Abstract
Rapid buildup of greenhouse gases is expected to increase the Earth surface mean temperature, with unclear effects on temperature variability1–3. This adds urgency to better understand the direct effects of the changing climate on human health. However, the effects of prolonged exposures to temperatures, which are important for understanding the public health burden, are unclear. Here we demonstrate that long-term survival was significantly associated with both seasonal mean values and standard deviations (SDs) of temperature among the Medicare population (aged 65+) in New England, and break that down into long-term contrasts between ZIP codes and annual anomalies. A rise in summer mean temperature of 1 °C was associated with 1.0% higher death rate whereas an increase in winter mean temperature corresponded to 0.6% lower mortality. Increases in temperature SDs for both summer and winter were harmful. The increased mortality in warmer summers was entirely due to anomalies, while it was long term average differences in summer SD across ZIP codes that drove the increased risk. For future climate scenarios, seasonal mean temperatures may in part account for the public health burden, but excess public health risk of climate change may also stem from changes of within season temperature variability.
Emissions of greenhouse gases will change the Earth’s climate, most notably by changing temperature and temperature variability1. The Intergovernmental Panel on Climate Change (IPCC), in its newly released fifth assessment report, forecasts a rise in world average temperature ranging from 0.2–5.5 °C by 21001. This has increased interest in the impact of temperature on health.
While many studies have reported associations between short-term temperature changes and increased daily deaths4–11, evidence on the association between annual mortality and changes in seasonal temperature averages is scarce12,13. Since such impacts by definition cannot be short-term mortality displacement (we are looking at annual averages and displacement of deaths by a few weeks will not influence these), these results can imply important public health effects of the changing climate. In addition to the seasonal mean temperature, its variability may also play a significant role in raising the risk of mortality12,14. There is evidence that people adapt to the usual temperature in their city14,15. For these reasons, this study focused on both mean temperature, and temperature variability for summer and winter.
Conventionally, ambient temperature (Ta) was obtained from monitors near airports, and analyzed at the city or county level16. Overlooking the temporal and spatial variation of the Ta may introduces an exposure measurement error and may bias health effect estimates17. We recently presented new hybrid models of assessing high-resolution spatio-temporal Ta for epidemiological studies, based on surface temperature (Ts) measured by satellite. This approach allows prediction of daily Ta at 1 × 1 km spatial resolution throughout the New England area18. We also showed that using high-resolution Ta predicted from the hybrid models better captured the associations between Ta and adverse health outcomes than temperature data from existing monitoring stations19.
Using temporally- and spatially-resolved Ta estimates, the present study aims to tease apart the associations of annual all-cause mortality with seasonal mean temperature and with temperature variability for both summer and winter, among the Medicare population in New England during 2000–2008, and to further separate these into long term spatial differences and annual anomalies. Temperature variability is represented by the standard deviation (SD) of daily mean temperature within season.
