Abstract
To assess performances of N95 respirators for Health Care Workers (HCWs) in a simulated health-care setting, we measured the Simulated Workplace Protection Factors (SWPFs) in real-time from the volunteers. A total of 49 study subjects, wearing 3 M respirator Model N95 1860 and 1860S, were fit tested using the OSHA Exercise Regimen. The test subjects were asked to perform simulated scenarios, including patient assessments, suction, and intravenous injection (IV) treatment. Two TSI PortaCount instruments continuously measured concentrations in the respirator and the room concentration. For Quantitative Fit Testing (QNFT), 36 out of 49 (73.5%) passed the fit factor (FF) criteria set at 100 and 13 (26.5%) failed. The results of QNFT were found to have a low correlation with SWPF, with R2=0.32. The geometric means (GM) and geometric standard deviations (GSD) of SWPF were 68.8 (1.1) for those subjects who passed and 39.6 (1.3) for those who failed. Real-time assessments of SWPF showed that lower SWPFs were; moving head up and down, and bending at the waist. This study identifies the needs for providing different sizes of respirators for HCWs and the importance of performing fit tests for HCWs regularly. And particular movements were identified as attributing factors affecting more on SWPFs.
Keywords: N95 respirators, Simulated Workplace Protection Factors (SWPFs), Real-time, Fit test
Introduction
Various types of workers comprise the health-care industry, including physicians, dentists, and nurses as well as a broad range of other workers such as medical and nursing school students, and volunteers who are constantly in contact with patients in settings other than hospitals1). These workers could be directly exposed to health-care-related infections as their jobs involve providing health care and treatment to individuals with infectious diseases. Thus, the risk of infection through contact with patients is high among workers in the health-care industry, and their morbid risk of work-related diseases is higher than that of workers in other services2). Health Care Workers (HCWs) can be exposed to infectious diseases through various modes. Among the modes of transmission is through air-borne infection, in which infected particles larger than 5 µm in diameter are projected into the air during coughing, sneezing, or conversation and splattered to the conjunctiva, or nasal or oral mucosa of humans, thereby spreading the infection3). For example, in case of tuberculosis world-wide, 8.5 million persons were newly contracted in 2011, of whom 1.45 million died. While tuberculosis is becoming a worldwide health issue, Korea was reported to have the highest incidence of tuberculosis and tuberculosis-related mortality rate among the OECD member countries4). For this reason, HCW are advised to wear N95 respirators that passed the fit test or high-quality respirators when they enter rooms where patients with suspected or confirmed respiratory organ tuberculosis (pulmonary or laryngeal tuberculosis) are confined3). In addition, the Korean Ministry of Health and Welfare established the Guideline for Nosocomial Infection Prevention Control, in which wearing of special masks such as the N95 respirator are recommended in order to prevent infection through inhalation of small (less than 5 µm) infectious particles floating in the air current along with dusts5). However, considering that reducing the inflow of pathogens to the body greatly depends on the degree of fit of masks to the face, regardless of the quality of respirators and the efficiency of filters, wearers are not fully protected unless the respirator appropriately fits them6). In a study that evaluated the effects of the N95 respirator and surgical masks within a simulated test space, the effects of an inappropriately worn respirator were worse than those of a loose-fitting respirator7). Furthermore, other studies indicated that the fit factor extremely decreased, unless the N95 respirator was worn appropriately8,9,10).
Therefore, a quantitative fit test is highly important. However, environmental conditions differ between workplaces. In addition, intrinsic respiratory rate and respiratory rate during work could differ, making it impossible to guarantee long-term protection11). Fit test results only indicate the degree of fit between the face of the wearer and the respirator under the condition at the time of measurement and do not predict the degree of protection provided to the wearer from harmful substances in real workplaces12, 13). Thereby, NIOSH suggested that a workplace test or a simulated workplace test should be included in the respiratory protection program14).
When wearing a respirator in real workplaces, the amount of aerosol particles that enter the respiratory area depends on various factors such as the concentration and size distribution of the aerosol particles in the surrounding environment of the wearer, the types of filters used, the amount of sweat and dusts on the face of the wearer, the movement of the facial muscles, and the wearer’s will to wear the respirator appropriately15). Therefore, it is important that respirator fit is evaluated while workers are performing actual work activities wearing a respirator. However, measuring respirator performance in actual workplaces is difficult16, 17). Hence, the Simulated Workplace Protection Factor (SWPF) can be evaluated by using a laboratory-based method in combination with real workplace environments18).
