Abstract
Background
Low patient-reported resilience is associated with ongoing risk of poor health and psychosocial outcomes. Using a large cross-sectional sample of survivors of Hematopoietic Cell Transplantation (HCT), we explored associations between patient-reported resilience, psychological distress, post-traumatic growth, and health-related quality of life
Methods
Between July 1, 2013 and June 30, 2014, the annual Fred Hutchinson Cancer Research Center (FHCRC) post-transplant survivorship survey queried patient-reported health and functional status, and included instruments assessing psychosocial outcomes: the 10-item Connor-Davidson Resilience Scale, the Post-Traumatic Growth Inventory, the Cancer and Treatment Distress measure, and the Medical Outcomes Study Short-Form 12 quality of life scale. Multivariate linear and logistic regression models included demographic and health covariates extracted from the FHCRC research database
Results
1,823 (39%) of 4,643 adult survivors of HCT responded after a single mailing and subsequent reminder letter. Participants’ median age was 59 years (IQR 50–66); 52.3% were male, most were non-Hispanic, white. The median time since HCT was 9 years (IQR 3–18). Lower patient-reported resilience was associated with higher severity chronic graft-versus-host disease, lower performance scores, missing work due to health, and permanent disability (all p<0.0001). After adjustment for demographic and health characteristics, patients reporting low resilience scores had higher odds of psychological distress (OR 3.0, 95% CI 2.1–4.3) and being in the lowest quartile of mental health-related quality of life (OR 5.9, 95% CI 4.4–8.0).
Conclusions
Patient-reported resilience is independently associated with health and psychosocial outcomes. Future studies must determine whether interventions can bolster resilience and improve survivorship outcomes.
Keywords: Resilience, survivorship, psychosocial factors, quality of life, bone marrow transplantation, outcomes studies
BACKGROUND
Resilience is an individual’s ability to maintain physical and emotional well-being in the face of adversity.1,2 Although theories conflict about how (or when) to objectively measure it, they consistently suggest that individual resilience enables patients to harness the resources needed to maintain well-being during and after cancer therapy, to move beyond their experience with hope and insight, and to better adapt to future adversity.3 Furthermore, patient-reports of personal resilience have been associated with outcomes. For example, data from the United States Health and Retirement Study suggest that patient-reported resilience buffers the impact of new chronic health conditions on activities of daily living; patients with low resilience have higher risks of later disability.4 Low patient-reported resilience also has been associated with higher risks of anxiety and depression among hospitalized cancer patients,5 and with psychological distress, poor quality of life, and risky health behaviors among parents of children with cancer.6 Self-perceived resilience may be modified; interventions directed at improving patient-perceptions of resilience also improve well-being, coping and subsequent survivorship.7–9 Therefore, understanding the role of resilience and enhancing it may help optimize the outcomes of cancer patients and their families, both during and after therapy.
Survivors of hematopoietic cell transplantation (HCT) face arduous treatment and experience a high burden of late effects. They are at high risk for medical morbidity and mortality, as well as comparatively poorer functional status and health-related quality of life.10–14 HCT survivors with poor psychosocial outcomes tend to be less adherent to recommended surveillance guidelines, which in turn, may accentuate their risk of serious health consequences.13,15
In order to inform future efforts to identify and intervene with high risk populations, we surveyed a large cross-sectional sample of HCT survivors and assessed relationships between patient-reported resilience and other patient-centered outcomes. Specifically, we aimed to explore correlations between resilience and psychological distress, post-traumatic growth, and health-related quality of life (HRQOL). We hypothesized that patients with low resilience would be particularly vulnerable to poor outcomes. Ultimately, this research may translate into prospective screening and/or intervention studies designed to improve outcomes among cancer survivors.
