Abstract
Objectives:
To explore the interrelationship and mediating effect of factors that are beneficial (i.e., antioxidants) and harmful (i.e., inflammation and oxidative stress) to the relationship between sleep and cardiometabolic health.
Design:
Cross-sectional data from the 2005–2006 National Health and Nutrition Examination Survey.
Setting:
Nationally representative population sample from the US.
Participants:
Age ≥ 20 y with sleep data; final analytical sample of n = 2,079.
Interventions:
N/A.
Measurements and Results:
Metabolic syndrome was classified according to the Joint Interim Statement, and sleep duration was categorized as very short, short, adequate, and long sleepers (≤ 4, 5–6, 7–8, and ≥ 9 h per night, respectively). The indirect mediation effect was quantified as large (≥ 0.25), moderate (≥ 0.09), modest (≥ 0.01), and weak (< 0.01). In general, inflammation was above the current clinical reference range across all sleep duration categories, whereas oxidative stress was elevated among short and very short sleepers. Select sleep duration– cardiometabolic health relationships were mediated by C-reactive protein (CRP), γ-glutamyl transferase (GGT), carotenoids, uric acid, and vitamins C and D, and were moderated by sex. Specifically, moderate-to-large indirect mediation by GGT, carotenoids, uric acid, and vitamin D were found for sleep duration–waist circumference and –systolic blood pressure relationships, whereas vitamin C was a moderate mediator of the sleep duration–diastolic blood pressure relationship.
Conclusions:
Several factors related to inflammation, oxidative stress, and antioxidant status were found to lie on the casual pathway of the sleep duration–cardiometabolic health relationship. Further longitudinal studies are needed to confirm our results.
Citation:
Kanagasabai T, Ardern CI. Contribution of inflammation, oxidative stress, and antioxidants to the relationship between sleep duration and cardiometabolic health. SLEEP 2015;38(12):1905–1912.
Keywords: antioxidants, cardiometabolic health, indirect mediation effect, inflammation and oxidative stress, sleep duration
INTRODUCTION
Sleep is important for maintaining health in almost all species on earth. In humans, evidence in the US suggests that sleep duration has decreased since the 1960s by approximately 1.5–2 h per day.1 Both short and long sleep durations are associated with increased risk for cardiometabolic dysfunction or metabolic syndrome (MetS).2 MetS is a cluster of cardio-metabolic risk factors, predominantly abdominal obesity, elevated plasma glucose, dyslipidemia, and blood pressure, that increases the risk for developing cardiovascular disease (CVD), diabetes, and certain types of cancers.3–5
Inflammation has an important role in the development of chronic diseases such as cancer, rheumatoid arthritis, asthma, neurodegenerative diseases, diabetes, and CVD.5,6 However, whether inflammation causes oxidative stress (or vice versa) is not clear, as reactive oxygen or nitrogen species can induce cellular damage and initiate inflammation.6,7 Fortunately, inflammation and oxidative stress can be sufficiently managed with endogenous and exogenous antioxidants.6 In those with MetS, inflammation and oxidative stress are increased, whereas antioxidants capacities are decreased.8–11 Similar relationships have been found among populations with sleep disorders,12–16 and one study has linked shift work to lower antioxidant capacities.17 To date, the effect of inflammation, oxidative stress, and antioxidants on sleep duration and cardiometabolic health in free-living adults is unknown.
The purpose of this study is to therefore (1) explore the interrelationship between sleep duration and inflammation (i.e., C-reactive protein [CRP]),5 oxidative stress (i.e., γ-glutamyl transferase [GGT]),11 and antioxidant capacities (i.e., bilirubin, carotenoids, uric acid, vitamins A, C, D, and E,8,9) and (2) to quantify the indirect mediating effect of these factors on the sleep duration–cardiometabolic health relationships in free-living adults.
METHODS
Participants
To address these questions, data from the US National Health and Nutrition Examination Survey (NHANES), a series of cross-sectional studies designed to assess the health and nutritional status of the US population, were used.18 NHANES began collecting data in the 1960s using interviews and physical examinations. Demographical, socioeconomic, dietary, and health-related questionnaires are used in the interview component. During the physical examination component, participants' medical, dental, and physiological details were collected by trained medical personnel.18,19 The average time between the interview and examination components of NHANES is 2 w. NHANES 2005–2006 cycle had an initial sample of 10,348 individuals. Subsequent exclusions were made for age (< 20 y: n = 5,369), missing sleep duration (n = 11), pregnancy (n = 335), and missing MetS components (nwaist circumference = 454, ntriglyceride = 196, nblood pressure = 79, nfasting plasma glucose = 1,825, and n HDL cholesterol = 0) for a final analytic sample of 2,079.
Metabolic Syndrome and Cardiometabolic Health
MetS was classified according to the Joint Interim Statement [≥ 3 measures of elevated waist circumference: men (≥ 102 cm), women (≥ 88 cm); elevated triglycerides or medication: ≥ 1.69 mM; low high-density lipoprotein (HDL) cholesterol or medication: men (< 1.04 mM), women (< 1.29 mM); elevated blood pressure or medication: systolic (≥ 130 mmHg) and/or diastolic (≥ 85 mmHg), and; elevated fasting plasma glucose or medication use (≥ 5.6 mM)].4 Number of MetS components [0, 1, 2, 3, 4, 5] were the sums of the aforementioned criteria. Cardiometabolic health markers were the individual MetS components.
