Abstract
Background:
Metastatic papillary thyroid carcinoma typically appears in local lymph nodes. Skin metastases are rare.
Purpose:
A man with progressive metastatic papillary thyroid carcinoma who developed a cutaneous metastasis on his nose is described. The clinical manifestations of metastatic papillary thyroid carcinoma to skin are reviewed.
Methods:
PubMed was used to search the following terms, separately and in combination: basal, cancer, carcinoma, cell, cutaneous, kinase, inhibitor, metastases, nose, papillary, rearranged during transfection, receptor, RET, thyroid, tyrosine, vandetanib.
Results:
Pathologic changes observed on the biopsy of the man’s nose lesion were similar to those of his original cancer. Genomic evaluation of the tumor revealed an aberration involving the rearranged during transfection (RET) receptor tyrosine kinase. The residual tumor was excised. Treatment with vandetanib, a RET inhibitor was initiated; his metastatic disease has been stable, without symptoms or recurrent cutaneous metastasis, for 2 years following the discovery of his metastatic nose tumor.
Conclusions:
Papillary thyroid carcinoma with skin metastases is rare. Nodules usually appear on the scalp or neck; the thyroidectomy scar is also a common site. Metastatic tumor, albeit infrequently, can present as a nose lesion. The prognosis for patients with cutaneous metastases from papillary thyroid carcinoma is poor. However, with the ability to test the tumor for genomic aberrations, molecular targeted therapies—such as tyrosine kinase inhibitors—may provide extended survival in these individuals.
Keywords: basal, cancer, carcinoma, cell, cutaneous, kinase, inhibitor, metastases, nose, papillary, rearranged during transfection, receptor, RET, thyroid, tyrosine, vandetanib
Introduction
The most common endocrine malignancy is thyroid cancer. Papillary and follicular thyroid carcinoma are the most frequent subtypes. Metastatic thyroid carcinoma usually appears in the local lymph nodes. Indeed, distant metastases of papillary and follicular thyroid carcinoma are uncommon. When these occur, the sites typically include lung and bone. However, albeit rare, papillary and follicular thyroid carcinoma have both been associated with skin metastases [1,2].
Cutaneous metastases from papillary thyroid carcinoma are reported in less than 1 in 1,000 patients with this cancer [2]. The scalp is the most frequent site [3–7]. A man with progressing metastatic papillary thyroid cancer to lung who developed a cutaneous metastasis on the nose mimicking a basal cell carcinoma is described and the various clinical presentations of metastatic papillary thyroid cancer to skin are reviewed.
Case report
A 72-year-old man was referred by his oncologist for evaluation of a lesion on his nose that was suspected to be a basal cell carcinoma. The lesion was painless and had appeared 3 weeks earlier.
His past medical history was significant for metastatic papillary thyroid carcinoma diagnosed 6.5 years earlier. A total thyroidectomy and neck dissection was followed by adjuvant radioactive iodine-131. When lung nodules were discovered 1.25 years later, he received another treatment with iodine-131. He subsequently developed progressive chest disease 0.75 years later and received an additional treatment of iodine-131 in combination with capecitabine. He received stereotactic radiosurgery to lung metastases 1 year later; 2 years and 3.3 years later, he had excision of enlarged chest lymph nodes that showed tumor.
Restaging, 3 months prior to his nose lesion, showed not only intrathoracic metastatic disease (with pulmonary nodules and enlarged mediastinal lymph nodes), but also metastases to the right adrenal gland and bone. He was experiencing progressive fatigue. However, there was neither cough nor difficulty breathing.
Cutaneous examination showed an asymptomatic 7 × 7 mm violaceous non-telangiectatic nodule with central erosion on the right nasal tip (Figure 1). Microscopic examination of a 2 mm punch showed scale crust and parakeratosis overlying an atrophic epidermis. In the dermis, there were multiple nodules composed of large cells forming papillary projections. The papillae were composed of a stratified lining of cuboidal and columnar tumor cells with eosinophilic cytoplasm and a central fibrovascular core that contained occasional lymphocytes. Focally, there were tumor cells with altered nuclear morphology. Some cells showed crowding and overlapping of enlarged and elongated nuclei. Other cells demonstrated intranuclear cytoplasmic pseudoinclusions (Figure 2). The tumor cells stained positive for thyroid transcription factor-1 (TTF-1) and paired box gene 8 (PAX8).
