Abstract
Purpose of Review
Atherosclerosis and associated cardiovascular disease (CVD) still remain the largest cause of mortality worldwide. Several recent studies have discovered that metabolism of common nutrients by gut microbes can produce a proatherogenic metabolite called trimethylamine-N-oxide (TMAO). The goal of this review is to discuss emerging evidence that the hepatic enzyme that generates TMAO, flavin monooxygenase 3 (FMO3), plays a regulatory role in maintaining whole body cholesterol balance and atherosclerosis development.
Recent Findings
Several independent studies have recently uncovered a link between either FMO3 itself or its enzymatic product TMAO with atherosclerosis and hepatic insulin resistance. These recent studies show that inhibition of FMO3 stimulates macrophage reverse cholesterol transport (RCT) and protects against atherosclerosis in mice.
Summary
A growing body of work demonstrates that nutrients present in high fat foods (phosphatidylcholine, choline, and L-carnitine) can be metabolized by the gut microbial enzymes to generate trimethylamine (TMA), which is then further metabolized by the host enzyme FMO3 to produce proatherogenic TMAO. Here we discuss emerging evidence that the TMAO producing enzyme FMO3 is centrally involved in the pathogenesis of atherosclerosis by regulating cholesterol metabolism and insulin resistance, and how these new insights provide exciting new avenues for CVD therapies.
Keywords: atherosclerosis, reverse cholesterol transport, insulin resistance, trimethylamine-N-oxide
Introduction
Cardiovascular disease affects approximately one in three adults in the United States, posing a significant public health burden that is only expected to grow due to increasing incidences of obesity and diabetes [1]. Atherosclerosis, a chronic disease driven by hypercholesterolemia and associated accumulation of cholesterol-laden macrophages in the artery wall, is the underlying cause of a majority of clinical cardiovascular events including myocardial infarction, angina, heart failure and stroke [1]. While there is clear evidence supporting genetic variation as an underlying cause of some cardiovascular disease risk [2-4], only approximately 11% of all coronary artery disease cases are attributable to genetic heritability [5]; therefore, the majority of research has focused on the role environmental factors play in atherosclerotic disease progression. Within the last decade, the gut microbiome has been recognized as an important endocrine organ that not only augments our nutrient metabolism, but can contribute to host pathologies such as obesity [6] and more recently cardiovascular disease. Clinical studies have demonstrated a striking correlation between cardiovascular disease and circulating levels of trimethylamine N-oxide (TMAO) [7-12], the production of which is dependent on microbiome and host synergism. First, gut microbes produce the gas trimethylamine (TMA), a product of metabolic precursors choline [10, 13, 14], L-carnitine [8], and betaine [7] which are derived from foods rich in phosphatidylcholine including red meat, poultry, fish, and eggs [15]. TMA is then oxidized by host hepatic flavin monooxygenase 3 (FMO3) into the proatherogenic compound TMAO [16]. Indeed, there is a positive correlation between FMO3 expression levels and TMAO production among mouse strains prone to atherosclerosis [16], highlighting the importance of FMO3 itself in the development of cardiovascular disease. While the biology of atherosclerosis development and progression [17-20] and the relationship between gut microbial environments and cardiovascular risk [21-24] have been highlighted in a number of recent reviews, the purpose of this review is to focus on the latest developments on the role of FMO3 in lipid metabolism and atherosclerosis.