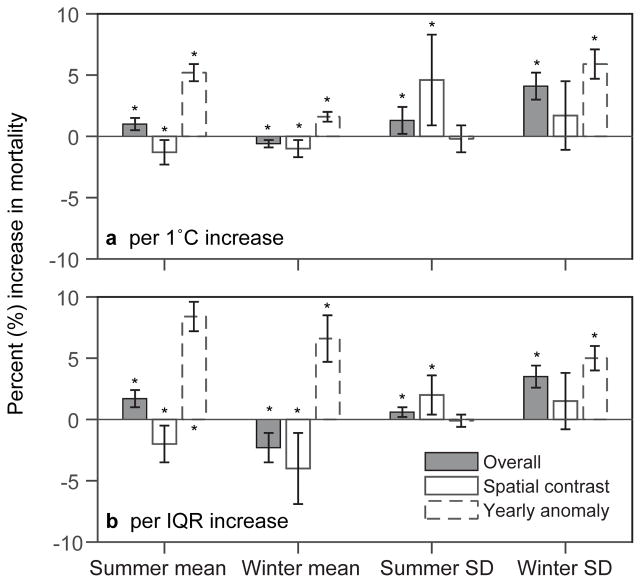
The results, presented as percent increase in mortality, are shown in Fig. 1 for spatial contrasts, annual anomalies, and the overall effect estimates. Both seasonal mean temperatures and temperature SDs were significantly associated with all-cause mortality for summer and winter (p<0.05). A rise of 1 °C in summer mean temperature corresponded to an overall estimated 1.0% increase in mortality (95% CI: 0.6, 1.5%). This was entirely due to yearly anomalies; living in a location with long-term warmer summer temperatures in New England was associated with lower mortality rates, suggesting acclimatization. A 1 °C increase in winter mean temperature was observed to lower mortality by 0.6% (95% CI: 0.3, 0.9%). Here, it was the spatial contrast that was associated with lower mortality, and the anomalies with higher mortality, suggesting little acclimatization to cold. For each 1 °C increase in temperature SDs, 1.3% (95% CI: 0.2, 2.4%) and 4.1% (95% CI: 3.0, 5.2%) increases in annual deaths were seen in summer and winter, respectively. The observed associations in summer and winter were respectively attributable to spatial contrasts and yearly anomalies.
Figure 1. Percent increase in mortality for per 1 °C and per Interquartile Range (IQR) increases in seasonal mean temperature and temperature variability across New England, 2003–2008.
IQR is defined as; IQR = third quartile – first quartile which reflects the current distribution of these variables. A sensitivity analysis controlling for the number of heat waves in each ZIP code in each year found essentially identical results. Error bars stand for 95% confidence intervals. * p < 0.05.
A key result of this study is that increases in temperature variability can have similar estimated effects on mortality as increases in mean temperature. This makes understanding the effect of climate change on seasonal temperature variability important for assessing health risks. In addition, we found that small area variations in long term average temperature and temperature SD across New England are associated with differences in mortality rates, which are quite different from the associations with anomalies. In particular they suggest even within New England, places with typically warmer summers have lower annual mortality rates while anomalies are associated with higher annual mortality rates in that year. Hence the negative health impacts of climate change may stem from the increase in year-to-year fluctuations of temperature from a level that people have been acclimated to for a long time, or an increase in daily variability within season, rather than the warmer temperature itself.
Short-term associations between daily temperature and mortality have been reported to be greater in locations with larger seasonal temperature variability9,14. Several recent studies suggested that a large change in temperature between neighboring days can elevate daily mortality10,11. Hence temperature variability emerges as an important risk factor for both short-term and long-term survival.
Subjects exercising in hot conditions for 12 days doubled their endurance time, while subjects alternately exercising in mild and hot conditions did not20. This suggests that more temperature variability in the summer can impede adaptation, which is consistent with our associations with seasonal SD. However, the underlying mechanisms for the observed relationship with seasonal mean temperature remain unresolved. That more people die when summers are warmer or when winters are colder than normal for their ZIP code may be due to accumulating effects over the season on the changes in blood pressure associated with short-term change in temperature, or lack of behavioral response.
Our results also suggest that living in warmer ZIP codes in New England reduced long-term mortality in both summer and winter, but living in ZIP codes with more variable temperature in either summer or winter increased mortality. In addition, higher annual anomalies were significantly associated with increased long-term mortality, though insignificantly for summer temperature SD.