METHODS
Participants
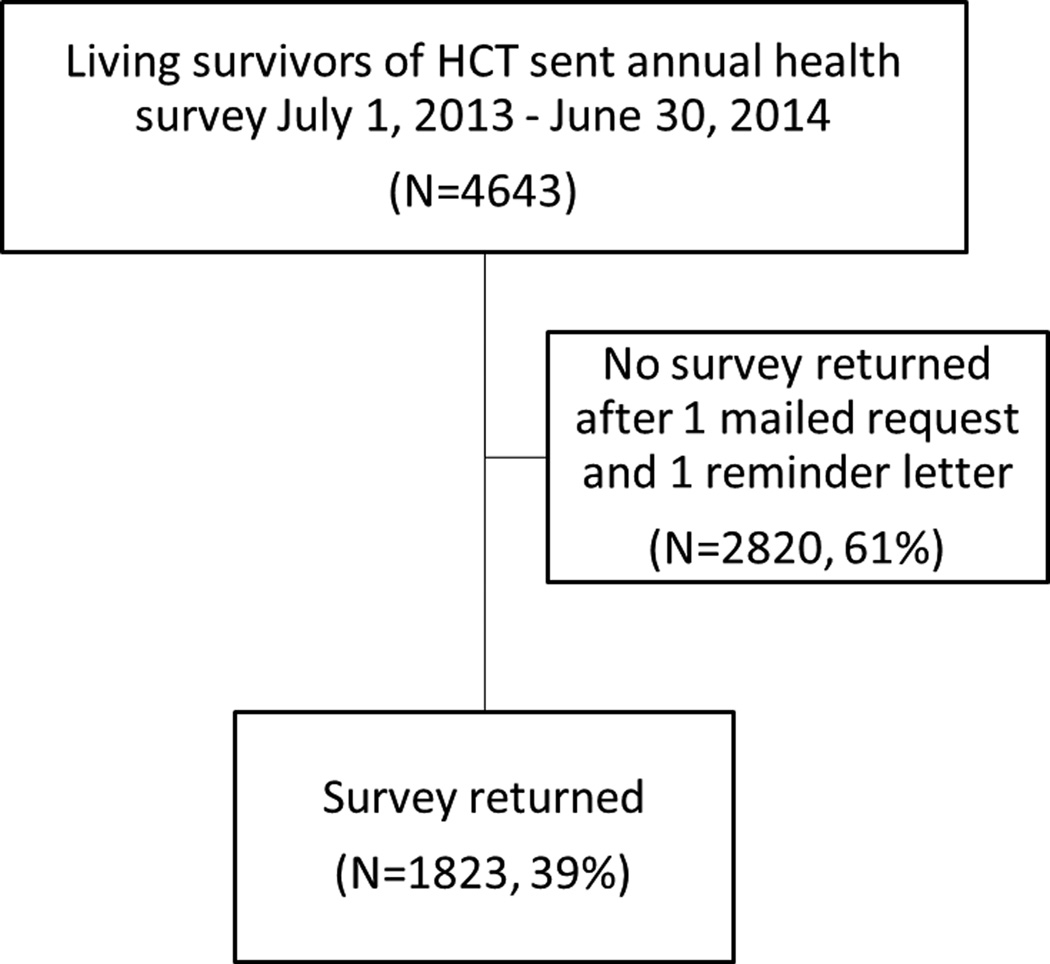
All patients currently ≥18 years-old who received HCT at the Fred Hutchinson Cancer Research Center (FHCRC) are surveyed annually by mail to assess comprehensive health status. This study was approved by the FHCRC Institutional Review Board. Between July 1, 2013 and June 30, 2014 a supplemental questionnaire focusing on patient-reported resilience, post-traumatic growth, and quality of life was included with the annual survey sent to all transplant survivors. The survey was mailed once to each survivor along with a stamped, self-addressed return envelope. Non-responders received one reminder letter approximately 1 month after the initial mailing and surveys were accepted through September 30, 2014. Of 4,643 patients who were mailed the survey, 1,823 (39%) returned it (Figure 1). This is a typical response rate for the annual survey.13
Figure 1.
Consort Diagram. Legend: HCT: Hematopoietic Cell Transplantation
Survey Instrument
The annual survey collected information regarding patient-reported health, occupational, and functional status. Additional detailed information regarding demographics, HCT-related exposures (e.g. initial diagnosis, transplant-type, conditioning regimen), and post-transplantation events (e.g., chronic GVHD, relapse) was extracted from the FHCRC research database.
