Abstract
Objectives
1) Identify life satisfaction trajectories after moderate to severe traumatic brain injury (TBI), 2) establish a predictive model for these trajectories across the first 5 years post-injury, and 3) describe differences in these life satisfaction trajectory groups, focusing on age, depressive symptoms, disability, and participation in specific life roles,.
Research Method
Analysis of the longitudinal TBI Model Systems National Database was performed on data collected prospectively at 1, 2, and 5 years post-TBI. Participants (n=3,012) had a moderate to severe TBI and were 16 years old and older.
Results
Four life satisfaction trajectories were identified across the first 5 years post-injury, including: Stable Satisfaction, Initial Satisfaction Declining, Initial Dissatisfaction Improving, and Stable Dissatisfaction. Age, depressive symptoms, cognitive disability, and life role participation as a worker, leisure participant, and/ or religious participant at one year post-injury significantly predicted trajectory group membership. Life role participation and depressive symptoms were strong predictors of life satisfaction trajectories across the first 5 years post TBI.
Conclusions
The previously documented loss of life roles and prevalence of depression after a moderate to severe TBI make this a vulnerable population for whom low or declining life satisfaction is a particularly high risk. Examining individual life role participation may help to identify relevant foci for community-based rehabilitation interventions or supports.
Keywords: life satisfaction, life roles, participation, depression, brain injury
Introduction
Life satisfaction is a critical and fluctuating outcome for individuals with acquired disabilities, particularly for those who experience ongoing cognitive and behavioral changes, pain and fatigue, and affective disorders (Dijkers, 2004; Fuhrer, 2000; Resch et al., 2009). Life satisfaction refers to an individual’s cognitive appraisal of his or her overall life. This global appraisal is influenced by satisfaction in those life domains or life roles that are most relevant to each individual (Diener & Suh, 1998; Dijkers, 2004). Individuals with moderate to severe traumatic brain injuries (TBI) often report relatively low life satisfaction initially after injury (Cicerone & Azulay, 2007; Williamson et al., 2013) and over time (Grauwmeijer, Heijenbrok-Kal, & Ribbers, 2014; Resch et al., 2009). Life satisfaction after moderate or severe TBI is associated with multiple factors, including race (Sander, Pappadis, Clark, & Struchen, 2011), income (Tsaousides et al., 2009), driving status (Corrigan et al., 2001), age (Tsaousides et al., 2009), depressive symptoms (Goverover & Chiaravalloti, 2013; Hart et al., 2011;), disability (Resch et al., 2009; Williamson et al., 2013), employment (Tsaousides et al., 2009), and social participation (Kalpakjian, Lam, Toussaint, & Merbitz, 2004; McLean, Jarus, Hubley, & Jongbloed, 2013),. Limitations in employment and leisure and recreational activities, with concomitant effects on quality of life, are also common after TBI (Cicerone & Azulay, 2007; Stålnacke, 2007; Temkin, Corrigan, Dikmen, & Machamer, 2009) and may explain life satisfaction changes. Individuals with TBI are at high risk for loss of friendships and tend to engage in more passive leisure activities than individuals without TBI (Mazaux & Richer, 1998; Morton & Wehman, 1995). In a sample of adults with TBI, 40% of those who had been working prior to injury were not working or volunteering at 2–5 years post-injury (Doig, Fleming, & Tooth, 2001).
Since life satisfaction is based on an individual’s self-appraisal of life domains or roles that are relevant to that individual, restricted life roles (e.g., worker, friend, family member) may contribute differentially to overall life satisfaction. Individuals with disabilities consider life role participation to be important for adjustment to disability (Walton, Macdermid, Taylor, & Icon, 2013), but there is little research on life roles after TBI. Only one study specifically assessed life role changes after TBI and found that all participants reported at least one life role change after injury, with nearly two-thirds reporting changes in 3 or 4 life roles (out of a possible 9; Hallett, Zasler, Maurer, & Cash, 1994). Of the changes reported, 71% were a loss in participation in a life role, and the losses most frequently reported were in the roles of worker, hobbyist, and friend (Hallett et al., 1994).
In the general population, life satisfaction changes across an individual’s lifespan, perhaps as a result of changing life roles as individuals develop from young to middle to late adulthood. Life satisfaction declines slightly from early adulthood to middle age, with the lowest satisfaction reported by those in their mid-40s. This trend is followed by a gradual increase into older age (Baird, Lucas, & Donnellan, 2010; Blanchflower & Oswald, 2008), but a sharp decline is observed among those over 70 years old (Baird et al., 2010). More specifically, there is a rapid decline in life satisfaction as individuals approach death (Gerstorf et al., 2008). Cross-sectional analyses of satisfaction with participation in personally important life roles among individuals with TBI show similar trends. For example, in one small study involving chronic TBI, those 25 to 59 years old had lower satisfaction with life role participation than those who were younger than 25 or 60 and over (Juengst, 2012). Similar patterns over time are reported for relationships between age and life satisfaction among individuals with moderate to severe TBI (Corrigan et al., 2014). Therefore, life satisfaction after TBI appears to follow a similar developmental trajectory as in the general population.
It is unclear, however, whether specific subgroups of individuals with TBI experience different life satisfaction trajectories after injury. After other traumatically acquired disabilities (spinal cord injury [SCI], burns, interarticular fractures), life satisfaction trajectories in the first 5 years after injury have appeared to be stable across time (Hernandez et al., 2014). In SCI, depression trajectories (which are strongly associated with life satisfaction) demonstrated four unique subgroup memberships, including chronic high symptoms, stable low symptoms, high symptoms with recovery, and delayed symptom elevation (Bonanno, Kennedy, Galatzer-Levy, Lude, & Elfstrom, 2012). This 4-group pattern for adjustment following trauma has been supported in other SCI studies (Bonnano et al., 2012; deRoon-Cassini, Mancini, Rusch, & Bonanno, 2010) and is associated with life satisfaction (Mancini, Bonanno, & Sinan, 2014). However, depressive symptoms and life satisfaction, while strongly associated, are distinct constructs (Diener & Biswas-Diener, 2008).
Analyses of life satisfaction trajectories specifically after TBI found that, overall, life satisfaction declined over time, with those experiencing greater disability in both motor and cognitive domains undergoing the steepest decline (Resch et al., 2009; Williamson et al., 2015). Kalpinski et al. (2013) found that participation in meaningful activities mediated the relationship between disability and life satisfaction after TBI. Therefore, examining participation in specific meaningful activities (or life roles) is essential for understanding trajectories of life satisfaction after TBI.
While distinct trajectories of psychological outcomes, typically differentiated into 4 unique trajectory groups, have been found in the context of adjustment to acute stress or trauma, this has yet to be explored after TBI. Furthermore, predictors of life satisfaction trajectories after TBI may differ from other traumatic injuries (e.g. SCI), as a result of different biological mechanisms associated with injury and different cognitive, emotional, and behavioral changes unique to the TBI population. Therefore, the objectives of this study were to: 1) determine whether there are distinct life satisfaction trajectories within the first 5 years after moderate to severe TBI; 2) identify factors at 1 year post-injury that predict these life satisfaction trajectories; and 3) describe how individuals in distinct life satisfaction trajectory groups differ from one another at 1, 2, and 5 years post-injury. These objectives were evaluated using latent class growth analysis in a large sample from the TBI Model Systems National Database. We hypothesized that there would be distinct life satisfaction trajectories from 1 to 5 years post-injury that are influenced by participation in meaningful life roles at year 1 post-injury, even when controlling for race, sex, education, driving status, substance abuse, health status (re-hospitalization in the last year), age, depressive symptoms, and disability at 1 year post-injury.
Methods
Participants
Study participants were enrolled in the multicenter, longitudinal TBI Model Systems National Database, a large prospective cohort study designed to track and assess long-term outcomes after TBI, including the hypotheses tested here. Participants were age 16 years old or older, and had sustained a moderate or severe TBI, defined as at least one of the following: Glasgow Coma Scale score <13, loss of consciousness over 30 minutes, post-traumatic amnesia > 24 hours, and/or trauma-related intracranial abnormality. Informed consent was provided by either participant or proxy as necessary, and all procedures were approved by each center’s Institutional Review Board. Detailed information on data collection and inclusion criteria has been previously reported (Dijkers, Harrison-Felix, & Marwitz, 2010) (https://www.tbindsc.org/). Also, to be included in this analysis, participants were required to have complete (no missing) life satisfaction data (Satisfaction with Life Scale) collected prospectively at 1, 2, and 5 years post-injury. Demographic and other data were also collected at each time point. These included sex, race, education, driving status, substance abuse within the past year, re-hospitalization within the past year, and age. Given the hypothesis that age is not linearly related to satisfaction with life, age was treated as a categorical variable with 4 levels (16–30, 31–45, 46–59, and 60 and older) based on previous work investigating trajectories of psychiatric symptoms post-TBI (Hart et al., 2014).
