Abstract
Background/Objective
Coincident with economic development, China has experienced a dramatic transition from undernutrition to overweight/obesity over the last few decades. We aimed to explore the burden of under- and overnutrition and nutrient adequacy among 2-12 y-old Chinese children.
Methods
We included anthropometry, dietary intake and biomarkers from 2-12-y-olds who participated in the 2009-2011 China Health and Nutrition Survey (n=1,191 in 2009; n=1,648 in 2011). Dietary intakes were compared with the 2013 Chinese Dietary Recommended Intakes.
Results
In 2011, approximately 19% of 2-6 y-old children were underweight, 4% were stunted, 10% were overweight and 12% were obese. Among 7-12 y-old children, stunting was almost 0% whereas approximately 21% were underweight, 13% were overweight and 6% were obese in 2011. Overweight and obesity were more prevalent among children from urban areas and higher income households. In particular, 2-6 y-old children from urban areas and higher income households experienced the highest increase in obesity from 2009 to 2011 (P<0.05). Children from urban areas and higher income households had overall higher intakes of total daily energy and most macro- and micronutrients (P<0.05). However, a significant proportion of children did not meet the recommendations for important micronutrients.
Conclusions
Underweight and stunting currently coexist with overweight and obesity among Chinese children <12 y-old. We found critical disparities in the prevalence of under- and overweight/obesity, as well as in nutrient intakes and dietary adequacies between children from different incomes, revealing that the burden of childhood under- and overnutrition may constitute a public health concern in modern China.
Keywords: undernutrition, overweight, children, China, nutrients
INTRODUCTION
The coexistence of under- and overnutrition has been linked to a process of rapid economic development, urbanization and overall modernization in low- and middle-income countries1-3. In particular, China has experienced a dramatic transition from a high prevalence of underweight to increasing overweight and obesity over the past few decades4-6. Traditional diets and healthier lifestyles have been progressively displaced by westernized eating patterns and sedentary lifestyles7-10.
For Chinese children, this transition has had a positive impact as nutritional status has improved while rates of underweight and stunting (low height for age) have been reduced5, 11, 12. In parallel, the Chinese pediatric population has experienced a greater relative increase in overweight compared to the adult population, with newer generations experiencing higher body mass indexes (BMI) at earlier ages than ever before12-14. However, a broad heterogeneity in weight change has been documented across China, providing a unique model for the dual burden of under- and overnutrition with a wide variation by age, gender, area of residence and socioeconomic status (SES)6, 15, 16.
The dual burden of under- and overnutrition has more recently been termed the triple burden when the focus is not only on under- and overnutrition but also on nutrient deficiencies17, 18. Under- and overnutrition can coexist within a country, a community, a household or an individual11, 19, 20. Within an individual, overweight or obesity might co-occur with micronutrient deficiencies (i.e. anemia) or stunting. To date, there is a lack of current data on this topic in the Chinese pediatric population. In addition, exploration of SES disparities is needed given the important differences in economic and social development between urban and rural areas across China21.
In the present study, we aimed to explore the double burden of under- and overnutrition (i.e. stunting, underweight, overweight and obesity) among Chinese children 2-12y old from the 2009-2011 China Health and Nutrition Survey. We also examined dietary intakes and nutrient adequacies across different SES categories, gender, age and weight status. We selected key macro- and micronutrients as well as biochemical parameters that are related to growth and overall health22. Our study focused on the health and nutritional status of Chinese children and provided a valuable analysis across age, gender and key SES groups for which nutrition-related interventions might be targeted to address malnutrition while avoiding obesity and its related complications.
METHODS
Study population: the China Health and Nutrition Survey (CHNS) 2009-2011
The CHNS is the only large-scale on-going longitudinal household-based cohort in China16, 21. The CHNS uses a multi-stage random cluster process to select individuals from 228 communities in 9 provinces and represents a wide range of economic and demographic variation. Since the baseline survey in 1989, the CHNS has only collected blood samples in 2009. In 2011, three megacities (Beijing, Shanghai and Chongqing) were sampled and added to the CHNS to increase representation of the larger developed cities.