Independent Variable
Patient-reported resilience was measured by the 10-item Connor-Davidson Resilience scale (CDRISC).16 This instrument has excellent psychometrics and responsiveness,17 and includes items querying personal ability to handle adversity, e.g., “I am able to adapt when changes occur,” “I tend to bounce back after illness, injury, or other hardships,” and, “I believe I can achieve my goals, even if there are obstacles.” Items are scored on a 5-point Likert scale (“not true at all” to “true nearly all of the time”) and total scores range from 0–40, with higher scores indicative of higher self-perceived resilience. The normative adult mean score in the USA is 31.8 (Standard Deviation [SD] 5.4),18 with estimated minimal clinically important difference 2.7.19 In order to identify outcomes associated with low (and potentially improvable) resilience, we empirically dichotomized CDRISC scores at the 25th percentile, as we have done previously.6
Dependent Variables
(1) HRQOL was measured with the Medical Outcomes Study 12-item short-form (SF-12), which includes physical and mental health composite scores, where higher scores indicate better patient-reported HRQOL.20 Analyses included both linear and dichotomized composite scores of the lowest quartile versus all others. (2) Psychological distress was measured with the Cancer and Treatment Distress (CTXD) measure, an instrument designed to detect clinically meaningful levels of anxiety, depression, and cancer-related distress. A score of 1.1 or greater is indicative of distress (area under the receiver-operator curve, 0.85); all analyses used the presence or absence of distress as a dichotomous outcome.21 (3) Post-traumatic growth was measured with the Post-Traumatic Growth Inventory (PTGI), which assesses perceived benefits and positive life-change after experiences such as HCT. Higher scores are suggestive of greater growth.22 Because no thresholds have been published to indicate clinically meaningful growth, analyses used continuous PTGI scores as linear outcome measures. (4) An additional item queried: “I have been able to put my illness and treatment behind me and get on with life,” and was scored on a 5-point Likert Scale (“not at all” to “very much”).23
Statistical Analyses
All variables were described based on their distribution. Group mean resilience scores were compared with student’s t-tests when there were 2 groups, and ANOVA otherwise. Associations between resilience and each dependent variable were assessed first with Pearson correlation coefficients and then with linear or logistic regression models for continuous or dichotomous outcomes, respectively. We considered multiple demographic and medical characteristics as potential interaction terms or confounders: current patient-age, age at and time since transplant (all categorized as in five-year intervals), sex, race/ethnicity, work-status,15 days missed work/school in past 3 months due to health, cancer-type, transplant-type, conditioning regimen (myeloablative, reduced intensity, non-myeloablative), patient-reported presence and severity of current chronic GVHD, history of prior acute or chronic GVHD or recurrent malignancy after HCT, number of current medications, patient-reported performance score (categorized a priori based on degree of assistance needed for activities of daily living), and permanent disability. In addition, we considered high or low post-traumatic growth (defined at the highest or lowest PTGI quartiles, respectively). Using likelihood ratio testing, none of these terms had a statistically significant interaction with the effect of resilience on outcomes (all pinteraction>0.05). Current work-status, GVHD, number of medications, and performance status, however, all changed point estimates of associations by >10%. Hence, all models were built by stepwise addition of these potentially confounding covariates; each covariate was retained in final models if p<0.1. Models also included age, sex, and race as additional demographic covariates. Finally, we found no patterns in missing data amongst responders, nor differences in mean CDRISC scores among participants who did and did not provider demographic or current health information. Given the planned number of comparisons (20 potential covariates and CDRISC as linear and dichotomous outcomes), we used a Bonferroni correction a priori, and defined the acceptable level of significance (alpha) as 0.05/40=0.001. Analyses were conducted with the SAS 9.4 and STATA 12 software systems (SAS Institute Inc., Cary NC; Stata-Corp, College Station, TX).
RESULTS
Participant characteristics and health status
Compared to non-responders, HCT survivors who responded to the survey were older (mean age 57 versus 47 years, p<0.0001), more likely to be female, non-Hispanic white, and have had prior chronic GVHD, and less likely to have received total body irradiation (TBI) as part of their transplant preparative regimen (all p<0.001). Otherwise, demographic, prior medical, and current health characteristics of responders and nonresponders were similar.