Therefore, this study aimed to identify the protective effect of the N95 respirator for HCWs in a simulated work place. In addition, several facial dimensions of test subjects were measured so as to identify correlations with the fit factor and SWPF through the fit test, and real-time SWPFs were measured while performing simulated tasks of nursing so as to identify contributing activities on SWPFs.
Methods
General Methods
A fit test using TSI PortaCount Pro+ 8038 equipment was performed while the test subjects wore the N95 respirator. The criteria of the Occupational Safety and Health Administration (OSHA) Protocol27) were used in the Quantitative Fit Testing (QNFT). QNFT scores higher than 100 were applied as the passing criteria. Every test subject stopped the intake of drinks or foods 30 min before the start of the experiment and avoided smoking28). The test subjects who completed the fit test were asked to undertake three scenarios. The real-time performances of the respirator were assessed by measuring the ambient air-borne particle concentrations in the room and outside and inside the respirator by using two kinds of fit test equipment. A simulated medical environment was utilized as shown in Fig. 2, and three health-care task scenarios were constructed by professional nurses and used in the setting. SWPF was calculated by using real-time measurement data of air-borne particle concentrations outside and inside the respirator while the subjects were performing care for patients.
Fig. 2.

View of health care setting environment.
1) Test subjects
For this study, test subjects were voluntarily recruited by posting advertisements or sending advertisement through e-mail, targeting health professionals, particularly nurses and nursing school students. In consideration of the appropriate sample size for the respirator fit test that was calculated19), 49 test subjects were evaluated.
Facial dimensions, namely face width and face length, were measured to examine if the recruited subjects were included in the NIOSH Respirator Fit Test Panel (the NIOSH panel). Referring to previous study results20,21,22), nasal root breadth, nose width, lip length, bitragion-subnasale arc, face length, and menton-subnasale length were also measured as illustrated in Fig. 123). A sliding caliper and a spreading caliper were used as measuring tools24, 25). For facial measurements, the reference points of the measurements were determined by using the guidelines from SizeKorea26). In order to reduce errors in the measurement values, mean values from 3 replications were calculated. In addition, only the individuals included in the NIOSH panel were selected as test subjects.
Fig. 1.
Facial dimensions measured.
2) Equipment
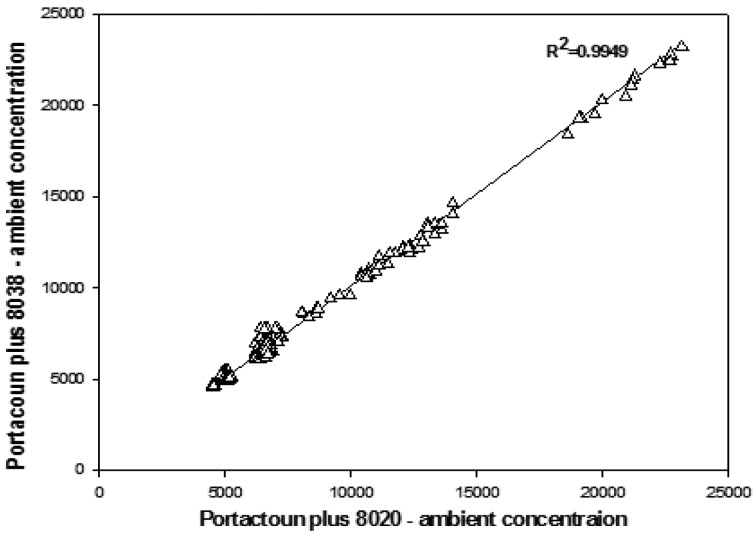
TSI PortaCount Pro+ 8038 and N95-Companion TSI PortaCount Plus Model 8020 equipment, which quantitatively measure the ambient air-borne dust concentration and the fit level of a respirator, respectively, were used. The linear correlation coefficient of the ambient air-borne dust concentrations between the two kinds of equipment was R2=0.9949 (Fig. 3). Thus two instruments were considered in good agreements to use side-by-side.
Fig. 3.
Relationship between the two instrument for ambient particle concentration (p/cm3).
