Abstract
Self-distancing, or viewing oneself from a third-person perspective, reduces reactivity when analyzing one's feelings. Self-distancing may have important effects among individuals with posttraumatic stress disorder (PTSD), who have heightened emotional and physiological reactivity to trauma memories, but the effects of self-distancing in this group are unclear. We randomly assigned 48 Veterans diagnosed with PTSD to analyze their trauma-related feelings from an immersed (first-person) or distanced (third-person) perspective, and measured physiological and subjective emotional reactivity. Self-distancing during trauma analysis protected against increases in physiological reactivity, such that participants in the immersed condition showed a significant increase in heart rate and skin conductance responses not seen in the distanced condition. However, self-distancing had no effect on self-reported emotional reactivity. Our findings suggest that the effects of self-distancing on subjective emotions may not extend to trauma memories. However, self-distancing during trauma analysis did change physiological reactivity, suggesting at least a short-term benefit for individuals with PTSD.
Keywords: Self-distancing, visual perspective, PTSD, trauma, memory
“Distance has the same effect on the mind as on the eye.”
-Samuel Johnson, The History of Rasslas, Prince of Abissinia
Humans are perhaps the only animals that engage in self-reflection, or thinking about our own thoughts, feelings, and experiences. Self-reflection can be adaptive, allowing us to learn from past experiences and gain insight into our emotions. Socrates’ famous assertion that “the unexamined life is not worth living” typifies the human need to look inward. However, when reflecting upon negative emotions or experiences, people often fall into maladaptive forms of self-reflection, such as rumination (Nolen-Hoeksema, Wisco, & Lyubomirksy, 2008). Rather than enhancing well-being, rumination leads to undesirable outcomes, including depression, anxiety, and even suicidal thoughts (Nolen-Hoeksema et al., 2008).
Self-distancing has been proposed as a potentially adaptive way to analyze negative emotional experiences without ruminating (Kross, Ayduk, & Mischel, 2005). Self-distancing is typically operationalized as adopting a third-person visual perspective, or viewing oneself from the perspective of an outside observer, when analyzing one's feelings about a past event (Kross et al., 2005; Kross, Gard, Deldin, Clifton, & Ayduk, 2012). It is related to prior memory research examining visual perspective (e.g., McIsaac & Eich, 2002; 2004), but is distinguished by the specific instruction to analyze one's feelings about the past event, which might typically lead to rumination. Self-distancing is thought to be beneficial because it allows individuals to change their thinking about past events and gain insight, rather than simply recount their negative emotions (e.g., Kross et al., 2005; 2012). In support of this model, self-distancing has been shown to reduce subjective emotional reactivity to anger-eliciting and sad memories among nonclinical samples (e.g., Ayduk & Kross, 2008; Kross et al., 2005; Kross & Ayduk, 2008). Self-distancing has also been shown to reduce physiological responses, including blood pressure reactivity to anger-eliciting memories, and heart rate reactivity to positive memories (Ayduk & Kross, 2008; Gruber et al., 2009). The short-term benefits of self-distancing have been demonstrated among individuals with elevated depressive symptoms (Kross & Ayduk, 2009; Wisco & Nolen-Hoeksema, 2011) and individuals diagnosed with mood disorders (Gruber et al., 2009; Kross et al., 2012). For these reasons, self-distancing has been proposed as an adaptive way of processing negative memories for individuals with emotional problems.
The possible effects of self-distancing may be particularly relevant for individuals with posttraumatic stress disorder (PTSD), a condition characterized by disruption in processing of negative memories, specifically memories of a traumatic event. The diagnostic criteria for PTSD include intense emotional responses (e.g., fear, anger) and heightened physiological reactivity (e.g., heart rate and sweating) to trauma memories and other reminders (American Psychiatric Association, 2000, 2013). Self-distancing may reduce these intense emotional and physiological reactions to trauma memories, at least in the short term. Moreover, evidence-based treatments for PTSD include an explicit focus on the trauma memory, often including instructions to visualize the trauma memory as part of treatment (e.g., imaginal exposure; Foa & Rothbaum, 1998). The visual perspective that one adopts while engaging in imaginal exposure might have important implications for the effectiveness of this technique.