The 1,823 responders had a median age of 59 years (IQR 50–66) and were predominantly white, non-Hispanic (Table 1). Their median age at HCT was 48 years (IQR 34–58); 119 (7%) received their HCT prior to the age of 18. Over half were male and 70% identified as working/studying at least part-time. Most patients received their HCT for acute leukemia, 63% received an allogeneic HCT, and 46% received TBI-based preparative regimens.
Table 1.
Demographic and Medical Characteristics of Study Participants (N=1823)
| CDRISC (n=1782) | |||||
|---|---|---|---|---|---|
| Characteristic | N | (%)* | Mean | SD | p-value** |
| Age, years | <0.0001 | ||||
| <40 | 191 | 10 | 30.5 | 6.7 | |
| 40–49 | 232 | 13 | 30.5 | 7.2 | |
| 50–59 | 475 | 26 | 30.9 | 6.4 | |
| 60–69 | 671 | 37 | 31.7 | 6.7 | |
| ≥70 | 254 | 14 | 33.2 | 5.8 | |
| Sex | 0.005 | ||||
| Male | 957 | (52.5) | 31.8 | 6.4 | |
| Female | 866 | (47.5) | 30.9 | 6.8 | |
| Race | 0.002 | ||||
| White | 1646 | (93) | 31.5 | 6.7 | |
| Asian | 68 | (4) | 28.8 | 7.4 | |
| African, Native American, Other | 47 | (3) | 32.6 | 5.3 | |
| Missing | 62 | ||||
| Ethnicity | 0.184 | ||||
| Non-Hispanic | 1737 | (97) | 31.5 | 6.6 | |
| Hispanic | 47 | (3) | 30.0 | 7.4 | |
| Missing | 39 | ||||
| Work-status | <0.0001 | ||||
| Full-time outside the home | 424 | (30) | 32.5 | 6.3 | |
| Part-time outside the home | 127 | (9) | 32.1 | 5.6 | |
| Student (full- or part-time) | 145 | (10) | 30.8 | 6.5 | |
| Work at home | 297 | (21) | 33.2 | 5.4 | |
| Not working or retired because of health | 370 | (26) | 29.1 | 7.3 | |
| Unemployed | 59 | (4) | 28.9 | 6.9 | |
| Missing | 410 | ||||
| Diagnosis | 0.094 | ||||
| Acute Leukemia | 449 | (25) | 30.9 | 6.8 | |
| Chronic Leukemia | 394 | (22) | 31.8 | 6.4 | |
| Lymphoma | 352 | (19) | 31.8 | 6.7 | |
| Multiple Myeloma | 262 | (14) | 31.2 | 6.7 | |
| Non-malignant disease | 173 | (10) | 31.7 | 6.4 | |
| Myelodysplastic Syndrome | 144 | (8) | 31.9 | 6.2 | |
| Solid Tumor | 40 | (2) | 29.3 | 7.0 | |
| Missing | 18 | ||||
| Hematopoietic Cell Transplant Type | 0.542 | ||||
| Autologous | 672 | (37) | 31.3 | 6.7 | |
| Allogeneic, Related | 620 | (34) | 31.3 | 6.8 | |
| Allogeneic, Unrelated | 531 | (29) | 31.7 | 6.4 | |
| Conditioning | 0.041 | ||||
| Total Body Irradiation | 795 | (46) | 31.1 | 6.7 | |
| No Total Body Irradiation | 952 | (54) | 31.7 | 6.5 | |
| Missing | 76 | ||||
Legend:
May not add up to 100% due to rounding error;
p-value based on Student’s t-test when 2 groups;
ANOVA otherwise; Alpha defined as p<0.001 based on Bonferroni correction. CDRISC: 10 item Connor-Davidson Resilience Scale score; SD: Standard Deviation
The median time since transplant was 9 years (IQR 3–18); 53% of allogeneic HCT recipients reported at least mild current chronic GVHD (Table 2). Over half were taking more than 4 prescription medications regularly. Twenty-seven percent reported needing some assistance with activities of daily living and 42% had missed at least one day or work or school due to health in the prior 3 months. Twenty percent met criteria for current psychological distress.
Table 2.
Select Health Outcomes since Hematopoietic Cell Transplant (N=1823)
| CDRISC (n=1782) | |||||
|---|---|---|---|---|---|
| Characteristic | N | (%)* | Mean | SD | p-value** |
| Time Since Transplant, years | 0.970 | ||||
| <10 | 938 | (51) | 31.4 | 6.7 | |
| ≥10 | 885 | (49) | 31.4 | 6.6 | |
| Missing | 8 | ||||
| Post-transplant relapse | 0.666 | ||||
| No | 1626 | (89) | 31.4 | 6.6 | |
| Yes | 197 | (11) | 31.6 | 6.9 | |
| Missing | 8 | ||||
| Current Chronic Graft Versus Host Disease (allogeneic patients only) | <0.0001 | ||||
| No | 542 | (47) | 31.7 | 6.7 | |
| Yes, mild | 227 | (20) | 31.7 | 6.0 | |
| Yes, moderate | 75 | (7) | 29.0 | 6.7 | |
| Yes, severe | 20 | (2) | 26.2 | 7.0 | |
| Missing | 287 | ||||
| Current number of medications taken | <0.0001 | ||||
| None | 57 | (4) | 32.8 | 5.9 | |
| ≤4 | 655 | (45) | 32.6 | 5.9 | |
| >4 | 750 | (51) | 30.2 | 7.0 | |
| Missing | 370 | ||||
| KarnofskyPerformance Score | <0.0001 | ||||
| ≥90%: normal activity, minor health complaints | 591 | (40) | 34.0 | 5.5 | |
| 80–89%: normal activity with effort, not fully healthy | 485 | (33) | 31.0 | 6.3 | |
| 50–79%: unable to work, able to meetsmost personal needs with variable assistance | 364 | (25) | 28.1 | 6.7 | |
| <50%: unable to care for self, needs assistance or hospital–level care | 34 | (2) | 24.7 | 7.4 | |
| Missing | 358 | ||||
| Number of days in past 3 months unable to work or go to school because of health | |||||
| None | 691 | (58) | 33.5 | 5.5 | <0.0001 |
| 1–5 | 272 | (23) | 29.6 | 6.6 | |
| 6 or more | 224 | (19) | 29.0 | 7.0 | |
| Missing | 645 | ||||
| Permanently disabled because of health | <0.0001 | ||||
| No | 1368 | (93) | 31.8 | 6.7 | |
| Yes | 109 | (7) | 26.2 | 7.5 | |
| Missing | 355 | ||||
Legend:
May not add up to 100% due to rounding error;
p-value based on Student’s t-test when 2 groups,
ANOVA otherwise; alpha defined as p<0.001 based on bonferroni correction, CDRISC: 10 item Connor-Davidson Resilience Scale score; SD: Standard Deviation.