Information on dietary intake data, anthropometric measurements and detailed individual, household and community sociodemograpic data was collected by trained interviewers at each home visit spanning 3 days21. The sample analyzed in this study includes children aged 2-12 from 2009 (n=1,191) and 2011 (n=1,648) with available anthropometric data. Since the CHNS is a longitudinal cohort, some children from the sample of 2009 were assessed again in 2011. For the purpose of our analyses, we treated each year as cross-sectional. Survey instruments, protocols and informed consents were approved by the institutional review committee of the University of North Carolina at Chapel Hill, the National Institute for Nutrition and Health Food Safety, the Chinese Center for Disease Control and Prevention, and the China-Japan Friendship Hospital, Ministry of Health.
Anthropometric measurements
Height was measured in bare-footed individuals to the nearest 0.2 cm using a portable Seca stadiometer (Seca North America, Chino, CA, USA). Weight was measured in light clothing and without shoes to the nearest 0.1 kg using a calibrated beam scale and waist circumference (WC) was measured using a Seca tape measure.
Classification of children based on their anthropometric measurements was determined based on the WHO growth standards for 0-5-y-olds and the WHO growth reference for 5-19-yolds23-25. Stunting was defined as <2SD of height-for-age z-scores. Underweight, normal weight, overweight and obesity were classified using the International Obesity Task Force international BMI cut points by age and gender 26, with cut-points that correspond to an adult BMI of 18.5 (underweight), 25 (overweight) and 30 (obesity).
Dietary intake measurements
For each individual, dietary intake was collected by trained interviewers using 3 consecutive 24-h recalls. Supplemental information was supplied by a daily household food inventory and by meeting with the household member that handled the food preparation to learn the exact details of each dish so recipes were individualized27, 28. In addition, trained interviewers used food models and pictures to record the type of food, amount, meal-time and place of consumption of all foods consumed on the previous day. All food consumed at home or away from home was reported by children ≥12 y. For children <12y of age, the mother or child's caregiver who handled food preparation at home or feeding outside the home was used as a proxy for the child's food consumption8. The present analysis used the 3-day averages of energy and nutrient intakes.
To capture nutrient intake, the latest Chinese food composition table was used, which includes approximately 2,500 foods29. For this study, we reported intake of total daily energy and macronutrients, including protein, total fat, carbohydrates and fiber. We also selected a few critical micronutrients for which the response to deficiencies compromises growth: a type I nutrient deficiency leads to a depletion in body stores and a reduced concentration in tissues with clinical signs related to metabolic functions dependent on the nutrient (i.e. thiamin, calcium, vitamin D, iron). For type II nutrients, because there are no stores other than the normal tissue, in case of a deficiency the body tends to preserve plasma and tissue levels, which results in a decreased growth rate and impaired repair and immune function (i.e. zinc, total protein, energy)22.
The 2013 Chinese Dietary Reference Intakes (DRIs) were used to evaluate nutrient adequacy and determine whether diets provided enough nutrients to ensure adequate growth without compromising health30. To investigate the prevalence of inadequate or excessive intakes, the proportion of participants above and below defined Chinese DRI cutoff values was calculated (Supplemental table 1)31.
Biochemical assessments
Fasting blood samples were obtained from individuals ≥7 years who participated in CHNS 2009 and visited a neighborhood clinic. For the present study, we selected three biomarkers of anemia including ferritin, transferrin and hemoglobin; and total serum protein.
Socioeconomic variables
At each home visit, information on demographic characteristics was collected for each individual (i.e. age, gender, area of residence) or head of the household (i.e. income, education) (Supplemental table 2). Area of residence was categorized as urban or rural based on population density, calculated as the total population of the community divided by the total community area obtained from official records. We used inflation-adjusted family income, which was calculated as the sum of self-reported individual incomes of all earners in the household, and was divided into tertiles for a proxy of lower, medium and higher income.