In addition, in order not to change the condition of face seal by the weight of the Tygon tube that was connected to TSI PortaCount Pro + 8038, which was used to measure the dust concentration inside the respirator, the tube was supported with a necklace attached with a binder clip18).
3) Respirator
3 M 1860 or 1860s models of the N95 respirators, which have been used and sold in medical work places, were used. The two models were certified by NIOSH.
4) SWPF
After discussion with an expert (a nursing professor), three health-care scenarios including patient assessment, suction treatment, and IV treatment were selected among various tasks nurses normally perform (Table 1). To simulate real hospital bed conditions, the following were prepared in the simulated environment: sphygmomanometer, hand sanitizer, wall aspirator, tracheotomy tube, disposable gloves, tourniquet, 2-cc syringe, alcohol cotton balls, and dummy (simulated patients).
Table 1. Health care scenarios developed for the study.
| Scenarios 1 (Assessment) | Scenarios 2 (Suction) | Scenarios 3 (IV Treatment) |
|---|---|---|
| 41 s to 1 min 48 s | 58 s to 1 min 44 s | 48 sec to 1 min 42 s |
| 1. Patient bedside diagnostics | 1. Upper airway suction | 1. Administer IV care |
| · Vitals : blood pressure | · Suction : by aspirator | · IV : Injection of vein |
| 2. Ask question | 2. Notify aspirator | 2. Notify IV care |
| 3. Check blood pressure | 3. Knock chest and put on gloves | 3. Clean alcohol |
| 4. Raise/lower stretcher as need | 4. Raise/lower stretcher as need | 4. Tie tourniquet, push IV medication |
| 5. Clean hands | 5. Perform aspirator | 5. Raise/lower stretcher as need |
SWPF was calculated by measuring the concentrations inside and outside the respirator and using the equation (1)26).
 |
...(1)
SWPF = Simulated Workplace Protection Factor
CA = concentration of particles outside the respirator
CB = concentration of particles inside the respirator
Overall SWPF was calculated for each SWPF activity by using equation (2) as follows:
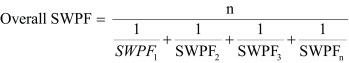 |
...(2)
SWPF = Each SWPF calculated by the concentrations outside and inside the respirator
n = total number of SWPF activities evaluated
Statistical analysis
The general characteristics of the subjects were subjected to a frequency analysis and expressed as percentages. The mean and standard deviation of each facial dimension (mm) was calculated, followed by a comparison of the mean difference between the men and women by using the t-test. The fit factors (FF) were expressed as geometric means (GM) and geometric standard deviations (GSD). A regression analysis between FF and SWPF was performed. The level of significance for all the statistical values was set at α=0.05. Collected data were analyzed by using the SPSS statistics 18.0 program.
Ethics
The study procedure was approved by the Catholic Medical Center Office of Human Research Protection Program.
Results
General characteristics of the test subjects
The test subjects were 49 individuals; 33 (67.3%) were female and 16 (32.7%) were male. Their mean age was 23.0 ± 3.8 yr. The age distribution was as follows: 36 persons (75.0%) younger than 25 yr; 9 persons (18.4%) between 25 and 30 yr; 3 persons (6.1%) between 30 and 35 yr; and 1 person (2.0%) older than 35 yr. The distribution of the subjects’ occupations was as follows: 37 subjects (75.5%) nursing students and 12 subjects (24.5%) nurses. The size distribution of the N95 respirator was as follows: 46 subjects (93.9%) wore the small (S), and 3 subjects (6.1%) wore the medium (M) size respirator (Table 2).
Table 2. General characteristics of the study subjects.
| Classification | N (%) | |
|---|---|---|
| Sex | Male | 16 (32.7%) |
| Female | 33 (67.3%) | |
| Age | 20–24 | 36 (73.5%) |
| 25–29 | 9 (18.4%) | |
| 30–34 | 3 (6.1%) | |
| ≥35 | 1 (2.0%) | |
| Job | Nursing student | 37 (75.5%) |
| Nurse | 12 (24.5%) | |
| N95 Size | Medium | 3 (6.1%) |
| Small | 46 (93.9%) |
N: Number of subjects
Facial dimensions
The statistical data of the facial dimensions of 49 subjects are presented in Table 3. The results of the t-test to identify sex-related differences in values indicate a statistically significant difference (p<0.05) in lip length (Table 3).