The mean patient-reported resilience score for the whole sample was 31.4 (SD 6.6). Age and work-status were associated with resilience scores (Table 1). For example, the mean resilience score among patients ages 70 years and older was 33.3 (SD 5.8) compared to 30.5 (SD 6.7) among those under 40 years (p<0.0001). Participants who were currently working full-time outside of the home reported mean resilience scores of 32.5 (SD 6.3) compared to 28.9 (SD 6.9) among those unemployed (p<0.001).
Post-transplant health status was also associated with patient-reported resilience. Mean scores were lower among patients who had more severe GVHD, who took ≥4 prescription medications, and who were unable to work due to their health (all p<0.0001, Table 2). Likewise, patients with lower Karnofsky Performance Scores (KPS) also reported lower mean resilience scores (p<0.0001). No other demographic or health characteristics were associated with resilience scores, including sex, race/ethnicity, cancer-type, HCT-type, conditioning regimen, age at or time since transplant, prior history of chronic GVHD, or history of recurrent disease.
Linear resilience scores correlated more strongly with psychological distress (r=−0.51, p<0.0001) and mental composite HRQOL scores (r=0.62, p<0.0001) than with physical composite HRQOL scores (r=31, p<0.0001) or post-traumatic growth. In multivariable linear regression models, each additional resilience point was associated with 0.8 higher mental composite score (p<0.001), 0.1 higher physical composite score (p=0.042), and 0.7 higher PTGI score (p<0.0001).
Low resilience was independently associated with multiple poor PROs (Table 3). After adjusting for work-status, medications, performance score, and covariates that were statistically associated with resilience, patients reporting the lowest quartile of resilience scores had higher odds of psychological distress (Odds Ratio [OR] 3.0, 95% CI 2.1, 4.3). Likewise, the adjusted OR’s of low mental HRQOL and perceived recovery from HCT were 5.9 (95% CI 4.4, 8.0) and 2.0 (95% CI 1.3, 3.3), respectively. Low resilience was not associated with low composite scores of physical HRQOL (OR 1.4, 95% CI 0.9, 2.2) or perceptions that “life has returned to normal” (OR 1.5, 95% CI 0.9, 2.5).
Table 3.
Odds Ratios of selected outcomes given lowest quartile resilience score and other measures of current health status*
| Outcome | OR | 95% CI |
|---|---|---|
| Current Psychological Distress† | ||
| Low resilience | 3.0 | 2.1, 4.3 |
| Not working | 2.9 | 2.0, 4.1 |
| Taking >4 medications | 2.0 | 1.4, 2.9 |
| Performance status <80% | 4.1 | 2.9,5.9 |
| Lowest quartile quality of mental health‡ | ||
| Low resilience | 5.9 | 4.4, 8.0 |
| Currently not working | 2.9 | 2.0, 4.1 |
| Performance status <80% | 1.6 | 1.2, 2.3 |
| Lowest quartile quality of physical health‡ | ||
| Low resilience | 1.4 | 0.9, 2.2 |
| Not working | 2.5 | 1.6, 3.9 |
| Moderate-severe chronic graft vs. host disease | 2.1 | 1.1, 4.1 |
| Taking >4 medications | 3.3 | 2.0, 5.4 |
| Performance status <80% | 4.7 | 3.0, 7.4 |
| “I have been able to put my illness/treatment behind me and get on with life”(“not at all/a little bit/somewhat”) | ||
| Low resilience | 2.4 | 1.5, 3.9 |
| Not working | 3.3 | 2.1, 5.2 |
| Moderate-severe chronic graft vs. host disease | 2.5 | 1.4, 4.6 |
| Taking >4 medications | 3.7 | 2.2, 6.3 |
| Performance status <80% | 5.2 | 3.3, 8.2 |
All adjusted for age, sex, race, resilience score, plus covariates listed below given outcome measure. Low resilience defined as lowest quartile on 10-item Connor-Davidson Resilience Scale. “Currently not working” defined as retired due to health or unemployed.
Based on Cancer Treatment and Distress (CTXD) scale;
Based on Medical Outcomes Survey Short Form 12
Legend: OR: Odds Ratio, CI: Confidence Interval
DISCUSSION
Patient-reported resilience is a strong candidate for screening, risk-stratification, and targeted intervention. To our knowledge, this is the first large analysis to describe associations between self-perceived resilience and outcomes among patients with cancer. In this cohort of HCT survivors, we found strong relationships between resilience, current health status, and psychosocial outcomes.
Our cross-sectional analysis suggests a number of hypotheses for future testing. We found that low patient-reported resilience was independently associated with poor outcomes. Future studies could prospectively assess perceived resilience before and after treatments, and follow patients to determine how it interacts with the illness experience and predicts later outcomes. Likewise, interventions designed to bolster resilience may improve quality of life. An important strength of our cohort is that it enables testing some of these hypotheses; we plan to determine whether current patient-reported resilience is associated with later health or psychosocial outcomes.