Measures
Depressive Symptoms
Depressive symptoms were assessed with the Patient Health Questionnaire-9 (PHQ-9), a 9-item questionnaire that has been validated for use after TBI (Fann et al., 2005). Total scores were used as a measure of depressive symptom severity and can be interpreted as follows: no depression (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), or severe depression (≥20) (Kroenke, Spitzer, & Williams, 2001).
Disability
Motor and cognitive disability were assessed with the Functional Independence Measure’s motor (FIM-MOT) and cognitive (FIM-COG) subscales, respectively (Linacre, Heinemann, Wright, Granger, & Hamilton, 1994). The FIM is a validated measure of disability assessing level of independence (1=complete dependence to 7=complete independence) in 18 functional domains. The FIM-MOT consists of 13 mobility and self-care items, with total scores ranging from 13–91, and the FIM-COG consists of 5 cognitive and communication items, with total scores ranging from 5–35.
Life Roles
Life role participation was assessed by recoding individual items from the Participation Assessment with Recombined Tools Objective (PART-O) (Whiteneck et al., 2011), which measures frequency of engagement in various activities in the household, family, community, and wider society. Based on questions from the PART-O, participants were categorized as having low, medium, or high levels of participation in each of the following 8 life roles (number of PART-O questions): home maintainer (2), student (1), worker (1), friend (2), family member (2), leisure activities participant (4), volunteer (1), religious activities participant (1). The categorical scoring approach and the 8 specific life roles were chosen based on their inclusion on the validated Role Checklist (Oakley, Kielhofner, Barris, & Reichler, 1986) which has been used previously in TBI research (Andersson, Bedics, & Falkmer, 2011; Hallett et al., 1994). The Role Checklist includes two additional roles: caregiver and participant in organizations. These roles were not included, as the PART-O does not contain questions that address these life roles. Based on the clinical judgment of the coauthors, participation in the worker, student, and volunteer roles was categorized as full-time (high), part-time (medium), or no participation (low); otherwise life roles were categorized based on frequency distribution cutoffs (<25% percentile, 25–75% percentile, and >75% percentile, respectively). As an example, the life role of Leisure participant was categorized based on 4 PART items: Eating out at a restaurant, Playing sports/exercising outside of the home, Going to the movies, Attending sports events. All were scored based on the number of times per month a participant had engaged in the activity. For each item, those below the 25th percentile were scored as 0, those between the 25th and 75th percentiles were scored as 1, and those above the 75th percentile were scored as 2. The scores for all four items were then summed (range 0–8) and categorized into Low participation (summed score 0–1), Medium participation (summed score 2–4), and High participation (summed score 5–8). This approach allowed for comparison across life roles and has been used previously in a community-based sample of adults with TBI (Juengst, Achille, Wagner, Arenth, & Skidmore, 2014), yielding similar results.
Life Satisfaction
The Satisfaction with Life Scale (SWLS) consists of 5 items expressing satisfaction with one’s life as a whole and rated on a 7-point Likert scale (level of agreement: 1=Strongly disagree, 7=Strongly agree), yielding a total summed score ranging from 5–35 (higher scores indicate greater satisfaction) (Diener, Emmons, Larsen, & Griffin, 1985). Scores greater than 20 indicate satisfaction and scores less than 20 indicate dissatisfaction. The SWLS is a valid measure that is sensitive to changes in life satisfaction (Pavot & Diener, 1993, 2008; Corrigan, Kolakowsky-Hayner, Wright, Bellon, & Carufel, 2013) and has been used several times in the TBI population (Cicerone et al., 2007; Davis, Sherer, Sander, Bogner, Corrigan, Dijkers, et al., 2012). Participants rated their satisfaction with life at 1, 2, and 5 years post-injury.
Statistical Analysis
Only study participants with complete SWLS data for the three time points were included in the analyses. Descriptive and demographic data, including means and standard deviations or frequencies and percentages, are reported both for participants and those excluded from the analyses. Tests of statistical significance were not applied to assess differences between included and excluded participants due to the high likelihood of achieving statistical significance in a large sample even in the absence of a meaningful difference. Group-based trajectory analyses, a data-driven identification of distinct groups in a given population that have unique profiles of change over time (Nagin & Odgers, 2010), were conducted using latent class growth curve analysis (LCGA) to assess distinct trajectories of life satisfaction. Although we were interested in how trajectory groups differed across time (at 1, 2, and 5 years), due to concerns for potential error in trajectory group class assignments associated with post hoc analyses and inflated Type I error as a result of multiple comparisons, descriptive comparisons, rather than formal tests of statistical significance, are reported at 1, 2, and 5 years post-injury by life satisfaction trajectory group for significant predictors.
LCGA analyses were conducted using Mplus version 7.1 software (Muthen & Muthen, 1998–2012). LCGA is a group-based trajectory analysis approach that identifies unique subgroups of individuals within the overall sample who follow similar patterns of change over time. Using an LCGA approach, individuals within trajectory groups are relatively homogenous with respect to life satisfaction patterns, while between groups trajectories vary by intercept and slope. The optimal number of distinct trajectories was determined by evaluating multiple indices, including the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), Lo-Mendell-Rubin (LMR) test, bootstrap likelihood ratio test (BLRT), entropy values (a measure of classification accuracy), and posterior probabilities of class membership. Lower values for information criteria indices, low p-values (<.05) for the LRT and BLRT, and high values (>.70) for entropy and posterior probabilities were sought. We also considered the clinical interpretation of life satisfaction trajectories when determining number of trajectory groups. Analyses were conducted in two steps to: 1) detect distinct life satisfaction trajectory groups in an unconditional model (without covariates/predictors); and2) assess the contribution of key predictors, identified a priori, of life satisfaction trajectory group membership in a conditional model with predictors entered simultaneously. Predictor variable inclusion directly into the LCGA analysis, which accounts for error in class assignment, generally outperforms other approaches in which error in class assignment is not modeled (McIntosh, 2013).
Results
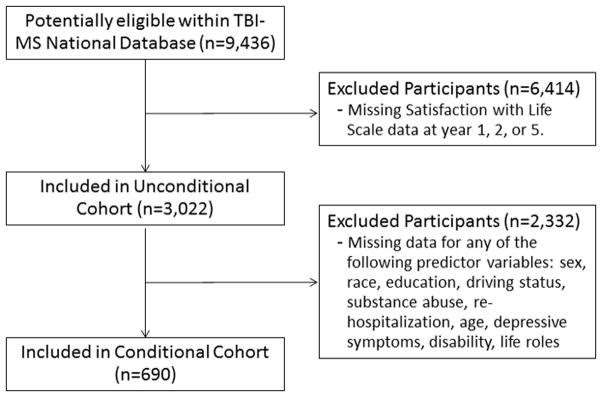
Of the original 9,436 potential TBIMS National Database participants, 6,414 had missing SWLS data at 1, 2, or 5 years post-injury and were excluded (Excluded Participants in Table 1). The remaining 3,022 had complete data and were used for identification of distinct life satisfaction trajectory groups (Unconditional Cohort in Table 1). A subset of this group (n=690) comprising all those who had complete (no missing) year 1 data for all the a priori selected potential predictors were included in the final conditional model (Conditional Trajectory Cohort in Table 2)(see Figure 1). Demographic and other data were descriptively examined for any meaningful differences (>5% or >1SD) between these groups. A higher percentage of individuals who were excluded (Excluded Participants) were racial minorities (8%), re-hospitalized within the first year post-injury (7% more), and not driving (14% more) compared to those included in the analyses (Unconditional Participants). There were no notable differences between the Unconditional Participants and the Conditional Trajectory Cohort used for the final conditional model with regard to sex, race, education, driving status, substance abuse, re-hospitalizations, age, depressive symptoms, disability, or satisfaction with life.
Table 1.