Flavin Monooxygenases
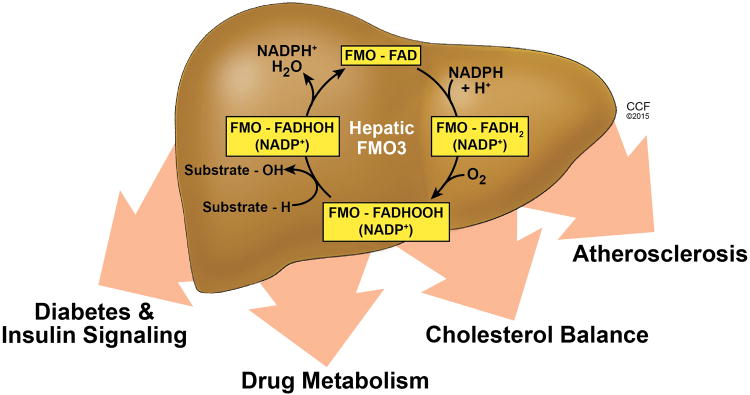
The family of flavin monooxygenases (FMO) is made up of five major isoforms (FMO1-5) capable of catalyzing the oxygenation of numerous nucleophilic sulfur- and nitrogen-containing xenobiotics, including TMA, and endogenous substrates in the adult liver [25]. FMO family members contain a single FAD that undergoes a two-electron reduction by NADPH in the first step of the catalytic cycle. Once reduced, the FMO enzyme reacts with molecular O2 to form a peroxyflavin intermediate, which, in turn, transfers one atom of O2 to a nucleophilic substrate (such as TMA) and the other atom to water (Fig. 1). Of note, a study in isolated microsomes demonstrates that in the presence of substrate, somewhere between 30 and 50% of O2 consumed by FMO1, FMO2, and FMO3 appears as H2O2 [26], suggesting that FMOs may play an important role in cellular redox.
Figure 1.
The trimethylamine-N-oxide (TMAO) generating enzyme flavin monooxygenase 3 (FMO3) regulates hepatic drug metabolism, diabetes and insulin signaling, cholesterol balance, and atherosclerosis development.
FMO1 and FMO3 are the two major hepatic FMO isoforms that efficiently catalyze the formation of TMAO from gut microbe-derived TMA. However, a recent report demonstrates that, of the two, FMO3 exhibits a 10-fold higher specific activity towards TMA [16]. The inability to oxidize TMA to TMAO presents in humans as trimethylaminuria or “fish odor syndrome”, a rare metabolic disease in which excessive TMA accumulates and is released into the patient's urine, sweat and breath producing a strong, fishy body odor. Early studies demonstrate that primary trimethylaminuria occurs in patients with mutations in the gene encoding FMO3, and is inherited following an autosomal recessive pattern [27-29]. Genetic analysis of patients with inherited trimethylaminuria demonstrates that the lack of FMO3 enzymatic activity often arises from mutations affecting the binding of necessary cofactors FAD [30] or NADPH [31]. As a result, patients are encouraged to maintain a diet low in fat and choline to minimize TMA production [32]. However, future therapeutics may include microbial intervention, such as the introduction of microorganisms that metabolize and deplete TMA [33].
FMO3 gene expression is regulated by a complex network of genetic and dietary factors. Interestingly, hepatic FMO3 expression patterns display robust sexual dimorphism in both mice and humans, with both FMO3 expression and circulating TMAO levels being significantly higher in females [16]. Additionally, a survey of 22 atherosclerosis-susceptible mouse strains demonstrates that female mice developed larger atherosclerotic lesions than their male genetic counterparts [34], providing a link between FMO3 gene expression and proatherogenic TMAO production [16]. Comparing male mice with intact testes to male mice that have been gonadectomized demonstrates that both hepatic FMO3 expression and TMAO generation are repressed by testosterone, while parallel studies in female mice demonstrate a positive correlation between estrogen and FMO3 gene expression. Furthermore, an estrogen receptor α binding site has been identified in the promoter region of FMO3 in both mouse and human samples [35]. Of note, the incidence of trimethylaminuria reported is higher among females, with patients reporting a worsening of symptoms occurring during menstruation [36].