Table 3. Summary statistics of facial dimension measurements.
| Item | Male (N=16) | Female (N=33) | p-value | ||||
|---|---|---|---|---|---|---|---|
| M±SD | 95th percentile | M±SD | 95th percentile | ||||
| LCL | UCL | LCL | UCL | ||||
| Face length | 117.2 ± 5.0 | 114.4 | 120.0 | 110.8 ± 4.2 | 109.3 | 112.3 | 0.356 |
| Lip length | 40.1 ± 3.4 | 38.2 | 41.9 | 37.9 ± 2.4 | 37.1 | 38.8 | 0.026* |
| Nose width | 35.4 ± 2.0 | 34.3 | 36.5 | 31.7 ± 2.5 | 30.8 | 32.5 | 0.435 |
| Nasale root breadth | 33.6 ± 3.2 | 31.8 | 35.3 | 31.6 ± 3.4 | 30.4 | 32.9 | 0.777 |
| Bitragion-subnasale arc | 179.4 ± 22.1 | 167.2 | 191.6 | 176.4 ± 19.3 | 169.5 | 183.2 | 0.229 |
| Bizygomatic breadth | 138.6 ± 8.1 | 134.2 | 143.1 | 131.6 ± 6.0 | 129.5 | 133.8 | 0.161 |
| Menton-subnasale length | 70.6 ± 3.7 | 68.5 | 72.6 | 65.7 ± 4.4 | 64.1 | 67.3 | 0.193 |
M ± SD: Mean and standard deviation (mm). LCL: Lower control limit, UCL: Upper control limit. *Statistically significant difference between gender by t-test.
Test Panel
The study subjects were 49 individuals who were included in the NIOSH panel. Of the subjects, 33 (67.3%) were female and 16 (32.7%) were male. Their facial lengths ranged from 102 to 126.7 mm, and their facial widths ranged from 120.5 to 153.3 mm (Fig. 4).
Fig. 4.
Distribution of test subjects in the NIOSH panel constructed.
Correlation between the fit test results and SWPF
Since the results of the fit test did not follow a normal distribution, both the FF and SWPF values were log transformed and the presented with GM (GSD). According to the results of the fit test using the 49 test subjects who were included in the NIOSH panel, 36 test subjects (73.5%) passed and the GM (GSD) of FF was 156.3 (1.3). However, 13 test subjects (26.5%) failed and the GM (GSD) of FF was 37.0 (1.7) (Table 4). The GM (GSD) of SWPF values of the test subjects who passed and those who failed the fit test were 68.8 (1.1) and 39.6 (1.3), respectively, indicating that the latter had generally lower values than the former (Table 5).
Table 4. Fit test result.
| Fit test | N (%) | GM (GSD) | ||
|---|---|---|---|---|
| Pass | Fail | Pass (FF≥100) | Fail (FF<100) | |
| 36 (73.5) | 13 (26.5) | 156.3 (1.3) | 37.0 (1.7) | |
GM: Geometric means, GSD: Geometric standard deviations
Table 5. SWPFs by subject who passed or failed the fit test.
| SWPF | N (%) | GM (GSD) | ||
|---|---|---|---|---|
| Pass | Fail | Pass (FF≥100) | Fail (FF<100) | |
| 36 (73.5) | 13 (26.5) | 68.8 (1.1) | 39.6 (1.3) | |
GM: Geometric means, GSD: Geometric standard deviations
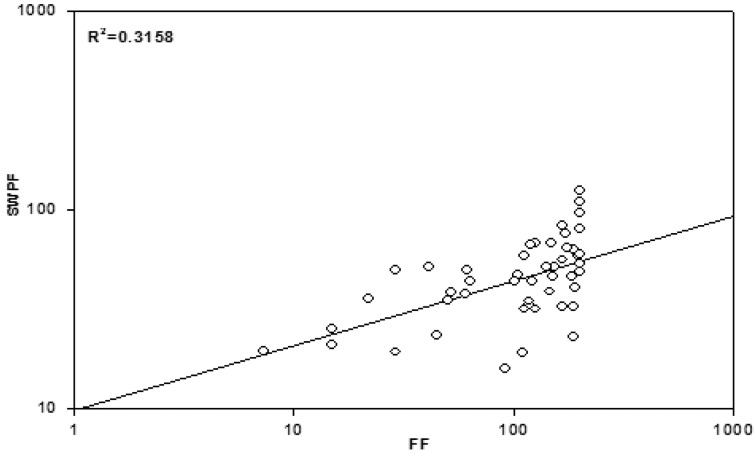
The relationship between FF and SWPF was analyzed using a regression analysis. When the fit factor was assessed regarding its effect on the SWPF, the explanatory power was 31.6% (Fig. 5).
