of laparoscopic myomectomy varying in size (4–7 cm) with up to seven fibroids were morcellated using Total Health Care technique of in-bag morcellation for their retrieval. There were no limitations, except in case of very large fibroids which is equal to 26 weeks size uterus, wherein the movement of the bag may be difficult.
The author has never come across a single case of sarcoma, during his vast experience of myomectomies and hysterectomies using morcellation.
We have used Steiner’s morcellator, power morcellator, morcelle, rotocut and morsafe for morcellation since 20 years.
Technique
Total Health Care Technique of Performing In-Bag Morcellation of Fibroids and Uterus
The steps of laparoscopic myomectomy and laparoscopic hysterectomy remain the same as done in a standardized fashion leaving the fibroid or uterus separated in the peritoneal cavity. The left lower port is widened to pass a 10-mm port and further with a finger mechanically stretched to make easy passage of the soft plastic sleeve carrying the bag.
As shown in Fig. 1, there is a medium-sized strong plastic bag in the shape like stomach but with a wider opening. The wide opening of the bag is folded and introduced in a one-side openable plastic cannula, which is designed to carry the bag inside the abdomen replacing the left lower 10-mm port (Fig. 2). Once the bag is seen inside the sleeve in the abdomen through the laparoscope, the assistant holds only the bag with a 5-mm atraumatic grasper allowing the removal of introducing plastic sleeve. The remaining part of the mouth of the bag is pulled systematically with atraumatic graspers held in sequence by the surgeon and assistant (Fig. 3). Once full bag is inside the abdomen, the 10-mm port is reintroduced with a reducer to carry a 5-mm instrument. The wide ring of the opening of the bag is identified and held by the assistant and surgeon, with a single-tooth grasper surgeon who holds the specimen and transfers it inside the bag (Fig. 4). The opening of the bag is systematically closed bringing one end close to the left lower 10-mm port carrying a 5-mm grasper. The two parts of the opening of the bag are held together and pulled out withdrawing the 10-mm trocar. And then holding the two margins of the mouth, the bag is mechanically pulled by two hands of the surgeon bringing the entire mouth of the bag outside the left lower port. The camera keeps a constant watch to see that the specimen is always inside the bag. Now from the right lower port with a 5-mm grasper, the duodenum shaped part of the bag, which we call as the ear with a hole, is held at the tip and railroaded inside the 10-mm trocar of the optics. Care is taken to keep the right semiflexed leg low to allow free movement of the 5-mm grasper holding the ear to be easily railroaded inside the 10-mm trocar which is withdrawn. Externally, this part of the bag is seen at the umbilical region. This part of the bag which is like the ear has a 5-mm hole which is widened to introduce the 10-mm trocar which will carry the optics. Once in place, the optics is introduced and CO2 insufflation is started. The optics and the screen clearly show opening of the bag with the specimen within, and the mouth of the bag coming from the left lower port is blocked by the assistant. Once everything is in place, a 12-mm morcellator hand piece with a blunt tip trocar is introduced under vision inside the bag from the left lower port. A clear vision makes you visualize that the bag has replaced practically as the peritoneal lining with all abdominal structures outside the bag, but the specimen is within the bag in front of the morcellator.
Fig. 1.

Medium-sized strong plastic bag
Fig. 2.

Wide opening of the bag is folded and introduced
Fig. 3.
Remaining part of the mouth of the bag pulled systematically with atraumatic graspers
Fig. 4.

Transferring specimen in the bag with single-tooth grasper
The unique feature of the morcellator handle is that the sharp inner blade is not fully exposed but only a rim is seen with a hood of the morcellator hand piece. A 10-mm single-tooth grasper is introduced inside the morcellator, which will hold the specimen, and morcellation is done under vision (Fig. 5). The projecting hood of the morcellator hand piece protects the sharp circular inner cutting blade, and the specimen gets morcellated exactly in the fashion of orange peeling of 10-mm-long pieces. With a series of long strips, the whole specimen is morcellated. The bag now contains the small bits of morcellated remnant pieces and the blood of specimen side. The morcellator hand piece is removed blocking the mouth of the bag to prevent unnecessary scatter of tissue or fluid on the face of surgeon or assistant. The 10-mm optics and the trocar carrying the optics are removed.
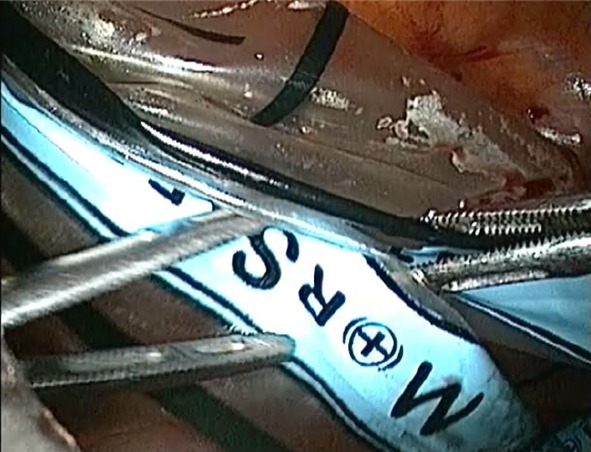
Fig. 5.