Statistical analyses
Statistical analyses were carried out using Stata (Release 13.0, Stata Corp., College Station, TX, USA). Age was used to classify children into two age groups: 2-6 y and 7-12 y. For each survey year (2009 and 2011), results are presented as crude prevalences or population means and standard error (SE). Means and prevalences were calculated within each age stratum and within age group and area of residence, gender, income and weight status. Differences across time (2009 to 2011) as well as differences between groups of urban/rural, gender, income and weight status were tested using two-tailed Student's t test for means or X2 test for prevalence data. A P value of 0.05 was set to denote statistical significance.
RESULTS
Prevalence of under- and overnutrition among Chinese children in urban and rural areas
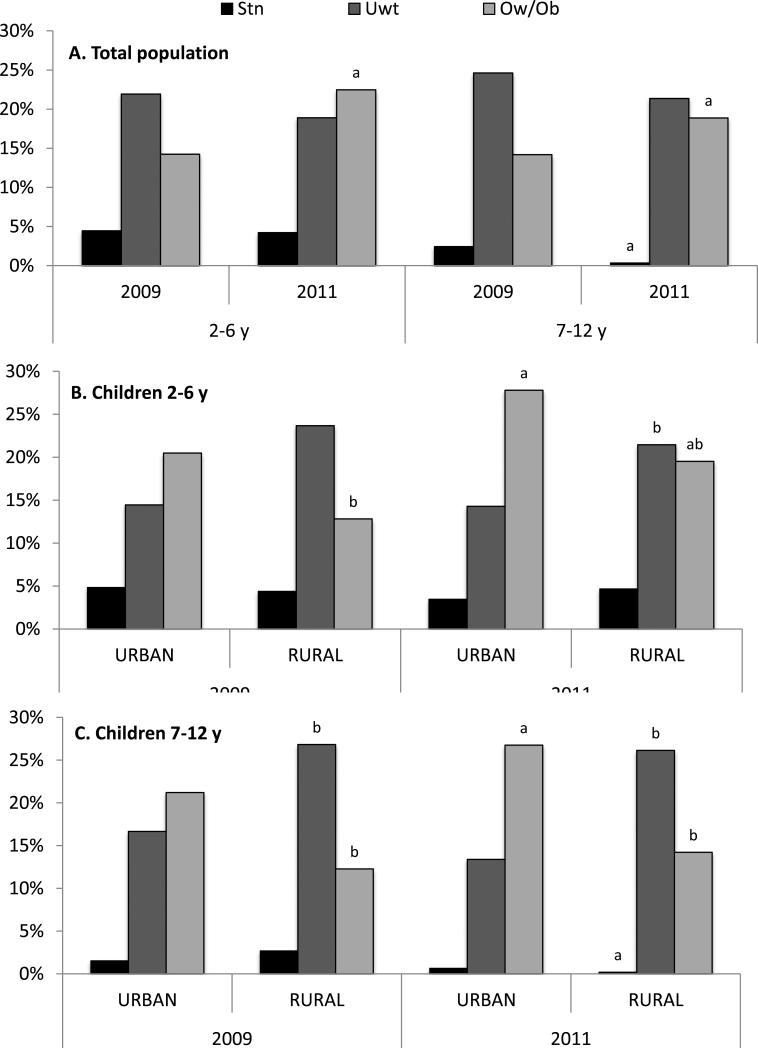
Underweight was prevalent in 2009 (21.9%) and 2011 (18.9%) among children aged 2-6y, while stunting was 4.5% in 2009 and 4.2% in 2011. In 2009, 7.7% and 6.6% of children 2-6y were overweight and obese, respectively; while 10.1% and 12.4% of them were overweight and obese, respectively in 2011 (Table 1, Figure 1). Among children 7-12y, stunting was 2.4% in 2009 but 0.4% in 2011, whereas 24.6% were underweight in 2009 and 21.4% in 2011. In 2009, 11.3% and 2.9% of children 7-12y were overweight and obese, respectively; while in 2011, 12.6% and 6.3% of them were overweight and obese, respectively. Wasting was nonexistent in both age groups (unreported results). Around 3.2% of children 2-6-y and 0.4% of 7-12-y were stunted and overweight in 2011. Since 2009, the mean BMI increased significantly in both age groups, and there was a two-fold increase in obesity rates among the younger children.