FMO3 gene expression has also been shown to be transcriptionally regulated by farnesoid x receptor (FXR) signaling [16]. The FMO3 gene has an FXR response element within its promoter, and treatment of mice with either an FXR agonist or the bile acid cholic acid leads to increases in FMO3 gene expression and concomitant elevations in plasma TMAO concentrations [16]. Nonetheless, FMO3's production of TMAO is also highly dependent on TMA delivery by the intestinal microbiota, which in turn is influenced by both host nutrient consumption and intestinal bacterial diversity. In fact, dietary delivery of TMA precursors carnitine and choline fail to elicit atherosclerotic lesion development in apolipoprotein E (ApoE)-/- mice treated with poorly absorbed broad-spectrum oral antibiotics [8, 10]. Distinct cecal microbial taxa have been identified whose proportions are associated with elevated TMA or TMAO levels [8] and bioinformatics studies reveal the presence of choline fermentation gene clusters (cut, which include choline TMA-lyase, cutC/D) across a range of human gut bacteria populations [37]. Importantly, Gregory and colleagues recently demonstrated that transplantation of gut microbes with enhanced ability to raise circulating TMAO was sufficient to transmit susceptibility to atherosclerosis in ApoE-/- mice [38]. Furthermore, quantitative trait loci analysis in mouse models with differing susceptibility to atherosclerosis development identified several single nucleotide polymorphisms within the FMO3 gene [39]. Collectively, the metaorganismal TMA/FMO3/TMAO pathway has emerged as an attractive new target for CVD [21, 23, 40], but much additional work is needed in order to identify points of therapeutic intervention.
FMO3 is A Modifier of Cholesterol Metabolism and Atherosclerosis
In a seminal study, Wang and colleagues utilized a metabolomic platform to identify circulating small molecules that predicted risk of CVD development in humans [10]. This study identified that choline, phosphatidylcholine, betaine, and TMAO were all shown to predict risk of CVD in several independent large clinical cohorts [10]. Importantly, within the last year, several laboratories have independently uncovered the same TMA/FMO3/TMAO pathway as driving chronic disease in genetically modified mouse models of altered cholesterol metabolism and insulin resistance [40-42]. Much like the original study by Wang and colleagues, these new studies have uncovered the importance of the gut microbe-driven TMA/FMO3/TMAO pathway by using unbiased screening approaches to understand novel disease mechanisms. Given the fact that this pathway has now been discovered in three independent screens using distinct models of cardiometabolic disease, there is strong rationale to target this pathway for atheroprotection.
A powerful new example of how the TMA/FMO3/TMAO pathway links to CVD comes from studies in mice with hepatic insulin resistance [40]. It has long been know that type II diabetes is a major risk factor for developing CVD. Given this link, Miao and colleagues recently used metabolomic profiling to identify novel hepatic targets of insulin action relevant to the development of CVD [40]. Using mice lacking hepatic insulin receptors (liver insulin receptor knockout mice, “LIRKO”) as a model of selective insulin resistance, they observed a 2.5-fold increase in plasma TMAO concentrations which was accompanied by a >1000 fold increase in hepatic FMO3 mRNA levels and robust expression of FMO3 protein in male mice [40]. Furthermore, studies in primary hepatocytes confirm that insulin represses and glucagon elevates FMO3 gene expression [40]. Antisense oligonucleotide (ASO)-mediated knockdown of FMO3 in LIRKO mice significantly improves glucose tolerance and promotes reductions in the expression of several gluconeogenic genes, all of which are targets of transcription factor Foxo1. In fact, Foxo1 protein levels are significantly reduced in LIRKO mice following FMO3 knockdown [40]. The authors propose a mechanistic link between FMO3 and Foxo1 expression via SREBP-2, the levels of which are significantly reduced in LIRKO livers, but normalized following FMO3 knockdown [40]. It was recently shown that SREBP-2 activates a microRNA (miRNA) locus that encodes miR-182 [43], which has been shown to suppress FoxO1 gene expression [43-45]. In line with this, Miao and colleagues demonstrate that overexpression of SREBP-2 in primary hepatocytes was sufficient to both overexpress miR-182 and suppress Foxo1 protein. In contrast, studies in streptozotocin-treated liver specific Foxo1 knockout mice demonstrate that Srebp-2 gene expression, as well as expression of several cholesterol biosynthesis genes that are known SREBP-2 targets, are significantly upregulated [44], suggesting that the regulatory effects of SREBP-2 on Foxo1 may not be unidirectional. Nonetheless, LIRKO mice, which have been shown to be susceptible to atherosclerosis when maintained on an atherogenic diet [46], are completely protected from atherogenesis when FMO3 is knocked down [40]. These FMO3 ASO-treated LIRKO mice had significantly decreased levels of circulating VLDL and LDL-associated cholesterol as well as an increase in the LDL receptor [40], which collectively likely play a predominant role in the atheroprotection seen. Taken together, these recent data demonstrate an important role for FMO3 in the development of both insulin resistance and atherosclerosis, possibly through the regulation of Foxo1 signaling. However, additional work is needed to fully understand mechanisms by which FMO3 enzymatic activity regulates Foxo1 expression in the liver.