However, little is known about the effects of self-distancing from trauma memories. One previous study compared emotional reactions to trauma memories when individuals with PTSD were asked to adopt the visual perspective they typically use to recall their trauma memory (McIsaac & Eich, 2004). This study found that individuals who used the distanced perspective reported reduced emotional reactions to trauma memories compared with individuals who used the immersed perspective, consistent with the broader self-distancing literature (McIsaac & Eich, 2004). Other research, however, has shown that PTSD symptoms are associated with an increased tendency to spontaneously adopt a distanced perspective when recalling a trauma memory (Kenny & Bryant, 2007), and that the tendency to use the distanced perspective prospectively predicts the development of PTSD (Kenny et al., 2009). These findings seem to contradict the premise that self-distancing from trauma memories serves as an adaptive emotion regulation strategy.
An important limitation of prior work on self-distancing and trauma memories is the reliance upon correlational designs, in which participants were not randomly assigned to visual perspective. To better determine the effect of self-distancing on one's reactions to trauma memories, we need to experimentally manipulate perspective. Moreover, all of the prior work on trauma memories has focused on perspective when simply recalling a trauma memory. The regulatory benefits of self-distancing are thought to emerge when analyzing one's feelings about a past event, not simply recounting the event (i.e., asking “why” rather than “what” one felt; Kross et al., 2005). Therefore, it is important to examine the effects of self-distancing in the specific context of analyzing one's feelings about a trauma. Additionally, prior research on self-distancing from trauma memories has been limited to self-reported emotional reactions. Because both emotional and physiological reactivity to trauma-related reminders are symptoms of PTSD, examining effects of self-distancing on both subjective emotional response and physiological arousal is especially important in this population.
This study examined the effects of self-distancing on physiological and subjective emotional reactivity while analyzing trauma memories among Veterans diagnosed with PTSD. Given prior findings of self-distancing while analyzing emotional memories, we predicted that analyzing trauma memories from the distanced perspective would lead to less subjective emotional and physiological reactivity than the immersed perspective.
Method
Participants
Potential participants were recruited from two sources: a database of Veterans who had previously consented to be contacted for research in a specialty VA PTSD clinic, and advertisements distributed at VA outpatient medical centers and an outreach event for homeless Veterans. Inclusion criteria for this study were: Veteran status, age 18 or older, ability to read and write in English, and a current diagnosis of PTSD. Due to safety concerns, we excluded individuals with implanted medical devices, active suicidality, or active homicidal ideation. Of 60 participants who consented to participate, we excluded 10 because they did not meet full criteria for PTSD according to diagnostic interview, and two due to safety concerns (active suicidal or homicidal ideation), leaving a final sample of 48 participants. Participants’ ages ranged from 24 to 70 with a mean of 53.94 (SD = 10.02); four (8.4%) participants were between the ages of 24 and 44, 30 (62.5%) were 45 to 59, and 14 (29.2%) were 60 or older. Participants reported their race/ethnicity as: 26 (54.2%) White (non-Hispanic), 18 (37.5%) Black, and 4 (8.3%) Hispanic; 46 (95.8%) participants were male.