Descriptive table for unconditional analysis and excluded participants
| Variable | Unconditional Participants n=3022 | Excluded Participants n=6414* | ||
|---|---|---|---|---|
| n (%) | Total n | n (%) | Total n | |
|
| ||||
| Sex (male) | 2110 (70.1%) | 3012 | 4786 (74.7%) | 6410 |
| Race (white) | 2268 (75.7%) | 3006 | 4248 (67.0%) | 6345 |
| Driver | 1505 (50.5%) | 2982 | 1962 (36.4%) | 5397 |
| Substance abuse | 570 (19.3%) | 2949 | 903 (17.1%) | 5275 |
| Re-hospitalized in past year | 698 (23.3%) | 3001 | 1699 (30.2%) | 5628 |
| Mean (SD) | Total n | Mean (SD) | Total n | |
|
|
||||
| Age | 37.8 (16.5) | 3011 | 43.6 (19.7) | 5702 |
| Education (years) | 13.0 (2.6) | 2777 | 12.5 (2.9) | 5281 |
| Satisfaction with Life (SWLS) | 21.5 (8.2) | 3022 | 20.8 (8.2) | 3951 |
| Depressive Symptoms (PHQ9) | 5.1 (5.6) | 715 | 5.6 (5.9) | 2466 |
| Motor Disability (FIM-MOT) | 87.0 (8.6) | 2923 | 81.1(17.8) | 5347 |
| Cognitive Disability (FIM-COG) | 31.8 (3.7) | 2929 | 29.6 (6.3) | 5444 |
Note.
potentially eligible participants are defined as anyone who had a year 1 interview completed after the introduction of the Satisfaction with Life Scale on 4/1/1998. Participants were excluded if they did not have complete data for the SWLS at years 1, 2, and 5. Reasons for missing data included inability to complete a self-report assessment, missed interview, loss to follow-up, death.
Table 2.
Descriptive Data for Conditional Trajectory Cohort (n=690).
| Variable | Year 1 | Year 2 | Year 5 |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
|
| |||
| Sex (male) | 497 (72.0%) | 497 (72.0%) | 497 (72.0%) |
| Race (white) | 504 (73.0%) | 504 (73.0%) | 504 (73.0%) |
| Driver | 332 (48.1%) | 396 (57.3%) | 430 (62.3%) |
| Substance abuse | 120 (17.4%) | 135 (19.6%) | 163 (23.6%) |
| Re-hospitalized in past year | 162 (23.5%) | 105 (15.2%) | 117 (17.0%) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
|
|
|||
| Age | 38.3 (16.9) | 39.3 (16.9) | 42.2 (16.9) |
| Education (years) | 13.1 (2.4) | 13.3 (2.4) | 13.5 (2.4) |
| Satisfaction with Life (SWLS) | 22.3 (8.1) | 22.8 (8.4) | 22.8 (8.1) |
| Depressive Symptoms (PHQ9) | 4.9 (5.5) | 4.8 (5.5) | 4.9 (5.4) |
| Participation (PART-O) | 1.8 (0.6) | 1.9 (0.7) | 1.9 (0.7) |
| Motor Disability (FIM-MOT) | 87.0 (7.7) | 87.8 (6.6) | 88.0 (6.2) |
| Cognitive Disability (FIM-COG) | 31.9 (3.3) | 32.5 (2.6) | 32.6 (2.5) |
Note. Year 2: Education (n=689); PHQ9 (n=688); PART-O (n=687); FIM-MOT (n=686); FIM-COG (n=685) Year 5: Education (n=689); PART-O (n=685); PHQ9 (n=681); FIM-MOT (n=673); FIM-COG (n=670)
Figure 1.
Consort diagram for inclusion in analyses.
Note. TBI-MS=Traumatic Brain Injury Model System
Unconditional Model
Unconditional LCGA models were conducted using participants (n=3,022) with complete data across the three time points (e.g., 1, 2, and 5 years). The number of trajectory classes evaluated ranged from 1 to 7. A four-class solution was selected based on clinical interpretability of the trajectories observed, the best fit indices, including AIC, BIC, and Entropy (Table 3), and high posterior probabilities indicating accurate class assignment (range 0.86–0.95). The largest trajectory group (n=1,346; 44.5%) was characterized by high life satisfaction across all 3 time points (Stable Satisfaction). The second group (Stable Dissatisfaction) was characterized by dissatisfaction with life across all years (n=632; 20.9%). The third group (Initial Dissatisfaction Improving) included participants who were initially dissatisfied with life, but whose satisfaction improved over time (n=598; 19.8%). The smallest group (Initial Satisfaction Declining) included participants who were initially satisfied with life, but experienced declining life satisfaction (n=446; 14.8%)
Table 3.
Model Fit Indices for Determination of Number of Latent Trajectories.
| Unconditional LCGA Models
| |||||||
|---|---|---|---|---|---|---|---|
| Fit Index | 1 class | 2 classes | 3 classes | 4 classes | 5 classes | 6 classes | 7 classes |
| AIC | 60864.0 | 61011.7 | 60565.2 | 60248.3 | 60157.6 | 60057.7 | 60005.4 |
| BIC | 60912.1 | 61059.8 | 60631.4 | 60332.5 | 60259.8 | 60177.9 | 60143.7 |
| Entropy | -- | .82 | .74 | .77 | .70 | .75 | .74 |
| LMR LRT p value | -- | <.001 | <.001 | <.001 | .01 | <.01 | .08 |
| BLRT p value | -- | <.001 | <.001 | <.001 | .01 | <.01* | <.001* |
Note. AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; LMR LRT = Lo-Mendell-Rubin Likelihood Ratio test; BLRT= Bootstrapped Likelihood Ratio test;
Bootstrapped model failed to converge.
Conditional Model
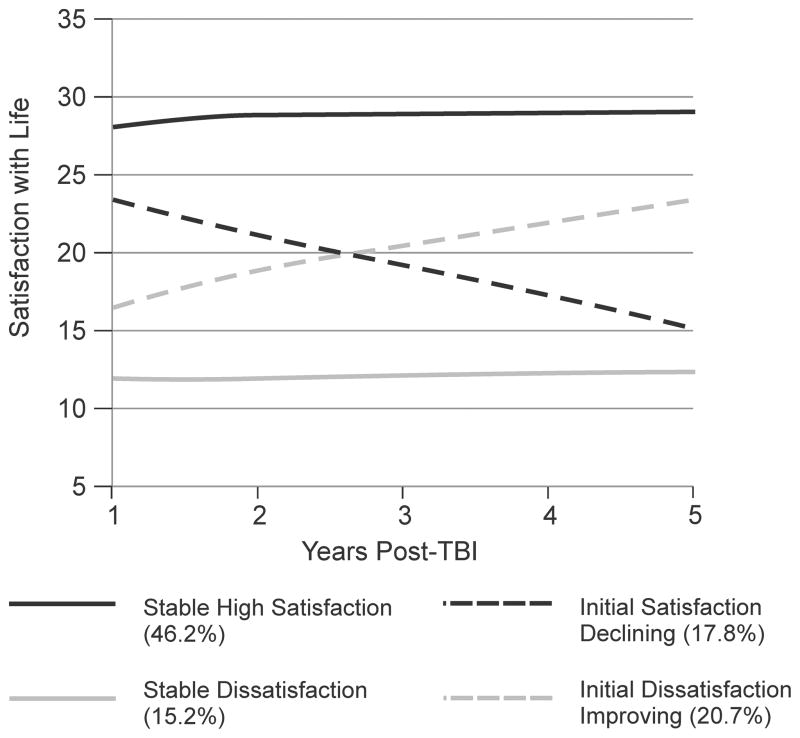
Based upon the four-class solution determined in the unconditional model, hypothesized predictor variables from 1 year post-injury were simultaneously entered into a four-class LCGA conditional model.1 Inclusion of these predictors resulted in a final sample size of 690 participants with complete data for all year 1 predictors. The final conditional model resulted in trajectory groups (see Figure 2) that were comparable to the unconditional four-class solution: Stable Satisfaction (n=319, 46.2%); Stable Dissatisfaction (n=105, 15.2%); Initial Dissatisfaction Improving (n=143, 20.7%); and Initial Satisfaction Declining (n=123, 17.9%). Odds ratios were calculated for each predictor and are presented in Tables 4a–4c. The final LCGA conditional model showed that several variables predicted life satisfaction trajectories. Participants in the 60+ age group (compared to 16–30 year group) at year 1 were more likely to belong to the Stable Satisfaction trajectory group than to the Stable Dissatisfaction or Initial Satisfaction Declining trajectory groups. These older adults were also more likely to be in the Initial Dissatisfaction Improving trajectory group, relative to the Stable Dissatisfaction trajectory group. Higher FIM-COG scores were indicative of greater likelihood of membership in the Stable Satisfaction and Initial Satisfaction Declining groups, relative to the Stable Dissatisfaction group. Higher depression scores increased the odds of membership in all dissatisfied groups (Stable Dissatisfaction; Initial Satisfaction Declining; Initial Dissatisfaction Improving) compared to the Stable Satisfaction trajectory group.
Figure 2.
Conditional Satisfaction with Life Trajectory Groups.
Note. Figure displays observed values for satisfaction with life at each time point. Standard error of the mean = <1 for all time points.
Table 4a.