Fig. 5.
Relationship between the overall SWPFs and FFs for three scenarios.
Real-time SWPF
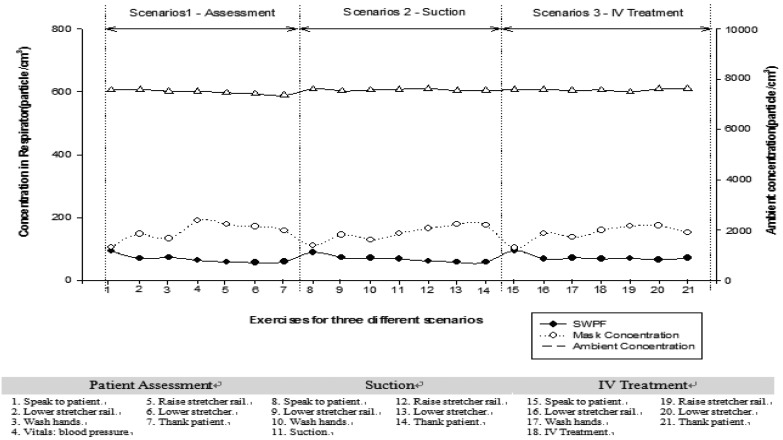
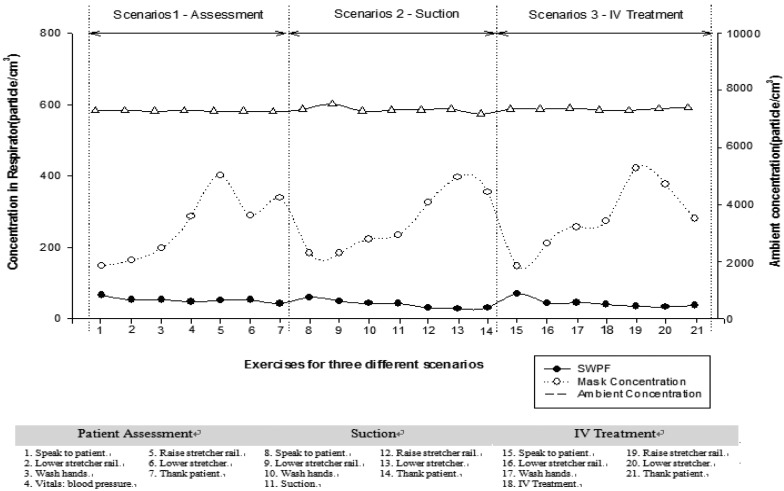
The mean concentrations outside and inside the N95 respirator, and the mean real-time measurement values of SWPF for all the test subjects who either passed or failed the fit test were calculated for each exercise and presented in Figs. 6 and 7. The air-borne dust concentrations outside in the simulated medical environment ranged from 3,420 to 17,800 p/cm3. The particle concentrations inside the respirator ranged from 11 to 3,949 p/cm3, and the real-time SWPF values ranged from 1.4 to 364.
Fig. 6.
Fluctuations of particle concentrations (ambient and respirator) and overall SWPFs by exercise for three different scenarios from test subjects who passed the fit test.
Fig. 7.
Fluctuations of particle concentrations (ambient and respirator) and overall SWPFs by exercise for three different scenarios from test subjects who failed the fit test.
Among real-time SWPFs by scenario assessed, greater fluctuations were observed from the test subjects who failed the fit test. In addition, lower SWPFs were measured while performing the following movements; moving head up and down, and bending at the waist (e.g. raising and/or lowering the stretcher rails). Therefore, while performing these movements, respirator seals around the face might have been broken and thus allowed particles leaked in the respirator, particularly from those who failed the fit test.