Sleep Duration
The Sleep Disorders Questionnaire was administered to participants aged ≥ 16 y who reported their typical sleep duration per night on weekdays or workdays, and responses were collected as whole numbers [1 to 11, and ≥ 12 h].18,19 Sleep duration was obtained from a single question [“How much sleep do you usually get at night on weekdays or workdays?”] from the Sleep Disorders Questionnaire, and categorized as ≤ 4, 5–6, 7–8, and ≥ 9 h per night (very short, short, adequate, and long sleepers, respectively).20,21
Mediators and Population Descriptors
Laboratory measures of CRP, GGT, bilirubin, carotenoids, uric acid, and vitamins A, C, D, and E were considered as potential mediators of the sleep duration–cardiometabolic health relationships.19 Other variables used to describe the study population were age (20 to < 40 y, 40 to < 65 y, and ≥ 65 y), sex, ethnicity (Non-Hispanic White, Non-Hispanic Black, Mexican American, and Other), income, education, alcohol intake, smoking history, and recreational physical activity (PA) adherence. Smoking was categorized as current, past (if smoked ≥ 100 cigarettes in one's life but not a current smoker) or never (if smoked < 100 cigarettes in one's life or reported never smoking). Educational attainment was categorized as < high school, high school, college; income as < $20,000, $20,000–44,999, and ≥ $45,000; and, alcohol intake as 0, < 3, and ≥ 3 drinks per day.22 For recreational PA adherence, the metabolic equivalent (MET) scores given by NHANES were used to calculate MET min/w, which were then categorized as no reported PA data, low PA (< 500 MET min/w), and guideline adherence (≥ 500 MET min/w).19,23
Statistics
Mean and 95% confidence interval (CI) for continuous variables, and frequency (%) and 95% CI for categorical variables were determined for each sleep duration category. Differences in demographic and behavioral characteristics of participants were assessed with analysis of variance and χ2 tests, as appropriate. The interrelationship between sleep duration, and CRP, GGT, bilirubin, carotenoids, uric acid, and vitamins A, C, D, and E were determined and displayed in relation to the American Medical Association's clinical reference ranges.24 Post hoc Tukey's test was used to determine whether significant differences between the sleep duration groups versus 7–8 h sleep duration exist. The indirect mediation effect of CRP, GGT, bilirubin, carotenoids, uric acid, and vitamins A, C, D, and E on the sleep duration–cardiometabolic health relationships were estimated using logistic regression for dichotomous outcomes and linear regression for continuous outcomes.25
Indirect mediation effect was estimated in a series of regression analyses (Figure 1). Briefly, mediation analysis helps to explain the underlying mechanism between an independent and a dependent variable by a third explanatory variable, i.e., a mediator.25 The paths of a mediation analysis are as follows: path a is a regression between exposure and mediator; path b is a regression between mediator and outcome while adjusting for the exposure; path c is a regression between exposure and outcome, and; path c' is a regression between exposure and outcome while adjusting for the mediator (Figure 1).25 For each mediation analysis, participants with the missing mediating variable were excluded to ensure the products of ab and c-c', estimates of indirect mediation, were equivalent.25 Large, moderate, modest, and weak indirect mediation effects were classified as ≥ 0.25, ≥ 0.09, ≥ 0.01, and < 0.01, respectively, based on recommendations.25 To detect a moderate mediation effect of ≥ 0.09 with 80% power, 105 participants in each sleep duration category were required. Both the Sobel test and joint significance test were used to evaluate the significance of the indirect effect. All analyses were weighted with the medical examination sample weights to represent the US adult population. Analyses were conducted using SAS version 9.3 (Cary, NC, USA) with statistical significance set at an α of 0.05.
Figure 1.
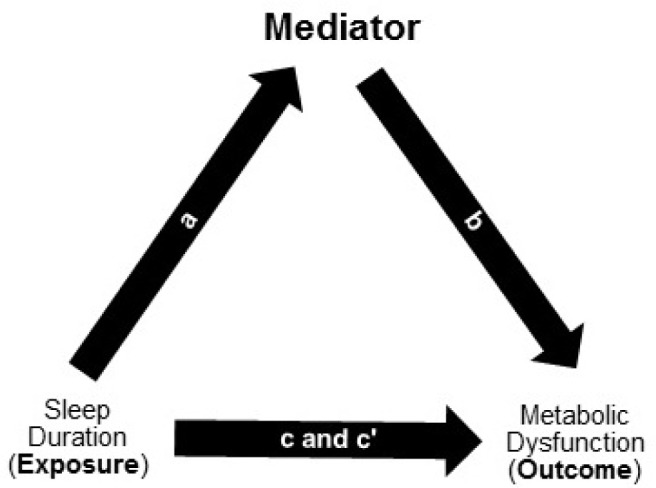
Multiple regression method of the indirect mediation model.25 a indicates the path from sleep durations (exposure) to mediator (i.e., inflammation, oxidative stress, and antioxidant. b indicates the path from mediator to outcome (i.e., metabolic syndrome (MetS), number of MetS components, and individual MetS components) controlling for the mediator. c indicates the path from exposure to outcome. c' indicates the path from exposure to outcome controlling for the mediator.