Procedure
Potential participants completed a telephone screen to determine eligibility criteria and probable PTSD diagnosis. Participants were randomly assigned to visual perspective condition (25 distanced, 23 immersed) and completed two study sessions within two weeks. All participants enrolled in the study returned for the second study session. The first session consisted of informed consent and an assessment battery including the Clinician-Administered PTSD Scale for DSM-IV (CAPS; Blake et al., 1995), which was used to verify PTSD status. During the second study session, participants were connected to the psychophysiological apparatus, rated their emotions and arousal using the Positive and Negative Affect Scale Expanded Form (PANAS-X; Watson, & Clark, 1999) and the Self-Assessment Manikin (SAM; Lang, Bradley, & Cuthbert, 1997), and completed a two minute resting baseline phase. Participants then completed the trauma memory analysis, in which they were asked to analyze their worst traumatic experience, which had previously been identified during the CAPS interview. Participants were instructed to form a clear image of their worst traumatic event in their minds from the assigned visual perspective, then to analyze why they felt the way they did at the time of the event for 90 seconds (30 seconds of instructions plus 60 seconds of analysis). Audiorecorded instructions were provided to elicit the assigned visual perspective (e.g., immersed: “Now see the situation unfold through your own eyes as if it were happening to you all over again;” distanced: “Take a few steps back. Move away from the situation to a point where you can now watch the event unfold from a distance and see yourself in the event.”). These instructions were derived from the induction created by Kross and colleagues (2005). After completing this task, participants completed a second PANAS-X and SAM in addition to a battery of self-report measures including emotional re-experiencing questions, demographics, and manipulation checks. Participants were compensated $75. All procedures were approved by the local Institutional Review Board.
Psychophysiological Procedure
Heart rate (HR) was recorded using 8mm disposable electrodes filled with electrolyte paste placed on the right forearm and left ankle. HR was analyzed using a Mindware ECG amplifier and a Mindware ECG software package. Skin conductance responses (SCRs) were collected using two disposable 8mm Ag/AgCl electrodes filled with paste, which were attached to the palm or index and middle fingers of the non dominant hand. SCRs were defined as responses of 0.05 microSiemens or greater and were analyzed using a Mindware galvanic SC transducer and software. HR in beats per minute and SCRs in number of SCRs per minute were averaged across the 120 second resting baseline phase to give baseline HR and SCRs, and averaged across the 90 second trauma analysis phase to give trauma analysis HR and SCRs.
Measures
Clinician Administered PTSD Scale (CAPS; Blake et al., 1995)
The CAPS is a semi-structured clinical interview designed to assess the 17 core symptoms of PTSD, as defined by the DSM-IV-TR (American Psychiatric Association, 2000). The CAPS allows the interviewer to rate the frequency and intensity of each symptom along 5-point ordinal scales. The total score for the CAPS PTSD ratings (frequency + intensity) range from 0 to 136. A diagnosis of PTSD was confirmed if participants received a total score of 40 or higher and endorsed at least one re experiencing, three avoidance, and two hyperarousal symptoms, using standard scoring criteria of a minimum frequency score of “1” and intensity score of “2” (Weathers, Keane, & Davidson, 2001). Interviews were administered by a postdoctoral fellow with specialty training in PTSD assessment. Interviews were audiorecorded, and a subset (n = 4) were rated for inter-rater reliability, which was excellent (ICC = .94).
Self-Assessment Manikin (SAM) Ratings (Lang, Bradley, & Cuthbert, 1997)
The SAM is a well-validated, brief, pictorial measure used to assess a person's current feelings. The arousal scale, illustrated with five pictures on a 9 point scale ranging from extremely aroused to extremely calm, was used for this study. Responses were coded such that higher numbers reflect greater levels of arousal.
Positive and Negative Affect Schedule–Expanded (PANAS-X) Form (Watson, & Clark, 1999)
The PANAS-X is a 60 item self-report measure that assesses positive and negative affect (e.g., cheerful, shy). Participants are instructed to rate each word on a Likert scale of 1 through 5 (1 = very slightly or not at all; 5 = extremely). The negative affect scale was used for this study and had excellent internal consistency (.88-.93).
Emotional Re-experiencing
Two additional questions were used to assess subjective emotional reactivity to trauma analysis. Participants were asked to rate on a Likert-type scale (from 1 = “not at all” to 7 = “a lot”) the extent to which they re-experienced the original negative emotions they experienced and with what intensity they re-experienced those emotions (Kross et al., 2005). The two highly correlated measures, r = .84, p < .001, were summed to form a single index of emotional re-experiencing.