Discussion
In medical environments, HCWs may reduce their risk of infection by wearing N95 respirators from infected patients and inhalation of contaminated substances in the air. A fit test was performed in this study to determine the protective effect of wearing the N95 respirator targeting HCWs, including nurses and nursing students, who are frequently exposed to health care-related infection mediated by droplets or air-borne pathogens. A simulated medical environment that is similar to real-world medical environments was created for the study. Three health-care tasks, selected by a field expert, namely patient assessment (measuring blood pressure), suction treatment, and IV treatment, were simulated and performed by the participants. The concentrations outside and inside the mask were measured in order to evaluate real-time SWPFs during the activities.
In the SWPF experiment, weak correlations (R2=0.316) between FF and SWPF were found in this study. The result was similar to that of the previous studies that showed a low correlation between two values17, 20,21,22). Another study done with the powered air purifying respirator29) found no correlation between QNFT and WPF. But, a previous research done in a simulated environment found that fit factor was found to be highly correlated with actual exposure measurement values in the simulated medical workplace18). Unidentified individual-specific variables were speculated to affect correlation variations13). However some exercises in this study, such as moving head up and down and bending over, were more influential on SWPF than others. During the assessment of real-time SWPFs, these movements were found to affect the degree of fit of the respirator. These influencing movements or activities need to be carefully managed during patients’ care so as to minimize the breakage of the respirator seals.
In contrast, a study on the real-time identification of the protection factor according to OSHA Protocol 1910.13433) showed that among the SWPFs, talking or grimace was more frequent than other activities34, 35). Hauge et al. study18), however, found no specific activities (e.g., talking or movement) to be related with the inside-respirator concentrations. Since the FF exercises used in this study were composed of only 6 exercises, excluding grimace, we had no information on the effects of grimace. Performing QNFT for respirator wearers is useful in terms of providing valuable training of donning as well as selecting correct sizes. But passing QNFT does not necessarily guarantee wearers’ protection because of lack of correlations with SWPF or WPF, a refinement of QNFT exercises so as better predict SWPF or WPF needs to be done.
All the subjects in this study, except three (3) subjects, wore small-size N95 respirators. This finding was similar to that of a study with subjects from the NIOSH panel 1–7 that showed maximum fit with the S-size respirator. Meanwhile, the subjects from test panel 8–10 exhibited maximum fit with the M-size respirator24, 25). In addition, according to the study with the NIOSH panel, subjects with small/ medium, or large facial dimensions who wore S- or M-size respirator, respectively, exhibited better fit24, 25). According to the result of the fit test, the pass rate was 73.5% (36 persons) among the 49 test subjects. This was higher than the result of the QNFT experiment using the same N95 respirator model, which showed a pass rate of 57.4%30). The US Centers for Disease Control and Prevention (CDC) indicated that the QNFT fail rate of the N95 respirator was 20–100%31) and recommended the use of respirator products with an optimal fit for each individual32). The result indicated that respirator wearers should be provided different sizes of respirators so as to decide a correct size for them after QNFT.
A limitation of this study is the difference in considering such influencing factors from those in real workplaces. For example, influencing factors, including the effect of duration of rewearing a respirator, the model or size of other respirators, and the effect of face size or type, have different effects on fit18). In addition, the ambient air particle concentrations in the simulated room, which were generally stable throughout the experiment, may be quite different from the real world situations where high and fluctuating concentrations can be found.
In a series of health care simulation studies by NIOSH researchers17, 33), several activities besides OSHA exercises were included such as, hanging an IV bag, inserting a syringe into an IV bag, carrying weight, and walking, etc. Although it is judged that this study did not fully consider influencing factors in real workplaces, we believe that a further study that compensates for these activities will provide HCWs with a higher level of protection with the use of respirators.
Despite of these shortcomings, this study evaluated the performance of the N95 respirator through the fit test, targeting health care workers, and identified levels of protection depending on the wearers’ activities by performing a real-time SWPF evaluation. We found that even with a high-quality respirator, if the respirator is not worn properly or the respirator size is not optimal, an adequate protection could not be provided to HCWs, who have a high risk of exposure to air-borne diseases such as tuberculosis due to their job activities and work environments.
Conclusions
This study aimed to determine the degree of protection that the N95 respirator provides to HCWs by performing a real-time SWPF evaluation. Test subjects performed 3 types of scenarios in a simulated patient treatment environment. In the SWPF evaluation depending on task, the concentration inside the respirators of the subjects who failed the fit test exhibited a higher fluctuation than that of the test subjects who passed the fit test. Because actions such as raising a rail or lowering a bed, which requires moving the head down or bending at waist, affect the fit level of the respirator, the concentration inside the respirator in each scenario tended to have a higher variation.
