Abstract
The purpose of this literature review is to describe and assess the cultural barriers to behavior change in migrant South Asians, given the high morbidity and mortality associated with cardiovascular disease in this population. We reviewed studies that explored the relationship between South Asian culture in the Diaspora and lifestyle behaviors. Our review produced 91 studies, of which 25 discussed the relationship between various aspects of South Asians’ belief system and their approach to modifying lifestyle habits. We identify 6 specific categories of beliefs which play the largest role in the difficulties South Asians describe with behavior change: gender roles, body image, physical activity misconceptions, cultural priorities, cultural identity, and explanatory model of disease. Future research and interventions should account for these cultural factors to successfully improve dietary habits and physical activity levels in migrant South Asian populations.
Keywords: South Asian, Diet, Exercise, Cardiovascular disease, Cultural barriers
Introduction
The last century and a half has seen a great deal of South Asian (people with ancestry from India, Pakistan, Bangladesh, or Sri Lanka) migration to developed countries such as the United Kingdom (UK), Canada, Australia, and the United States (US). As a result, South Asians make up a significant and growing portion of the population in many of these countries [1]. For instance, in the United Kingdom, South Asians comprise the largest ethnic group [2]. According to the 2009 American Community Survey 1 year estimates, the Asian Indian population had a 55% growth rate in the last decade, surpassing that of Hispanics (37%), Chinese (28%), and Filipinos (34%), and have become the second most populous Asian ethnic group in the US Among Asian ethnic groups in the US, only the Chinese (population 3,106,005) outnumber South Asians (population 3,077,599) [3, 4]. Since South Asians represent a substantial proportion of these nations’ populations, medical conditions that are prevalent among South Asians are increasingly important to their societies and public health.
Cardiovascular disease (CVD) is one of the most prevalent health problems facing South Asians today. Regardless of location, South Asians exhibit the highest rates of cardiovascular disease among all ethnic groups [5–8]. The earliest reports of the higher prevalence of CVD originated in Singapore in 1957. In a series of nearly 1,000 autopsies, coronary heart disease (CHD) was seven times higher in Indian males than in Chinese males [9]. The more recent Singapore Cardiovascular Cohort study, a longitudinal study following 5,920 individuals also found a much higher risk of CHD in Asian Indians, compared to Chinese and Malays [10]. Data from the UK’s Health Survey of England found that the prevalence of CVD was at least 30–40% higher in South Asians compared to Caucasians [11–13]. In the UK, it has been shown that second generation South Asians also have a higher risk for CVD [14]. Additionally, the SHARE study in Canada found the prevalence of CAD in South Asians to be more than twice that of Caucasians and Chinese [15]. Other countries such as, South Africa, Uganda, and Trinidad have also found higher rates of CVD in their South Asian populations [5, 16, 17]. Although US data on South Asian health is sparse, the disparity here is also clear. A Kaiser study in the 1980s revealed that Asian Indians had a 4 times higher hospitalization rate for cardiovascular disease compared to Caucasians [18]. Additionally, the Coronary Artery Disease Study in Indians (CADI), which studied Asian Indian physicians in the US, found that the age adjusted prevalence of CAD was 10.5% in Asian Indian physicians compared to 2.5% in the Framingham offspring Cohort [5]. Furthermore, in a cross-sectional study conducted from 1990 to 2000 in California conducted by the Stanford Research Prevention Center, Asian Indians had the highest proportional mortality ratio (PMR) due to coronary heart disease (ratio of the number of deaths attributed to a specific cause to the total number of deaths occurring in the population during a time period) compared to Caucasians, African Americans, Hispanics, Chinese Americans and Japanese Americans [19]. In India itself, comparison of various epidemiological studies have revealed that the prevalence of CAD has increased from 1% in 1960 to 10.5% in 1998 in the urban population [20]. It is felt that the South Asian region contributes more than any other region to the global burden of CVD [21–24].
The disparity between South Asians and other ethnic groups is most prevalent at younger age groups. The average age of first MI on the South Asian subcontinent is 53 compared to 60–65 for Caucasians in North America and Western Europe [20, 24]. Studies undertaken at Calicut Medical College in India have revealed that 25% of heart attacks in India occurred in individuals under the age of 40, compared to 4–6% in Western Europe and North America [25]. This disparity exists when comparing migrant South Asian populations to other ethnic groups as well. In the UK, the rate of MIs for men under the age of 40 in South Asians was 4 times that in Caucasians [25, 26]. In the above mentioned Stanford University study, the PMR for CHD was highest in Asian Indian men in the 24–44 age group [19].
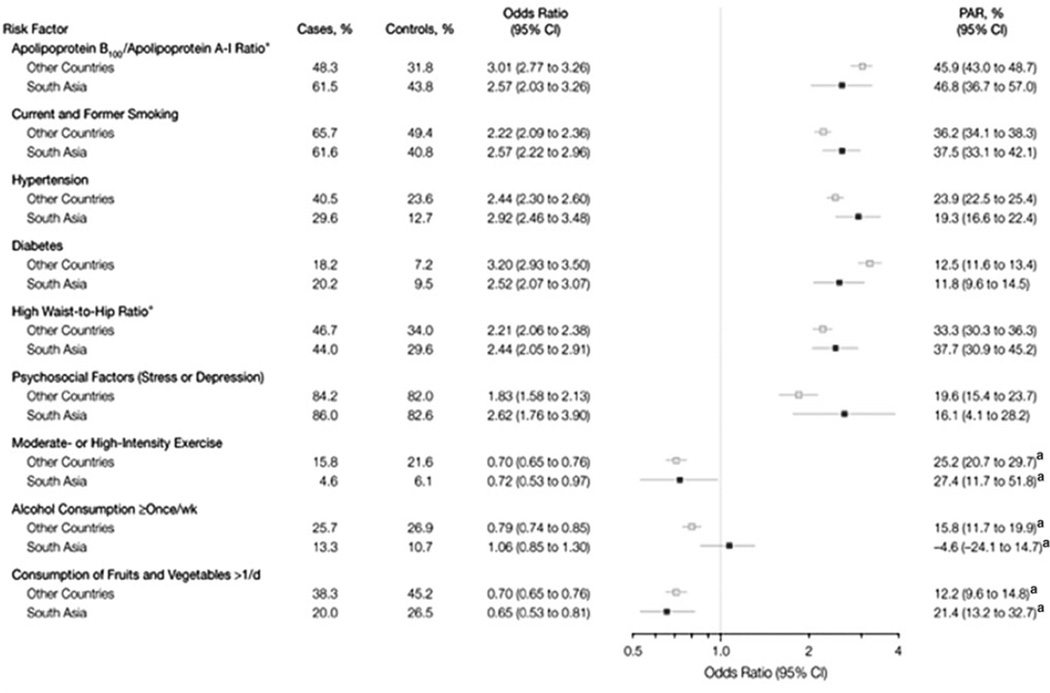
In searching for an explanation for the high prevalence of CAD in South Asians, the CADI study found that there was a higher prevalence of diabetes, higher triglyceride levels, and lower HDL levels in Asian Indians compared to Caucasians [16, 25]. Additionally, data from the UK and India have shown that South Asians have more total and central adiposity compared to Caucasians, contributing to higher rates of insulin resistance and diabetes [27–34]. The INTER-HEART study, a multinational cross-sectional study which enrolled 15,152 cases of first AMI and 14,820 age-matched controls in 262 centers in 52 countries, examined CVD risk factors across many different ethnic groups. The 9 risk factors listed in Table 1 are felt to explain 86% of the risk in South Asians. The low consumption of fruits and vegetables in South Asians, the lack of regular exercise, and the high waist:hip ratio were felt to contribute the most to higher rates of CHD seen in South Asians [24]. Studies in the UK and Canada also have consistently found lower levels of physical activity among South Asians compared to other ethnic groups [35–38]. In the US, a study conducted in Texas where participants were recruited from health fairs revealed not only a higher prevalence of the metabolic syndrome in South Asians, but also low physical activity levels [39]. In examining dietary habits, data from the SHARE study and the CADI study have shown that South Asian diets are high in carbohydrates and fat and contribute to low HDL and high triglyceride levels [40, 41]. Studies have shown that low physical activity levels, low fruit and vegetable intake, and high carbohydrate intake are common in South Asian children and adolescents, leading to acquisition of central obesity, insulin resistance, diabetes, and low HDL levels at younger ages (in their 30 s) compared to other ethnic groups, thus leading to CVD at young ages [20, 37, 42, 43]. Therefore, addressing the lifestyle behaviors of diet modification and physical activity levels can have a tremendous impact on CVD prevalence in South Asians. However, an understanding of how social factors and cultural beliefs relate to diet and exercise behaviors in migrant South Asian communities is crucial to addressing these lifestyle behaviors.