Figure 1.


Lateral (a) and upward (b) views of cutaneous metastatic papillary thyroid carcinoma presenting as an asymptomatic nodule with central erosion on the right nasal tip that morphologically mimicked a basal cell carcinoma. [Copyright: ©2015 Cohen.]
Figure 2.
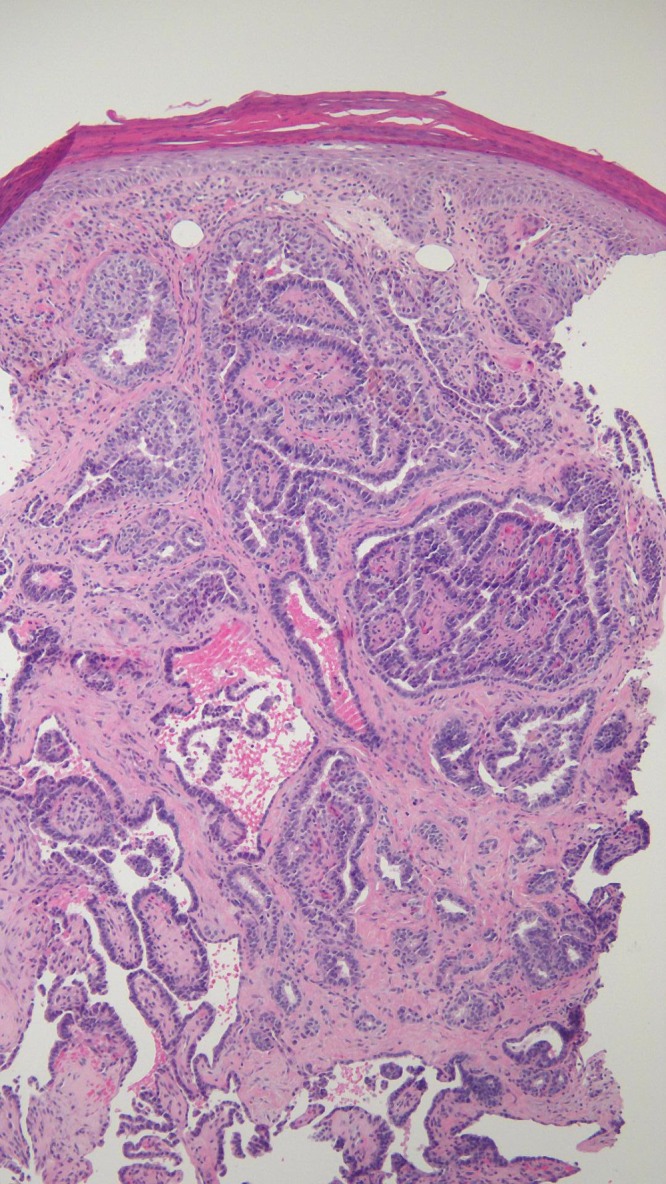
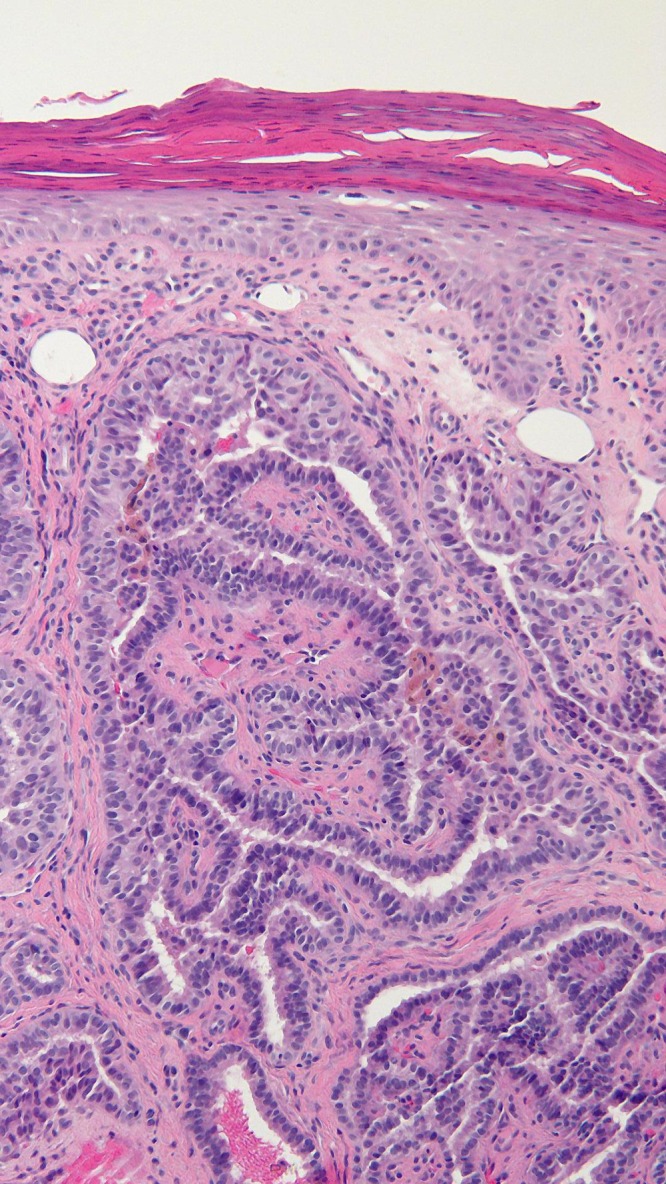
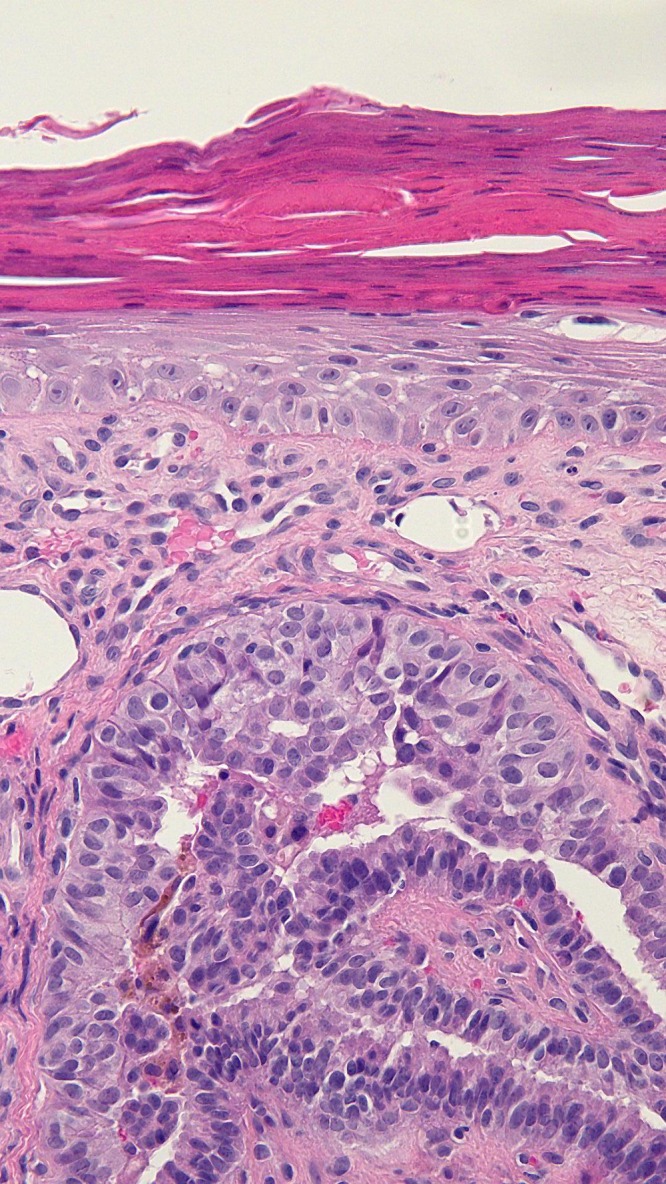
Low (a), medium (b), and high (c) magnification views of the papillary thyroid carcinoma metastasis shows aggregates of tumor cells in the dermis that are similar to those of the primary thyroid neoplasm. Cuboidal and columnar cells line the lymphocyte-containing fibrovascular cores of tumor papillae. The cells have eosinophilic cytoplasm; some of them also have nuclear changes including enlarged and enlongated nuclei that are crowded and overlapping and nuclear pseudoinclusions [hematoxylin and eosin; a = ×10, b = ×20, c = ×40]. [Copyright: ©2015 Cohen.]