Manipulation Check
Participants were asked to respond to a question assessing how well they were able to adopt the instructed perspective. Following Wisco and Nolen-Hoeksema (2011), participants in the immersed condition were asked “to what extent were you able to see the situation through your own eyes?” and participants in the distanced condition were asked “to what extent were you able to see yourself in the situation?” Both groups rated the questions on a five point Likert-type scale, from “not at all” to “very well.”
Data Analysis
Primary analyses consisted of separate repeated measures ANOVAs for each measure of reactivity, to include two measures of physiological reactivity (HR and number of SCRs per minute) and two measures of subjective emotional reactivity (SAM arousal rating, PANAS negative affect). For all repeated measures ANOVAs, time (baseline, trauma analysis) was entered as a within subjects variable and condition (distanced, immersed) was entered as a between-subjects variable. An additional univariate ANOVA was planned to examine the effect of condition on the self-report measure of emotional re-experiencing.
Results
Participants in the distanced and immersed conditions did not differ by age, F(1, 46) = 0.20, p =.659, ηp2 = .004, gender, race, or handedness, χ2s < 0.80, ps > .650, φs <0.15. There was a marginally significant difference in PTSD severity (CAPS total score), between participants in the distanced (M = 73.88, SD = 15.73) and immersed (M = 65.61, SD = 13.50) conditions, F(1, 46) = 3.79, p = .058, ηp2 = .076.1 The memories analyzed during the experimental sessions represented a wide variety of trauma types: natural disaster (n = 1), transportation accident (n = 3), other serious accident (n = 1), physical assault (n = 4), assault with a weapon (n = 3), sexual assault (n = 9), other unwanted or uncomfortable sexual experience (n = 1), combat or war-zone exposure (n = 8), captivity (n = 1), life-threatening illness or injury (n = 2), severe human suffering (n = 5), sudden, violent death (n = 5), sudden unexpected death of someone close to the participant (n = 2), and serious injury, harm, or death the participant caused to someone else (n = 3). The trauma type of the memory analyzed did not differ by condition, χ2 (13, N = 48) = 15.29, p = .290, φ = 0.56. The time since the trauma also varied, with the number of years elapsed since the traumatic event ranging from one to 50 years (M = 32.25, SD = 12.56). The time since the trauma did not differ by condition, F = 0.48, p = .49, ηp2 = .010.1 Analysis of the manipulation check questions revealed that the conditions did not differ on the degree to which participants reported adopting the intended perspective, F(1, 43) = 2.00, p =.164, ηp2 = .044.1
Physiological Reactivity
Due to difficulty obtaining a valid signal, HR data were unavailable for two participants, and SCR data were unavailable for one participant. Repeated measures ANOVA of HR revealed a marginally significant main effect of time, F(1, 44) = 3.78, p =.058, ηp2 =.079, which was in the direction of HR increasing during trauma analysis, relative to baseline. A significant interaction between time and condition emerged, F(1, 44) = 5.07, p = .029, ηp2 = .103 (see Figure 1).
Figure 1.
Physiological Reactivity to Trauma Memory Analysis
Follow-up paired t-tests showed that participants in the immersed condition showed a significant increase in HR from baseline to trauma analysis, t(21) = 2.31, p =.031, d = 0.49, whereas participants in the distanced condition showed no change in HR, t(23) = 0.33, p =.747, d = 0.08. The analysis of SCRs per minute revealed a significant effect of time, F(1, 45) = 7.82, p =.008, ηp2 =.148, such that participants showed an increase in number of SCRs during trauma analysis relative to baseline. This main effect of time was qualified by a significant interaction between time and condition, F(1, 45) = 5.35, p = .025, ηp2 = .106 (Figure 1). Follow-up paired t-tests revealed that participants in the immersed condition showed a significant increase in SCRs per minute from baseline to trauma analysis, t(21) = 2.88, p =.009, d = 0.71, whereas participants in the distanced condition showed no change in SCRs per minute, t(24) = 0.46, p = .648, d = 0.09.