Table 1.
Risk factors associated With acute myocardial infarction in South Asians compared with other participants in INTERHEART Study
Source: Joshi et al. [24]
Indicates that the population attributable risk (PAR) related to South Asia versus the rest of the world is significantly different at the 0.05 level
Purpose and Objectives
The purpose of this review is to describe and assess the literature that addresses the difficulties migrant South Asians face in modifying diet and exercise behaviors. We evaluated literature that examined immigrant South Asian’s experiences with behavior change and identified 6 categories of beliefs affected by South Asian culture which influence approaches to these lifestyle behaviors: gender roles, body image, physical activity misconceptions, cultural priorities, cultural identity, and explanatory model of disease.
This review will guide clinicians and providers on how to navigate cultural issues when caring for South Asian patients, provide a basis for future investigations regarding barriers to behavior change, and direct researchers and community organizations on how to design interventions for this rapidly growing population.
Methods
Search Strategies
We reviewed recent and past literature using OVID Med-line, OVID Embase, OVID Social Work Abstracts, Pub Med, Google Scholar, and Web of Science. Key search terms included South Asian, Asian Indian, Pakistan, Bangladesh, Sri Lanka, cardiovascular disease, diabetes, lifestyle modification, behavior change, education, and attitudes and beliefs. We also reviewed the references to capture articles missed in our search.
Inclusion and Exclusion Criteria
Articles were included if they met the following inclusion criteria: (a) written in English (b) focused on South Asian populations outside of the Indian subcontinent (c) explored diet and exercise behavior modification (d) explored cultural barriers to behavior change. We focused on diet and exercise behaviors because of their importance in the prevention and treatment of cardiovascular disease and diabetes. In our search, we found 91 articles that studied diet and exercise behavior in migrant South Asians. Of these, 24 discussed South Asian customs and belief systems and their relation to lifestyle behavior change. Preference was given to articles using qualitative methods as these gave more in-depth information regarding cultural beliefs and perceptions regarding lifestyle behavior change. These articles are outlined in Table 2.
Table 2.
Cited primary articles examining migrant South Asians cultural influences on behaviour change
| Author | Methods | Summary | Issues discussed |
|---|---|---|---|
| Tremblay [38] | Sample: 171,513 individuals across 8 ethnic groups who participated in the Canadian Community Health Survey. Method: Cross- sectional questionnaire. | Examined the change in physical activity after immigration in immigrant groups in Canada | Physical activity misconceptions |
| Astin [44] | Sample: 45 South Asian patients, 37 South Asian care givers, 20 White-European patients, 17 White-European care givers. Qualitative study in the UK using semi-structured individual interviews. | Explored the differences between South Asian and Caucasian patients’ family support and family members’ roles | Gender roles, cultural identity |
| Farooqi [45] | Sample: 6 focus groups of 12 South Asians over 40. Qualitative study in UK using focus group analysis. | Explored attitudes towards lifestyle risk factors to identify cultural barriers to behavior change | Gender roles, cultural identity |
| Kalra [46] | Sample: 8 focus groups of Asian Indians in Northern California. Qualitative study using focus group analysis. | Identified community and cultural factors that influenced approach to CVD prevention by using focus groups to evaluate perceptions regarding CVD risk | Gender roles, cultural identity |
| Visram [47] | Sample: Individual and focus group interviews with 9 South Asian women participating in a cardiac rehab exercise intervention in a UK community. Qualitative study using semi- structured interviews. | Examined how cultural factors and lack of confidence are barriers to starting cardiac rehab by interviewing staff and clients of a cardiac rehabilitation program | Gender roles |
| Sriskantharajah [48] | Sample: 15 South Asian women with CHD or diabetes in a UK community. Exploratory qualitative study with semi-structured interviews. | Identified cultural barriers to exercise in interviews with South Asian women | Gender roles, physical activity misconceptions |
| Lawton [49] | Sample: 32 South Asian patients with diabetes in a UK community. Qualitative study with individual semi-structured interviews. | Explored social and cultural issues that contributed to low physical activity levels in South Asian patients | Gender roles, physical activity misconceptions, cultural priorities |
| Netto [50] | Sample: 6 focus groups of South Asian men and women in a UK community. Qualitative study with longitudinal action research approach: focus group interviews before and after an action research project. | Discussed the need to address cultural, social, historical, environmental and psychological forces in designing an intervention through focus group interviews | Gender roles, cultural identity |
| Khanam [51] | Sample: 25 Bangladeshis in East London felt to be overweight by their GPs and referred to a gym. Method: Questionnaire with additional open-ended questions. | Identified cultural beliefs and attitudes that affected approach to physical activity in Bangladeshi women | Gender roles |
| Abbott [52] | Sample: 6 focus groups of providers who have many Bangladeshi patients. Method: Focus group interviews using semi-structured interviews. | Examined primary care providers’ perceptions on how language, religion, and a lack of knowledge impede behavior change | Cultural priorities |
| Carroll [53] | Sample: South Asian Muslim women in 5 different districts in England and Wales. Method: Qualitative interviews in response to an exercise by prescription intervention. | Identified barriers to exercise in a pilot intervention to promote physical activity in South Asian Muslim women | Gender roles |
| Grace [54] | Sample: 17 focus groups in a community outside of London. Bangladeshis without diabetes, religious leaders and scholars, and health professionals were interviewed. Method: Qualitative focus group semi-structured interviews. | Explored beliefs and attitudes toward healthy lifestyle choices in British Bangladeshis | Gender roles, cultural identity |
| Bush [55] | Sample: 259 UK South Asian, Italian, and general population of women. Method: Cross- sectional study using silhouettes to assess perceptions of body image. | Explored body image perceptions in South Asian, Italian, and general population of women in the UK | Body image |