Correlation of the clinical history and pathology established a diagnosis of metastatic papillary thyroid carcinoma to skin. The residual tumor on the nose was excised without recurrence. However, within 6 months, he had progressive shortness of breath; follow up studies showed progressive chest disease.
His tumor was sent for genomic studies (Foundation One, Cambridge, MA). An aberration in the rearranged during transfection (RET) receptor tyrosine kinase was identified: an in-frame fusion of coiled-coil domain containing 6 (CCDC6) up to intron 1, with RET from intron 11 to the end. Treatment was initiated and maintained with the RET inhibitor vandetanib; he has had stable metastatic disease without symptoms 1.5 years after starting this drug.
Discussion
Cutaneous metastases may develop in patients with an established diagnosis of cancer. In this setting, they typically herald the onset of either relapsing or progressive disease in an oncology patient. However—albeit less commonly—they can be the initial presentation of an unsuspected internal malignancy in a previously cancer-free individual.
The morphology of cutaneous metastases is variable. The lesions can present as patches, plaques, papules or nodules. They can mimic other conditions such as alopecia, infections (erysipelas and paronychia), benign cysts (epidermoid or pilar), pyogenic granuloma and cutaneous malignant neoplasms (basal cell carcinoma and keratoacanthoma) [4,5,7].
Common skin manifestations of metastatic papillary thyroid cancer, in addition to scalp nodules, include neck nodules [3,4,8] and lesions on the thyroidectomy scar [1]. Metastatic tumor at the fine-needle aspiration biopsy site has been observed [8]. Also, lesions of cutaneous papillary thyroid carcinoma metastases have been described on the abdominal wall [6,9], arm [6], buttock [9], chest wall [3], face [3,6], shoulder [6] and thigh [9].
Microscopic examination of papillary thyroid carcinoma cutaneous metastases shows similar pathology features as the primary cancer. Immunohistochemical stains can also be helpful to confirm the diagnosis and exclude tumors originating from other organs. Papillary thyroid carcinoma typically expresses thyroid transcription factor-1 (TTF-1, a 38-kd homeodomain containing DNA binding nuclear protein expressed in the follicular cells of the thyroid and present in 93% of thyroid tumors) [4,10] and thyroglobulin (a 670-kd glycoprotein synthesized in the cytoplasm of follicular thyroid epithelial cells and detected in 95% of papillary thyroid carcinomas) [3,4]. It also usually expresses cytokeratin 7 (a type II keratin found in the follicular cells of the thyroid gland) [11] and paired box gene 8 (PAX8, a nephric-lineage transcription factor that is a crucial transcription factor for the organogenesis of the kidney, the Mullerian system and the thyroid gland) [12].
The nose is an unusual site for cutaneous metastases. In addition to thyroid carcinoma, other cancers with metastatic lesions on the nose include solid tumors originating from the breast, cervix, liver, lung and testes [13]; immunohistochemical markers can be used to differentiate the organ of origin of these metastatic tumors (Table 1). The described patient was referred for evaluation of a suspected basal cell carcinoma. Morphologic features of the nodule that suggested the possibility of metastatic tumor included its violaceous appearance and the absence of telangiectasias.
TABLE 1.