In agreement with these studies, Shih and colleagues recently reported that ASO-mediated knockdown of hepatic FMO3 attenuates atherosclerosis development in LDL receptor knockout (Ldlr-/-) mice [42]. Despite lesion macrophage content commensurate with control ASO-treated Ldlr-/- mice, atherosclerotic lesion area is significantly reduced in FMO3 ASO-treated Ldlr-/- maintained on a high cholesterol diet. As seen in the study by Miao and colleagues [40], FMO3 knockdown significantly reduces the levels of VLDL and LDL cholesterol in LDLr-/- mice, which is likely the driving force of atheroprotection in this model. Interestingly, hepatic knockdown of FMO3 also corresponded with significantly decreased expression of genes involved in gluconeogenesis and lipogenesis [42]. Because dietary supplementation of FMO3 product TMAO did not significantly affect plasma glucose or lipid levels of ApoE-/- mice [8, 10], the authors propose the possibility of a yet unknown physiological FMO3 substrate that influences hepatic lipid and glucose metabolism.
In parallel to these atherosclerosis studies, our group independently identified the TMA/FMO3/TMAO pathway as a key regulator of reverse cholesterol transport (RCT) [41]. To identify novel regulators of the non-biliary branch of RCT, we performed a transcriptional profiling screen in mouse models where the non-biliary pathway was selectively enhanced. Results from this screen identified FMO3 as being coordinately down-regulated in both acute [47] and chronic [48] mouse models of stimulated non-biliary RCT. Interestingly, knockdown of FMO3 significantly altered multiple aspects of cholesterol balance including intestinal cholesterol absorption, hepatic cholesterol ester storage, and macrophage RCT in a dietary cholesterol-dependent fashion [41]. Importantly, FMO3 knockdown potently stimulated both basal and liver X receptor (LXR)-stimulated macrophage RCT, which likely contributes to the atheroprotection seen with FMO3 ASO treatment in other recent studies [40, 42]. However, inhibition of hepatic FMO3 also causes unwanted recruitment of macrophages into the liver resulting in severe hepatic inflammation and endoplasmic reticulum (ER) stress [41]. This unexpected deleterious effect of FMO3 inhibition likely involves diminished hepatic LXR signaling, given that oxysterol ligand abundance is severely diminished in FMO3 ASO treated mice, and the fact that provision of endogenous (dietary cholesterol) or exogenous (T0901317) LXR agonists blunts FMO3 ASO-driven hepatic inflammation [41]. To determine the involvement of gut microbial metabolites TMA and TMAO in the ability of FMO3 ASOs to reorganize cholesterol balance and hepatic inflammation, we suppressed gut microbial communities using a poorly absorbed cocktail of antibiotics or provided exogenous TMAO in the diet. Importantly, the administration of antibiotics to suppress any gut microbial generation of FMO3 substrate TMA normalizes intestinal cholesterol absorption and fecal neutral sterol loss in FMO3 ASO-treated mice, but does not diminish hepatic inflammation. On the other hand, dietary supplementation with TMAO fails to normalize cholesterol balance or hepatic inflammation in FMO3 ASO-treated mice. These results suggest that, although chronic elevation of TMAO can be proatherogenic in mice, TMAO is likely not involved in the ability of FMO3 inhibition to reorganize cholesterol balance and hepatic inflammation. Therefore, through mechanisms independent of its enzymatic product TMAO, FMO3 appears to act as an important regulatory switch integrating cholesterol balance and hepatic inflammatory responses.