| Darr [58] | Sample: 45 South Asians and 20 Caucasians in West Yorkshire, UK admitted to hospital for angina. Qualitative study in UK using semi- structured interviews. | Discussed difficulties with behavior change in South Asian and Caucasian patients | Gender roles, cultural priorities, cultural identity, explanatory model of disease |
| Lawton [61] | Sample: 23 Pakistanis and 9 Asian Indians with type 2 diabetes in Edinburgh, UK Method: Qualitative study using individual semi- structured interviews. | Explored South Asian patients’ attitudes toward their traditional diet | Cultural identity |
| Vallianatos [62] | Sample: Arabic and South Asian women in a small Canadian community. Method: Focus group semi-structured interviews. | Explored the meaning of food to South Asian women and their experiences maintaining ethnic cuisine in a new country | Cultural identity |
| Stone [63] | Sample: 15 South Asian and 5 Caucasian patients in Leicester, UK Method: Individual semi-structured interviews with diabetic patients. | Examined attitudes and experiences that promote and hinder behavior change in South Asians | Cultural identity |
| Keval [64] | Sample: 18 Asian Indian type 2 diabetic patients in 3 UK communities. Method: Qualitative study using individual semi-structured interviews. | Explored how South Asians use their life experiences, history, and social and cultural community to manage their medical conditions | Cultural identity |
| Lawton [67] | Sample: 32 Caucasian and 32 South Asian diabetic patients in Edinburgh, UK Method: Qualitative study using individual, in-depth interviews. | Explored beliefs regarding disease management and self responsibility in Caucasians and South Asians | Explanatory model of disease |
| Grewal [68] | Sample: 53 South Asians and 509 Caucasians from 2 hospitals in Ontario, Canada. Method: Cross-sectional study using Medical Outcomes Study Social Support Scale and Illness Perception Questionnaire. | Examined perceptions regarding CAD causation in Caucasians and South Asians | Explanatory model of disease |
| Rhodes [69] | Sample: 12 Bangladeshi diabetic patients in Bradford, UK Method: Qualitative study using individual in-depth interviews | Examined Bangladeshi patients’ experiences and struggles interacting with healthcare providers | Explanatory model of disease |
| Kandula [71] | Sample: 270 South Asians recruited from health centers in the Chicago area. Method: Cross- sectional study using surveys to assess perceptions of CHD. | Explored knowledge and perception of CVD Risk among South Asian immigrants | Explanatory model of disease |
| Tirodkar [70] | Sample: 75 South Asian patients from a federally qualified health center and community center in Chicago. Method: Qualitative study using individual semi- structured interviews. | Identified cultural, spiritual, physical, and psychosocial influences on beliefs regarding disease causation in South Asian immigrants | Explanatory model of disease |
Results
Gender Roles
Men and women have distinct roles in the typical South Asian household. The male (husband or father) is traditionally the head of the household and the decision maker, whereas the female (wife or mother) is responsible for food preparation and raising children. Although these responsibilities have become more shared in many Caucasian families, migrant South Asians have maintained these distinctions within their own households. A study conducted in West Yorkshire, UK, comparing family support of Caucasian and South Asian patients undergoing cardiac rehab found that in South Asian families, it is the male head of the household that exerts influence over dietary decisions, and hence is from where much of the resistance to dietary modification emanates. Although this study only involved patients undergoing cardiac rehab, patients and their caregivers were interviewed, specifically generating rich qualitative data on gender roles within families. Frequently, even if the female spouse seeks to make dietary changes to accommodate her husband’s health needs, she is unable to do so because her husband refuses to sacrifice taste. Women also are less likely to make dietary changes even if they are the family member with the health issue requiring diet modification. The entire family is expected to make modifications for the male’s medical condition, but not vice versa. In these instances, some females have described preparing a separate dish for themselves. However, the extra time and labor required to do this have caused these women to revert to their previous cooking methods [44].
Some households, for example, in which extended families live together, are dominated instead by the most senior or eldest persons living in the home. The dietary decisions in these households are made by the eldest female in the household. Younger women have expressed difficulties making healthy dietary changes due to the resistance they encounter by their parents or grandparents [44–46].
Further, the expected roles of women in the South Asian household are often a deterrent to starting an exercise regimen as well. Numerous qualitative studies conducted in South Asian communities in the UK have discussed how the majority of household and familial responsibilities fall on women, leaving little time to exercise. Although these studies had small sample sizes, they were able to recruit patients with various subethnic and religious backgrounds, and were able to successfully engage South Asian patients by conducting interviews in native languages. In many South Asian families, it was felt that women should not even designate time in one’s daily schedule to exercise [45, 47–50]. In a study where one on one individual interviews were conducted with South Asian women with CHD or diabetes from 3 primary care practices in the UK, subjects discussed how devoting time to exercise is viewed as taking time away from caring for the family, cooking, and tending to children’s needs, and therefore is felt to be culturally inappropriate in their families and communities. This view was more commonly held among older women [48]. Another study which explored barriers to physical activity using one on one interviews in South Asian diabetic patients in Edinburgh, UK found that for many women in South Asian families, any spare time is expected to be utilized to help benefit the family, such as by helping with the family business or by finding other ways to bring in more income [49]. In certain households, male members do not want their wives to go outside and exercise [47–49, 51]. For instance, the female figure in the home is expected to be available in order to provide food for the male when he wants it, making it hard or even unacceptable for women to leave the home [49, 52]. These views are often upheld by others in the community. As a result, a woman who is seen exercising or even going for a walk outside may be looked down upon, as is her family [53].