Morcellation done under vision
A knot is tied on the long ear-shaped plastic, next from the left lower port under external vision the bag is pulled out and one can see the knotted part of the ear getting withdrawn inside the umbilicus into the abdominal cavity and then comes out from the left lower port (Fig. 6).
Fig. 6.

Knot tied and bag pulled out
The optics is reintroduced from the 10-mm umbilical port, and under vision with a port closure device the left lower port is closed. A good look of the entire peritoneal cavity confirms hemostasis and also clearly shows that not a drop of specimen side fluid or a small piece of the specimen is seen within the peritoneal cavity.
With this technique, the author has successfully removed twenty-one cases of uteri or fibroid as big as 1.4 kg or 26 weeks in size. Also, a case of seven fibroids varying from 4 to 7 cm were removed all with in-bag morcellation.
Technical Issues
Care has to be taken that the abdominal opening for the morcellator to enter should be adequate for free movements.
The mouth of the bag once out from lower left port; the ear has to come out from the umbilical port without any twists. Thus, the learning curve would include making sure to align the two marked parallel lines of the bag to the optics, to avoid the twist.
When faced with technical difficulty in one such case, sharp part of rotocut was used to puncture the bag, and to our surprise complete morcellation without any spillage, in the bag itself, was possible.
Emphasis would again be on the technique which is simple and dependable and achieves all the functions of no spillage of any tissue material from the specimen into the peritoneal cavity.
Discussion
Recent statistics regarding clinical characteristics and management experience of unexpected uterine sarcoma stated that among 4248 patients who underwent myomectomy for presumed leiomyoma, 9 (0.2 %) had unexpected uterine sarcoma [1 (<0.1 %) had leiomyosarcoma and 8 (0.2 %) endometrial stromal sarcoma]. The malignancy was identified in 5 (0.2 %) of 3068 women who were treated by laparoscopy with power morcellation and 4 (0.3 %) of 1180 who underwent laparotomy (P = 0.274). Thus, the overall incidence of unexpected uterine sarcoma after myomectomy was low, and incidental power morcellation of unexpected uterine sarcoma seemed to cause no increase in sarcoma dissemination [3].
AAGL issued a statement as a reply to FDA, stating that it is possible that different risk profiles exist among the various methods of morcellation, but specific data are lacking with respect to these differences (Level C). Hysteroscopic removal of symptomatic submucosal uterine myoma in premenopausal women need not be exchanged for definitive treatment (i.e., hysterectomy) simply to avoid morcellation (Level A). Women with asymptomatic uterine myoma can be managed expectantly (Level A). Laparoscopy has well-documented advantages over laparotomy regarding surgical complications and patient outcomes (Level A). Sarcomas have been diagnosed after alternative uterine-preserving treatments such as uterine artery ligation. The same challenges in preoperative diagnosis of uterine sarcoma apply to these surgical alternatives (Level C). The use of morcellation within specimen retrieval pouches for containment of benign or malignant uterine tissue requires significant skill and experience, and the use of specimen retrieval pouches should be investigated further for safety and outcomes in a controlled setting (Level C) [4].
ACOG came up with a special report, stating that the practitioners should quote a risk estimate of 2:1000 for undiagnosed uterine sarcoma including leiomyosarcoma [5].
Extensive patient counseling is a must and alternative to power morcellation should be offered. Ideal is to predict preoperative diagnosis. Demographic factors do not help and may be present in young patients in age group of 20s and 30s.
A prospective small study revealed high sensitivity and specificity of combination of dynamic MRI and measurement of total LDH and LDH isoenzyme type 3, but there were no results on large scale; thus, more research was recommended [6].
Conclusion