Our analysis does not allow any causal inferences, however. It is possible that self-perceptions of resilience develop only after significant life events. For example, patients who previously experienced severe chronic GVHD may consequently report poorer current HRQOL and/or lower personal resilience. Our multivariable models suggest that self-perceptions of resilience are independently associated with poor outcomes, even after adjustment for measurable health and functional status. This observation is important because personal perceptions may be more immediately modifiable than coexisting disabilities or chronic medical conditions.7,8,24–26 Likewise, low self-perceived resilience may indicate additional vulnerability to future stressors.4,27 Whether the poor outcomes cause low resilience, or whether low resilience causes poor outcomes, patients with both are vulnerable on two fronts: (1) poor health; and, (2) decreased capacity to deal with poor health and future threats.
Our sample was derived from a single center, had little racial/ethnic diversity, and a relatively low response rate. Others have described more diversity and response rates of 69% with one-time surveys of HCT survivors at multiple sites.28 Our survey is mailed annually with a limited response-window and no active follow-up; survivors may therefore feel less inclined to respond. We do not know if responders felt more or less resilient than non-responders. Likewise, responders were more likely to have received TBI-based preparation for HCT and to have chronic GVHD, both of which are associated with medical late effects. For all these reasons, our results might not fully represent the general population of HCT survivors.
Operationalizing resilience in people with cancer is challenging because how (or when) to measure it remains unclear.6,29–32 Some theoretical models suggest it is equated with an overall positive adjustment after trauma,1,33,34 and studies suggest HCT survivors have high capacity for post-traumatic growth.35 We found negligible correlation between self-perceived resilience and post-traumatic growth. Indeed, we have previously found PTGI scores to be inconsistent with subjective perceptions of resilience,31 and both adolescent and young adult patients with cancer and their parents have reported that their maintenance of normalcy is proof of their resilience.30,32
Likewise, recent theories suggest that trajectories of resilience differ for individuals facing chronic stressors (e.g., poverty), compared to those facing acute stressors (e.g., death of a loved one).34 Where cancer survivors fit into these theories is unclear. Although cancer diagnosis and treatment, including HCT, often represent a discreet time-interval, survivors face long-lasting challenges related to their physical and psychosocial health.10–14,36 How do we define appropriate or “stable” trajectories of function during survivorship?
To overcome these challenges, we and others have relied on patients’ own reports of resilience.4–6,16,31,32,37,38 Indeed, patient-reported outcomes have been encouraged in psychosocial oncology research because they allow better understanding of patients’ values, thereby informing clinical decision-making and providing patient-centered care.39,40 While few studies explicitly describe patient-reported resilience amongst patients with cancer,5,29,32,41 our data are consistent with others’ which suggest that personal perceptions of resilience play important roles in health and psychosocial outcomes. Patient-reported resilience has been shown to buffer the impact of aging and protect against later disability.4 Low self-perceived resilience predicts poorer pharmaco-adherence among patients with diabetes,27 and higher resilience predicts positive treatment responses among patients with post-traumatic stress disorder.38
Our overall objectives are to determine how to screen for and promote resilience amongst survivors of cancer and their families. Future analyses of the present cohort will determine if current patient-reported resilience truly predicts later health and psychosocial outcomes. Meanwhile, several studies suggest individual perceptions may be modified by skills-based interventions that teach stress-management, goal-setting or positive re-appraisal techniques.2,7,8,26,42–44 Likewise, interventions directed at promoting positive psychology, including post-traumatic growth, have high potential.9,44 Future research must prospectively test such interventions, while also deconstructing the interrelated constructs of self-perceived resilience, psychological growth, quality of life, and other outcomes. While serious illnesses and its treatment requirements cannot be avoided, attention to promoting patient-reported resilience could have meaningful benefits by improving health outcomes, minimizing the adverse long-term psychological effects, and, in turn, enhancing quality of life.
Acknowledgments
Funding: NIH grant numbers CA18029, HL36444, CA 78902, CA160684, KL2TR000421, and L40CA170049.
Footnotes
Disclosures: None of the authors has a financial or other conflict of interest to declare.