Table 1.
Anthropometric parameters and prevalence (%) of under- and over-nutrition by age group and area of residence among children 2-12 y who participated in the China Health and Nutrition Survey in 2009 and 2011.
| 2-6 y |
7-12 y |
|||||
|---|---|---|---|---|---|---|
| YEAR 2009 | Total n=528 | Urban n=102 | Rural n=426 | Total n=663 | Urban n=143 | Rural n=520 |
| WC (cm) | - | - | - | 59.4±9.2 | 60.5±10.0 | 59.1±8.9 |
| BMI (kg/m2) | 15.8±2.4 | 16.1±2.3 | 15.7±2.5 | 16.7±3.1 | 17.6±3.6 | 16.5±2.9 a |
| Underweight | 21.9 | 14.5 | 23.7 | 24.6 | 16.7 | 26.8 a |
| Normal Weight | 63.8 | 65.1 | 63.5 | 61.2 | 62.1 | 60.9 |
| Overweight | 7.7 | 15.7 | 5.8 a | 11.3 | 15.2 | 10.2 |
| Obesity | 6.6 | 4.8 | 7.0 | 2.9 | 6.1 | 2.1 a |
| Stunting | 4.5 | 4.8 | 4.4 | 2.4 | 1.5 | 2.7 |
| Ow/Ob & Stunting | 2.7 | 2.4 | 2.8 | 0.5 | 1.5 | 0.2 |
| YEAR 2011 | Total n=772 | Urban n=281 | Rural n=491 | Total n=876 | Urban n=327 | Rural n=549 |
|---|---|---|---|---|---|---|
| WC (cm) | - | - | - | 60.1±10.5 | 62.5±11.7 | 58.7±9.5 a |
| BMI (kg/m2) | 17.0±4.9 b | 18.0±6.0 b | 16.5±4.0 ab | 17.3±3.7 b | 18.2±4.1 | 16.7±3.3 a |
| Underweight | 18.9 | 14.3 | 21.5 a | 21.4 | 13.4 | 26.1 a |
| Normal Weight | 58.6 | 57.9 | 59.0 | 59.7 | 59.9 | 59.7 |
| Overweight | 10.1 | 11.2 | 9.4 b | 12.6 | 18.8 | 8.9 a |
| Obesity | 12.4 b | 16.6 b | 10.1 a | 6.3 b | 8.0 | 5.3 b |
| Stunting | 4.2 | 3.5 | 4.7 | 0.4 b | 0.6 | 0.2 b |
| Ow/Ob & Stunting | 3.2 | 3.1 | 3.2 | 0.4 | 0.6 | 0.2 |
Estimates presented as mean ± SE or prevalence (%). Underweight, normal weight, overweight and obesity classified using the International Obesity Task Force international BMI cut points by age and sex; the cut points correspond to an adult BMI of 18.5 (underweight), 25 (overweight) or 30 (obesity). Stunting defined as <2SD of height-for-age z-score using the WHO Child Growth Standards.
Significantly different between urban vs. rural, Student's t test for means or Chi square test for proportions, P<0.05.
Significantly different between 2009 vs. 2011 within each age or urban/rural group, Student's t test for means or Chi square test for proportions, P<0.05.
Figure 1.
Prevalence (%) of under- and over-nutrition by age group (A) and area of residence (B-C) among children 2-12 y who participated in the China Health and Nutrition Survey in 2009 and 2011.
a Significantly different between 2009 vs. 2011 within each age or urban/rural group, Chi square test, P<0.05.
b Significantly different between urban vs. rural, Chi square test, P<0.05.