During the experiment, we found that particular movements, such as bending at the waist and moving head up and down, were identified as contributing factors affecting more on SWPFs. Therefore, it is necessary to perform the fit test using simulated activities of the real workplaces. Performing the fit test before distributing respirators and training the proper use of respirators seem to be very important for HCWs. Considering the recent increase in the incidence of air-borne diseases such as tuberculosis among HCWs, a better respiratory protection program with regular trainings should be provided in order to protect them from infectious diseases. This study also identified the needs for providing different sizes of respirators for HCWs.
Acknowledgments
This study was supported by a basic research fund from 3 M Korea in 2014. Also a set of TSI fit testing equipment was donated by APM Engineering. We appreciate both companies for supporting this research.
References
- 1.Kang JO. (2011) Occupational infections of health care personnel in Korea. Hanyang Med Rev 31, 200–10. [Google Scholar]
- 2.The Occupational Safety and Health Research Institute (2002) A study on development health administration manual of health care workers. The Occupational Safety and Health Research Institute, Korea. [Google Scholar]
- 3.Jung SY. (2011) How to prevent transmission of infectious agents in healthcare settings. Hanyang Med Rev 31, 190–9. [Google Scholar]
- 4.World Health Organization (2011) Global tuberculosis control: WHO report 2011, World Health Organization, Geneva. [Google Scholar]
- 5.MOH (2005) Prevention of nosocomial infection control guideline. Ministry of Health & Welfare, Korea. [Google Scholar]
- 6.Colton CE, Birkner LR, Brosseau LM. (1991) Respiratory Protection: A Manual and Guideline, 2nd Ed., American Industrial Hygiene Association, Akron. [Google Scholar]
- 7.Noti JD, Lindsley WG, Blachere FM, Cao G, Kashon ML, Thewlis RE, McMillen CM, King WP, Szalajda JV, Beezhold DH. (2012) Detection of infectious influenza virus in cough aerosols generated in a simulated patient examination room. Clin Infect Dis 54, 1569–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee SA, Grinshpun SA, Adhikari A, Li W, McKay R, Maynard A, Reponen T. (2005) Laboratory and field evaluation of a new personal sampling system for assessing the protection provided by the N95 filtering facepiece respirators against particles. Ann Occup Hyg 49, 245–57. [DOI] [PubMed] [Google Scholar]
- 9.Lee SA, Grinshpun SA, Reponen T. (2008) Respiratory performance offered by N95 respirators and surgical masks: human subject evaluation with NaCl aerosol representing bacterial and viral particle size range. Ann Occup Hyg 52, 177–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oberg T, Brosseau LM. (2008) Surgical mask filter and fit performance. Am J Infect Control 36, 276–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dixon SW, Nelson TJ. (1984) Workplace protection factors for negative pressure half-mask facepiece respirators. J Int Soc Resp Prot 2, 347–61. [Google Scholar]
- 12.Myers WR, Peach MJ., 3rd (1983) Performance measurements on a powered air-purifying respirator made during actual field use in a silica bagging operation. Ann Occup Hyg 27, 251–9. [DOI] [PubMed] [Google Scholar]
- 13.Byeon SH, Na MC, Kim HW, Lim HS. (1999) Evaluation of workplace protection factors for some half—facepiece respirators in welding workplace. J Korean Soc Occup Environ Hyg 9, 14–22. [Google Scholar]
- 14.NIOSH (1987) NIOSH Guide to Industrial Respiratory Protection, No. 87–116, U.S Department of Health and Human Services. National Institute for Occupational Safety and Health, Cincinnati. [Google Scholar]
- 15.Myers WR, Lenhart SW, Campell K, Provost G. (1983) Letter to the editor. Am Ind Hyg Assoc J 44, B25–6. [Google Scholar]