Conclusion
The recent discovery linking the meta-organismal TMA/FMO3/TMAO pathway to CVD risk in humans has broad implications in the field of cardiovascular medicine. Furthermore, recent studies showing that inhibition of FMO3 reorganizes hepatic insulin resistance and cholesterol metabolism strengthen the rationale to target this pathway for therapeutic intervention. While the ability of TMAO to promote atherosclerosis has been shown in numerous studies [7-12], it remains possible that TMAO's proatherogenic potential may be mutually exclusive from the ability of FMO3 inhibitors to reorganize cholesterol balance and hepatic inflammation [41]. Therefore, it will become increasingly important to identify the repertoire of substrates that can be utilized by FMO3, and to explore the possibility that FMO3 may have regulatory functions distinct from its enzymatic activity. Given that FMO3 inhibition and gain of function reciprocally reorganize cholesterol balance, inflammation, and ER stress [41] FMO3 is uniquely positioned among the FMO family of enzymes to impact human disease. However, further studies are warranted to determine whether this pathway can be exploited pharmacologically in lipid- or inflammatory-driven diseases. Of particular relevance to novel therapeutic interventions for atherosclerosis, the identification of FMO3 substrates and products that play a primary role in promoting non-biliary macrophage RCT, without increasing hepatic inflammation, would be an attractive strategy for novel cholesterol lowering drugs in the post statin era. Advancement in our understanding of the enzymology of FMO3 is thus predicted to not only be informative in xenobiotic toxicology studies, but also may provide insights into novel therapeutic strategies for the treatment or prevention of atherosclerotic CVD.
Key Points.
Hepatic expression of the enzyme flavin monooxygenase 3 (FMO3) is altered in mouse models of stimulated non-biliary reverse cholesterol transport and hepatic insulin resistance.
The FMO3 enzymatic product trimethylamine-N-oxide has been linked to cardiovascular disease risk in humans.
Inhibition of FMO3 promotes non-biliary reverse cholesterol transport and protects mice against atherosclerosis.
Therapies targeting gut microbe-driven TMA/FMO3/TMAO pathway hold promise for prevention or treatment of cardiovascular disease.
Acknowledgments
Illustrations were created by David Schumick, B.S, C.M.I, and reprints are available with the permission of the Cleveland Clinic Center for Medical Art & Photography © 2015
Financial Support and Sponsorship: This work was supported by grants provided by the National Institutes of Health: R00 HL096166 (J.M.B.), and R01 HL122283 (J.M.B.).