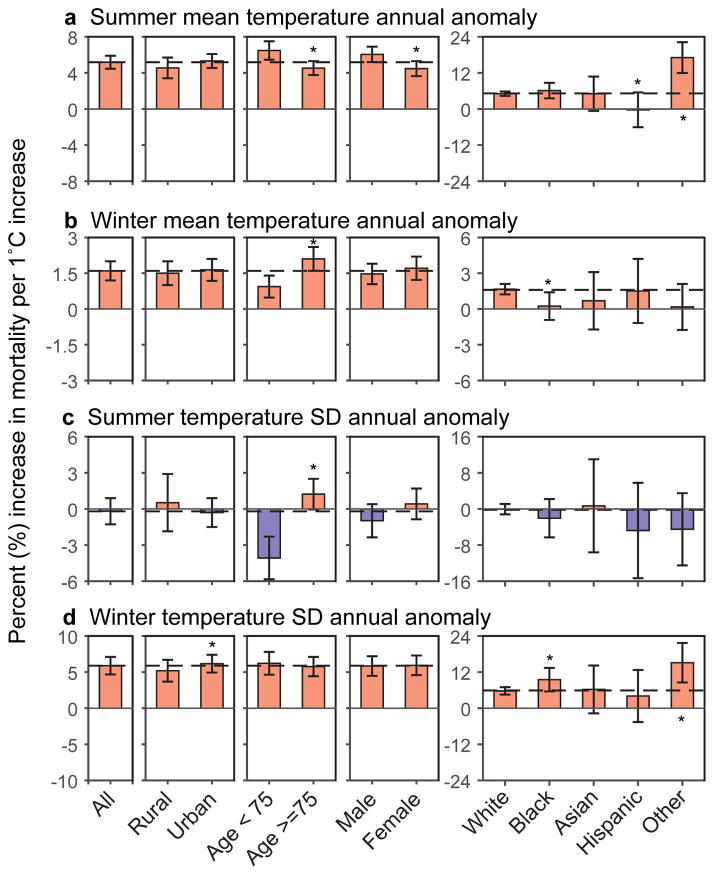
We also examined effect modifications (Fig. 2 and 3). For seasonal mean temperature anomalies, consistent increases in mortality rates for positive anomalies were seen across the groups (cf. Fig. 2). While some differences were statistically significant (e.g., between males and females for summer mean), the differences in effects were not large except for some noise in smaller racial groups. Anomalies for the SD of temperature within winter also showed consistently positive associations across group. Summer temperature SD anomalies showed no association with mortality overall, but opposite effects by age, with higher mortality rates in persons 75+, and lower rates in 65–75.
Figure 2. Modifications of the effect for annual anomalies of different temperature indices by population density, age, sex, and race.
It displays the percent increases of death (95% CI) for each 1 °C increase in (a) summer mean temperature annual anomaly (b) winter mean temperature annual anomaly (c) summer temperature standard deviation annual anomaly (d) winter temperature standard deviation annual anomaly in each subgroup, respectively. Red indicates increased risk of death, and blue stands for decreased risk of death. Error bars stand for 95% confidence intervals. * p < 0.05.
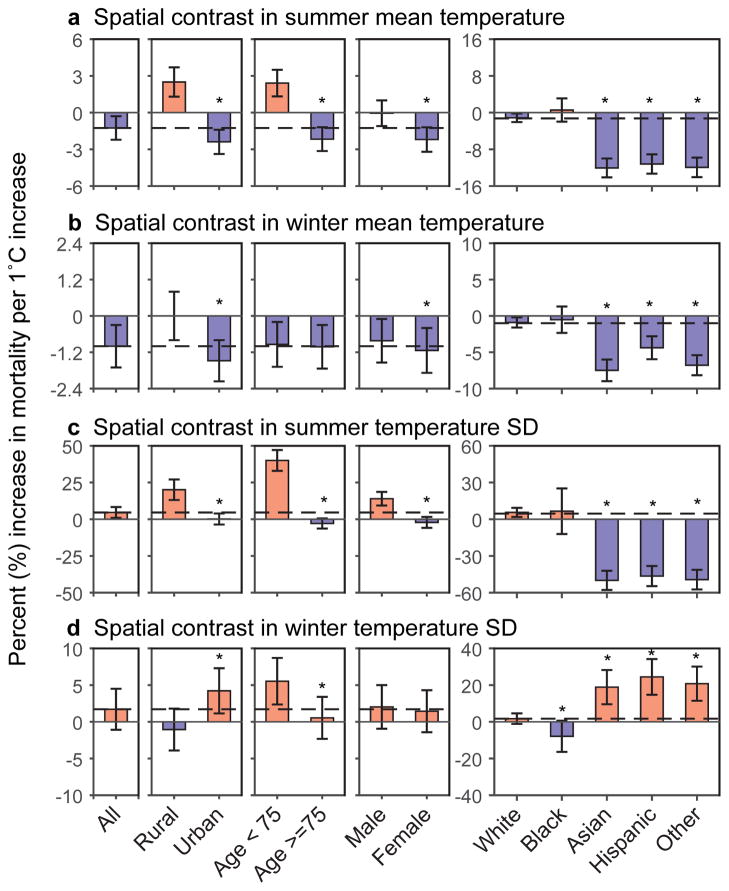
Figure 3. Modifications of the effect for spatial variability in different temperature indices by population density, age, sex, and race.