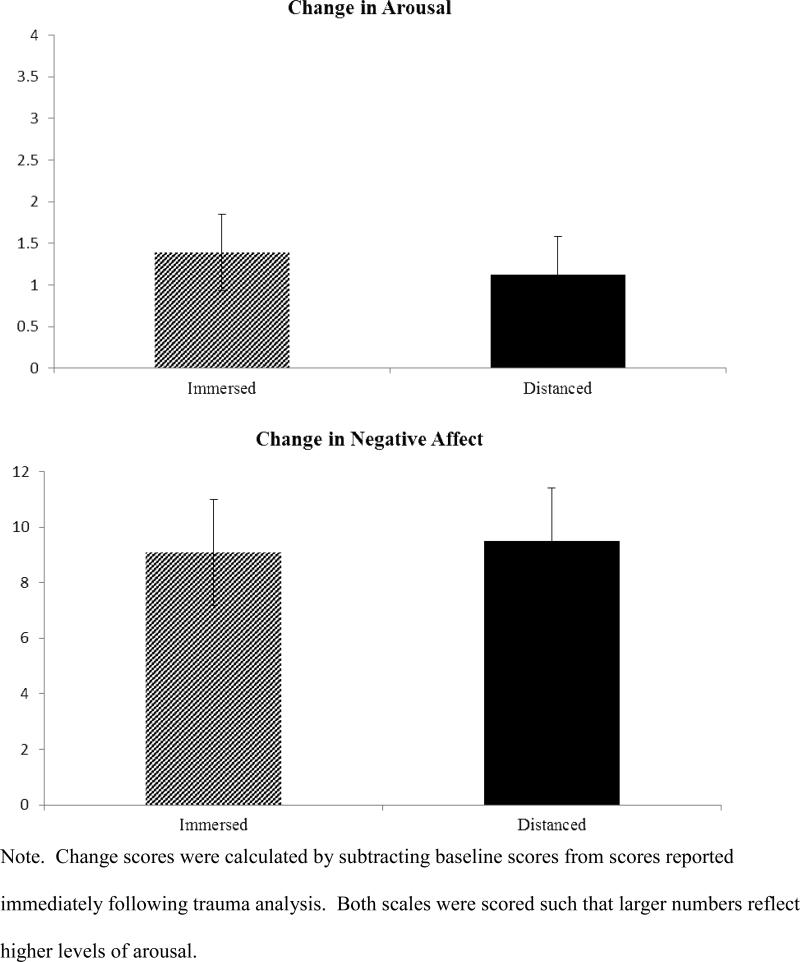
Subjective Emotional Reactivity
There was a significant effect of time on self-reported (SAM) arousal, F(1, 46) = 14.72, p < .001, ηp2 = .242, such that participants in general reported an increase in arousal from baseline to trauma analysis. The interaction between time and condition on arousal was not significant, F(1, 46) = 0.17, p = .680, ηp2 = .004 (see Figure 2).
Figure 2.
Emotional Reactivity to Trauma Memory Analysis
The analysis of negative affect also revealed a significant effect of time, F(1, 44) = 47.28, p < .001, ηp2 = .518, such that negative affect increased from baseline to trauma analysis.2 The interaction between time and condition on negative affect was not significant, F(1, 44) = 0.02, p = .880, ηp2 = .001. Finally, there was no effect of condition on self-reported emotional re-experiencing during trauma analysis, F(1, 45) = 0.28, p = .600, ηp2 = .006.2
Discussion
Individuals who analyzed their trauma-related feelings from the immersed perspective showed significant increases in HR and SCRs. In contrast, individuals who self-distanced showed no change in HR or SCRs. Importantly, this finding was consistent across two channels indexing physiological response, offering strong support for the finding that self-distancing from trauma protects against expected increases in physiological reactivity among individuals with PTSD.