Compared to children from rural areas in 2011, children from urban areas had a lower prevalence of underweight (14.3% vs. 21.5% among 2-6-y-olds; 13.4% vs. 26.1% among 7-12-yolds, P<0.05) but a higher prevalence of overweight (18.8% vs. 8.9% among 7-12-y-olds, P<0.05) and obesity (16.6% vs. 10.1% among 2-6-y-olds, P<0.05). From 2009 to 2011, obesity experienced almost a 4-fold increase among 2-6-y-olds from urban areas. Among children from rural areas, overweight increased among 2-6-y-olds whereas obesity increased among 7-12-y-olds over the same period.
Gender and income differences in the prevalence of under- and overnutrition
In 2011, boys had significantly higher mean BMI compared to girls of both age groups and the prevalence of underweight was significantly higher among 7-12-y-old girls (24.4% vs. 18.5% in 2011, P<0.05) (Table 2). Obesity increased significantly in boys from 2009 to 2011, with almost a 3-fold increase among 2-6-y-old boys (5.0% to 13.8%, P<0.05) and a 2-fold increase among 7-12-y-old boys (3.6% to 7.6%, P<0.05).
Table 2.
Anthropometric parameters and prevalence (%) of under- and over-nutrition by age group, gender and poverty level among children 2-12 y who participated in the China Health and Nutrition Survey in 2009 and 2011.
| 2-6 y |
7-12 y |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| YEAR 2009 | Boys n=289 |
Girls n=239 |
Lower income n=173 |
Middle income n=184 |
Higher income n=167 |
Boys n=368 |
Girls n=295 |
Lower income n=220 |
Middle income n=209 |
Higher income n=225 |
| WC (cm) | - | - | - | - | - | 60.3±9.5 | 58.2±8.7a | 57.6±8.5 | 58.8±8.9 | 61.4±9.8b |
| BMI (kg/m2) | 15.9±2.4 | 15.7±2.5 | 16.1±2.9 | 15.6±2.3 | 15.8±2.0 | 16.9±3.1 | 16.5±3.0 | 16.5±3.1 | 16.3±2.8 | 17.3±3.3b |
| Underweight | 21.1 | 23.0 | 19.9 | 27.5 | 17.5 | 21.3 | 28.7a | 29.6 | 27.7 | 17.8b |
| Normal Weight | 67.4 | 59.5 | 63.6 | 61.4 | 67.2 | 63.9 | 57.8 | 59.3 | 60.5 | 62.9 |
| Overweight | 6.6 | 9.0 | 7.3 | 5.2 | 10.9 | 11.2 | 11.3 | 7.5 | 10.3 | 15.5b |
| Obesity | 5.0 | 8.5 | 9.3 | 5.9 | 4.4 | 3.6 | 2.2 | 3.5 | 1.5 | 3.8 |
| Stunting | 4.1 | 4.9 | 5.3 | 2.5 | 5.8 | 0.9 | 4.3a | 5.0 | 1.5 | 0.9b |
| Ow/Ob & Stunting | 2.9 | 2.5 | 3.3 | 1.3 | 3.6 | 0.3 | 0.7 | 1.5 | 0.0 | 0.0 |
| YEAR 2011 | Boys n=412 |
Girls n=360 |
Lower income n=246 |
Middle income n=253 |
Higher income n=259 |
Boys n=454 |
Girls n=422 |
Lower income n=292 |
Middle income n=284 |
Higher income n=278 |
|---|---|---|---|---|---|---|---|---|---|---|
| WC (cm) | - | - | - | - | - | 61.1±10.5 | 59.1±10.4a | 58.5±9.0 | 59.4±9.6 | 62.6±12.1b |
| BMI (kg/m2) | 17.5±5.6c | 16.5±3.8ac | 16.8±4.4 | 16.5±4.2c | 17.5±5.3c | 17.6±3.7c | 16.9±3.6a | 16.7±3.7 | 17.0±3.2 | 18.0±3.8b |
| Underweight | 19.2 | 18.6 | 18.8 | 21.0 | 17.3 | 18.5 | 24.4a | 29.7 | 17.9bc | 16.8b |
| Normal Weight | 58.6c | 58.7 | 57.8 | 62.6 | 55.2c | 60.2 | 59.3 | 54.1 | 66.8b | 58.4 |