RESULTS
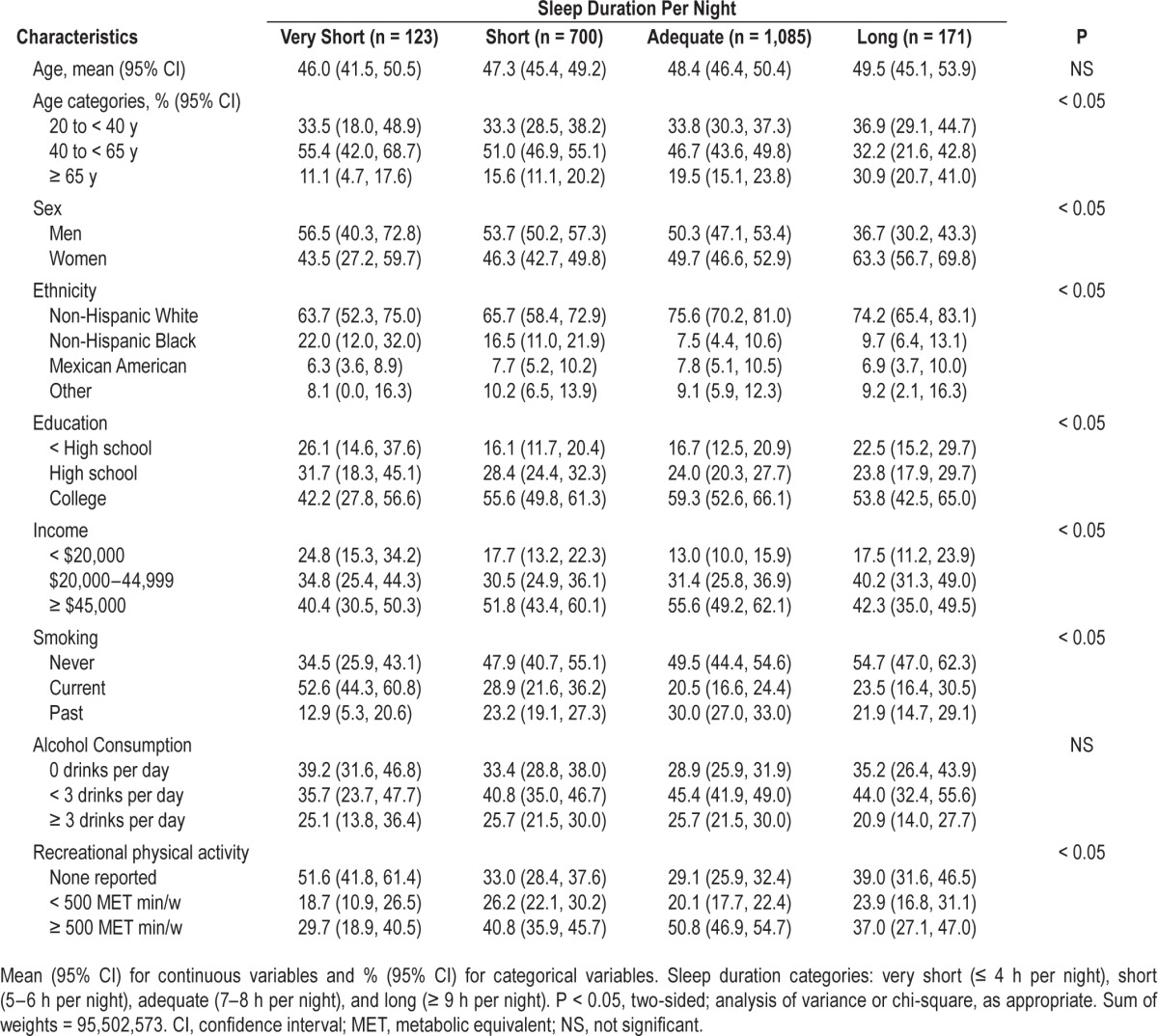
Table 1 describes the sample characteristics, stratified by categories of sleep duration. In general, sleep duration varied by both modifiable (physical activity and smoking) and non-modifiable (sex, age, ethnicity, education, and income) factors. Specifically, middle-aged adults (40 to < 65 y) tended to be very short, short, and adequate sleepers, whereas older adults (≥ 65 y) were long sleepers. Short and very short sleep durations were more common among men, non-Hispanic Blacks, current smokers, and those reporting the lowest household income (< $20,000). Adequate sleepers tended to be non-Hispanic Whites, noncurrent smokers, report higher household income and educational attainment, and adhere to the PA guidelines.
Table 1.
Characteristics of the US adult population ≥ 20 y of age.