Although it is changing, traditionally, South Asian culture has emphasized physical separation between men and women. Hence, in regards to physical activity, many women only feel comfortable in female specific facilities and feel that it is culturally inappropriate to exercise around men. The absence of separation in most exercise facilities and gyms often dissuades South Asian females from taking advantage of exercise programs or joining a health club [48, 53]. Muslim South Asian women encounter additional cultural barriers to exercise related to the clothing they wear. The amount of traditional clothing worn by women on a day to day basis after immigrating varies. While many South Asian women wear western clothing daily, a substantial number wear traditional clothing every day. Maintaining these codes creates uncertainties about if and how to assimilate into society or utilize available services in one’s new community. For instance, many women are uncertain how they will be viewed by others, particularly those unfamiliar with their cultural practices, if they wear their hijab or traditional clothing while exercising outdoors or at an exercise facility. The fear that others will stare or talk about them, and thus make them feel uncomfortable, discourages many women from starting any form of physical activity [54].
Body Image
In western societies, much of the motivation to eat well and to be physically active stems from body images that favor being slim. However, for many South Asian immigrants, larger body types are associated with sound health, which affects the motivation to engage in healthy lifestyle behaviors. Among South Asians, attitudes towards body image depend on the context of the outcome. One cross-sectional study compared body image perceptions among migrant South Asians, Italians, and the general population of women 20–40 years of age in the UK The study did recruit immigrant and British-born South Asians and Italians, but was not able to delve deeply into body image perceptions since it was a survey-based study asking subjects to choose preferred body types designated by silhouettes. Nevertheless, all 3 groups overwhelmingly felt that the thinnest body types were beneficial for finding a spouse, a good job, and longevity. However, when asked to choose which silhouettes were most likely to have eaten healthy foods, give birth to healthy children, and be a healthy woman, 42% of migrant South Asians chose a silhouette depicting a woman with a BMI over 28, whereas only 8% of migrant Italians and 4% of the general population chose that silhouette [55]. The reason for this is that a thin body type is preferred when looking for a husband. However, a woman is expected to gain weight and “fill out” after marriage and not doing so is seen as a sign of a stressful marriage [56]. Furthermore, South Asians were less likely to have attempted to lose weight in the past and less likely to feel external pressure to lose weight, reflecting how, to a certain extent, women with higher BMIs are accepted and preferred in South Asian culture [55]. These beliefs concerning healthy weight and body image are obstacles that mitigate the motivation towards exercise and diet control.
Physical Activity Misconceptions
In general, South Asians immigrants tend to have lower levels of physical activity than other ethnic groups [57]. Much of this stems from culture and attitudes on the subcontinent itself. Within South Asian countries, there is not much emphasis on physical activity for health reasons (such as cardiovascular health, obesity, decreasing risk of type 2 Diabetes, bone and muscle strength, improved mood and mental health, maintaining ability to do daily activities upon aging) and as a result, many South Asians have not been brought up to exercise or participate in organized sports [49]. As South Asians immigrate to new communities, this unfamiliarity with the concept of physical activity hinders them from starting an exercise program when advised to do so by providers in their new communities. However, this apprehension often decreases with time. A Canadian study evaluating different immigrant groups revealed that physical activity increases with time since immigration. The largest difference was found in South Asian immigrant groups. South Asians that had lived in Canada longer tended to be more physically active compared to more recent immigrants [38]. Nevertheless, this unfamiliarity with physical activity has led to a variety of perceptions that further impede behavior change for migrant South Asians. Among some, there is anxiety concerning the physical effects of exercise, particularly that feelings of breathlessness and a rapid heart rate are signs of illness rather than normal physiological responses to exercise [49]. There is a fear of having these symptoms and not knowing what they mean, which discourages one to exercise on his or her own, particularly among those who do not speak English and are not able to ask for assistance [48].
Cultural Priorities
Despite the apprehension of exercising, the social priorities inherent among immigrant South Asians often makes it difficult to routinely exercise. The constraints felt by family responsibilities are not only limited to women of South Asian descent. In the previously mentioned qualitative study in Yorkshire, UK, men, in different ways, also expressed that there was not enough time to engage in physical activity. Although not primarily responsible for taking care of the household, immigrant South Asian men place much emphasis on spending the majority of their time providing for or helping their family. Although this is not uniquely a South Asian phenomenon, it is a barrier that many South Asian men identify with [49, 52, 58]. It is believed that time outside of work should not be spent on ‘leisure’ activities for oneself such as exercising, but instead should be used to help or care for other relatives or for spending time with their children. Even for men, exercising is looked upon as taking time out for oneself and is deemed culturally inappropriate. This belief is particularly strong among migrant South Asians, most of whom have sacrificed a great deal to leave their homelands and to provide better lives for their family and children. As a result of immigration, many South Asians rely on starting, managing, or working in businesses that open early and close late, such as shops or restaurants [49]. In fact, in a study of Asian Indians in the US, it was found that engaging in health promoting behaviors, such as exercise, was negatively related to the number of hours worked [59]. Many South Asians who have emigrated share the belief that South Asians have a strong work ethic and they take pride in the fact that this is part of their belief system and believe that it distinguishes them in their new communities. As a result, it has become almost expected to sacrifice health and physical activity for one’s work and family [49, 60].
Maintaining Cultural Identity
For many migrant South Asians, reconciling advice on lifestyle behavior with their own cultural practices is very challenging, particularly when it regards dietary change. Unique customs that immigrants have brought with them are a great source of pride and identity, and holding onto these customs is a high priority. A central component of South Asian culture revolves around food and the unique qualities and blend of ingredients, oils, and spices that are part of the traditional South Asian diet. The fundamental role that food plays in South Asian culture affects attitudes toward dietary modification. One qualitative study in Leicester, UK utilized 6 different focus groups of South Asians of various religious backgrounds and purposely sampled individuals above the age of 40 in order to gain in-depth perspectives on culturally specific attitudes from those at higher risk of heart disease. A common belief among South Asians was that since their diet had been passed down for generations and because it is perceived that the earlier ancestors did not struggle with CVD, the traditional South Asian diet cannot be unhealthy or linked to heart disease [45]. Another common perception among vegetarian South Asians is that the absence of meat in their diet is healthy and a protective factor for CVD [46]. Additionally, many South Asians exhibit a resistance to change their cooking practices. Many hold the belief that their foods and vegetables are meant to be fried and not baked or broiled and changing their cooking method would require a sacrifice in taste and signify a transition away from their traditional diet [45, 61].
Food is a central component of South Asian social gatherings and is another manner in which South Asians preserve cultural ties to their homeland [62]. At these gatherings, it is considered unacceptable to turn down certain foods, increasing the struggle to maintain dietary change [58, 61]. In large communities, there are frequent social functions where the patient cannot control how the food was prepared [44, 46, 63, 64]. On the same token, in a number of communities, it is also considered inhospitable and shameful to serve curries with reduced oil and spices [54]. In a study exploring perceptions regarding cardiovascular risk from 8 focus groups involving Asian Indians from urban, suburban, and rural communities in Northern California, participants discussed how food was a central part of the family unit. They felt that giving food, particularly food that contains butter and milk, is a nurturing act, one given from the wife or mother to the rest of the family. Reducing butter and milk content is felt like depriving, oneself, one’s family, or one’s guests. However, there were some generational differences in opinions as well. Younger women would want to give children low fat or skim milk. However, the older generation of women resisted this change, asserting that giving low fat milk would be taking nutrients away from them [46].