| Overweight | 8.4 | 12.0 | 13.5 | 7.0 | 10.1 | 13.7 | 11.5 | 10.0 | 10.4 | 17.9b |
| Obesity | 13.8c | 10.8 | 9.9 | 9.5 | 17.3bc | 7.6c | 4.9 | 6.1 | 4.9 | 6.9 |
| Stunting | 5.3 | 3.0 | 5.7 | 2.9 | 3.6 | 0.5 | 0.2c | 0.4bc | 0.0 | 0.4 |
| Ow/Ob & Stunting | 4.3 | 1.8 | 3.6 | 1.6 | 3.6 | 0.5 | 0.2 | 0.4 | 0.0 | 0.4 |
Estimates presented as mean ± SE or prevalence (%). Underweight, normal weight, overweight and obesity classified using the International Obesity Task Force international BMI cut points by age and sex; the cut points correspond to an adult BMI of 18.5 (underweight), 25 (overweight) or 30 (obesity). Stunting defined as <2SD of height-for-age z-score using the WHO Child Growth Standards.
Significantly different between boys vs. girls, Student's t test for means or Chi square test for proportions, P<0.05.
Significantly different between lower vs. middle or higher income, Student's t test for means or Chi square test for proportions, P<0.05.
Significantly different between 2009 vs. 2011 within each gender or income group, Student's t test for means or Chi square test for proportions, P<0.05.
Children aged 7-12 y from higher income households had higher values of WC and BMI compared to children from lower income households. In 2011, obesity was more prevalent among 2-6-y-olds from higher income households compared to lower income (17.3% vs. 9.9%, P<0.05) whereas overweight but not obesity was more prevalent among 7-12-y-olds from higher income households compared to lower income (17.9% vs. 10.0%, P<0.05). Since 2009, the prevalence of obesity experienced approximately a 4-fold increase among higher income children aged 2-6 y (4.4% to 17.3%, P<0.05). Stunting decreased from 2009 to 2011 among 7-12 y-old girls (4.3% to 0.2%, P<0.05) and lower income children (5.0% to 0.4%, P<0.05).
Dietary intakes and nutritional status of Chinese children
We reported age-stratified mean energy and nutrient intakes in 2011 and biochemical markers in 2009 (Table 3, Supplemental tables 3-4). Children from urban areas had significantly higher intakes of total daily energy, protein, carbohydrates (only among 7-12-y-olds), fat, thiamin (only among 2-6-y-olds), calcium, vitamin D, iron (only among 2-6-y-olds) and zinc (Table 3). Boys and higher income children had significantly higher intakes of total energy and most macro- and micronutrients compared to girls or lower income children, respectively (Supplemental table 3). Compared to normal weight children, those with overweight or obesity had a higher intake of total daily energy, protein, and higher plasma concentrations of transferrin and total protein (Supplemental Table 4).
Table 3.
Daily intake of energy, macro- and micronutrients in 2011 and concentration of selected biochemical parameters in 2009 by age group and gender among children 2-12 y who participated in the China Health and Nutrition Survey 2009-2011.