It displays the percent increases of death (95% CI) for each 1 °C increase in (a) spatial contrasts of summer mean temperature (b) spatial contrasts of winter mean temperature (c) spatial contrasts of summer temperature standard deviation (d) spatial contrasts of winter temperature standard deviation in each subgroup, respectively. Red indicates increased risk of death, and blue stands for decreased risk of death. Error bars stand for 95% confidence intervals. * p < 0.05.
For ZIP code differences in the long term means of the temperature parameters, more heterogeneity was seen across population groups (cf. Fig. 3). Higher effect estimates were found in less dense areas for both mean and SD of summer temperature. This is consistent with a recent study suggesting that subjects in rural counties were more vulnerable to heat21. We also found that subjects in urban areas benefited more from living in regions with warmer winters but were at higher risk for elevated winter temperature variability. In addition, the relatively younger age group (65–74 y) was more sensitive to the changes of most temperature indices. This may be due to their having more outdoor activities than the older age group. A similar reason may also explain why in summer higher effect estimates were found for subjects living in rural areas. However in the cold and snowy winter of New England, possibly outdoor activities of studied subjects in rural areas were limited, therefore winter mean temperature and SD had lower effect estimates for subjects in rural areas than that in urban. Females were more sensitive to increased mean temperature in summer and winter but less sensitive to increased summer temperature SD compared to males. We saw a number of interactions by race that are not always easy to understand. It is possible that the decreased risk of death in locations with higher summer mean temperatures in Asian, Hispanic and “other” race group is because elderly subjects in these groups immigrated from warm areas, such as South China, Southeast Asia, India, and Mexico. These subjects were more acclimated to a warmer summer. This could also explain that Asian, Hispanic and “other” race groups significantly benefited more from a warmer winter, but were more adversely impacted by greater winter SD. However, we note that the percent of the population over 65 in New England that is not white is only 5.9%, and for 4.3% ZIP codes was zero, so some of the observed variability across race may result from unstable estimates.
A potential limitation of the present study is that there is still potential residual confounding resulting from the lack of individual level risk factors for mortality. In addition, bias could also be induced by spatial or temporal auto-correlation, which can lead to spuriously narrow standard errors and CIs.
Implications for future climate research
Scientific understanding of how mean surface temperature responds to the increasing anthropogenic emission of GHGs has been greatly improved in recent decades1. Considering the comparable increments of both summer and winter mean temperatures predicted for the future 50 years, the benefit of warmer winter may be largely compensated by the harm of hotter summer. However, for annual anomalies, warmer winter temperature actually increases annual mortality. The degree of temperature variability, such as the within season SD, which is influenced by many factors such as the intensity and pattern of atmospheric circulations, remains highly uncertain for future climate scenarios22,23. For example, Petoukhov and Semenov proposed that the weakening of the polar vortex may bring about increased frequency of very cold winters in northern America24. However, Huntingford and coauthors suggested that there is no significant change in global temperature variability in spite of changing regional patterns3. That study assessed variability across the entire year, including seasonal variability, and it is not clear whether variability changed within some seasons3. This uncertainty can be propagated into the projection of temperature-related health risk.
This study, by estimating impacts of both mean temperature and temperature variability in summer and winter simultaneously, adds considerable strength to the evidence of a significant association between prolonged exposures to temperatures and mortality, especially temperature variability. In addition to the within season variability we also showed that between year variability (anomalies) increased mortality risks. Hence the variability of atmospheric temperature emerges as a key factor of the potential health impacts of climate change.