Conditional Latent Growth Curve Analysis – Stable High Life Satisfaction as Referent Trajectory Group
| Stable Dissatisfaction (n = 105) | Initial Dissatisfaction, Improving (n = 143) | Initial Satisfaction, Declining (n = 123) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex | 0.77 | 0.23–2.53 | 0.98 | 0.44–2.19 | 0.78 | 0.31–2.56 |
| Race | ||||||
| Black vs White | 2.93 | 0.77–11.17 | 1.38 | 0.48–3.97 | 0.92 | 0.35–3.23 |
| Other vs White | 4.52 | 0.92–22.16 | 2.00 | 0.53–7.65 | 0.48 | 0.09–4.36 |
| Education (years) | 1.03 | 0.86–1.24 | 1.09 | 0.94–1.25 | 0.94 | 0.90–1.11 |
| Driver (Y/N) | 4.77 | 0.74–30.71 | 1.03 | 0.46–2.31 | 0.93 | 0.39–2.24 |
| Substance Abuse (Y/N) | 0.97 | 0.28–3.37 | 0.52 | 0.16–1.69 | 0.69 | 0.21–2.24 |
| Re-hospitalization in last year (Y/N) | 2.96 | 1.00–8.82 | 1.54 | 0.42–5.65 | 0.68 | 0.14–3.31 |
| Age at Injury | ||||||
| 31–45 yrs vs 16–30 yrs | 2.04 | 0.64–6.48 | 1.42 | 0.45–4.45 | 0.73 | 0.24–2.17 |
| 46–60 yrs vs 16–30 yrs | 0.95 | 0.25–3.54 | 0.92 | 0.29–2.93 | 0.71 | 0.26–1.98 |
| 61+ yrs vs 16–30 yrs | 0.06 | 0.01–0.40 | 0.90 | 0.29–2.80 | 0.28 | 0.08–0.93 |
| Depressive Symptoms | 1.29 | 1.12–1.49 | 1.23 | 1.10–1.38 | 1.14 | 1.04–1.25 |
| FIM Motor | 0.97 | 0.91–1.03 | 0.98 | 0.93–1.04 | 1.01 | 0.96–1.07 |
| FIM Cognitive | 0.76 | 0.62–0.95 | 0.92 | 0.91–1.05 | 0.91 | 0.78–1.05 |
| Life Roles | ||||||
| Home Maintainer | 0.51 | 0.21–1.19 | 0.98 | 0.40–2.40 | 0.68 | 0.30–1.67 |
| Student | 0.07 | 0.01–3.50 | 0.49 | 0.19–1.23 | 0.27 | 0.05–1.67 |
| Worker | 0.46 | 0.24–0.89 | 0.80 | 0.46–1.38 | 0.42 | 0.19–0.93 |
| Friend | 0.75 | 0.36–1.57 | 1.20 | 0.56–2.56 | 0.68 | 0.36–1.30 |
| Family Member | 1.21 | 0.48–3.09 | 0.97 | 0.43–2.17 | 1.02 | 0.35–2.95 |
| Leisure | 0.38 | 0.14–1.05 | 0.85 | 0.48–1.50 | 0.53 | 0.30–0.95 |
| Religious Participant | 0.36 | 0.19–0.68 | 0.56 | 0.36–0.87 | 0.76 | 0.52–1.10 |
Note. Comparison group = Stable High Life Satisfaction (n = 319); OR = odds ratio; CI = confidence interval; bolded values are statistically significant (p<.05).
Table 4c.
Conditional Latent Growth Curve Analysis – Initial Dissatisfaction, Improving as Referent Trajectory Group
| Stable High Satisfaction (n = 319) | Stable Dissatisfaction (n = 105) | Initial Satisfaction, Declining (n = 123) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex | 1.02 | 0.46–2.27 | 0.78 | 0.29–2.07 | 0.79 | 0.33–1.87 |
| Race | ||||||
| Black vs White | 0.73 | 0.25–2.09 | 2.12 | 0.53–8.55 | 0.67 | 0.18–2.48 |
| Other vs White | 0.50 | 0.13–1.91 | 2.26 | 0.46–11.00 | 0.24 | 0.03–2.08 |
| Education (years) | 0.92 | 0.80–1.07 | 0.95 | 0.78–1.16 | 0.87 | 0.71–1.07 |
| Driver (Y/N) | 0.97 | 0.43–2.19 | 4.64 | 0.75–28.84 | 0.91 | 0.25–3.29 |
| Substance Abuse (Y/N) | 1.92 | 0.59–6.24 | 1.86 | 0.51–6.74 | 1.32 | 0.27–6.40 |
| Re-hospitalization in last year (Y/N) | 0.65 | 0.18–2.38 | 1.93 | 0.69–5.35 | 0.44 | 0.03–5.51 |
| Age at Injury | ||||||
| 31–45 yrs vs 16–30 yrs | 0.71 | 0.23–2.21 | 1.43 | 0.51–4.04 | 0.51 | 0.13–2.04 |
| 46–60 yrs vs 16–30 yrs | 1.09 | 0.34–3.47 | 1.03 | 0.28–3.93 | 0.78 | 0.20–3.04 |
| 61+ yrs vs 16–30 yrs | 1.11 | 0.36–3.43 | 0.06 | 0.01–0.42 | 0.31 | 0.07–1.29 |
| Depression Symptoms | 0.81 | 0.73–0.91 | 1.05 | 0.94–1.16 | 0.93 | 0.93–1.03 |
| FIM Motor | 1.02 | 0.96–1.08 | 0.98 | 0.94–1.03 | 1.03 | 0.97–1.10 |
| FIM Cognitive | 1.09 | 0.95–1.24 | 0.83 | 0.68–1.01 | 0.99 | 0.92–1.18 |
| Life Roles | ||||||
| Home Maintainer | 1.02 | 0.42–2.52 | 0.52 | 0.26–1.03 | 0.69 | 0.28–1.70 |
| Student | 2.05 | 0.82–5.15 | 0.14 | 0.00–6.15 | 0.56 | 0.10–3.012 |
| Worker | 1.25 | 0.73–2.16 | 0.58 | 0.31–1.06 | 0.53 | 0.26–1.09 |
| Friend | 0.93 | 0.39–1.78 | 0.62 | 0.27–1.42 | 0.57 | 0.18–1.79 |
| Family Member | 1.03 | 0.46–2.31 | 1.25 | 0.46–3.42 | 1.05 | 0.25–4.41 |
| Leisure | 1.18 | 0.67–2.08 | 0.45 | 0.16–1.23 | 0.63 | 0.30–1.29 |
| Religious Participant | 1.78 | 1.15–2.76 | 0.64 | 0.35–1.17 | 1.34 | 0.83–2.18 |
Note. Comparison group = Initial Dissatisfaction, Improving (n = 143); OR = odds ratio; CI = confidence interval; bolded values are statistically significant (p<.05).
Three life roles discriminated between trajectory group memberships. The Stable Satisfaction group was more likely to participate as workers than the Stable Dissatisfaction or Initial Satisfaction Declining groups. The Initial Satisfaction Declining group was less likely to be involved in leisure activities than the Stable Satisfaction group. Membership in either dissatisfaction trajectory group (Stable Dissatisfaction; Initial Dissatisfaction Improving) was associated with lower religious participation relative to the Stable Satisfaction group, while those in the Initial Satisfaction Declining group were more likely to be involved in religious activities than Stable Dissatisfaction group members.
Life Satisfaction Trajectory Group Differences Over Time: Descriptive Characterization
Descriptive characterization of age group, life satisfaction, depressive symptoms, cognitive disability, and participation as a Worker, Leisure Participant, and Religious Participant are presented in Table 5. Overall, the Stable High Satisfaction trajectory group had the highest percentage of participants 16–30 years old and of participants reporting high levels of participation across the relevant life roles (i.e., worker, leisure participant, religious participant) at all years. These participants also reported the lowest cognitive disability and depressive symptoms at all years. Conversely, the Stable Dissatisfaction group had the lowest percentage of participants reporting high levels of participation across roles and reported the highest depressive symptoms and greatest cognitive disability at all years. This group also had the highest percentage of participants 31–59 years old. Those whose satisfaction declined over time reported lower participation as workers and in leisure activities and had a lower percentage of participants 60 and older than those whose satisfaction improved over time. Finally, the Initial Dissatisfaction Improving group started with the second lowest life satisfaction and second highest depressive symptom burden (second only to the Stable Dissatisfaction group), but had improved by year 5 to have higher satisfaction and lower depressive symptoms than the Initial Satisfaction Declining group. The Initial Dissatisfaction Improving group also had the second highest percentages in participation across all time points, suggesting participation may be important for improving life satisfaction over time.
Table 5.