Nevertheless, in the qualitative study investigating the food practices of South Asians in Edinburgh, UK, the majority of the respondents expressed that the South Asian diet was at least partially responsible for the high prevalence of type 2 diabetes in their communities. However, even among these respondents, there’s a stringent defense of the cultural importance of their diet. Even though many felt that foods such roti (a type of flat bread), rice and foods prepared using ghee (a form of clarified butter) can be “dangerous” for their health, they strongly felt that these were staples, considering them the foundation of their diet and who they are as a people. There is significant pride in the flavor and flare of South Asian foods compared to British or American foods which are thought to be bland [61]. Regardless of how much one believes the South Asian diet contributes to disease, the overarching theme is that the diet is of central importance to their identity. Suggestions from physicians or dieticians often challenge some of the core principles of the South Asian diet, and it is felt that following these suggestions, would make one less Indian, Pakistani, Bangladeshi, or Sri Lankan, and more American or British, and therefore are met with a great deal of resistance [61]. These responses appear to reflect misconceptions regarding dietary change. Many do not believe it is possible to modify their dietary habits or cooking practices while still maintaining the inherent cultural and ethnic qualities of their diet. Some families, however, have started to make the necessary changes such as baking foods and using less oil [46]. Additionally, immigrants that have lived in the US longer have been more flexible in making changes to their diet, reducing the amount of ghee that is used or decreasing carbohydrate intake [65]. Much of the data regarding difficulty with dietary change has been generated from interviews with middle-aged to older South Asians and may not consistently apply to second generation South Asian immigrants. Nevertheless, reconciling dietary modification with maintenance of cultural identity is one of the most challenging barriers to healthy lifestyle modification in South Asians.
Explanatory Model of Disease
Unique qualities of an ethnic group’s belief structure and explanatory model of illness also affect attitudes towards lifestyle behaviors. Perceptions regarding self-control over disease causation are an important determinant in behavior change; individuals who do not believe their lifestyle factors contribute to acquiring disease are less likely to engage in healthy lifestyle behaviors [66]. The belief that acquiring diseases such as diabetes or CVD is not under one’s own control is prevalent among South Asians. This can partially be explained by a heavy spiritual foundation found in South Asian culture. There is the belief that much of life is in a higher power’s control and therefore not under one’s own control. Along the same lines, many migrant South Asians believe that acquiring diabetes or CVD is due to fate [58, 67, 68]. One underlying factor which perpetuates these beliefs is difficulty in explaining disease causation between close friends and families. Even though many South Asians are able to reiterate that diet and exercise are important to reduce the occurrence of diabetes or CVD, they still do not feel like this offers sufficient explanation to why their husband, wife, mother, father, or sibling developed CVD or diabetes. Many have observed that their family members have adopted healthy lifestyles and still acquired disease [46]. Additionally, one can trace this view of disease causation to access to care on the South Asian subcontinent itself. In resource limited areas, such as the South Asian subcontinent, access to western medicine is expensive and limited. Most of the population in Bangladesh, for instance, uses traditional healers and thus, diseases are often understood in terms of humoral imbalances or supernatural factors, rather than environmental or lifestyle factors [69].
Nevertheless, it is not only this perspective that makes up the South Asians’ belief structure, but also the concept that other uncontrollable external factors are mostly to blame for acquiring conditions like diabetes or CVD. A comparative qualitative study in Edinburgh, UK using individual, in-depth interviews to explore illness perceptions among 32 Caucasian and 32 South Asian diabetics revealed a marked difference in beliefs regarding responsibility for diabetes and was able to deeply delve into perceptions regarding disease causation. The sense of individual responsibility was a central theme to Caucasians’ responses to disease causation but was notably lacking in the South Asians’ responses. South Asians more frequently attributed disease to external factors and rarely to their own habits [67]. One of those external factors involves psychological stress [68]. Additionally, in a study which used open-ended interviews to examine views on heart disease etiology and prevention among South Asians in Chicago 20–75 years of age, psychosocial factors were often mentioned as contributing to disease [70]. Stress is one of the most frequently mentioned contributors to heart disease and diabetes among South Asians, regardless of age or generation [58, 67, 70, 71]. Many migrant South Asians feel that their immigrant status- living and adjusting to life in another country- adds to the regular stressors of life [58, 72]. The struggle to maintain one’s ethnic and cultural identity often augments the stresses of finding work and raising children. Yet, data from the INTER-HEART study found that stress was less of a contributor to heart disease in South Asians than in other ethnic groups [24, 70]. Overly attributing the development of CVD to stress has led to a de-emphasis on diet and exercise behavior among South Asians.
In the above mentioned qualitative studies exploring beliefs regarding diet and exercise habits, most South Asians are able to express the link between these factors and disease. However, in the comparative qualitative study examining illness perceptions between Caucasians and South Asians in Edinburgh, deeper analysis uncovered how South Asians’ cultural belief system influences views on these lifestyle factors. Many feel that they are not able to control habits such as their diet. They attribute causality of unhealthy lifestyle habits to external factors, and not internal ones. For example, immigration to a new country, lack of food options, and long work hours were blamed for unhealthy dietary practices [67]. Perceptions regarding individual responsibility and causation of a disease are significant hurdles clinicians and researchers face in influencing lifestyle behavior change in migrant South Asians.
Discussion
Some of the most difficult and frustrating tasks for clinicians involve inspiring their patients to employ healthy lifestyle behaviors involving food intake and physical activity. A number of barriers exist for the general population, including access to healthier and cheaper food, access to markets, knowledge about healthy eating practices, and a means to be physically active. However, for certain ethnic groups, certain aspects of their culture impart additional barriers to behavior change. These cultural mores can conflict with western concepts of healthy lifestyle practices. For migrant South Asians, culture takes on even more importance than it did in their homeland. Immigrant groups in general, due to the sheer nature of not being immersed in a society that shares their customs, often hold on to certain beliefs and cultural practices more rigidly than their friends who have remained at home. As a result, influencing behavior change, particularly when the changes are perceived to clash with one’s own customs is particularly difficult in these groups.
The aspects of South Asian culture outlined above are all inter-related, although some beliefs may be more important in some families and communities than in others. However, they are all issues that must be considered when caring for migrant South Asian populations. Due to the interplay between South Asian culture and behavior change, providers may need to spend additional time discussing difficulties with dietary improvements and physical activity with their South Asian patients. Additionally, physicians and dieticians should discuss lifestyle factors with the entire family when caring for a diabetic patient or a patient at risk for diabetes or CVD. It has been shown that interventions that have recruited husbands to participate can overcome the traditional resistance to dietary change from male family members [73]. Providers must gain an understanding of the cultural importance of the South Asian diet as well as the cultural barriers to physical activity in order to suggest feasible ways to make changes to these lifestyle factors.