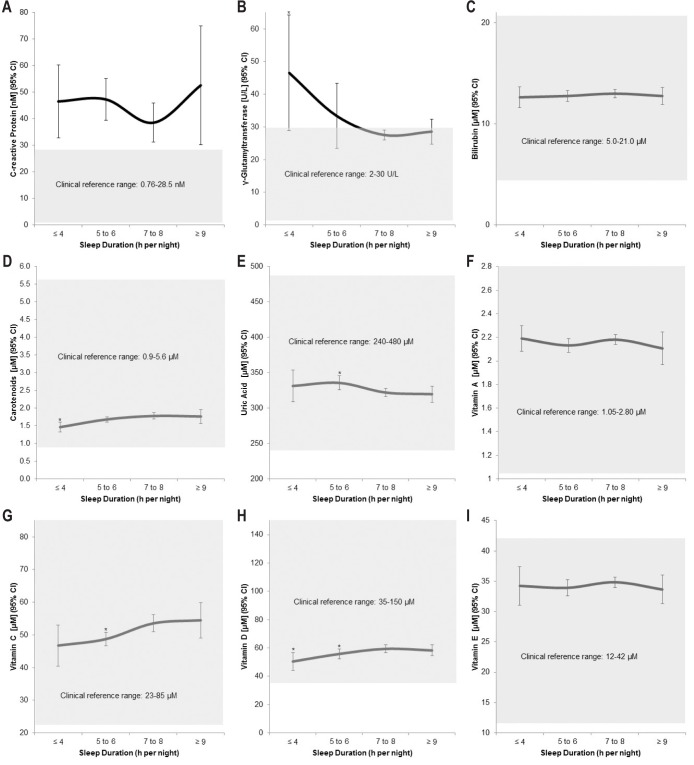
As expected, those who slept 7–8 h per night (i.e., adequate sleepers) had the optimal inflammation (Figure 2A), oxidative stress (Figure 2B), and antioxidants (Figures 2C–2I) profiles. Short sleep duration was associated with elevated CRP, GGT, uric acid, and vitamin A levels, and lower bilirubin, carotenoids, and vitamin C, D, and E levels. Compared to 7–8 h sleep duration, short or very short sleep duration was associated with significantly lower carotenoids and vitamins C and D levels. GGT and uric acid were higher among those with very short and short sleep durations, respectively. Further, CRP level was higher than the clinical reference range (gray shaded area) among all sleep durations, but lowest among adequate sleepers. Compared to the clinical reference range, GGT was also higher among short and very short sleepers; however, the antioxidants were within the reference ranges for all sleep durations.
Figure 2.
Interrelationship between sleep duration and inflammation (A), oxidative stress (B), and antioxidants (C–I). Gray shaded areas are clinical reference ranges.24 *P < 0.05 versus 7–8 h sleep duration.
Table 2 contains the estimated indirect effect for each mediator on the relationship between sleep duration–MetS and –number of MetS components. Overall, GGT, carotenoids, uric acid, and vitamins C and D were considered modest mediators (≥ 0.01 to < 0.09) of the sleep duration–MetS and –number of MetS components relationships. Table 3 contains the estimated indirect effect for the mediators on the sleep duration–individual MetS component relationships. In the analysis, carotenoids, uric acid, and vitamins C and D were large mediators (≥ 0.25) of the sleep duration–waist circumference relationship, whereas GGT was a moderate mediator (≥ 0.09 to < 0.25). GGT and carotenoids were moderate mediators of the sleep duration–systolic blood pressure relationship, whereas uric acid and vitamin D were large mediators. Vitamin C was a moderate mediator of the sleep duration–diastolic blood pressure relationship.
Table 2.
Indirect effect of mediators on the sleep duration–metabolic syndrome and number of metabolic syndrome components relationships.
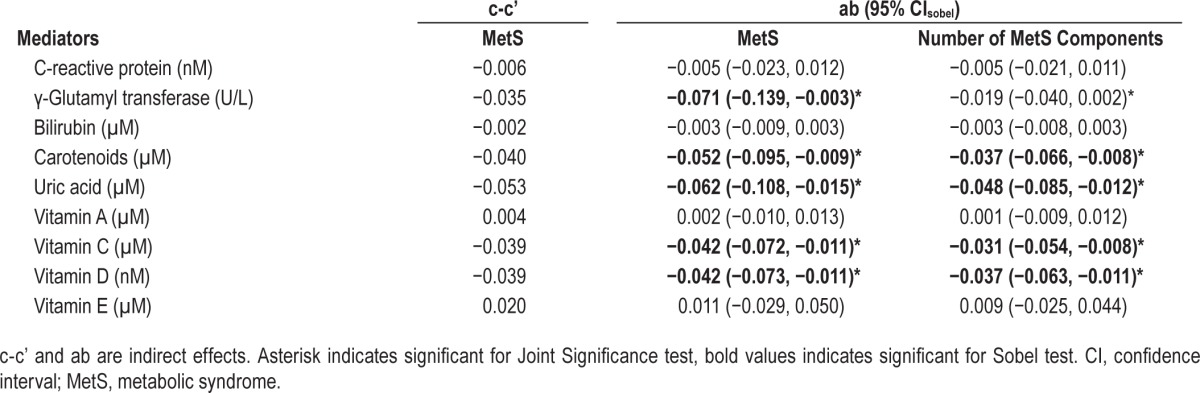
Table 3.
Indirect effect of mediators on the sleep duration–individual metabolic syndrome component relationship.