Descriptive characterization of life satisfaction and significant year 1 predictors of life satisfaction trajectories at 1, 2, and 5 years post-injury by trajectory group
| Stable High Satisfaction n=319 | Initial Satisfaction Declining n=123 | Initial Dissatisfaction, Improving n=143 | Stable Dissatisfaction n=105 | |
|---|---|---|---|---|
| n(%) | n(%) | n(%) | n(%) | |
| Age at Injury | ||||
| 16–30 years | 168 (52.7) | 55 (44.7) | 57 (39.9) | 35 (33.3) |
| 31–45 years | 52 (16.3) | 26 (21.1) | 36 (25.2) | 40 (38.1) |
| 46–59 years | 53 (16.6) | 31 (25.2) | 25 (17.5) | 29 (27.6) |
| 60+ years | 46 (14.4) | 11 (8.9) | 25 (17.5) | 1 (1.0) |
| Life Roles (High Participation) | ||||
| Worker | ||||
| Year 1 | 110 (34.5) | 9 (7.3) | 32 (22.4) | 8 (7.6) |
| Year 2 | 108 (34.0) | 14 (11.4) | 31 (21.7) | 7 (6.7) |
| Year 5 | 140 (44.0) | 18 (14.6) | 37 (25.9) | 6 (5.7) |
| Leisure Participant | ||||
| Year 1 | 161 (50.5) | 25 (20.3) | 53 (37.1) | 13 (12.4) |
| Year 2 | 147 (46.1) | 33 (26.8) | 43 (30.1) | 17 (16.2) |
| Year 5 | 155 (48.6) | 30 (24.4) | 41 (28.9) | 17 (16.3) |
| Religious Participant | ||||
| Year 1 | 132 (41.4) | 44 (35.8) | 35 (24.5) | 13 (12.4) |
| Year 2 | 135 (42.3) | 37 (30.1) | 41 (28.7) | 23 (21.9) |
| Year 5 | 132 (41.4) | 31 (25.2) | 41 (28.7) | 16 (15.4) |
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |
|
|
||||
| Life Satisfaction (SWLS) | ||||
| Year 1 | 28.0 (5.0) | 23.4 (5.4) | 16.4 (5.6) | 11.9 (4.9) |
| Year 2 | 28.8 (4.7) | 21.1 (7.3) | 18.9 (6.3) | 11.9 (5.7) |
| Year 5 | 29.0 (4.1) | 15.3 (4.8) | 23.2 (4.8) | 12.3 (4.6) |
| Depressive Symptoms (PHQ-9) | ||||
| Year 1 | 2.5 (3.2) | 5.3 (4.7) | 6.5 (5.8) | 9.9 (7.0) |
| Year 2 | 2.5 (3.2) | 5.7 (6.0) | 5.9 (5.5) | 9.5 (6.5) |
| Year 5 | 2.7 (3.5) | 6.7 (6.1) | 5.5 (5.2) | 9.1 (6.5) |
| Cognitive Disability (FIM-COG) | ||||
| Year 1 | 33.2 (2.1) | 31.4 (3.5) | 31.8 (2.8) | 29.0 (4.3) |
| Year 2 | 33.5 (1.9) | 31.9 (3.1) | 32.3 (2.2) | 30.4 (2.9) |
| Year 5 | 33.4 (2.0) | 32.0 (2.5) | 32.7 (2.1) | 31.0 (3.0) |
Note. Stable High Satisfaction group: n=318 for Worker life roles and Depressive Symptoms at years 2 and 5, n=317 and n=309 for Cognitive Disability at years 2 and 5, respectively; Initial Satisfaction Declining group: n=121 for Depressive Symptoms at year 5, n=122 and n=120 for Cognitive Disability at years 2 and 5, respectively; Initial Dissatisfaction Improving group: n=142 for Leisure Participant life roles and Depressive Symptoms at 5 years, n=142 and n=139 for Cognitive Disability at years 2 and 5, respectively; Stable Dissatisfaction group: n=104 for all life roles variables at year 5, n=104 for Cognitive Disability and Depressive Symptoms at 2 years, n=102 for Cognitive Disability at 5 years, n=100 for Depressive Symptoms at 5 years.
Discussion
Low life satisfaction is a well-documented consequence of TBI (Cicerone & Azulay, 2007; Corrigan et al., 2001; Mailhan et al., 2005) and is associated with greater functional impact of injury (Resch et al., 2009; Stålnacke, 2007; Williamson et al., 2015). Life satisfaction can decline immediately following a life-altering event (Diener, 2012), but evidence suggests that most individuals’ level of satisfaction improves over time (Corrigan, Smith-Knapp, & Granger, 1998; Diener, 2012; Headey & Wearing, 1992). This adaptation, however, can take many years and is not always a return to pre-injury baseline (Diener, 2012). Previous studies in life satisfaction after TBI have demonstrated contradictory results with regard to return-to-baseline (Cicerone & Azulay, 2007; Corrigan et al., 2001; Mailhan et al., 2005). However, prior studies generally present sample averages and do not account for the possible existence of distinct subgroups for which adaptation may not occur or may not be complete and for which life satisfaction may remain low or even decline further over time.
Findings from this study revealed four distinct life satisfaction trajectories in the first five years after TBI, consistent with trajectories of depressive symptoms and adjustment identified in other traumatic conditions (Bonanno et al., 2012; Mancini et al., 2014). The Stable Dissatisfaction group had average scores across all three time points (range 12–14) in the bounds of dissatisfaction (Diener et al., 1985) and lower than average scores reported in previous studies of satisfaction with life after moderate to severe TBI (range 19.1 to 20.8) (Dijkers, 2004). This group also demonstrated the lowest life role participation and highest depressive symptom burden at every time point. The Initial Satisfaction Declining group’s SWLS scores fell into the range of dissatisfied by year 5; these individuals (~18% of the total) demonstrated lower participation in life roles over time than those with high or improving satisfaction. Ongoing follow-up beyond the first year post-injury to address life roles and depressive symptoms could be helpful to prevent or even reverse decline in satisfaction among these individuals.
As hypothesized, the life satisfaction trajectory groups differed by age. In the general population, those in middle age groups are more likely to have low life satisfaction compared to younger and older adults, (Baird et al., 2010) a pattern which has also been identified among those with TBI (Corrigan et al., 2014). We found that those over 60, when compared with those under 30, were most likely to have high satisfaction and were more likely to have improving satisfaction, even if it was initially low. Several studies have investigated the relationship between age and life satisfaction, with many looking to life roles and other factors as possible mediators (Chmiel, Brunner, Martin, & Schalke, 2012; Darbonne, Uchino, & Ong, 2013; Frijters & Beatton, 2012). Compared to older adults, middle aged adults may perceive life roles as both more important to their overall satisfaction and more limited by the effects of a chronic disease (Gignac et al., 2013). Therefore, it may be that the relatively lower life satisfaction in middle adulthood is explained more by life role participation than by age per se; this could explain why being in the middle age group was not a significant predictor of life satisfaction trajectory in our study, as we also included life role participation in our models. Still, a larger percentage of those 31–45 years old were in the Stable Dissatisfaction group than in any other trajectory group. The relatively higher life satisfaction observed in older adults may be, in part, due to natural changes in life roles that occur with aging, such as retirement, greater religious participation, having a smaller and closer circle of friends, and possible self-perceived leisure activity enhancements
Losses of life roles, particularly as worker, hobbyist, and friend, are common after TBI (Dijkers, 2004; Hallett et al., 1994). We found that participation as a worker, leisure activities participant, and religious participant significantly predicted life satisfaction trajectory group, with lower participation in these life roles generally being associated with dissatisfaction. Those with higher participation as workers were more likely to demonstrate high stable satisfaction compared to declining or low satisfaction, supporting the need for ongoing vocational rehabilitation services to improve employment outcomes and prevent loss of the worker life role. Those whose satisfaction declined over time demonstrated significantly lower participation in leisure roles than those whose satisfaction remained high. Pilot studies suggest that leisure interventions (e.g., leisure activities in the context of rehabilitation or home-based leisure programs), which could be implemented through community-based programs, support groups, or by families, may improve quality of life and depressive symptoms for individuals with acquired brain injuries (Dorstyn, Roberts, Kneebone, Kennedy, & Lieu, 2014; Mitchell, Veitch, & Passey, 2013). Finally, religious participation was related to life satisfaction in the first year post-injury, as it differentiated those who had higher satisfaction at year 1 from those who had lower satisfaction. Religious participation in the general population increases as individuals age and is often associated with life satisfaction among older adults (Krause, 2003; Bradshaw, Ellison, Fang, & Mueller, 2014), and may partially explain the greater likelihood of high stable satisfaction among those over 60 years compared to those under 30 in our study. Engagement in these life roles in the first year post-injury may improve initial dissatisfaction or prevent satisfaction decline over time. Beyond management of health and disability, individuals need to be returning to or developing new meaningful life roles after TBI.