| 2-6 y |
7-12 y |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Urban | Rural | Total | Urban | Rural | |||||||
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | |
| Energy (Kcal) | 1105.7 | 15.8 | 1186.1 | 28.1 | 1060.1 | 18.7a | 1465.0 | 17.7 | 1517.6 | 28.9 | 1433.4 | 22.3a |
| Macronutrients (g) | ||||||||||||
| Protein | 38.2 | 0.6 | 43.8 | 1.1 | 35.1 | 0.7a | 51.1 | 0.7 | 56.7 | 1.1 | 47.7 | 0.9a |
| Carbohydrates | 145.8 | 2.3 | 150.9 | 4.0 | 142.8 | 2.7 | 191.7 | 2.8 | 184.5 | 4.3 | 195.9 | 3.6a |
| Fat | 41.0 | 0.8 | 45.2 | 1.3 | 38.7 | 0.9a | 54.8 | 0.9 | 61.3 | 1.6 | 50.9 | 1.1a |
| Fiber | 6.4 | 0.2 | 6.3 | 0.2 | 6.4 | 0.2 | 9.4 | 0.2 | 9.4 | 0.3 | 9.4 | 0.3 |
| Micronutrients | ||||||||||||
| Thiamin (mg) | 0.5 | 0.0 | 0.6 | 0.0 | 0.5 | 0.0a | 0.7 | 0.0 | 0.7 | 0.0 | 0.7 | 0.0 |
| Calcium (mg) | 315.8 | 10.9 | 420.4 | 23.1 | 256.4 | 10.0a | 337.1 | 7.3 | 405.6 | 14.4 | 295.9 | 7.4a |
| Vitamin D (μg) | 3.3 | 0.2 | 4.2 | 0.3 | 2.8 | 0.2a | 3.7 | 0.2 | 4.5 | 0.2 | 3.3 | 0.2a |
| Iron (mg) | 11.0 | 0.2 | 11.8 | 0.4 | 10.6 | 0.3a | 15.2 | 0.3 | 15.9 | 0.4 | 14.8 | 0.4 |
| Zinc (mg) | 5.9 | 0.1 | 6.5 | 0.2 | 5.5 | 0.1a | 7.8 | 0.1 | 8.3 | 0.2 | 7.6 | 0.1a |
| Biochemical markers | ||||||||||||
| Ferritin (ng/mL) | - | - | - | - | - | - | 49.9 | 42.6 | 45.5 | 22.9 | 51.0 | 46.2 |
| Transferrin (ng/mL) | - | - | - | - | - | - | 296.1 | 51.7 | 296.0 | 42.6 | 296.1 | 53.9 |
| Hemoglobin (g/dL) | - | - | - | - | - | - | 13.4 | 1.5 | 13.6 | 1.8 | 13.4 | 1.5 |
| Total Protein (g/dL) | - | - | - | - | - | - | 7.6 | 0.5 | 7.6 | 0.5 | 7.6 | 0.5 |
Estimates presented as mean ± SE. Dietary intake was collected in 2011 for the entire sample of children 2-12y; biochemical parameters were collected in 2009 for children 7-12y.
Significantly different between urban vs. rural, Student's t test, P<0.05.
Dietary adequacy was evaluated against the 2013 Chinese DRIs (Tables 4-5). A high proportion of children in both age groups did not meet the recommendations for dietary fiber, thiamin, calcium and vitamin D (Table 4). In general, a higher proportion of children from rural areas, girls and lower income children had inadequate intakes of selected macro- and micronutrients (Table 5). Compared to normal weight children, a lower proportion of overweight or obese children had inadequate intakes of calcium (among 2-6-y-olds); and protein and zinc (among 7-12-y-olds) (Supplemental table 5). Among children 7-12-y old, the prevalence of anemia according to plasma concentrations of hemoglobin was below 3% and almost 0% only among children from urban areas (unreported results).
Table 4.