However, self-distancing from trauma-related feelings did not reduce subjective emotional reactivity. This is inconsistent with prior research examining self-distancing from anger-eliciting and sad memories in nonclinical and clinically depressed samples. We examined Veterans with PTSD, who may differ in important ways from unselected undergraduates or even clinically depressed individuals. One key distinction is the type of disorder we assessed: self-distancing may have very different effects for individuals with PTSD than individuals with depression. Alternatively, perhaps participants in our study were less able to follow instructions to self-distance than participants in prior work. However, participants in our study reported that they followed the instructions on a manipulation check, and self-distancing had a significant effect on two measures of physiological arousal. A potential explanation for the null effect on subjective emotional reactivity in our study is the type of memories analyzed. Our study used memories of traumatic events, which commonly elicit intense emotional responses, particularly among individuals diagnosed with PTSD. Compared with prior self-distancing work with anger-eliciting memories, our participants reported greater emotional re-experiencing and negative affect (Kross et al., 2005).3 This study offers initial evidence that the effects of self-distancing on subjective emotional reactivity may not extend to extremely distressing memories, such as trauma memories. However, it is important to note that we did not directly compare trauma memories with less distressing memories. Future research should examine the extent to which emotional memory intensity moderates the effects of self-distancing.
Therefore, individuals in the self-distanced condition reported strong emotional reactions but showed no physiological response to trauma memory analysis. These findings have potentially important implications for PTSD treatment. Imaginal exposure to trauma memories is a key component of evidence-based treatments for PTSD (Foa & Rothbaum, 1998). Although imaginal exposure differs from our experimental manipulation in important ways, our findings offer the possibility that self-distancing could be tested as a complement to currently used evidence-based practices. Specifically, a client who has difficulty tolerating exposure to his/her trauma memories from the immersed perspective due to extreme physiological reactions might benefit from a graded approach, first visualizing the trauma from the distanced perspective followed by the immersed perspective once s/he is able to better tolerate the exposures. However, it will be important to test this use of the distanced perspective in the context of treatment to determine its effects before implementing this technique. Given evidence that spontaneous self-distancing is associated with increased PTSD risk (Kenny et al., 2009), it is possible that this technique might be harmful rather than helpful in the context of therapy.
Additionally, exposure-based treatments typically rely upon patients’ self-reported distress as the sole measure in determining whether or not a fear response has been elicited, and this self-reported distress is used to make important clinical decisions, such as when to end an exposure session. Our findings suggest that self-reported and physiological arousal do not always correspond among individuals with PTSD (see also Marx et al., 2012). Importantly, our results suggest that patients who self distance while engaging in imaginal exposure may report high levels of subjective arousal without experiencing physiological arousal. Future research examining exposure-based therapies for PTSD would benefit from including both physiological and self-report measures of arousal to examine whether physiological measures might offer additional clinically relevant information.
It is important to note this study's limitations. First, we did not include a comparison group of individuals who were allowed to choose their visual perspective (i.e., a group that was not given explicit instructions regarding which visual perspective to use). Thus, this study cannot address questions regarding what visual perspective individuals with PTSD are most likely to use when imagining their traumatic event(s). We also did not include a group of individuals without PTSD and therefore it is not clear whether our results would extend to individuals who experienced traumatic events but did not develop PTSD. Our sample was also predominantly male and restricted to United States military Veterans. Thus, it will be important to replicate these findings in women and in other populations.
Further work is needed before our results can be readily translated into clinical practice. Consistent with prior self-distancing research (e.g., Kross et al., 2005), we examined the effects of self-distancing from trauma memories over a period of time that is considerably shorter than the typical duration of imaginal exposure in PTSD treatment. Future research should examine the effects of self-distancing from trauma memories when memories are analyzed for a longer period of time. Importantly, our findings also cannot speak to the long-term consequences of self-distancing's effect on immediate physiological reactivity. One possibility is that the short-term decrease in physiological reactivity reflects an adaptive emotion regulatory function that is beneficial in the long term, as conceptualized by Kross and colleagues (2005). Another possibility, however, is that self-distancing reflects a maladaptive way to avoid one's physiological reactions to trauma memories (Foa & Rothbaum, 1998; Kenny et al., 2009; McIsaac & Eich, 2004). According to this view, self-distancing reduces physiological reactivity in the short-term, but this temporary relief represents a means of avoiding uncomfortable physical sensations. Longitudinal research examining the long-term effects of self-distancing when analyzing trauma memories is needed to determine whether this technique represents an adaptive form of emotion regulation or maladaptive form of avoidance.