There have been a number of interventions that have targeted diet and exercise behavior change in the migrant South Asian communities. As mentioned above, educational programs, as well as programs that have involved active participation of male family members, have shown some success in dietary improvements. Other efforts have shown modest benefit or have not been evaluated for their long term performance. However, to achieve more consistent and enduring improvements, researchers must take cultural beliefs and practices into account when addressing diet and exercise behaviors. Addressing these cultural barriers as part of behavior change interventions can potentially produce great strides in convincing migrant South Asians to alter their approach to lifestyle behaviors. These approaches will most likely be successful if studied and implemented at the community level. This enables researchers and community leaders to assess and work with the customs their community strongly adheres to. Certainly it is not feasible to change customs, but when researchers work with migrant South Asian communities, how these issues will be dealt with must play a significant role in the planning process.
Conclusion
With the growing size and steady migration of this population, South Asian health issues will play an increasing role in many western nations’ overall health. Advice from health care providers that appears to contradict with cultural beliefs tends to disengage migrant South Asian communities from the medical community. Less contact between health providers and the South Asian community decreases the opportunities to encourage preventative lifestyle behaviors. Policy makers must grant more opportunities to ideas that work with South Asian community members and account for cultural factors when studying behavior change interventions. A greater emphasis on prevention of diabetes and CVD in this population will not only be beneficial to researchers and communities in creating innovative community based solutions, but make clinicians more cognizant of the health issues facing the South Asian patients they treat.
Acknowledgments
The authors would like to acknowledge Helen-Ann Brown Epstein, MLS MS AHIP for her assistance with the literature review for this manuscript. This work was supported by the Agency for Healthcare Research and Quality Grant Number T32 HS000066. Erica Phillips-Caesar and Carla Boutin-Foster are also supported by the Center for Excellence in Health Disparities Research and Community Engagement (CEDREC) NIMHD P60 MD003421-02.
Contributor Information
Mihir Patel, Email: patelmihirk@gmail.com, Department of Medicine, Divison of General Internal Medicine, St. Luke’s-Roosevelt Hospital Center, 1111 Amsterdam Avenue, New York, NY 10025, USA.
Erica Phillips-Caesar, Email: erp2001@med.cornell.edu, Division of Clinical Epidemiology and Evaluative Sciences Research, Weill Cornell Medical College, New York, NY, USA.
Carla Boutin-Foster, Email: cboutin@med.cornell.edu, Division of Clinical Epidemiology and Evaluative Sciences Research, Weill Cornell Medical College, New York, NY, USA.
References
- 1.Rangaswamy P. South Asian Diaspora. In: Ember M, Ember CR, Skoggard I, editors. Encyclopedia of the diasporas: immigrant and refugee cultures around the world. New York: Springer; 2005. pp. 285–296. [Google Scholar]
- 2.United Kingdom Office of National Statistics. Focus on Ethnicity and Identity. 2005 Mar;:2005. [Google Scholar]
- 3.US Census Bureau. Census. Summary File 1, Table DP-1. [Accessed 20 October 2010];Profile of general demographic characteristics: 2000. 2000 generated by Mihir Patel, using American FactFinder; http://factfinder.census.gov.
- 4.US Census Bureau. [Accessed 20 October 2010];American Community Survey, 2009 Summary Tables; generated by Mihir Patel; using American Fact-Finder. http://factfinder.census.gov.
- 5.Enas EA. Heart disease among Indians living abroad. How to beat the heart disease epidemic among south asians downers grove: advanced heart lipid clinic. 2005:24–30. [Google Scholar]
- 6.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104(23):2855–2864. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Shaping the future. Geneva: WHO; 2003. [Accessed July 31, 2010]. The World Health Report 2003; p. 2003. Available at: http://www.who.int/whr/2003/chapter6/en/index1.html. [Google Scholar]
- 8.Balarajan R. Ethnicity and variations in the nation’s health. Health Trends. 1995;27:114–119. [PubMed] [Google Scholar]
- 9.Danaraj TJ, Acker MS, Danaraj W, Ong WH, Yam TB. Ethnic group differences in coronary heart disease in Singapore: an analysis of necropsy records. Am Heart J. 1959;58:516–526. doi: 10.1016/0002-8703(59)90085-7. [DOI] [PubMed] [Google Scholar]
- 10.Lee J, Heng D, Chia KS, Chew SK, Tan BY, Hughes K. Risk factors and incident coronary heart disease in Chinese, Malay and Asian Indian males: the Singapore cardiovascular cohort study. Int J Epidemiol. 2001;30(5):983–988. doi: 10.1093/ije/30.5.983. [DOI] [PubMed] [Google Scholar]
- 11.U.K. Department of Health. [Accessed Oct 14, 2011];Health Survey for England: the health of minority ethnic groups’99 The Stationery Office 2001. Available at http://www.archive.offical-documents.co.uk/document/doh/survey99/hse99-00.htm.