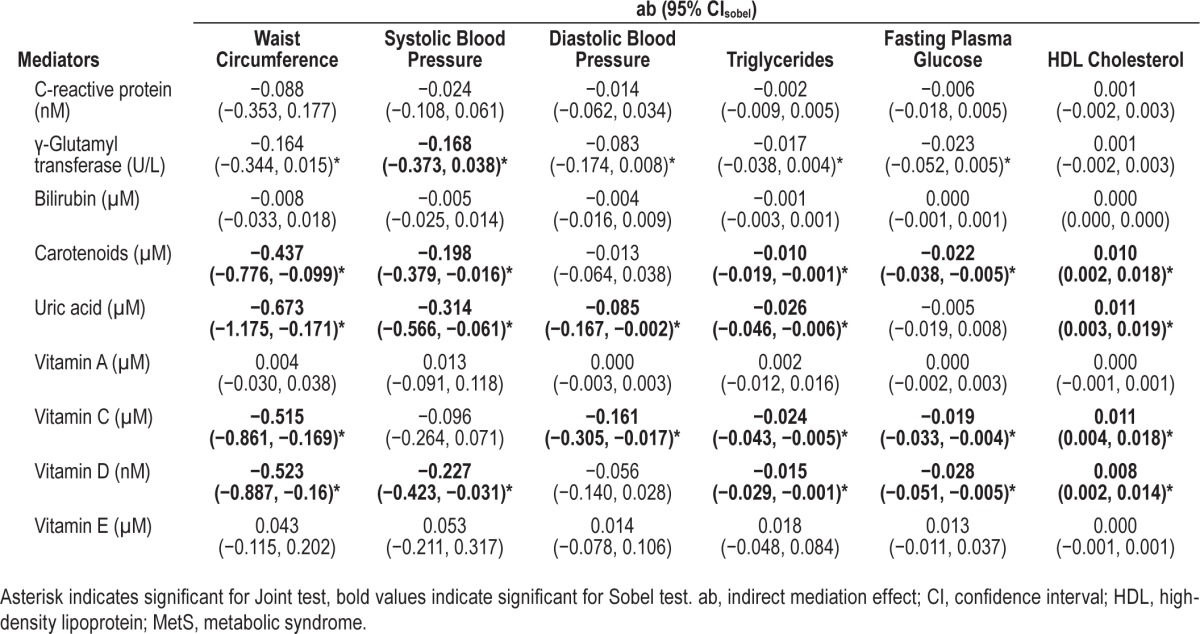
Sex differences in the indirect effects are provided in Tables S1 and S2 (supplemental material). Overall, no significant indirect effects were observed in men (data not shown). In women, carotenoids and vitamins C and D were modest-to-moderate mediators of the sleep duration–MetS and number of MetS components (Table S1), and large mediators of the sleep duration–waist circumference relationships (Table S2). Similarly, carotenoids and vitamin D were large mediators of the sleep duration–systolic blood pressure relationship, whereas vitamin C was a moderate mediator of the sleep duration–diastolic blood pressure.
DISCUSSION
In our study, short or very short sleep duration was more common among men and non-Hispanic Blacks; whereas those reporting adequate sleep were noncurrent smokers, non-Hispanic Whites, had higher education and income, and adhered to PA guidelines. Adequate sleepers also had better serum-measured inflammation, oxidative stress, and anti-oxidants profiles. Our findings suggest that GGT, carotenoids, uric acid, and vitamins C and D are modest mediators of the sleep duration–MetS relationship, which are largely due to the moderate-to-large mediating effect of these factors on the sleep duration–waist circumference, and –systolic/diastolic blood pressure relationships.
Inflammation, Oxidative Stress, and Antioxidants Profiles
Compared to short or long sleepers, adequate sleepers tend to have a healthier lifestyle, which is reflected in their inflammation, oxidative stress, and antioxidants profile.26 To date, only a few studies have considered the association between these factors and sleep. In clinical populations with sleep disorders, inflammation and oxidative stress are often elevated,13,27,28 whereas antioxidants are reduced.14–16 For instance, in patients with dyslipidemia and sleep apnea-hypopnea syndrome (n = 26), Murri et al.16 found that one month of continuous positive airway pressure treatment significantly decreased uric acid, and increased antioxidant capacity. This is consistent with our results: uric acid is increased among short sleep duration, but carotenoids, and vitamins C and D are decreased. Further, in the study by Murri et al.,16 both the pretreatment and posttreatment uric acid values were within the clinical reference range. In our study, all antioxidants were within the clinical reference range, but were optimal among adequate sleepers. Furthermore, our analysis suggests that CRP is high regardless of sleep duration, but is lowest among adequate sleepers; and, GGT is higher among short and very short sleep duration categories, but within clinical reference range amongst adequate sleepers. When taken together, these analyses suggest that adequate sleep duration is associated with an optimal inflammation, oxidative stress, and antioxidant profile.
Indirect Mediation Effect
Our second objective was to evaluate the mediating effect of inflammation, oxidative stress, and antioxidants on the relationship between sleep duration and cardiometabolic health. Although our overall finding suggests only modest mediating effects of GGT, carotenoids, uric acid, and vitamins C and D on the sleep duration–MetS and –number of MetS components relationships, the moderate-to-large mediating effects found for sleep duration–waist circumference and blood pressure relationships warrant discussion.