REFERENCES
- 1.Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annual review of clinical psychology. 2011;7:511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- 2.Southwick SM, Charney DS. The science of resilience: implications for the prevention and treatment of depression. Science. 2012;338(6103):79–82. doi: 10.1126/science.1222942. [DOI] [PubMed] [Google Scholar]
- 3.Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. European journal of psychotraumatology. 2014;5 doi: 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manning LK, Carr DC, Kail BL. Do Higher Levels of Resilience Buffer the Deleterious Impact of Chronic Illness on Disability in Later Life? The Gerontologist. 2014 doi: 10.1093/geront/gnu068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Min JA, Yoon S, Lee CU, et al. Psychological resilience contributes to low emotional distress in cancer patients. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2013;21(9):2469–2476. doi: 10.1007/s00520-013-1807-6. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg AR, Wolfe J, Bradford MC, et al. Resilience and psychosocial outcomes in parents of children with cancer. Pediatric blood & cancer. 2014;61(3):552–557. doi: 10.1002/pbc.24854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loprinzi CE, Prasad K, Schroeder DR, Sood A. Stress Management and Resilience Training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clinical breast cancer. 2011;11(6):364–368. doi: 10.1016/j.clbc.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Robb SL, Burns DS, Stegenga KA, et al. Randomized clinical trial of therapeutic music video intervention for resilience outcomes in adolescents/young adults undergoing hematopoietic stem cell transplant: a report from the Children's Oncology Group. Cancer. 2014;120(6):909–917. doi: 10.1002/cncr.28355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC public health. 2013;13:119. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin PJ, Counts GW, Jr, Appelbaum FR, et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. Journal of clinical oncology. 2010;28(6):1011–1016. doi: 10.1200/JCO.2009.25.6693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chow EJ, Mueller BA, Baker KS, et al. Cardiovascular hospitalizations and mortality among recipients of hematopoietic stem cell transplantation. Annals of internal medicine. 2011;155(1):21–32. doi: 10.7326/0003-4819-155-1-201107050-00004. [DOI] [PubMed] [Google Scholar]
- 12.Baker KS, Ness KK, Steinberger J, et al. Diabetes, hypertension, and cardiovascular events in survivors of hematopoietic cell transplantation: a report from the bone marrow transplantation survivor study. Blood. 2007;109(4):1765–1772. doi: 10.1182/blood-2006-05-022335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khera N, Storer B, Flowers ME, et al. Nonmalignant late effects and compromised functional status in survivors of hematopoietic cell transplantation. Journal of clinical oncology. 2012;30(1):71–77. doi: 10.1200/JCO.2011.38.4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bishop MM, Beaumont JL, Hahn EA, et al. Late effects of cancer and hematopoietic stem-cell transplantation on spouses or partners compared with survivors and survivor-matched controls. Journal of clinical oncology. 2007;25(11):1403–1411. doi: 10.1200/JCO.2006.07.5705. [DOI] [PubMed] [Google Scholar]
- 15.Khera N, Chow EJ, Leisenring WM, et al. Factors associated with adherence to preventive care practices among hematopoietic cell transplantation survivors. Biology of blood and marrow transplantation. 2011;17(7):995–1003. doi: 10.1016/j.bbmt.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of traumatic stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 17.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health and quality of life outcomes. 2011;9:8. doi: 10.1186/1477-7525-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell-Sills L, Forde DR, Stein MB. Demographic and childhood environmental predictors of resilience in a community sample. Journal of psychiatric research. 2009;43(12):1007–1012. doi: 10.1016/j.jpsychires.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 19.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Medical care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 20.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Syrjala KLYJ, Langer SL. Psychometric Properties of the Cancer and Treatment Distress (CTXD) Measure in Hematopoietic Cell Transplant Patients. Psycho-oncology. 2015 doi: 10.1002/pon.3861. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. Journal of traumatic stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 23.Lee SJ, Fairclough D, Parsons SK, et al. Recovery after stem-cell transplantation for hematologic diseases. Journal of clinical oncology. 2001;19(1):242–252. doi: 10.1200/JCO.2001.19.1.242. [DOI] [PubMed] [Google Scholar]
- 24.Sahler OJ, Dolgin MJ, Phipps S, et al. Specificity of problem-solving skills training in mothers of children newly diagnosed with cancer: results of a multisite randomized clinical trial. Journal of clinical oncology. 2013;31(10):1329–1335. doi: 10.1200/JCO.2011.39.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher PL, McNicol K, Young B, Smith E, Salmon P. Alleviating Emotional Distressin Adolescent and Young Adult Cancer Survivors: an open trial of metacognitive therapy. Journal of adolescent and young adult oncology. 2015;4(2):64–69. doi: 10.1089/jayao.2014.0046. [DOI] [PubMed] [Google Scholar]