- 12.Harding S. Mortality of migrants from the Indian subcontinent to England and wales: effect of duration of residence. Epidemiology. 2003;14(3):287–292. [PubMed] [Google Scholar]
- 13.McKeigue PM, Marmot MG. Mortality from coronary heart disease in Asian communities in London. BMJ. 1988;297(6653):903. doi: 10.1136/bmj.297.6653.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ashraf SS, Shaukat N, Akhtar K, Love H, Shaw J, Rowlands DJ, et al. A comparison of early mortality and morbidity after single and bilateral internal mammary artery grafting with the free right internal mammary artery. Br Heart J. 1994;72(4):321–326. doi: 10.1136/hrt.72.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the study of health assessment and risk in ethnic groups (SHARE) Lancet. 2000;356(9226):279–284. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 16.Enas EA, Yusuf S, Mehta JL. Prevalence of coronary artery disease in Asian Indians. Am J Cardiol. 1992;70(9):945–949. doi: 10.1016/0002-9149(92)90744-j. 10/1. [DOI] [PubMed] [Google Scholar]
- 17.McKeigue PM, Miller GJ, Marmot MG. Coronary heart disease in South Asians overseas: a review. J Clin Epidemiol. 1989;42(7):597–609. doi: 10.1016/0895-4356(89)90002-4. [DOI] [PubMed] [Google Scholar]
- 18.Klatsky AL, Tekawa I, Armstrong MA, Sidney S. The risk of hospitalization for ischemic heart disease among Asian Americans in northern California. Am J Public Health. 1994;84(10):1672–1675. doi: 10.2105/ajph.84.10.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004;14(7):499–506. doi: 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Sharma M, Ganguly NK. Premature coronary artery disease in Indians and its associated risk factors. Vasc Health Risk Manag. 2005;1(3):217–225. [PMC free article] [PubMed] [Google Scholar]
- 21.Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97(6):596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
- 22.Reddy KS. Cardiovascular disease in non-Western countries. N Engl J Med. 2004;350(24):2438–2440. doi: 10.1056/NEJMp048024. [DOI] [PubMed] [Google Scholar]
- 23.Yusuf S, Reddy KS, Ounpuu S, Anand S. global burden of cardiovascular diseases Part I: general considerations, the epidemiological transition, risk factors and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 24.Joshi PP, Islam S, Pais P, Reddy KS, Prabhakaran D, Kazmi K. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 25.Enas EA, Kannan S. Malignant heart disease in young Indians. How to beat the heart disease epidemic among South Asians: a prevention and management guide for Asian Indians and their doctors.: Downers Grove: Advanced Heart Lipid Clinic. 2005:34–39. [Google Scholar]
- 26.Balarajan R. Ethnic differences in mortality from ischaemic heart disease and cerebrovascular disease in England and Wales. BMJ. 1991;302(6776):560–564. doi: 10.1136/bmj.302.6776.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lovegrove JA. Are definitions of adiposity appropriate for identification of cardiovascular disease risk in South Asian populations? Nutr Bull. 2007;32(2):129–137. [Google Scholar]
- 28.Lovegrove JA. CVD risk in South Asians: the importance of defining adiposity and influence of dietary polyunsaturated fat— symposium on nutrition interventions in high-risk groups. Proc Nutr Soc. 2007;66(2):286–298. doi: 10.1017/S0029665107005514. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 30.Misra A, Pandey RM, Sinha S, Guleria R, Sridhar V, Dudeja V. Receiver operating characterisitics curve analysis of body fat & body mass index in Dyslipidaemic Asian Indians. Indian J Med Res. 2003;117:170–179. [PubMed] [Google Scholar]
- 31.Misra A, Vikram N. Insulin resistance syndrome (metabolic syndrome) and obesity in Asian Indians: evidence and implications. Nutrition. 2004;20:482–491. doi: 10.1016/j.nut.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 32.Misra A, Vikram NK, Gupta R, Pandey RM, Wasir JS, Gupta VP. Waist circumference cutoff points and action levels for Asian Indians for identification of abdominal obesity. Int J Obes. 2006;30:106–111. doi: 10.1038/sj.ijo.0803111. [DOI] [PubMed] [Google Scholar]
- 33.Eapen D, Kalra GL, Merchant N, Arora A, Khan BV. Metabolic syndrome and cardiovascular disease in South Asians. Vasc Health Risk Manag. 2009;5:731–743. doi: 10.2147/vhrm.s5172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991;337(8738):382–386. doi: 10.1016/0140-6736(91)91164-p. [DOI] [PubMed] [Google Scholar]
- 35.Hayes L, White M, Unwin N, Bhopal R, Fischbacher C, Harland J, et al. Patterns of physical activity and relationship with risk markers for cardiovascular disease and diabetes in Indian, Pakistani, Bangladeshi and European adults in a UK population. J Public Health. 2002;24(3):170–178. doi: 10.1093/pubmed/24.3.170. [DOI] [PubMed] [Google Scholar]
- 36.Khunti K, Stone MA, Bankart J, Sinfield PK, Talbot D, Farooqi A, et al. Physical activity and sedentary behaviours of South Asian and white European children in inner city secondary schools in the UK. Fam Pract. 2007;24(3):237–244. doi: 10.1093/fampra/cmm013. [DOI] [PubMed] [Google Scholar]
- 37.Fischbacher CM, Hunt S, Alexander L. How physically active are South Asians in the United Kingdom? a literature review. J Public Health. 2004;26(3):250–258. doi: 10.1093/pubmed/fdh158. [DOI] [PubMed] [Google Scholar]
- 38.Tremblay MS, Bryan SN, Pérez CE, Ardern CI, Katzmarzyk PT. Physical activity and immigrant status: evidence from the Canadian community health survey. Can J Public Health. 2006;97(4):277–282. doi: 10.1007/BF03405603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balasubramanyam A, Rao S, Misra R, Sekhar R, Ballantyne C. Prevalence of metabolic syndrome and associated risk factors in Asian Indians. J Immigr Minor Health. 2008;10(4):313–323. doi: 10.1007/s10903-007-9092-4. [DOI] [PubMed] [Google Scholar]
- 40.Merchant AT, Anand SS, Kelemen LE, Vuksan V, Jacobs R, Davis B, et al. Carbohydrate intake and HDL in a multiethnic population. Am J Clin Nutr. 2007;85(1):225–230. doi: 10.1093/ajcn/85.1.225. [DOI] [PubMed] [Google Scholar]
- 41.Yagalla MV, Hoerr SL, Song WO, Enas E, Garg A. Relationship of diet, abdominal obesity, and physical activity to plasma lipoprotein levels in Asian Indian physicians residing in the United States. J Am Diet Assoc. 1996;96(3):257–261. doi: 10.1016/S0002-8223(96)00077-6. [DOI] [PubMed] [Google Scholar]
- 42.Gupta R, Gupta VP, Sarna M, Bhatnagar S, Thanvi J, Sharma V. Prevalence of coronary heart disease and risk factors in an urban Indian population: Jaipur Heart Watch-2. Indian Heart J. 2002;54:59–66. [PubMed] [Google Scholar]
- 43.Gupta R, Misra A, Vikram NK, Kondal D, Gupta SS, Agrawal A, et al. Younger age of escalation of cardiovascular risk factors in Asian Indian subjects. BMC Cardiovasc Disord. 2009;9:28–39. doi: 10.1186/1471-2261-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Astin F, Atkin K, Darr A. Family support and cardiac rehabilitation: a comparative study of the experiences of South Asian and White-European patients and their carer’s living in the United Kingdom. Eur J Cardiovasc Nurs. 2008;7(1):43–51. doi: 10.1016/j.ejcnurse.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 45.Farooqi A, Nagra D, Edgar T, Khunti K. Attitudes to lifestyle risk factors for coronary heart disease amongst South Asians in Leicester: a focus group study. Fam Pract. 2000;17(4):293–297. doi: 10.1093/fampra/17.4.293. [DOI] [PubMed] [Google Scholar]