Immunohistochemistry markers of solid tumors that metastasize to the nose
| Tumor origin | Immunohistochemical marker |
|---|---|
|
| |
| Breast |
|
|
| |
| Cervix |
|
|
| |
| Liver |
|
|
| |
| Lung | |
| NSCLC |
|
| SCLC |
|
|
| |
| Testes | |
| GCT |
|
| SC/ST |
|
|
| |
| Thyroid |
|
Abbreviations: GCT, germ cell tumor; NSCLC, non-small cell lung cancer; SCLC, small cell lung cancer; SC/ST, sex cord/stromal tumor.
In addition to the patient in this report, another man with papillary thyroid carcinoma also had a cutaneous metastasis on his nose; in this individual, the nose lesion was the initial presentation of his metastatic disease [14]. He was a 73-year-old Caucasian man who developed a raised, non-pigmented lesion on his left nasal ridge; biopsy revealed papillary thyroid carcinoma. In addition to a thyroid mass, he had metastases to his lungs, bone and liver. Management included a partial thyroidectomy, palliative radiotherapy (to the neck and cervical spine to treat tracheal invasion of the tumor and spinal cord compression, respectively), doxorubicin and radioactive iodine. Three years later, his lung and pleural lesions progressed; pathology demonstrated anaplastic transformation of his tumor [14].
Similar to the reported patient, other investigators have commented that since “ . . . the natural history of thyroid cancer is one of slow progression skin metastases may be confused with other skin neoplasms such as basal cell carcinoma . . .” [5] Indeed, their patient—a 70-year-old man—presented with a enlarged thyroid gland and cervical lymphadenopathy; pathology from his total thyroidectomy and neck dissection established a diagnosis of papillary thyroid carcinoma. Three years after receiving adjuvant treatment with radioactive iodine ablation and external beam radiotherapy, he developed a 1 cm nodular scalp lesion that was clinically thought to be a basal cell carcinoma; however, excisional biopsy showed papillary thyroid carcinoma. Within four months, he died [5].
Cutaneous metastasis of papillary thyroid carcinoma may be the presenting manifestation of previously undiagnosed malignancy [3,14]. The described patient’s nose lesion of metastatic papillary thyroid carcinoma occurred 6.5 years following his initial diagnosis of cancer and in the setting of progressive metastatic disease that had been treated with iodine-131 (on three occasions, without or with concurrent capecitabine) and stereotactic radiosurgery. Similar to this patient, many of the individuals who develop skin metastases from papillary thyroid carcinoma typically present with cutaneous lesions several years (ranging from less than 2 years to 20 years) following the diagnosis of their original cancer [1,3,4,6–8].
The prognosis for patients with metastatic papillary thyroid carcinoma to the skin, in general, is unfavorable [3,5]. However, there are several individuals with metastatic papillary thyroid carcinoma who survive several years after diagnosis with indolent disease [1,3,9]. Also, similar to the described patient, with the advent of molecular targeted therapies, such as tyrosine kinase inhibitors, the prognosis for patients with metastatic disease—and particularly those with rearranged during transfection (RET) proto-oncogene aberrations—is better than that observed in individuals with papillary thyroid carcinoma who were treated prior to the discovery of these agents [15].