Waist Circumference
Previously, the mediating effects of oxidative stress, inflammation, and antioxidants on the sleep duration–waist circumference relationships were unknown. In general, literature suggests chronic inflammation and oxidative stress lie on the causal pathway of many age-related diseases, including CVD, diabetes, and cancers,6 but only our findings for GGT supports this. The lack of significant mediating effect for CRP in our study, however, may be due to it being an acute-phase marker of inflammation,29 and thus, exploring the mediating effect other inflammatory biomarkers (i.e., interleukin-6 and adiponectin) may provide insight into the role of inflammation on the sleep duration–abdominal obesity relationship.30 Further, the beneficial effects of a healthy diet on serum antioxidants and weight are well known.14,31 However, the inverse association between vitamin C and waist circumference may be moderated by sex.32 For vitamin D, Ford et al.33 found low levels of it significantly increased the odds of abdominal obesity; Cheng et al.34 found it was strongly associated with abdominal (β: −2.34, P < 0.0001), not subcutaneous (β: −1.12, P < 0.016), adiposity. Conversely, evidence for uric acid suggests a positive association with cardiometabolic risk,35 and weight gain: a 5-y follow up study (n = 433) found uric acid was a significant predictor of weight gain of > 10% in body mass index.36 Therefore, our findings provide initial evidence for the mediating role of oxidative stress and antioxidants on the sleep duration– abdominal obesity relationship.
Blood Pressures
Because of the known association between blood pressure and oxidative stress with antioxidants,36–39 we evaluated the mediating effect of these factors within the context of sleep duration. First, GGT and uric acid have been found to be good predictors of baseline and incident hypertension, which supports our finding that they lie on the casual pathway of the sleep duration–blood pressure relationships.36,38 Additionally, an inverse association between vitamin C and blood pressure in general39 and systolic blood pressure in older adults has been found.40 Vitamin C supplements also improved endothelial function in patients with obstructive sleep apnea15 and lowered systolic blood pressure in older adults.41 However, in our analysis we did not find vitamin C significantly mediated the sleep duration–systolic blood pressure relationship, which could have varied by age. Furthermore, our finding of moderate mediation for the sleep duration–systolic blood pressure relationship for vitamin D could have been distorted by other factors that were unadjusted in the analyses. For instance, a cross-sectional study found no significant association with systolic blood pressure after multivariable adjustments (β: −0.48, P = 0.08),34 whereas a meta-analysis found only a weak relationship in hypertensive individuals.37 However, the immune modulating role of vitamin D may also help explain our finding, which is supported by emerging evidence that vitamin D deficiency increases the risks of sleep disorders and CVD.42
Sex-Stratified Indirect Mediation Effect
We found that carotenoids and vitamins C and D were moderate-to-large mediators of several sleep duration–cardiometabolic health relationships in women only. This is supported by studies that have reported sex-based disparities in serum concentrations of some antioxidants.8,32 In the study by Beydoun et al.,8 significant differences between serum carotenoids, and vitamins C, D, and E levels, and MetS status were found in the sex-stratified analyses. In Johnston et al.'s32 study, vitamin C correlated with body composition measures in women only. This early evidence suggests that dietary and sleep-based interventions may be of particular benefit to women.
Strengths and Limitations
Our analyses are based on evidence that inflammation, oxidative stress, and antioxidants are contributors to both sleep quantity decrease and cardiometabolic dysfunction.6,15 Although this cross-sectional study provides initial evidence of their interrelationship, we cannot infer causality from our analyses alone, and future longitudinal studies are needed. Important limitations to our methodological approach are that we excluded all participants with missing cardiometabolic health data, which resulted in the loss of over 50% of the initial adult sample. Specifically, fasting plasma glucose was available for morning session participants only, and including the afternoon session participants would result in estimation error for our outcome variables (i.e., MetS and number of MetS components).9 However, the generalizability of our overall findings is unlikely to change by excluding them; and we have sufficient sample to have at least 80% power. Further, we used self-report sleep duration in our study, but the correlation between self-reported and objectively measured sleep duration is weak to moderate and varies across subpopulations.43 All analyses are based on single measurements of exposure, outcome, and mediators, even though inflammation, oxidative stress, and antioxidant levels may be altered by fluctuating dietary habits between questionnaire and examination components, geographic location, and supplement use.
CONCLUSIONS
Results from this study suggest that adequate sleep duration is an important contributor to cardiometabolic health. While difficult, the promotion of adequate sleep duration could improve inflammation, oxidative stress and antioxidant capacities, and act together to prevent or improve early cardio-metabolic dysfunction. In order to more fully understand the many factors that may contribute to this relationship, targeted longitudinal studies are needed.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. The work was performed at York University.
ACKNOWLEDGMENTS
The authors thank Professor George Monette, PhD and Ms. Mirka Ondrack, MSc of Statistical Consulting Services-Institute of Social Research at York University for their advice on mediation analysis.