Depressive symptoms have been associated previously with life satisfaction after TBI and should continue to be monitored and addressed across recovery (Underhill, Lobello, Stroud, Terry, Devivo, & Fine, 2003). We found that depressive symptoms at year 1 predicted life satisfaction trajectory group membership and remained relatively stable within each trajectory group over time, with a slight trend towards increasing in the Declining satisfaction group and decreasing in the Improving satisfaction group. Among those with Stable Satisfaction, depressive symptoms were minimal and remained so at every time point, whereas those with Stable Dissatisfaction consistently had mild to moderate depressive symptoms. Effectively treating depression may be beneficial to life satisfaction and depressive symptomatology should be monitored regularly post-TBI. One effective approach to treating depression in the general population, related to participation in life roles, is behavior activation to engage individuals in the process of resuming enjoyable and meaningful activities. Preliminary evidence suggests that behavioral activation may be efficacious for treating depression after TBI (Fann et al., 2014). Additionally, there is evidence to suggest that poor psychosocial functioning – such as loss of life roles – precedes depression after TBI (Pagulayan, Hoffman, Temkin, Machamer, & Dikmen, 2008; Schönberger, Ponsford, Gould, & Johnston, 2011), providing additional support that addressing life role participation may improve depressive symptoms and, as a result, life satisfaction.
While previous research suggests that both physical and cognitive disability are linked to life satisfaction after traumatic injuries (Hernandez et al., 2014; Huebner et al., 2003; Resch et al., 2009; Williamson et al., 2013), the present study found that only cognitive disability significantly predicted life satisfaction trajectories. Inspection over time across trajectory groups for cognitive disability revealed mostly small differences below the minimal clinically important difference threshold (where a meaningful difference is ≥3 points for FIM-COG; Beninato, Gill-Body, Salles, Stark, Black-Schaffer, & Stein, 2006). The greatest disability was reported in the Stable Dissatisfaction group and the least disability in the Stable Satisfaction group across all time points. It may be that life role participation captures aspects of disability not measured by the FIM (Dijkers, 1997), and, in combination with depressive symptoms, may be more important to life satisfaction after TBI than motor or even cognitive disability.
Notably, demographic factors such as sex, race, and education, and other factors, including driving status, substance abuse, and re-hospitalization, were not significantly associated with life satisfaction trajectories. Unlike previous studies that identified predictors of life satisfaction at individual time points, this study examined temporal life satisfaction trajectories, which may explain why these previously associated factors were not found to be predictors of life satisfaction in the present study.
Finally, there were multiple life roles that were not associated with life satisfaction trajectories after TBI, including those of home maintainer, student, family member, volunteer, and friend. Previous TBI literature identified worker, friend, and hobbyist as the roles in which individuals reported the greatest loss (Hallett et al., 1994), supporting findings from this study. Other life roles may not have changed from before to after injury, may have held less personal relevance to individuals – and therefore did not influence satisfaction – or may have been less important to an individual’s satisfaction for other reasons. Data were not available for pre-injury life role participation to assess TBI-induced life role change or satisfaction with life role participation, which may provide more meaningful links to life satisfaction than frequency of participation alone. Notably, this study highlights the need to look at specific life roles, not just global measures of community participation, with regard to long-term psychosocial outcomes after TBI, and for education and other resources targeting life role participation after injury.
Study Limitations
This sample consisted of participants with complete (no missing) data, representing a relatively small percentage of the total TBI-MS National Database sample. Therefore, while the results are robust for the population represented, generalizations to the broader population with TBI should be made with caution, for the following reasons. A higher percentage of excluded participants were not driving and had been re-hospitalized during their first year post-injury. These individuals may have had more medical complications, less support, or fewer resources than those with complete data, or died prior to the year 5 follow-up. Additionally, life satisfaction was measured through self-report and could not be completed via proxy. Those excluded may, therefore, include those with greater functional deficits and less support, representing those who have the greatest need for intervention. Similar to most studies in TBI, numerous premorbid characteristics were also unknown and may be important with regard to life satisfaction (Davis et al., 2012). These premorbid characteristics include life satisfaction, depressive symptoms or substance abuse, and disability or participation in life roles. Additionally, no data are available as to the personal importance of each of these life roles, which may be particularly meaningful with regard to life satisfaction. Lastly, because participation in life roles data were derived from the PART-O, measurement of participation in certain roles may have been less precise, which may explain the failure to find an association between certain life roles and life satisfaction trajectory.
Future Directions
This study is among the first to demonstrate the importance of life roles with regard to life satisfaction after TBI. The known loss of life roles and prevalence of depression after TBI put individuals with TBI at high risk for low or declining satisfaction. The importance of age and its relationship to life role participation requires further exploration. Future studies should consider examining participation in specific life roles (e.g. worker, leisure participant), personal importance of specific life roles, and change in life roles from pre- to post-injury to identify relevant foci for community-based or vocational rehabilitation programs. In addition, development of education and intervention programs to address these issues may be critical to life satisfaction after brain injury, both initially after injury and once individuals have returned to the community. These data highlight the importance of addressing depressive symptoms and participation early after TBI, as these factors at one year post-injury may have long-term implications for the trajectory of life satisfaction over time. There is clearly a need for ongoing community outreach and infrastructure to support individuals with TBI who may experience changing life roles and decreasing depressive symptnoms and satisfaction after they have been discharged from traditional rehabilitation services.
Table 4b.
Conditional Latent Growth Curve Analysis – Stable Dissatisfaction as Referent Trajectory Group
| Stable High Satisfaction (n = 319) | Initial Dissatisfaction, Improving (n = 143) | Initial Satisfaction, Declining (n = 123) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex | 1.31 | 0.40–4.31 | 1.28 | 0.48–3.40 | 1.01 | 0.39–2.61 |
| Race | ||||||
| Black vs White | 0.34 | 0.09–1.30 | 0.47 | 0.12–1.90 | 0.31 | 0.09–1.05 |
| Other vs White | 0.22 | 0.05–1.09 | 0.44 | 0.09–2.16 | 0.11 | 0.02–0.74 |
| Education (years) | 0.97 | 0.80–1.16 | 1.05 | 0.86–1.28 | 0.91 | 0.76–1.09 |
| Driver (Y/N) | 0.21 | 0.03–1.35 | 0.22 | 0.04–1.33 | 0.20 | 0.03–1.52 |
| Substance Abuse (Y/N) | 1.03 | 0.30–3.61 | 0.54 | 0.15–1.95 | 0.71 | 0.18–2.83 |
| Re-hospitalization in last year (Y/N) | 0.34 | 0.11–1.00 | 0.52 | 0.19–1.44 | 0.23 | 0.03–1.69 |
| Age at Injury | ||||||
| 31–45 yrs vs 16–30 yrs | 0.49 | 0.15–1.57 | 0.70 | 0.25–1.96 | 0.36 | 0.11–1.22 |
| 46–60 yrs vs 16–30 yrs | 1.06 | 0.28–3.94 | 0.97 | 0.26–3.59 | 0.75 | 0.22–2.53 |
| 61+ yrs vs 16–30 yrs | 17.42 | 2.50–121.50 | 15.71 | 2.40–102.70 | 4.83 | 0.91–25.47 |
| Depression Symptoms | 0.78 | 0.67–0.89 | 0.96 | 0.86–1.06 | 0.88 | 0.79–0.99 |
| FIM Motor | 1.04 | 0.97–1.10 | 1.02 | 0.97–1.07 | 1.05 | 0.99–1.12 |
| FIM Cognitive | 1.31 | 1.06–1.62 | 1.21 | 0.99–1.47 | 1.19 | 1.01–1.40 |
| Life Roles | ||||||
| Home Maintainer | 1.98 | 0.84–4.68 | 1.94 | 0.97–3.85 | 1.34 | 0.67–2.69 |
| Student | 14.50 | 0.29–735.90 | 7.07 | 0.16–307.30 | 3.97 | 0.04–387.60 |
| Worker | 2.17 | 1.13–4.17 | 1.73 | 0.94–3.19 | 0.92 | 0.37–2.25 |
| Friend | 1.34 | 0.64–2.80 | 1.60 | 0.70–3.66 | 0.91 | 0.36–2.32 |
| Family Member | 0.93 | 0.32–2.10 | 0.80 | 0.29–2.18 | 0.84 | 0.28–2.53 |
| Leisure | 2.62 | 0.94–7.31 | 2.23 | 0.82–6.12 | 1.40 | 0.56–3.46 |
| Religious Participant | 2.77 | 1.46–5.26 | 1.56 | 0.86–2.84 | 2.09 | 1.14–3.84 |
Note. Comparison group = Stable Dissatisfaction (n = 105); OR = odds ratio; CI = confidence interval; bolded values are statistically significant (p<.05).
Impact.