Finally, future research should examine the extent to which the effects of self-distancing are specific to imagery-based thought. Recent work has suggested that verbal forms of self-distancing (e.g., referring to oneself in the third person) have similar effects as visual self-distancing (Kross et al., 2014). Thus, research addressing the possible effects of verbal self-distancing among individuals with PTSD is another important topic for future research.
This study represents the first to examine whether the short-term benefits of self-distancing while “asking why” extend to trauma memories among individuals with PTSD. We found that self-distancing protects against physiological but not subjective emotional reactivity to trauma memory analysis among Veterans with PTSD. Strengths include the experimental design, the use of a carefully diagnosed clinical sample of individuals with PTSD, and the inclusion of physiological arousal as well as subjective emotional response. Our findings suggest that the short-term benefits of self-distancing on subjective emotional reactivity, previously found with other emotional memories, may not extend to trauma memories, at least among individuals with PTSD. However, self-distancing during trauma memory analysis did protect against physiological reactivity among individuals with PTSD, indicating that self-distancing has at least a short-term benefit even among this highly distressed group.
Acknowledgements
This project and Blair E. Wisco were supported by Award Number T32MH019836 from the National Institute of Mental Health, awarded to principal investigator Terence M. Keane. The content is solely the responsibility of the authors and does not represent the official views of the National Institute of Mental Health. The authors would like to thank Michelle Bovin and Paola Rodriguez, who served as reliability coders.
Footnotes
Separate sensitivity analyses were run statistically controlling for variables that might affect the results. No results changed if CAPS score, memory age, or the manipulation check were entered into the models as covariates.
Two participants did not follow the PANAS instructions and could not be included in the analysis of negative affect (NA). Exploratory analyses examining the NA subscales (fear, hostility, guilt, and sadness) revealed a similar pattern to the overall NA scale, with no significant interactions between time and condition emerging, Fs < 2, ps > .25, ηp2s < .04. One participant did not complete the emotional re-experiencing questions and could not be included in the emotional re-experiencing analysis.
Emotional re-experiencing scores in our sample were Mdistanced = 10.13 (SD = 3.52), Mimmersed = 10.61 (SD = 2.69), compared to Mdistanced = 3.90 (SD = 1.52), Mimmersed = 4.58 (SD = 1.46; Kross et al., 2005). Kross et al (2005) also included the PANAS NA scale, which they measured in terms of mean item score (rather than total score). Using this metric, our participants reported NA of M = 2.60 (SD = 1.01), compared to M = 1.76 (SD = 0.68; Kross et al., 2005).
References
- American Psychiatric Association Diagnostic and statistical manual of mental disorders. (4th ed., text rev.) 2000 doi:10.1176/appi.books.9780890423349. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Ayduk O, Kross E. Enhancing the pace of recovery: Self distanced analysis of negative experiences reduces blood pressure reactivity. Psychological Science. 2008;19:229–231. doi: 10.1111/j.1467-9280.2008.02073.x. doi: 10.1111/j.1467-9280.2008.02073.x. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A. Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy. 2008;46:5–27. doi: 10.1016/j.brat.2007.10.003. doi: 10.1016/j.brat.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BA. Treating the trauma of rape: Cognitive behavioral therapy for PTSD. Guilford Press; New York: 1998. [Google Scholar]