- 26.Folkman S, Greer S. Promoting psychological well-being in the face of serious illness: when theory, research and practice inform each other. Psycho-oncology. 2000;9(1):11–19. doi: 10.1002/(sici)1099-1611(200001/02)9:1<11::aid-pon424>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 27.Yi JP, Vitaliano PP, Smith RE, Yi JC, Weinger K. The role of resilience on psychological adjustment and physical health in patients with diabetes. British journal of health psychology. 2008;13(Pt 2):311–325. doi: 10.1348/135910707X186994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun CL, Francisco L, Baker KS, Weisdorf DJ, Forman SJ, Bhatia S. Adverse psychological outcomes in long-term survivors of hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study (BMTSS) Blood. 2011;118(17):4723–4731. doi: 10.1182/blood-2011-04-348730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Molina Y, Yi JC, Martinez-Gutierrez J, Reding KW, Yi-Frazier JP, Rosenberg AR. Resilience among patients across the cancer continuum: diverse perspectives. Clinical journal of oncology nursing. 2014;18(1):93–101. doi: 10.1188/14.CJON.93-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosenberg AR, Baker KS, Syrjala KL, Back AL, Wolfe J. Promoting resilience among parents and caregivers of children with cancer. Journal of palliative medicine. 2013;16(6):645–652. doi: 10.1089/jpm.2012.0494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosenberg AR, Starks H, Jones B. "I know it when I see it." The complexities of measuring resilience among parents of children with cancer. Supportive care in cancer. 2014;22(10):2661–2668. doi: 10.1007/s00520-014-2249-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosenberg AR, Yi-Frazier JP, Wharton C, Gordon K, Jones B. Contributors and Inhibitors of Resilience Among Adolescents and Young Adults with Cancer. Journal of adolescent and young adult oncology. 2014;3(4):185–193. doi: 10.1089/jayao.2014.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mancini AD, Bonanno GA. Predictors and parameters of resilience to loss: toward an individual differences model. Journal of personality. 2009;77(6):1805–1832. doi: 10.1111/j.1467-6494.2009.00601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bonanno GA, Diminich ED. Annual Research Review: Positive adjustment to adversity--trajectories of minimal-impact resilience and emergent resilience. Journal of child psychology and psychiatry, and allied disciplines. 2013;54(4):378–401. doi: 10.1111/jcpp.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zebrack BJ, Stuber ML, Meeske KA, et al. Perceived positive impact of cancer among long-term survivors of childhood cancer: a report from the childhood cancer survivor study. Psycho-oncology. 2012;21(6):630–639. doi: 10.1002/pon.1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhatia S, Francisco L, Carter A, et al. Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood. 2007;110(10):3784–3792. doi: 10.1182/blood-2007-03-082933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yi-Frazier JP, Yaptangco M, Semana S, et al. The association of personal resilience with stress, coping, and diabetes outcomes in adolescents with type 1 diabetes: Variable- and person-focused approaches. Journal of health psychology. 2013 doi: 10.1177/1359105313509846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davidson J, Stein DJ, Rothbaum BO, Pedersen R, Szumski A, Baldwin DS. Resilience as a predictor of treatment response in patients with posttraumatic stress disorder treated with venlafaxine extended release or placebo. Journal of psychopharmacology. 2012;26(6):778–783. doi: 10.1177/0269881111413821. [DOI] [PubMed] [Google Scholar]
- 39.Basch E, Abernethy AP, Mullins CD, et al. Recommendations for incorporating patient-reported outcomes into clinical comparative effectiveness research in adult oncology. Journal of clinical oncology. 2012;30(34):4249–4255. doi: 10.1200/JCO.2012.42.5967. [DOI] [PubMed] [Google Scholar]
- 40.Garcia SF, Cella D, Clauser SB, et al. Standardizing patient-reported outcomes assessment in cancer clinical trials: a patient-reported outcomes measurement information system initiative. Journal of clinical oncology. 2007;25(32):5106–5112. doi: 10.1200/JCO.2007.12.2341. [DOI] [PubMed] [Google Scholar]
- 41.Keshet Y, Schiff E, Samuels N, Ben-Arye E. Giving voice to cancer patients: assessing non-specific effects of an integrative oncology therapeutic program via short patient narratives. Psycho-oncology. 2015;24(2):169–174. doi: 10.1002/pon.3621. [DOI] [PubMed] [Google Scholar]
- 42.Antoni MH, Lechner SC, Kazi A, et al. How stress management improves quality of life after treatment for breast cancer. Journal of consulting and clinical psychology. 2006;74(6):1143–1152. doi: 10.1037/0022-006X.74.6.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kent M, Rivers CT, Wrenn G. Goal-Directed Resilience in Training (GRIT): A Biopsychosocial Model of Self-Regulation, Executive Functions, and Personal Growth (Eudaimonia) in Evocative Contexts of PTSD, Obesity, and Chronic Pain. Behavioral sciences. 2015;5(2):264–304. doi: 10.3390/bs5020264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rosenberg AR, Yi-Frazier JP, Eaton L, et al. Promoting Resilience in Stress Management: A Pilot Study of a Novel Resilience-Promoting Intervention for Adolescents and Young Adults With Serious Illness. Journal of pediatric psychology. 2015 doi: 10.1093/jpepsy/jsv004. [DOI] [PMC free article] [PubMed] [Google Scholar]