Although low life satisfaction is well documented after TBI, trajectories of life satisfaction over time found in other disability populations have not been well-documented after TBI. Furthermore, this study is the first to explore the effects of life role participation on life satisfaction trajectories after injury.
The current paper adds to the existing literature by showing a link between depression, life role participation, and life satisfaction up to 5 years post TBI and establishment of a predictive model for these trajectories using a large multicenter sample.
These findings have multiple implications for clinical practice. Practitioners will better understand life satisfaction changes and the importance of addressing participation in life roles when working to improve life satisfaction after TBI. This may lead to improved intervention efforts that promote life satisfaction by focusing on participation in valued life roles at different time points over the course of recovery from TBI.
Acknowledgments
This work was supported by the National Institute on Disability and Rehabilitation Research through Traumatic Brain Injury Model System (TBIMS) grant numbers H133A120887, H133A120084, H133A070029, H133A120037, H133A120026, H133A120096, H133A120085 and partly supported by the National Institute on Aging (5T32AG027677).
Footnotes
The Conditional model was fit using the three-step estimator, with confirmation that inferences were unchanged.
Bibliography
- Andersson EE, Bedics BK, Falkmer T. Mild traumatic brain injuries: a 10-year follow-up. Journal of Rehabilitation Medicine: Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2011;43(4):323–329. doi: 10.2340/16501977-0666. [DOI] [PubMed] [Google Scholar]
- Baird BM, Lucas RE, Donnellan MB. Life Satisfaction Across the Lifespan: Findings from Two Nationally Representative Panel Studies. Social Indicators Research. 2010;99(2):183–203. doi: 10.1007/s11205-010-9584-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beninato J, Gill-Body KM, Salles S, Stark PC, Black-Schaffer RM, Stein J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Archives of Physical Medicine & Rehabilitation. 2006;87:32–39. doi: 10.1016/j.apmr.2005.08.130. [DOI] [PubMed] [Google Scholar]
- Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Social Science & Medicine (1982) 2008;66(8):1733–1749. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Kennedy P, Galatzer-Levy IR, Lude P, Elfstrom ML. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabilitation Psychology. 2012;57:236–47. doi: 10.1037/a0029256. [DOI] [PubMed] [Google Scholar]
- Bradshaw M, Ellison CG, Fang Q, Muller C. Listening to religious music and mental health in later life. The Gerontologist. 2014 doi: 10.1093/geront/gnu020. [DOI] [PubMed] [Google Scholar]
- Chmiel M, Brunner M, Martin R, Schalke D. Revisiting the Structure of Subjective Well-Being in Middle-Aged Adults. Social Indicators Research. 2012;106(1):109– 116. doi: 10.1007/s11205-011-9796-7. [DOI] [Google Scholar]
- Cicerone KD, Azulay J. Perceived self-efficacy and life satisfaction after traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2007;22(5):257–266. doi: 10.1097/01.HTR.0000290970.56130.81. [DOI] [PubMed] [Google Scholar]
- Corrigan J, Bogner JA, Mysiw WJ, Clinchot D, Fugate L. Life satisfaction after traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2001;16(6):543–555. doi: 10.1097/00001199-200112000-00003. [DOI] [PubMed] [Google Scholar]
- Corrigan JD, Cuthbert JP, Harrison-Felix C, Whiteneck GG, Bell JM, Miller AC, Pretz CR. US Population Estimates of Health and Social Outcomes 5 Years After Rehabilitation for Traumatic Brain Injury. The Journal of Head Trauma Rehabilitation. 2014 doi: 10.1097/HTR.0000000000000020. [DOI] [PubMed] [Google Scholar]
- Corrigan JD, Kolakowsy S, Wrigth J, Bellon K, Carufel P. The satisfaction with life scale. Journal of Head Trauma Rehabilitation. 2013;28:489–491. doi: 10.1097/HTR.0000000000000004. [DOI] [PubMed] [Google Scholar]
- Corrigan JD, Smith-Knapp K, Granger CV. Outcomes in the first 5 years after traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 1998;79(3):298–305. doi: 10.1016/S0003-9993(98)90010-7. [DOI] [PubMed] [Google Scholar]
- Darbonne A, Uchino BN, Ong AD. What Mediates Links Between Age and Well-being? A Test of Social Support and Interpersonal Conflict as Potential Interpersonal Pathways. Journal of Happiness Studies. 2013;14(3):951–963. doi: 10.1007/s10902-012-9363-1. [DOI] [Google Scholar]
- Davis LC, Sherer M, Sander AM, Bogner JA, Corrigan JD, Dijkers MP, et al. Preinjury predictors of life satisfaction at 1 year after traumatic brain injury. Archives of Physical Medicine & Rehabilitation. 2012;93:1324–1330. doi: 10.1016/j.apmr.2012.02.036. [DOI] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno GA. Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabilitation Psychology. 2010;55:1–11. doi: 10.1037/a0018601. [DOI] [PubMed] [Google Scholar]
- Diener E. New findings and future directions for subjective well-being research. American Psychologist. 2012;67(8):590–597. doi: 10.1037/a0029541. [DOI] [PubMed] [Google Scholar]
- Diener E, Biswas-Diener R. Happiness: Unlocking the Mysteries of Psychological Wealth. 1. Malden, MA; Oxford: Wiley-Blackwell; 2008. [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. Journal of Personality Assessment. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Diener E, Suh ME. Subjective well-being and age: An international analysis. In: Schaie KW, Lawton MP, editors. Annual review of gerontology and geriatrics, Vol. 17: Focus on emotion and adult development. New York, NY, US: Springer Publishing Co; 1998. pp. 304–324. [Google Scholar]
- Dijkers M. Quality of life after spinal cord injury: a meta-analysis of the effects of disablement components. Spinal Cord. 1997;35(12):829–840. doi: 10.1038/sj.sc.3100571. [DOI] [PubMed] [Google Scholar]
- Dijkers MP. Quality of life after traumatic brain injury: a review of research approaches and findings. Archives of Physical Medicine and Rehabilitation. 2004;85(Supplement 2):21–35. doi: 10.1016/j.apmr.2003.08.119. [DOI] [PubMed] [Google Scholar]
- Dijkers MP, Harrison-Felix C, Marwitz JH. The Traumatic Brain Injury Model Systems: History and Contributions to Clinical Service and Research. Journal of Head Trauma Rehabilitation Gedenkschrift Honoring Mitchell Rosenthal. 2010;25(2):81–91. doi: 10.1097/HTR.0b013e3181cd3528. [DOI] [PubMed] [Google Scholar]
- Doig E, Fleming J, Leigh T. Patterns of community integration 2–5 years post-discharge from brain injury rehabilitation. Brain Injury. 2001;15(9):747–762. doi: 10.1080/02699050119845. [DOI] [PubMed] [Google Scholar]
- Dorstyn D, Roberts R, Kneebone I, Kennedy P, Lieu C. Systematic review of leisure therapy and its effectiveness in managing functional outcomes in stroke rehabilitation. Topics in Stroke Rehabilitation. 2014;21(1):40–51. doi: 10.1310/tsr2101-40. [DOI] [PubMed] [Google Scholar]
- Fann JR, Bombardier CH, Dikmen S, Esselman P, Warms CA, Pelzer E, Temkin N. Validity of the Patient Health Questionnaire-9 in assessing depression following traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2005;20(6):501–511. doi: 10.1097/00001199-200511000-00003. [DOI] [PubMed] [Google Scholar]
- Fann JR, Bombardier CH, Vannoy S, Dyer J, Ludman E, Dikmen S, Temkin N. Telephone and In-Person Cognitive Behavioral Therapy for Major Depression after Traumatic Brain Injury: A Randomized Controlled Trial. Journal of Neurotrauma. 2014 doi: 10.1089/neu.2014.3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frijters P, Beatton T. The mystery of the U-shaped relationship between happiness and age. Journal of Economic Behavior & Organization. 2012;82(2–3):525–542. doi: 10.1016/j.jebo.2012.03.008. [DOI] [Google Scholar]
- Fuhrer MJ. Subjectifying quality of life as a medical rehabilitation outcome. Disability and Rehabilitation. 2000;22(11):481–489. doi: 10.1080/096382800413961. [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Ram N, Estabrook R, Schupp J, Wagner GG, Lindenberger U. Life satisfaction shows terminal decline in old age: longitudinal evidence from the German Socio-Economic Panel Study (SOEP) Developmental Psychology. 2008;44(4):1148–1159. doi: 10.1037/0012-1649.44.4.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gignac MAM, Backman CL, Davis AM, Lacaille D, Cao X, Badley EM. Social role participation and the life course in healthy adults and individuals with osteoarthritis: are we overlooking the impact on the middle-aged? Social Science & Medicine (1982) 2013;81:87–93. doi: 10.1016/j.socscimed.2012.12.013. [DOI] [PubMed] [Google Scholar]