- Gruber J, Harvey AG, Johnson SL. Reflective and ruminative processing of positive emotional memories in bipolar disorder and healthy controls. Behaviour Research and Therapy. 2009;47:697–704. doi: 10.1016/j.brat.2009.05.005. doi: 10.1016/j.brat.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaycox LH, Foa EB, Morral AR. Influence of Emotional Engagement and Habituation on Exposure Therapy for PTSD. Journal of Consulting and Clinical Psychology. 1998;66(1):185–192. doi: 10.1037//0022-006x.66.1.185. doi: 10.1037/0022 006X.66.1.185. [DOI] [PubMed] [Google Scholar]
- Kenny LM, Bryant RA. Keeping memories at an arm's length: Vantage point of trauma memories. Behaviour Research and Therapy. 2007;45:1915–1920. doi: 10.1016/j.brat.2006.09.004. doi: 10.1016/j.brat.2006.09.004. [DOI] [PubMed] [Google Scholar]
- Kenny LM, Bryant RA, Silove D, Creamer M, O'Donnell M, McFarlane AC. Distant memories: A prospective study of vantage point of trauma memories. Psychological Science. 2009;20:1049–1052. doi: 10.1111/j.1467-9280.2009.02393.x. doi: 10.1111/j.1467 9280.2009.02393.x. [DOI] [PubMed] [Google Scholar]
- Kross E, Ayduk O. Facilitating adaptive emotional analysis: Distinguishing distanced-analysis of depressive experiences from immersed analysis and distraction. Personality and Social Psychology Bulletin. 2008;34:924–938. doi: 10.1177/0146167208315938. [DOI] [PubMed] [Google Scholar]
- Kross E, Ayduk O. Boundary conditions and buffering effects: Does depressive symptomology moderate the effectiveness of distanced-analysis for facilitating adaptive self reflection? Journal of Research in Personality. 2009;43:923–92. doi: 10.1016/j.jrp.2009.04.004. doi:10.1016/j.jrp.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kross E, Ayduk O, Mischel W. When asking “why” does not hurt: Distinguishing rumination from reflective processing of negative emotions. Psychological Science. 2005;16:709–715. doi: 10.1111/j.1467-9280.2005.01600.x. doi: 10.1111/j. 1467 9280.2005.01600.x. [DOI] [PubMed] [Google Scholar]
- Kross E, Gard D, Deldin P, Clifton J, Ayduk O. “Asking why” from a distance: Its cognitive and emotional consequences for people with major depressive disorder. Journal of Abnormal Psychology. 2012;121:559–569. doi: 10.1037/a0028808. doi: 10.1037/a0028808. [DOI] [PubMed] [Google Scholar]
- Kross E, Bruehlman-Senecal E, Park J, Burson A, Dougherty A, Shablack H, Ayduk O. Self-talk as a regulatory mechanism: How you do it matters. Journal of Personality and Social Psychology. 2014;106(2):304. doi: 10.1037/a0035173. doi: 10.1037/a0035173. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, Cuthbert BN. Motivated attention: Affect, activation and action. In: Lang PJ, Simons RF, Balaban MT, editors. Attention and orienting: Sensory and motivational processes. Erlbaum; Hillsdale, NJ: 1997. pp. 97–135. [Google Scholar]
- Marx BP, Bovin MJ, Suvak MK, Monson CM, Sloan DM, Fredman SJ, Humphreys KL, Kaloupek DG, Keane TM. Concordance between physiological arousal and subjective distress among Vietnam combat veterans undergoing challenge testing for PTSD. Journal of Traumatic Stress. 2012:416–425. doi: 10.1002/jts.21729. doi: 10.1002/jts.21729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIsaac HK, Eich E. Vantage point in episodic memory. Psychonomic bulletin & review. 2002;9(1):146–150. doi: 10.3758/bf03196271. [DOI] [PubMed] [Google Scholar]
- McIsaac HK, Eich E. Vantage point in traumatic memory. Psychological Science. 2004;15(4):248–253. doi: 10.1111/j.0956-7976.2004.00660.x. doi: 10.1111/j.0956-7976.2004.00660.x. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives in Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. doi: 10.1111/j. 1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Watson E, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule-Expanded Form. Iowa Research Online Department of Psychology Publications; 1999. [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Wisco BE, Nolen-Hoeksema S. Effect of visual perspective on memory and interpretation in dysphoria. Behaviour Research and Therapy. 2011;49:406–412. doi: 10.1016/j.brat.2011.03.012. doi: 10.1016/j.brat.2011.03.012. [DOI] [PubMed] [Google Scholar]