ABBREVIATIONS
- CI
confidence interval
- CRP
C-reactive protein
- CVD
cardiovascular disease
- GGT
γ-Glutamyl transferase
- MET
metabolic equivalent
- MetS
metabolic syndrome
- NHANES
National Health and Nutrition Examination Survey
REFERENCES
- 1.Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008;9:S23–28. doi: 10.1016/S1389-9457(08)70013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ju S-Y, Choi W-S. Sleep duration and metabolic syndrome in adult populations: a meta-analysis of observational studies. Nutr Diabetes. 2013;3:e65. doi: 10.1038/nutd.2013.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Russo A, Autelitano M, Bisanti L. Metabolic syndrome and cancer risk. Eur J Cancer. 2008;44:293–7. doi: 10.1016/j.ejca.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 5.Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14,719 initially healthy American women. Circulation. 2003;107:391–7. doi: 10.1161/01.cir.0000055014.62083.05. [DOI] [PubMed] [Google Scholar]
- 6.Khansari N, Shakiba Y, Mahmoudi M. Chronic inflammation and oxidative stress as a major cause of age-related diseases and cancer. Recent Pat Inflamm Allergy Drug Discov. 2009;3:73–80. doi: 10.2174/187221309787158371. [DOI] [PubMed] [Google Scholar]
- 7.Scrivo R, Vasile M, Bartosiewicz I, et al. Inflammation as “common soil” of the multifactorial diseases. Autoimmun Rev. 2011;10:369–74. doi: 10.1016/j.autrev.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Beydoun MA, Shroff MR, Chen X, Beydoun HA, Wang Y, Zonderman AB. Serum antioxidant status is associated with metabolic syndrome among U.S. adults in recent national surveys. J Nutr. 2011;141:903–13. doi: 10.3945/jn.110.136580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ford ES, Mokdad AH, Giles WH, Brown DW. The metabolic syndrome and antioxidant concentrations: findings from the Third National Health and Nutrition Examination Survey. Diabetes. 2003;52:2346–52. doi: 10.2337/diabetes.52.9.2346. [DOI] [PubMed] [Google Scholar]
- 10.De Bona KS, Bonfanti G, Bitencourt PER, et al. Butyrylcholinesterase and γ-glutamyltransferase activities and oxidative stress markers are altered in metabolic syndrome, but are not affected by body mass index. Inflammation. 2013;36:1539–47. doi: 10.1007/s10753-013-9697-9. [DOI] [PubMed] [Google Scholar]
- 11.Bo S, Gambino R, Durazzo M, et al. Associations between gamma-glutamyl transferase, metabolic abnormalities and inflammation in healthy subjects from a population-based cohort: a possible implication for oxidative stress. World J Gastroenterol. 2005;11:7109. doi: 10.3748/wjg.v11.i45.7109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oyama J, Yamamoto H, Maeda T, Ito A, Node K, Makino N. Continuous positive airway pressure therapy improves vascular dysfunction and decreases oxidative stress in patients with the metabolic syndrome and obstructive sleep apnea syndrome. Clin Cardiol. 2012;35:231–6. doi: 10.1002/clc.21010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brady EM, Davies MJ, Hall AP, Talbot DC, Dick JL, Khunti K. An investigation into the relationship between sleep-disordered breathing, the metabolic syndrome, cardiovascular risk profiles, and inflammation between South Asians and Caucasians residing in the United Kingdom. Metab Syndr Relat Disord. 2012;10:152–8. doi: 10.1089/met.2011.0073. [DOI] [PubMed] [Google Scholar]
- 14.Svendsen M, Blomhoff R, Holme I, Tonstad S. The effect of an increased intake of vegetables and fruit on weight loss, blood pressure and antioxidant defense in subjects with sleep related breathing disorders. Eur J Clin Nutr. 2007;61:1301–11. doi: 10.1038/sj.ejcn.1602652. [DOI] [PubMed] [Google Scholar]
- 15.Grebe M, Eisele HJ, Weissmann N, et al. Antioxidant vitamin C improves endothelial function in obstructive sleep apnea. Am J Respir Crit Care Med. 2006;173:897–901. doi: 10.1164/rccm.200508-1223OC. [DOI] [PubMed] [Google Scholar]
- 16.Murri M, Alcázar-Ramírez J, Garrido-Sánchez L, et al. Oxidative stress and metabolic changes after continuous positive airway pressure treatment according to previous metabolic disorders in sleep apneahypopnea syndrome patients. Transl Res. 2009;154:111–21. doi: 10.1016/j.trsl.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Sharifian A, Farahani S, Pasalar P, Gharavi M, Aminian O. Shift work as an oxidative stressor. J Circadian Rhythms. 2005;3:15. doi: 10.1186/1740-3391-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.NCHS. NHANES - About the National Health and Nutrition Examination Survey. [Accessed December 27, 2014]. Available at: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 19.NCHS. NHANES - NHANES 2005-2006 - Manuals. [Accessed December 27, 2014]. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/manuals05_06.htm.
- 20.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–4. [PubMed] [Google Scholar]
- 21.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 22.Kanagasabai T, Nie JX, Mason C, et al. Metabolic syndrome and prevalent any-site, prostate, breast and colon cancers in the US adult population: NHANES 1999-2010. J Metab Synd. 2014;3:135. [Google Scholar]
- 23.Physical activity guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2008. [Google Scholar]
- 24.AMA. SI Conversion Calculator - AMA Manual of Style. [Accessed April 12, 2014]. Available at: http://www.amamanualofstyle.com/page/si-conversion-calculator.