Abbreviations
- ASO
antisense oligonucleotide
- ApoE
apolipoprotein E
- CVD
cardiovascular disease
- FAD
flavin adenine dinucleotide
- FMO3
flavin monooxygenase 3
- FXR
farnesoid X receptor
- HDL
high density lipoprotein
- LDL
low density lipoprotein
- NADPH
nicotinamide adenine dinucleotide phosphate
- RCT
reverse cholesterol transport
- TMA
trimethylamine
- TMAO
trimethylamine-N-oxide
Footnotes
Conflicts of interest: None.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Teslovich TM, Musunuru K, Smith AV, et al. Biological, clinical and population relevance of 95 loci for blood lipids. Nature. 2010;466:707–13. doi: 10.1038/nature09270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kathiresan S, Voight BF, Purcell S, et al. Genome-wide association of early-onset myocardial infarction with single nucleotide polymorphisms and copy number variants. Nat Genet. 2009;41:334–41. doi: 10.1038/ng.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kathiresan S, Willer CJ, Peloso GM, et al. Common variants at 30 loci contribute to polygenic dyslipidemia. Nat Genet. 2009;41:56–65. doi: 10.1038/ng.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deloukas P, Kanoni S, Willenborg C, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2013;45:25–33. doi: 10.1038/ng.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turnbaugh PJ, Ley RE, Mahowald MA, et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 7*.Koeth RA, Levison BS, Culley MK, et al. γ-Butyrobetaine is a proatherogenic intermediate in gut microbial metabolism of L-carnitine to TMAO. Cell Metab. 2014;20:799–812. doi: 10.1016/j.cmet.2014.10.006. γButyrobetain is shown to be the major gut microbial metabolite formed from dietary L-carnitine in mice. γButyrobetain is converted into TMA (and then TMAO) in a gut microbiota-dependent manner, and accelerates atherosclerosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koeth RA, Wang Z, Levison BS, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19:576–85. doi: 10.1038/nm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang WH, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368:1575–84. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472:57–63. doi: 10.1038/nature09922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Z, Tang WH, Buffa JA, et al. Prognostic value of choline and betaine depends on intestinal microbiota-generated metabolite trimethylamine-N-oxide. Eur Heart J. 2014;35:904–10. doi: 10.1093/eurheartj/ehu002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang WH, Wang Z, Shrestha K, et al. Intestinal microbiota-dependent phosphatidylcholine metabolites, diastolic dysfunction, and adverse clinical outcomes in chronic systolic heart failure. J Card Fail. 2015;21:916. doi: 10.1016/j.cardfail.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.al-Waiz M, Mikov M, Mitchell SC, et al. The exogenous origin of trimethylamine in the mouse. Metabolism. 1992;41:135–6. doi: 10.1016/0026-0495(92)90140-6. [DOI] [PubMed] [Google Scholar]
- 14.Miller CA, Corbin KD, da Costa KA, et al. Effect of egg ingestion on trimethylamine-N-oxide production in humans: a randomized, controlled, dose-response study. Am J Clin Nutr. 2014;100:778–86. doi: 10.3945/ajcn.114.087692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeisel SH, Mar MH, Howe JC, et al. Concentrations of choline-containing compounds and betaine in common foods. J Nutr. 2003;133:1302–7. doi: 10.1093/jn/133.5.1302. [DOI] [PubMed] [Google Scholar]
- 16.Bennett BJ, de Aguiar Vallim TQ, Wang Z, et al. Trimethylamine-N-oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab. 2013;17:49–60. doi: 10.1016/j.cmet.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tabas I, Garcia-Cardena G, Owens GK. Recent insights into the cellular biology of atherosclerosisa. J Cell Biol. 2015;209:13–22. doi: 10.1083/jcb.201412052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moore KJ, Sheedy FJ, Fisher EA. Macrophages in atherosclerosis: a dynamic balance. Nat Rev Immunol. 2013;13:709–21. doi: 10.1038/nri3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hilgendorf I, Swirski FK, Robbins CS. Monocyte fate in atherosclerosis. Arterioscler Thromb Vasc Biol. 2015;35:272–9. doi: 10.1161/ATVBAHA.114.303565. [DOI] [PubMed] [Google Scholar]