- 46.Kalra P, Srinivasan S, Ivey S, Greenlund K Results from focus groups conducted in Asian Indian communities in Northern California. Knowledge and practice: the risk of cardiovascular disease among Asian Indians. Ethn Dis. 2004;14(4):497–504. [PubMed] [Google Scholar]
- 47.Visram S, Crosland A, Unsworth J, Long S. Engaging women from South Asian communities in cardiac rehabilitation. Br J Community Nurs. 2007;12(1):13–8. doi: 10.12968/bjcn.2007.12.1.22686. [DOI] [PubMed] [Google Scholar]
- 48.Sriskantharajah J, Kai J. Promoting physical activity among South Asian women with coronary heart disease and diabetes: what might help? Fam Pract. 2007;24(1):71–76. doi: 10.1093/fampra/cml066. [DOI] [PubMed] [Google Scholar]
- 49.Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. ‘I can’t do any serious exercise’: barriers to physical activity amongst people of Pakistani and Indian origin with Type 2 diabetes. Health Educ Res. 2006;21(1):43–54. doi: 10.1093/her/cyh042. [DOI] [PubMed] [Google Scholar]
- 50.Netto G, McCloughan L, Bhatnagar A. Effective heart disease prevention: lessons from a qualitative study of user perspectives in Bangladeshi, Indian and Pakistani communities. Public Health. 2007;121(3):177–186. doi: 10.1016/j.puhe.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 51.Khanam S, Costarelli V. Attitudes towards health and exercise of overweight women. J R Soc Promot Health. 2008;128(1):26–30. doi: 10.1177/1466424007085225. [DOI] [PubMed] [Google Scholar]
- 52.Abbott S, Riga M. Delivering services to the Bangladeshi community: the views of healthcare professionals in East London. Public Health. 2007;121(12):935–941. doi: 10.1016/j.puhe.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 53.Carroll R, Ali N, Azam N. Promoting physical activity in South Asian muslim women through “exercise on prescription”. Health Technol Assess. 2002;6(8) doi: 10.3310/hta6080. http://www.hta.ac.uk/fullmono/mon608.pdf. [DOI] [PubMed] [Google Scholar]
- 54.Grace C, Begum R, Subhani S, Kopelman P, Greenhalgh T. Prevention of type 2 diabetes in British Bangladeshis: qualitative study of community, religious, and professional perspectives. BMJ. 2008;337:a1931. doi: 10.1136/bmj.a1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bush HM, Williams RGA, Lean MEJ, Anderson AS. Body image and weight consciousness among South Asian, Italian and general population women in Britain. Appetite. 2001;37(3):207–215. doi: 10.1006/appe.2001.0424. [DOI] [PubMed] [Google Scholar]
- 56.Kishwar M. When India missed the universe. Manushi. 1995;88:9–19. [Google Scholar]
- 57.Palaniappan L, Anthony M, Mahesh C, Elliott M, Killeen A, Giacherio D, et al. Cardiovascular risk factors in ethnic minority women aged ≤30 years. Am J Cardiol. 2002;89(5):524–529. doi: 10.1016/s0002-9149(01)02291-3. [DOI] [PubMed] [Google Scholar]
- 58.Darr A, Astin F, Atkin K. Causal attributions, lifestyle change, and coronary heart disease: illness beliefs of patients of South Asian and European origin living in the United Kingdom. Heart Lung J Acute Critical Care. 2008;37(2):91–104. doi: 10.1016/j.hrtlng.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 59.Misra R, Gupta R. Predictors of health promotion behavours among Asian Indian immigrants: implications for Practitioners. Int J Sociol Soc Policy. 2004;24(12):66–86. [Google Scholar]
- 60.Pardhan S, Mahomed I. Knowledge, self-help and socioeconomic factors in South Asian and Caucasian diabetic patients. Eye (Lond) 2004;18(5):509–513. doi: 10.1038/sj.eye.6700680. [DOI] [PubMed] [Google Scholar]
- 61.Lawton J, Ahmad N, Hanna L, Douglas M, Bains H, Hallowell N. ‘We should change ourselves, but we can’t’: accounts of food and eating practices amongst British Pakistanis and Indians with type 2 diabetes. Ethn Health. 2008;13(4):305–319. doi: 10.1080/13557850701882910. [DOI] [PubMed] [Google Scholar]
- 62.Vallianatos H, Raine K. Consuming food and constructing identities among Arabic and South Asian immigrant women. Food Culture Society. 2008;11(3):355–373. [Google Scholar]
- 63.Stone M, Pound E, Pancholi A, Farooqi A, Khunti K. Empowering patients with diabetes: a qualitative primary care study focusing on South Asians in Leicester UK. Fam Pract. 2005;22(6):647–652. doi: 10.1093/fampra/cmi069. [DOI] [PubMed] [Google Scholar]
- 64.Keval H. Cultural negotiations in health and illness: the experience of type 2 diabetes among Gujarati-speaking South Asians in England. Divers Health Care. 2009;6(4):255–265. [Google Scholar]
- 65.Raj S, Ganganna P, Bowering J. Dietary habits of Asian Indians in relation to length of residence in the United States. J Am Diet Assoc. 1999;99(9):1106–1108. doi: 10.1016/S0002-8223(99)00266-7. [DOI] [PubMed] [Google Scholar]
- 66.MacInnes JD. The illness perceptions of women following acute myocardial infarction: implications for behaviour change and attendance at cardiac rehabilitation. Women Health. 2006;42(4):105–121. doi: 10.1300/j013v42n04_06. [DOI] [PubMed] [Google Scholar]
- 67.Lawton J, Ahmad N, Peel E, Hallowell N. Contextualising accounts of illness: notions of responsibility and blame in white and South Asian respondents’ accounts of diabetes causation. Sociol Health Illn. 2007;29(6):891–906. doi: 10.1111/j.1467-9566.2007.01036.x. [DOI] [PubMed] [Google Scholar]
- 68.Grewal K, Stewart DE, Grace SL. Differences in social support and illness perceptions among South Asian and Caucasian patients with coronary artery disease. Heart Lung J Acute Critical Care. 2010;39(3):180–187. doi: 10.1016/j.hrtlng.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 69.Rhodes P, Nocon A, Wright J. Access to diabetes services: the experiences of Bangladeshi people in Bradford, UK. Ethn Health. 2003;8(3):171–188. doi: 10.1080/1355785032000136407. [DOI] [PubMed] [Google Scholar]
- 70.Tirodkar M, Baker D, Makoul G, Khurana N, Paracha M, Kandula N. Explanatory models of health and disease among South Asian immigrants in Chicago. J Immigr Minor Health. 2011;13(2):385–394. doi: 10.1007/s10903-009-9304-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kandula N, Tirodkar M, Lauderdale DS, Makoul G, Paracha MW, Baker D. Awareness, perception, and knowledge of heart disease risk and prevention among South Asian immigrants. J Gen Intern Med. 2009;24(Supplement 1):S29. [Google Scholar]
- 72.Baylav A. Overcoming culture and language barriers. Practitioner. 1996;240(1563):403–406. [PubMed] [Google Scholar]
- 73.Davies J, Damani P, Margetts B. Intervening to change the diets of low-income women. Proc Nutr Soc. 2009;68:210–215. doi: 10.1017/S0029665109001128. [DOI] [PubMed] [Google Scholar]