- 25.Kenny DA. Mediation. 2013. [Accessed October 3, 2013]. Available at: http://davidakenny.net/
- 26.Ohida T, Kamal AM, Uchiyama M, et al. The influence of lifestyle and health status factors on sleep loss among the Japanese general population. Sleep. 2001;24:333–8. doi: 10.1093/sleep/24.3.333. [DOI] [PubMed] [Google Scholar]
- 27.Lin Q-C, Chen L-D, Yu Y-H, Liu KX, Gao SY. Obstructive sleep apnea syndrome is associated with metabolic syndrome and inflammation. Eur Arch Otorhinolaryngol. 2014;271:825–31. doi: 10.1007/s00405-013-2669-8. [DOI] [PubMed] [Google Scholar]
- 28.Kanbay A, Kaya E, Buyukoglan H, et al. Serum gamma-glutamyl transferase activity is an independent predictor for cardiovascular disease in obstructive sleep apnea syndrome. Respir Med. 2011;105:637–42. doi: 10.1016/j.rmed.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 29.Festa A, D'Agostino R, Tracy RP, et al. Elevated levels of acute-phase proteins and plasminogen activator inhibitor-1 predict the development of type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetes. 2002;51:1131–7. doi: 10.2337/diabetes.51.4.1131. [DOI] [PubMed] [Google Scholar]
- 30.Mangge H, Almer G, Truschnig-Wilders M, Schmidt A, Gasser R, Fuchs D. Inflammation, adiponectin, obesity and cardiovascular risk. Curr Med Chem. 2010;17:4511–20. doi: 10.2174/092986710794183006. [DOI] [PubMed] [Google Scholar]
- 31.Sluijs I, Beulens JWJ, Grobbee DE, van der Schouw YT. Dietary carotenoid intake is associated with lower prevalence of metabolic syndrome in middle-aged and elderly men. J Nutr. 2009;139:987–92. doi: 10.3945/jn.108.101451. [DOI] [PubMed] [Google Scholar]
- 32.Johnston CS, Beezhold BL, Mostow B, et al. Plasma vitamin C is inversely related to body mass index and waist circumference but not to plasma adiponectin in nonsmoking adults. J Nutr. 2007;137:1757–62. doi: 10.1093/jn/137.7.1757. [DOI] [PubMed] [Google Scholar]
- 33.Ford ES, Ajani UA, McGuire LC, Liu S. Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care. 2005;28:1228–30. doi: 10.2337/diacare.28.5.1228. [DOI] [PubMed] [Google Scholar]
- 34.Cheng S, Massaro JM, Fox CS, et al. Adiposity, cardiometabolic risk, and vitamin D status: the Framingham Heart Study. Diabetes. 2010;59:242–8. doi: 10.2337/db09-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li Q, Yang Z, Lu B, et al. Serum uric acid level and its association with metabolic syndrome and carotid atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol. 2011;10:72. doi: 10.1186/1475-2840-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masuo K, Kawaguchi H, Mikami H, Ogihara T, Tuck ML. Serum uric acid and plasma norepinephrine concentrations predict subsequent weight gain and blood pressure elevation. Hypertension. 2003;42:474–80. doi: 10.1161/01.HYP.0000091371.53502.D3. [DOI] [PubMed] [Google Scholar]
- 37.Witham MD, Nadir MA, Struthers AD. Effect of vitamin D on blood pressure: a systematic review and meta-analysis. J Hypertens. 2009;27:1948–54. doi: 10.1097/HJH.0b013e32832f075b. [DOI] [PubMed] [Google Scholar]
- 38.Cheung BM, Ong K-L, Tso AW, et al. Gamma-glutamyl transferase level predicts the development of hypertension in Hong Kong Chinese. Clin Chim Acta. 2011;412:1326–31. doi: 10.1016/j.cca.2011.03.030. [DOI] [PubMed] [Google Scholar]
- 39.Ness AR, Chee D, Elliott P. Vitamin C and blood pressure-an overview. J Hum Hypertens. 1997;11:343–50. doi: 10.1038/sj.jhh.1000423. [DOI] [PubMed] [Google Scholar]
- 40.Bates CJ, Walmsley CM, Prentice A, et al. Does vitamin C reduce blood pressure? Results of a large study of people aged 65 or older. J Hypertens. 1998;16:925–32. doi: 10.1097/00004872-199816070-00005. [DOI] [PubMed] [Google Scholar]
- 41.Fotherby MD, Williams JC, Forster LA, Craner P, Ferns GA. Effect of vitamin C on ambulatory blood pressure and plasma lipids in older persons. J Hypertens. 2000;18:411–5. doi: 10.1097/00004872-200018040-00009. [DOI] [PubMed] [Google Scholar]
- 42.McCarty DE, Chesson AL, Jr, Jain SK, Marino AA. The link between vitamin D metabolism and sleep medicine. Sleep Med Rev. 2014;18:311–9. doi: 10.1016/j.smrv.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 43.Van De Water ATM, Holmes A, Hurley DA. Objective measurements of sleep for non-laboratory settings as alternatives to polysomnography - a systematic review. J Sleep Res. 2011;20:183–200. doi: 10.1111/j.1365-2869.2009.00814.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.