- 20.Lovren F, Teoh H, Verma S. Obesity and atherosclerosis: mechanistic insights. Can J Cardiol. 2015;31:177–83. doi: 10.1016/j.cjca.2014.11.031. [DOI] [PubMed] [Google Scholar]
- 21.Brown JM, Hazen SL. Metaorganismal nutrient metabolism as a basis of cardiovascular disease. Curr Opin Lipidol. 2014;25:48–53. doi: 10.1097/MOL.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown JM, Hazen SL. The gut microbial endocrine organ: bacterially derived signals driving cardiometabolic diseases. Annu Rev Med. 2015;66:343–59. doi: 10.1146/annurev-med-060513-093205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tang WH, Hazen SL. The contributory role of gut microbiota in cardiovascular disease. J Clin Invest. 2014;124:4204–11. doi: 10.1172/JCI72331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ussher JR, Lopaschuk GD, Arduini A. Gut microbiota metabolism of L-carnitine and cardiovascular risk. Atherosclerosis. 2013;231:456–61. doi: 10.1016/j.atherosclerosis.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 25.Cashman JR, Zhang J. Human flavin-containing monooxygenases. Annu Rev Pharmacol Toxicol. 2005;46:65–100. doi: 10.1146/annurev.pharmtox.46.120604.141043. [DOI] [PubMed] [Google Scholar]
- 26.Siddens LK, Krueger SK, Henderson MC, et al. Mammalian flavincontaining monooxygenase (FMO) as a source of hydrogen peroxide. Biochem Pharmacol. 2014;89:141–7. doi: 10.1016/j.bcp.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Akerman BR, Lemass H, Chow LM, et al. Trimethylaminuria is caused by mutations of the FMO3 gene in a North American cohort. Mol Genet Metab. 1999;68:24–31. doi: 10.1006/mgme.1999.2885. [DOI] [PubMed] [Google Scholar]
- 28.Cashman JR, Bi YA, Lin J, et al. Human flavin-containing monooxygenase form 3: cDNA expression of the enzymes containing amino acid substitutions observed in individuals with trimethylaminuria. Chem Res Toxicol. 1997;10:873–41. doi: 10.1021/tx9700533. [DOI] [PubMed] [Google Scholar]
- 29.Treacy EP, Akerman BR, Chow LM, et al. Mutations of the flavincontaining monooxygenase gene (FMO3) cause trimethylaminuria, a defect in detoxication. Hum Mol Genet. 1998;7:839–45. doi: 10.1093/hmg/7.5.839. [DOI] [PubMed] [Google Scholar]
- 30.Zhang J, Tran Q, Lattard V, et al. Deleterious mutations in the flavincontaining monooxygenase 3 (FMO3) gene causing trimethylaminuria. Pharmacogenetics. 2003;13:495–500. doi: 10.1097/00008571-200308000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Fujieda M, Yamazaki H, Togashi M, et al. Two novel single nucleotide polymorphisms (SNPs) of the FMO3 gene in Japanese. Drug Metab Pharmacokinet. 2003;18:333–5. doi: 10.2133/dmpk.18.333. [DOI] [PubMed] [Google Scholar]
- 32.Busby MG, Fischer L, da Costa KA, et al. Choline- and betaine-defined diets for use in clinical research and for the management of trimethylaminuria. J Am Diet Assoc. 2004;104:1836–45. doi: 10.1016/j.jada.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 33.Brugere JF, Borrel G, Gaci N, et al. Archaebiotics: proposed therapeutic use of archaea to prevent trimethylaminuria and cardiovascular disease. Gut Microbes. 2014;5:5–10. doi: 10.4161/gmic.26749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bennett BJ, Orozco L, Kostem E, et al. High-resolution association mapping of atherosclerosis loci in mice. Atherscler Thromb Vasc Biol. 2012;32:1790–8. doi: 10.1161/ATVBAHA.112.253864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Esposito T, Varriale B, D'Angelo R, et al. Regulation of flavin-containing mono-oxygenase (Fmo3) gene expression by steroids in mice and humans. Horm Mol Biol Clin Investig. 2014;20:99–109. doi: 10.1515/hmbci-2014-0012. [DOI] [PubMed] [Google Scholar]