The controversy of morcellating a fibroid or uterus which may have unsuspected malignancy or leiomyosarcoma is voiced and over-hyped beyond genuine scientific proportion. We have a few groups of patients and activists who put laparoscopic morcellation to a total disrepute, in contrary to recent meta-analysis suggesting the actual risk of an unexpected leiomyosarcoma not more than 1 in 2000 cases or probably even less. Benefits of laparoscopic morcellation should be given as an option along with vaginal removal of the specimen, especially in young and deserving patients, wherein benefits of laparoscopic minimal access surgery with a quick recovery should be extended after proper counseling. The new in-bag morcellation technique as described by the author would easily take care of fibroids or uterus up to 26 weeks in size or weighing up to 2 kg.
The most interesting scientific aspect of this controversy is that even if a leiomyosarcoma is removed by an open en bloc surgery still there is 50 % risk of spread or already residual existing disease compared to 60 % risk when done by laparoscopic morcellation, that is only a 10 % risk reduction with open surgery [7, 8]. Further with the in-bag morcellation, the risk of spread drops down drastically unless originally the sarcoma or cancer was already spread.
The in-bag morcellation technique appears to handle the issue of ULMS and allows laparoscopic myomectomy and hysterectomy possible with fair safety. The scientific focus should be directed toward diagnosing leiomyosarcoma or a malignancy prior to surgery far more accurately with methods that are yet not totally identified.
Dr. Prakash H. Trivedi
who has released 8 books on endoscopic surgery, assisted reproduction, infertility dilemmas, safe minimal access surgery, etc. and has a unique sense of passion, a clean directed message and great expertise in all the fields. Apart from being a specialist and a good vaginal surgeon, he has deep driving interest in pelvic floor and urogynecological surgeries. His special interest in endoscopy and minimally invasive surgery is of paramount interest not only to him, peers and colleagues but also for the patient. I am sure that the knowledge and skills picked up from him will help many women of India and all over the world.
Compliance with Ethical Standards
Conflict of interest
All the corresponding authors note that there is no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Dr. Prakash H. Trivedi is a Professor and the Head of Department of Obstetrics and Gynecology, Rajawadi Hospital and he is the Scientific Director of Total Women Health Care Centre, Aakar IVF - ICSI Centre; Dr. Sandeep S. Patil is the Director of Yashadaa Hospital and he was the Ex-Clinical Associate of Dr. Trivedi’s Total Health Care Pvt. Ltd; Dr. Nishita A. Parekh is a Clinical Associate of Dr. Trivedi’s Total Health Care Pvt. Ltd; Dr. Animesh C. Gandhi is a Assistant Professor of BYL Nair Hospital; Dr. Soumil P. Trivedi is a Fellow in MUHS Recognised Minimally Access Surgery Gynaecology, Dr. Trivedi’s Total Health Care Pvt. Ltd; Dr. Mohini O. Abreo is a Clinical Assistant, Dr. Trivedi’s Total Health Care Pvt. Ltd.
References
- 1.U.S. Food and Drug Administration. 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. Accessed 17 April 2014.
- 2.Pritts EA, Vanness DJ. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12:165–177. doi: 10.1007/s10397-015-0894-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang J, Zhang J, Dai Y, et al. Clinical characteristics and management experience of unexpected uterine sarcoma after myomectomy. Int J Gynaecol Obstet. 2015;130(2):195–199. doi: 10.1016/j.ijgo.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 4.AAGL Practice Report: morcellation during uterine tissue extraction. J Minim Invasive Gynecol 2014:21(4):517–30. [DOI] [PubMed]
- 5.The American College of Obstetricians and Gynecologists (2014) Power morcellation and occult malignancy in gynecologic surgery. A Special Report
- 6.Goto A, Takeuchi S, Sugimura K, et al. Usefulness of Gd-DTPA contrast-enhanced dynamic MRI and serum determination of LDH and its isozymes in the differential diagnosis of leiomyosarcoma from degenerated leiomyoma of the uterus. Int J Gynecol Cancer. 2002;12(4):354–361. doi: 10.1046/j.1525-1438.2002.01086.x. [DOI] [PubMed] [Google Scholar]
- 7.Leung F, Terzibachian JJ. Re: “The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma”. Gynecol Oncol. 2012;124(1):172–173. doi: 10.1016/j.ygyno.2011.08.035. [DOI] [PubMed] [Google Scholar]
- 8.Seidman MA, Oduyebo T, Muto MG, et al. Peritoneal dissemination complicating morcellation of uterine mesenchymal neoplasms. PLoS ONE. 2012;7(11):e50058. doi: 10.1371/journal.pone.0050058. [DOI] [PMC free article] [PubMed] [Google Scholar]