This work provides an important example of how temperature may affect human health in a temperate climate region. We would expect that the health effects of seasonal mean temperature and temperature variability can vary greatly among different climate zones12. Such variation may also exist across areas with distinct socio-economical status, which can convey vulnerability to the changing climate. A quantitative assessment of the projected risk of human health associated with future climate change can be estimated world-widely by incorporating more comprehensive epidemiological studies and projected climate scenario data for different climate zones. However, as an important environmental stressor emphasized in this study, the uncertainty of the projected changes in the temperature variability can induce significant errors in such estimate. Hence better climate projections on temperature variability at multiple scales are important for the human health risk assessment.
Methods
Study Population
We constructed a cohort using Medicare data for all residents aged 65 and older for the years 2000–2008 in New England (cf. Table S1 in Supplemental Material). This was an open cohort, including eligible persons from 1999, or at the year when they subsequently turned 65. Subjects entered the cohort for survival if they were still alive on January 1st of the year following the year that they enrolled in Medicare, and follow-up years (our time metric) were calendar years. As a national social insurance program administered by the U.S. federal government since 1966, Medicare guarantees Americans aged 65 and older access to health insurance25. The Medicare beneficiary denominator file from the Centers for Medicare and Medicaid services (CMS) lists all beneficiaries enrolled in the Medicare fee-for-service (FFS), and contains information on beneficiaries’ eligibility and enrollment in Medicare, as well as the date of death.
Exposure data
The present study uses 1 × 1 km ambient temperature (Ta) data estimated from surface temperature (Ts) measured by satellites18. Specifically, we started by calibrating the Ts − Ta relationship for each day using grid cells with both Ta and Ts measurements (model 1). This daily calibration was then used to predict Ta in grid cells in the study domain without Ta measurements but with available Ts measurements. To fill in cells or days when no Ts measurements were available, a generalized additive mixed model was fit with a smooth function of latitude and longitude of the grid cell centroid (model 2). The performance of the estimated Ta was validated by ten-fold cross-validation. Out-of-sample R2 was found to be very high (R2 = 0.947, yearly variation 0.933–0.958 for the years 2000–2011) for days with available satellite Ts measurements. Excellent performance was also observed even in days with no available Ts data (R2 = 0.940, yearly variation 0.902–0.962 for the years 2000–2011). More details are published17.
By linking the ZIP code centroid to the nearest temperature grid, we assigned the grid-cell temperature exposures to each ZIP code. The predicted daily ambient temperatures allow us to calculate, for each year and each ZIP code, the mean temperature for summer (June–August), the mean temperature for winter (December–February), the standard deviation (SD) of daily mean summertime temperature, and the SD of daily mean wintertime temperature. We refer to these as summer mean temperature, winter mean temperature; summer temperature variability and winter temperature variability, respectively (cf. Table S2 in Supplemental Material). Table S2 also presents the distribution of the spatial and temporal variations for the temperature variables. Table S3 in Supplemental Material displays the correlation coefficients between these explanatory variables.
Covariates
Medicare provides information on age, race and sex of all individuals. From the U.S. Census Bureau 2000, we obtained ZIP code tabulation area level socio-economic variables, including population density, percent of green space, percent of the population (age>=65) in poverty status, and median value for owner occupied housing units. In addition, based on ZIP code level primary and secondary hospital admissions for lung cancer, we calculated the long-term average hospital admission rate for lung cancer in each ZIP code as a surrogate for smoking experience. The census data were merged with individuals based on their ZIP code of residence. County-level percent of diabetes and percent of lack of physical activity, obtained from the CDC Behavioral Risk Factor Surveillance survey for the entire country were adjusted as well.
Statistical Methods
In our dataset, one observation is created for each Medicare participant for each year of follow-up, using the Andersen Gill formulation of survival analysis. Survival times were calculated from enrollment date until death or December 31, 2008 (censoring), whichever came first.