- 16.Coffey CC, Campbell DL, Myers WR, Zhuang Z, Das S. (1998) Comparison of six respirator fit-test methods with an actual measurement of exposure in a simulated health care environment: part I—protocol development. Am Ind Hyg Assoc J 59, 852–61. [DOI] [PubMed] [Google Scholar]
- 17.Coffey CC, Campbell DL, Myers WR, Zhuang Z. (1998) Comparison of six respirator fit-test methods with an actual measurement of exposure in a simulated health care environment: part II—method comparison testing. Am Ind Hyg Assoc J 59, 862–70. [DOI] [PubMed] [Google Scholar]
- 18.Hauge J, Roe M, Brosseau LM, Colton C. (2012) Real-time fit of a respirator during simulated health care tasks. J Occup Environ Hyg 9, 563–71. [DOI] [PubMed] [Google Scholar]
- 19.Landsittel D, Zhuang Z, Newcomb W, Berry Ann R. (2014) Determining sample size and a passing criterion for respirator fit-test panels. J Occup Environ Hyg 11, 77–84. [DOI] [PubMed] [Google Scholar]
- 20.Kim HW, Kim KY. (2011) Review on the development of 3—dimensional face recognition and measurement for the design of respirators. J Korean Soc Occup Environ Hyg 11, 92–101. [Google Scholar]
- 21.Han DH, Choi KL. (2002) Development of half-masks well-fitting for Korean faces (1)—facial dimensions and predictors of fit for half-mask. J Korean Soc Occup Environ Hyg 12, 46–54. [Google Scholar]
- 22.Han DH, Rhi JY. (2004) Development of half-masks well-fitting for Korean faces (2)—pilot study—. J Korean Soc Occup Environ Hyg 14, 8–17. [Google Scholar]
- 23.Hack AL, McConville JT. (1978) Respirator protection factors: part I—development of an anthropometric test panel. Am Ind Hyg Assoc J 39, 970–5. [DOI] [PubMed] [Google Scholar]
- 24.Zhuang Z, Groce D, Ahlers HW, Iskander W, Landsittel D, Guffey S, Benson S, Viscusi D, Shaffer RE. (2008) Correlation between respirator fit and respirator fit test panel cells by respirator size. J Occup Environ Hyg 5, 617–28. [DOI] [PubMed] [Google Scholar]
- 25.Zhuang Z, Bradtmiller B, Shaffer RE. (2007) New respirator fit test panels representing the current U.S. civilian work force. J Occup Environ Hyg 4, 647–59. [DOI] [PubMed] [Google Scholar]
- 26.Size Korea. Size Korea of Standardization anthropometry. http://sizekorea.kr/01_sizekorea/research.asp?OlapCode=SIZU0102 Accessed February 19, 2014.
- 27.OSHA Fit Testing Procedures (Mandatory). https://www.osha.gov/pls/oshaweb /owadisp.show_document?p_table=STANDARDS&p_id=9780. Accessed August 4, 2014.
- 28.Inc TSI (2001) PortaCount Plus TM Model 8020 Operation and Service Manual (Product Manual), TSI Inc, St. Paul. [Google Scholar]
- 29.Myers WR, Peach MJ, 3rd, Cutright K, Iskander W. (1984) Workplace protection factor measurements on powered air-purifying respirators at a secondary lead smelter: results and discussion. Am Ind Hyg Assoc J 45, 681–8. [DOI] [PubMed] [Google Scholar]
- 30.Lam SC, Lee JK, Yau SY, Charm CY. (2011) Sensitivity and specificity of the user-seal-check in determining the fit of N95 respirators. J Hosp Infect 77, 252–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention (CDC) (1998) Laboratory performance evaluation of N95 filtering facepiece respirators, 1996. MMWR Morb Mortal Wkly Rep 47, 1045–9. [PubMed] [Google Scholar]
- 32.Derrick JL, Chan YF, Gomersall CD, Lui SF. (2005) Predictive value of the user seal check in determining half-face respirator fit. J Hosp Infect 59, 152–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.OSHA (1998) Respiratory Protection: 29 CFR 1910.134, Appendix A., US Department of Labor, Occupational Safety and Health Administration, Washington, DC. [Google Scholar]
- 34.Coffey CC, Campbell DL, Myers WR. (1999) Comparison of six respirator fit-test methods with an actual measurement of exposure in a simulated health care environment: part III—validation. Am Ind Hyg Assoc J 60, 363–6. [DOI] [PubMed] [Google Scholar]
- 35.Coffey CC, Lawrence RB, Campbell DL, Zhuang Z, Calvert CA, Jensen PA. (2004) Fitting characteristics of eighteen N95 filtering-facepiece respirators. J Occup Environ Hyg 1, 262–71. [DOI] [PubMed] [Google Scholar]