- 36.Krueger SK, Williams DE. Mammalian flavin-containing monooxygenases: structure/function, genetic polymorphisms and role in drug metabolism. Pharmacol Ther. 2005;106:357–87. doi: 10.1016/j.pharmthera.2005.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martinez-Del Campo A, Bodea S, Hamer HA, et al. Characterization and detection of a widely distributed gene cluster that predicts anaerobic choline utilization by human gut bacteria. MBio. 2015;6:e00042–15. doi: 10.1128/mBio.00042-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38*.Gregory JC, Buffa JA, Org E, et al. Transmission of atherosclerosis susceptibility with gut microbial transplantation. J Biol Chem. 2015;290:5647–60. doi: 10.1074/jbc.M114.618249. Transplantation of gut microbes with enhanced ability to raise circulating TMAO was sufficient to transmit susceptibility to atherosclerosis prone mice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kayashima Y, Makhanova NA, Matsuki K, et al. Identification of aortic arch-specific quantitative trait loci for atherosclerosis by an intercross of DBA/2J and 129S6 apolipoprotein E-deficient mice. PLoS ONE. 2015;10:e0117478. doi: 10.1371/journal.pone.0117478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40**.Miao J, Ling AV, Manthena PV, et al. Flavin-containing monooxygenase 3 as a potential player in diabetes-associated atherosclerosis. Nat Commun. 2015 doi: 10.1038/ncomms7498. In Press. FMO3 knockdown in insulin-resistant mice suppresses Foxo1 and prevents the development of hyperglycaemia, hyperlipidemia and atherosclerosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41**.Warrier M, Shih DM, Burrows AC, et al. The TMAO-Generating Enzyme Flavin Monooxygenase 3 Is a Central Regulator of Cholesterol Balance. Cell Rep. 2015;10:326–338. doi: 10.1016/j.celrep.2014.12.036. FMO3 is identified as a central integrator of hepatic cholesterol and triacylglycerol metabolism, inflammation, and ER stress: FMO3 knockdown stimulates basal and liver X receptor-stimulated macrophage RCT, improving cholesterol balance, while simultaneously exacerbating hepatic endoplasmic reticulum stress and inflammation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42*.Shih DM, Wang Z, Lee R, et al. Flavin containing monooxygenase 3 exerts broad effects on glucose and lipid metabolism and atherosclerosis. J Lipid Res. 2015;56:22–37. doi: 10.1194/jlr.M051680. Knockdown of hepatic FMO3 in LDL receptor knockout mice results in decreased circulating TMAO levels and atherosclerosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jeon TI, Esquejo RM, Roqueta-Rivera M, et al. An SREBP-responsive microRNA operon contributes to a regulatory loop for intracellular lipid homeostasis. Cell Metab. 2013;18:51–61. doi: 10.1016/j.cmet.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guttilla IK, White BA. Coordinate regulation of FOXO1 by miR-27a, miR-96, and miR-182 in breast cancer cells. J Biol Chem. 2009;284:23204–16. doi: 10.1074/jbc.M109.031427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim KM, Park SJ, Jung SH, et al. miR-182 is a negative regulator of osteoblast proliferation, differentiation, and skeletogenesis through targeting FoxO1. J Bone Miner Res. 2012;27:1669–79. doi: 10.1002/jbmr.1604. [DOI] [PubMed] [Google Scholar]
- 46.Stittrich AB, Haftmann C, Sgouroudis E, et al. The microRNA miR-182 is induced by IL-2 and promotes clonal expansion of activated helper T lymphocytes. Nat Immunol. 2010;11:1057–62. doi: 10.1038/ni.1945. [DOI] [PubMed] [Google Scholar]
- 47.Marshall SM, Gromovsky AD, Kelley KL, et al. Acute sterol oacyltransferase 2 (SOAT2) knockdown rapidly mobilizes hepatic cholesterol for fecal excretion. PLoS ONE. 2014;9:e98953. doi: 10.1371/journal.pone.0098953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Temel RE, Sawyer JK, Yu L, et al. Biliary sterol secretion is not required for macrophage reverse cholesterol transport. Cell Metab. 2010;12:96102. doi: 10.1016/j.cmet.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]