We considered the following possible exposure indices: summer mean temperature, winter mean temperature, summertime temperature SDs and wintertime temperature SDs in each follow-up year. To separate the independent associations of mortality with mean temperature and temperature variability, all temperature-related indices were entered into the models simultaneously and treated as time-varying exposures.
We applied extended Cox proportional hazard models (Proc PHREG, SAS 9.3), which allow for time-varying covariates in survival analysis. The models were adjusted for individual risk factors including age, sex, race, ZIP code level covariates such as population density, percent of green space, percent of the population below poverty level, median value for owner occupied housing units, and hospital admission rate for lung cancer (a surrogate for smoking experience), as well as county-level percent of diabetes, and percent of lack of physical activity. To adjust for time trend, we entered an indicator for each year of follow-up. To allow for possible non-proportionality of hazard, participants were stratified by sex, 5-year age groups, and race (white, black, and others), such that each sex/age/race group had its own baseline hazard.
We then assessed the association of mortality with the four exposure indices. The analyses were also repeated without mutual adjustment for seasonal mean temperatures and temperature SDs (cf. Table S4 in Supplemental Material). To separate the contribution of the spatial and temporal components of the temperature variables, we fit a model with two terms for each temperature variable. We defined each term as its mean in that ZIP code over the entire study period plus that difference (anomaly) from that mean for ith ZIP code in tth follow-up year. With all 8 terms put in the model, the mean for each ZIP code captures purely geographic contrasts, the anomaly indicate the effects of yearly variations within each ZIP code.
The results are expressed as percent increase in mortality for each °C increase in an exposure index, for spatial contrasts, annual anomalies, and the overall effect estimates. Percent increases in mortality were also calculated for per IQR (Interquartile Range; IQR = third quartile – first quartile) increase, to reflect the current distribution of these variables. For example, an 8.4% (95% CI: 7.3, 9.6%) increase of mortality was observed for per IQR increase of yearly anomaly of summer mean temperature. This result can be interpreted as that within a ZIP code, the risk of death in a relatively warm summer (third quartile in the studied period) was 8.4% higher than in a relatively cold summer (first quartile). A sensitivity analysis controlling for the number of heat waves in each ZIP code in each year was performed as well.
We also examined age (defined as >=75 y and 65–74 y), sex, race (white, black, Asian, Hispanic, and other), and population density (less than 33th percentile, rural, and otherwise urban) as effect modifiers for both spatial contrasts and temperature anomalies respectively, by adding interaction terms between such variables and each of the eight temperature indices in the model.
Supplementary Material
Acknowledgments
This study was funded by NIEHS grant R21ES020695 and NIEHS R21ES024012. This publication was made also possible by USEPA grant (RD-83479801). Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the USEPA. Further, USEPA does not endorse the purchase of any commercial products or services mentioned in the publication. The authors also thank Lu Shen for fruitful discussions.
Footnotes
Author Contributions
J.D.S. designed research and directed its implementation; A.Z. and I.K. prepared dataset; L.S., P.L., and J.D.S. analyzed data; L.S., P.L., and J.D.S. wrote the paper, and all authors contributed to the revision of the manuscript.
Competing Financial Interests Statement
All authors declare that they have no actual or potential conflicts of interest.