- Goverover Y, Chiaravalloti N. The impact of self-awareness and depression on subjective reports of memory, quality-of-life and satisfaction with life following TBI. Brain Injury. 2013 doi: 10.3109/02699052.2013.860474. [DOI] [PubMed] [Google Scholar]
- Grauwmeijer E, Heijenbrok-Kal M, Ribbers G. Health-related quality of life 3 years after moderate to severe traumatic brain injury: a prospective cohort study. Archives of Physical Medicine and Rehabilitation. 2014 doi: 10.1016/j.apmr.2014.02.002. [DOI] [PubMed] [Google Scholar]
- Hallett JD, Zasler ND, Maurer P, Cash S. Role change after traumatic brain injury in adults. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association. 1994;48(3):241–246. doi: 10.5014/ajot.48.3.241. [DOI] [PubMed] [Google Scholar]
- Hart T, Benn EKT, Bagiella E, Arenth P, Dikmen S, Hesdorffer DC, Zafonte R. Early trajectory of psychiatric symptoms after traumatic brain injury: relationship to patient and injury characteristics. Journal of Neurotrauma. 2014;31(7):610–617. doi: 10.1089/neu.2013.3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart T, Brenner L, Clark AN, Bogner JA, Novack TA, Chervoneva I, Arango-Lasprilla JC. Major and minor depression after traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2011;92(8):1211–1219. doi: 10.1016/j.apmr.2011.03.005. [DOI] [PubMed] [Google Scholar]
- Headey B, Wearing A. Understanding Happiness: A Theory of Subjective Well-being. Longman Cheshire; 1992. [Google Scholar]
- Hernandez CL, Elliott TR, Berry JW, Underhill AT, Fine PR, Lai MH. Trajectories of life satisfaction five years after medical discharge for traumatically acquired disability. Rehabilitation Psychology. 2014;59:183–92. doi: 10.1037/a0035887. [DOI] [PubMed] [Google Scholar]
- Juengst SB. Self Awareness and Community Integration after Traumatic Brain Injury. University of Pittsburgh; 2012. Sep 20, [Google Scholar]
- Juengst SB, Achille SC, Wagner A, Arenth PM, Skidmore E. Examining Life Roles After Traumatic Brain Injury Using the Participation Assessment With Recombined Tools Objective. Archives of Physical Medicine and Rehabilitation. 2014;95(10):e71. doi: 10.1016/j.apmr.2014.07.228. [DOI] [Google Scholar]
- Kalpakjian CZ, Lam CS, Toussaint LL, Merbitz NKH. Describing quality of life and psychosocial outcomes after traumatic brain injury. American Journal of Physical Medicine & Rehabilitation / Association of Academic Physiatrists. 2004;83(4):255–265. doi: 10.1097/01.phm.0000118033.07952.8c. [DOI] [PubMed] [Google Scholar]
- Kalpinski RJ, Williamson MLC, Elliott TR, Berry JW, Underhill AT, Fine PR. Modeling the prospective relationships of impairment, injury severity, and participation to quality of life following traumatic brain injury. BioMed Research International. 2013;2013:102570. doi: 10.1155/2013/102570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N. Religious meaning and subjective well-being in late life. Journal of Gerontology, Series B, Psychological Sciences and Social Sciences. 2003;58:S160–170. doi: 10.1093/geronb/58.3.s160. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Archives of Physical Medicine & Rehabilitation. 1994;75:127–132. [PubMed] [Google Scholar]
- Mailhan L, Azouvi P, Dazord A. Life satisfaction and disability after severe traumatic brain injury. Brain Injury. 2005;19(4):227–238. doi: 10.1080/02699050410001720149. [DOI] [PubMed] [Google Scholar]
- Mancini AD, Bonanno GA, Sinan B. A brief retrospective method for identifying longitudinal trajectories of adjustment following acute stress. Assessment. 2014 doi: 10.1177/1073191114550816. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Mazaux JM, Richer E. Rehabilitation after traumatic brain injury in adults. Disability and Rehabilitation. 1998;20(12):435–447. doi: 10.3109/09638289809166108. [DOI] [PubMed] [Google Scholar]
- McIntosh CN. Pitfalls in subgroup analysis based on growth mixture models: a commentary on van Leeuwen et al. (2012) Quality of Life Research. 2013;22(9):2625–2629. doi: 10.1007/s11136-013-0385-x. [DOI] [PubMed] [Google Scholar]
- McLean AM, Jarus T, Hubley AM, Jongbloed L. Associations between social participation and subjective quality of life for adults with moderate to severe traumatic brain injury. Disability and Rehabilitation. 2013 doi: 10.3109/09638288.2013.834986. [DOI] [PubMed] [Google Scholar]
- Mitchell EJ, Veitch C, Passey M. Efficacy of leisure intervention groups in rehabilitation of people with an acquired brain injury. Disability and Rehabilitation. 2013 doi: 10.3109/09638288.2013.845259. [DOI] [PubMed] [Google Scholar]
- Morton MV, Wehman P. Psychosocial and emotional sequelae of individuals with traumatic brain injury: a literature review and recommendations. Brain Injury: [BI] 1995;9(1):81–92. doi: 10.3109/02699059509004574. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthen & Muthen; 1998. [Google Scholar]
- Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annual Review of Clinical Psychology. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- Oakley F, Kielhofner G, Barris R, Reichler RK. The Role Checklist: Development and empirical assessment of reliability. Occupational Therapy Journal of Research. 1986;6(3):157–170. [Google Scholar]
- Pavot W, Diener E. The Satisfaction With Life Scale and the emerging construct of life satisfaction. The Journal of Positive Psychology. 2008;3(2):137–152. doi: 10.1080/17439760701756946. [DOI] [Google Scholar]
- Resch JA, Villarreal V, Johnson CL, Elliott TR, Kwok OM, Berry JW, Underhill AT. Trajectories of life satisfaction in the first 5 years following traumatic brain injury. Rehabilitation Psychology. 2009;54(1):51–59. doi: 10.1037/a0015051. [DOI] [PubMed] [Google Scholar]
- Sander AM, Pappadis MR, Clark AN, Struchen MA. Perceptions of community integration in an ethnically diverse sample. The Journal of Head Trauma Rehabilitation. 2011;26(2):158–169. doi: 10.1097/HTR.0b013e3181e7537e. [DOI] [PubMed] [Google Scholar]
- Stålnacke BM. Community integration, social support and life satisfaction in relation to symptoms 3 years after mild traumatic brain injury. Brain Injury: [BI] 2007;21(9):933–942. doi: 10.1080/02699050701553189. [DOI] [PubMed] [Google Scholar]
- Temkin NR, Corrigan JD, Dikmen SS, Machamer J. Social functioning after traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2009;24(6):460–467. doi: 10.1097/HTR.0b013e3181c13413. [DOI] [PubMed] [Google Scholar]
- Tsaousides T, Warshowsky A, Ashman TA, Cantor JB, Spielman L, Gordon WA. The relationship between employment-related self-efficacy and quality of life following traumatic brain injury. Rehabilitation Psychology. 2009;54(3):299–305. doi: 10.1037/a0016807. [DOI] [PubMed] [Google Scholar]
- Underhill AT, Lobello SG, Stroud TP, Terry KS, Devivo MJ, Fine PR. Depression and life satisfaction in patients with traumatic brain injury: a longitudinal study. Brain Injury. 2003;17(11):973–982. doi: 10.1080/0269905031000110418. [DOI] [PubMed] [Google Scholar]
- Walton DM, Macdermid JC, Taylor T ICON. What does “recovery” mean to people with neck pain? Results of a descriptive thematic analysis. The Open Orthopaedics Journal. 2013;7:420–427. doi: 10.2174/1874325001307010420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteneck GG, Dijkers MP, Heinemann AW, Bogner JA, Bushnik T, Cicerone KD, Millis SR. Development of the participation assessment with recombined tools-objective for use after traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2011;92(4):542–551. doi: 10.1016/j.apmr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Williamson MLC, Elliott TR, Berry JW, Underhill AT, Stavrinos D, Fine PR. Predictors of health-related quality-of-life following traumatic brain injury. Brain Injury: [BI] 2013;27(9):992–999. doi: 10.3109/02699052.2013.801512. [DOI] [PubMed] [Google Scholar]
- Williamson MLC, Elliott TR, Bogner JA, Dreer L, Arango-Lasprilla JC, Kolakowsky-Hayner S, Perrin PB. Trajectories of Life Satisfaction over the first ten years after Traumatic Brain Injury: Race, gender, and functional impairment. Journal of Head Injury Rehabilitation. 2015 doi: 10.1097/HTR.0000000000000111. In Press. [DOI] [PubMed] [Google Scholar]