Conclusion
Papillary thyroid carcinoma with skin metastases is rare. Cutaneous metastases of papillary thyroid carcinoma most commonly occur as nodules on the scalp, neck, and thyroidectomy scars. A man with progressive metastatic papillary thyroid carcinoma developed a cutaneous metastasis on his nose; the lesion morphologically mimicked a basal cell carcinoma. Cutaneous papillary thyroid carcinoma metastases may not only occur several years following the diagnosis of the primary cancer, but also can occur on the nose or mimic basal cell carcinoma or both. Cutaneous metastases of papillary thyroid carcinoma have previously been associated with a poor prognosis; however, some of the patients have indolent neoplastic disease and survive for several years. Similar to the described patient, whose genomic evaluation of the tumor showed an aberration involving the rearranged during transfection (RET) receptor tyrosine kinase, the use of molecular targeted therapies may provide extended survival for individuals diagnosed with cutaneous metastatic papillary thyroid carcinoma.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Bruglia M, Palmonella G, Silvetti F, et al. Skin and thigh muscle metastasis from papillary thyroid cancer. Singapore Med J. 2009;50:e61–e64. [PubMed] [Google Scholar]
- 2.Koller EA, Tourtelot JB, Pak HS, et al. Papillary and follicular thyroid carcinoma metastatic to the skin: a case report and review of the literature. Thyroid. 1998;8:1045–50. doi: 10.1089/thy.1998.8.1045. [DOI] [PubMed] [Google Scholar]
- 3.Dahl PR, Brodland DG, Goellner JR, Hay ID. Thyroid carcinoma metastatic to the skin: a cutaneous manifestation of a widely disseminated malignancy. J Am Acad Dermatol. 1997;36:531–7. doi: 10.1016/s0190-9622(97)70239-1. [DOI] [PubMed] [Google Scholar]
- 4.Alwaheeb S, Ghazarian D, Boerner SL, Asa SL. Cutaneous manifestations of thyroid cancer: a report of four cases and review of the literature. J Clin Pathol. 2004;57:435–8. doi: 10.1136/jcp.2003.012922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Makris A, Goepel JR. Cutaneous metastases from a papillary thyroid carcinoma [letter] Br J Dermatol. 1996;135:860–1. doi: 10.1111/j.1365-2133.1996.tb03910.x. [DOI] [PubMed] [Google Scholar]
- 6.Horiguchi Y, Takahashi C, Imamura S. Cutaneous metastasis from papillary carcinoma of the thyroid gland: report of two cases. J Am Acad Dermatol. 1984;10:988–92. doi: 10.1016/s0190-9622(84)80320-5. [DOI] [PubMed] [Google Scholar]
- 7.Aghasi MR, Valizadeh N, Soltani S. A 64 year-old female with scalp metastasis of papillary thyroid cancer. Indian J Endocr Metab. 2011;15(S2):S136–7. doi: 10.4103/2230-8210.83353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tamiolakis D, Antoniou C, Venizelos J, et al. Papillary thyroid carcinoma metastasis most probably due to fine needle aspiration biopsy. A case report. Acta Dermatoven APA. 2006;15:169–72. [PubMed] [Google Scholar]
- 9.Loureiro MM, Lette VH, Boavida JM, et al. An unusual case of papillary carcinoma of the thyroid with cutaneous and breast metastases only. Eur J Endocrinol. 1997;137:267–9. doi: 10.1530/eje.0.1370267. [DOI] [PubMed] [Google Scholar]
- 10.Ordonez NG. Value of thyroid transcription factor-1 immunostaining in tumor diagnosis: a review and update. Appl Immunohistochem Mol Morphol. 2012;20:429–44. doi: 10.1097/PAI.0b013e31825439bc. [DOI] [PubMed] [Google Scholar]
- 11.Chu PG, Lau SK, Weiss LM. Keratin expression in endocrine organs and their neoplasms. Endocr Pathol. 2009;20:1–10. doi: 10.1007/s12022-009-9061-7. [DOI] [PubMed] [Google Scholar]
- 12.Laury AR, Perets R, Piao H, et al. A comprehensive analysis of PAX8 expression in human epithelial tumors. Am J Surg Pathol. 2011;35:816–26. doi: 10.1097/PAS.0b013e318216c112. [DOI] [PubMed] [Google Scholar]
- 13.Chun SM, Kim YC, Lee J-B, et al. Nasal tip cutaneous metastases secondary to lung carcinoma: three case reports and a review of the literature. Acta Derm Venereol. 2013;93:569–72. doi: 10.2340/00015555-1529. [DOI] [PubMed] [Google Scholar]
- 14.Khan OA, Roses DF, Peck V. Papillary thyroid carcinoma metastatic to skin may herald aggressive disease. Endocr Pract. 2010;16:446–8. doi: 10.4158/EP09178.CR. [DOI] [PubMed] [Google Scholar]
- 15.Prescott JD, Zeiger MA. The RET oncogene in papillary thyroid carcinoma. Cancer. 2015 doi: 10.1002/cncr.29044. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