References
- 1.IPCC. Climate change 2013: The physical science basis. Cambridge University Press; Cambridge, UK, and New York: 2013. [Google Scholar]
- 2.Alexander L, Perkins S. Debate heating up over changes in climate variability. Environmental Research Letters. 2013;8:041001. doi: 10.1088/1748-9326/8/4/041001. [DOI] [Google Scholar]
- 3.Huntingford C, Jones PD, Livina VN, Lenton TM, Cox PM. No increase in global temperature variability despite changing regional patterns. Nature. 2013;500:327–330. doi: 10.1038/nature12310. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease: the effects of temperature and humidity. Epidemiology. 2004;15:755–761. doi: 10.1097/01.ede.0000134875.15919.0f. [DOI] [PubMed] [Google Scholar]
- 5.Goodman PG, Dockery DW, Clancy L. Cause-specific mortality and the extended effects of particulate pollution and temperature exposure. Environmental Health Perspectives. 2004;112:179. doi: 10.1289/ehp.6451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology. 2007;18:369–372. doi: 10.1097/01.ede.0000257515.34445.a0. [DOI] [PubMed] [Google Scholar]
- 7.Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology (Cambridge, Mass) 2009;20:205. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu W, et al. Daily average temperature and mortality among the elderly: a meta-analysis and systematic review of epidemiological evidence. International journal of biometeorology. 2012;56:569–581. doi: 10.1007/s00484-011-0497-3. [DOI] [PubMed] [Google Scholar]
- 9.Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 US cities. Environmental Health Perspectives. 2002;110:859. doi: 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo Y, et al. A large change in temperature between neighbouring days increases the risk of mortality. PloS one. 2011;6:e16511. doi: 10.1371/journal.pone.0016511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin H, et al. Temperature changes between neighboring days and mortality in summer: a distributed lag non-linear time series analysis. PloS one. 2013;8:e66403. doi: 10.1371/journal.pone.0066403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD. Summer temperature variability and long-term survival among elderly people with chronic disease. Proceedings of the National Academy of Sciences. 2012;109:6608–6613. doi: 10.1073/pnas.1113070109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rehill N, Armstrong B, Wilkinson P. Clarifying life lost due to cold and heat: a new approach using annual time series. BMJ open. 2015;5:e005640. doi: 10.1136/bmjopen-2014-005640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braga ALF, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology. 2001;12:662–667. doi: 10.1097/00001648-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 15.McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environmental Health Perspectives. 2001;109:185. doi: 10.1289/ehp.109-1240665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas D, Stram D, Dwyer J. Exposure measurement error: influence on exposure-disease relationships and methods of correction. Annual review of public health. 1993;14:69–93. doi: 10.1146/annurev.pu.14.050193.000441. [DOI] [PubMed] [Google Scholar]
- 18.Kloog I, Nordio F, Coull BA, Schwartz J. Predicting spatiotemporal mean air temperature using MODIS satellite surface temperature measurements across the Northeastern USA. Remote Sensing of Environment. 2014;150:132–139. [Google Scholar]
- 19.Kloog I, Melly SJ, Coull BA, Nordio F, Schwartz JD. Using Satellite-Based Spatiotemporal Resolved Air Temperature Exposure to Study the Association between Ambient Air Temperature and Birth Outcomes in Massachusetts. Environ Health Perspect. 2015 doi: 10.1289/ehp.1308075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nielsen B, et al. Human circulatory and thermoregulatory adaptations with heat acclimation and exercise in a hot, dry environment. The Journal of Physiology. 1993;460:467–485. doi: 10.1113/jphysiol.1993.sp019482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lippmann SJ, Fuhrmann CM, Waller AE, Richardson DB. Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environmental research. 2013;124:35–42. doi: 10.1016/j.envres.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Zorita E, González-Rouco F. Disagreement between predictions of the future behavior of the Arctic Oscillation as simulated in two different climate models: Implications for global warming. Geophysical Research Letters. 2000;27:1755–1758. [Google Scholar]
- 23.Riddle EE, Butler AH, Furtado JC, Cohen JL, Kumar A. CFSv2 ensemble prediction of the wintertime Arctic Oscillation. Climate dynamics. 2013;41:1099–1116. [Google Scholar]
- 24.Petoukhov V, Semenov VA. A link between reduced Barents-Kara sea ice and cold winter extremes over northern continents. Journal of Geophysical Research. 2010;115 doi: 10.1029/2009jd013568. [DOI] [Google Scholar]
- 25.Kloog I, Coull BA, Zanobetti A, Koutrakis P, Schwartz JD. Acute and chronic effects of particles on hospital admissions in New-England. PloS one. 2012;7:e34664. doi: 10.1371/journal.pone.0034664. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.