Prevalence (%) of inadequate or excessive intakes of energy, macro- and micronutrients by age group and area of residence among children 2-12 y who participated in the China Health and Nutrition Survey 2011.
| 2-6 y |
7-12 y |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Urban | Rural | Total | Urban | Rural | |||||||
| % <EAR | % >UL | % <EAR | % >UL | % <EAR | % >UL | % <EAR | % >UL | % <EAR | % >UL | % <EAR | % >UL | |
| Macronutrients | ||||||||||||
| Protein | 20.1 | - | 10.8 | - | 25.3a | - | 29.0 | - | 19.3 | - | 34.9a | - |
| Carbohydrates | 38.7 | - | 37.8 | - | 39.2 | - | 23.7 | - | 23.5 | - | 23.7 | - |
| Fiber | 98.0 | - | 98.9 | - | 97.6 | - | 97.1 | - | 98.5 | - | 96.3 | - |
| Micronutrients | ||||||||||||
| Thiamin | 65.5 | - | 60.1 | - | 68.6a | - | 78.9 | - | 75.5 | - | 80.9 | - |
| Calcium | 88.7 | 1.3 | 81.3 | 2.9 | 92.9a | 0.4a | 97.8 | 0.1 | 96.9 | 0.3 | 98.3 | <1 |
| Vitamin D | 89.1 | 0.1 | 87.4 | 0.4 | 90.0 | <1 | 86.0 | 0.0 | 85.0 | <1 | 86.6 | <1 |
| Iron | 18.9 | 3.1 | 12.9 | 4.0 | 22.2a | 2.7 | 28.6 | 2.1 | 23.2 | 2.1 | 31.8a | 2.0 |
| Zinc | 27.1 | 7.8 | 20.1 | 11.5 | 31.0a | 5.7a | 36.3 | 0.5 | 30.3 | 0.3 | 39.9a | 0.6 |
* Estimates presented as %. Inadequate or excessive intakes were calculated using EARs and ULs from the 2013 Dietary Reference Intakes for the Chinese Population.
Significantly different between urban vs. rural, Chi square test, P<0.05.
Table 5.
Prevalence (%) of inadequate or excessive intakes of energy, macro- and micronutrients by age group, gender and income level among children 2-12 y who participated in the China Health and Nutrition Survey 2011.
| Boys | Girls | Lower income | Middle income | Higher income | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AGES 2-6 y | % <EAR | % >UL | % <EAR | % >UL | % <EAR | % >UL | % <EAR | % >UL | % <EAR | % >UL |
| Macronutrients | ||||||||||
| Protein | 19.3 | - | 20.9 | - | 28.8 | - | 20.8b | - | 10.5b | - |
| Carbohydrates | 34.2 | - | 43.7a | - | 43.2 | - | 37.2 | - | 35.7 | - |
| Fiber | 98.3 | - | 97.8 | - | 97.2 | - | 98.4 | - | 98.4 | - |
| Micronutrients | ||||||||||
| Thiamin | 59.2 | - | 72.7a | - | 68.4 | - | 67.2 | - | 60.9 | - |
| Calcium | 86.8 | 1.5 | 90.8 | 1.1 | 93.6 | <1 | 90.4 | 1.6 | 81.8b | 2.3 |
| Vitamin D | 87.3 | 0.2 | 91.1 | <1 | 94.4 | <1 | 90.0 | <1 | 83.3b | 0.4 |
| Iron | 15.9 | 3.2 | 22.3a | 3.1 | 28.0 | 2.0 | 16.0b | 2.0 | 12.4b | 5.4 |
| Zinc | 25.2 | 9.0 | 29.2 | 6.4 | 38.8 | 6.4 | 23.6b | 5.2 | 18.6b | 11.2 |
| AGES 7-12 y | ||||||||||
| Macronutrients | ||||||||||
| Protein | 24.2 | - | 34.3a | - | 35.5 | - | 30.8 | - | 20.4b | - |
| Carbohydrates | 17.5 | - | 30.2a | - | 24.6 | - | 26.6 | - | 18.5 | - |
| Fiber | 96.7 | - | 97.6 | - | 96.9 | - | 97.2 | - | 97.1 | - |
| Micronutrients | ||||||||||
| Thiamin | 77.4 | - | 80.5 | - | 80.5 | - | 80.4 | - | 75.3 | - |
| Calcium | 98.0 | <1 | 97.6 | 0.2 | 98.0 | 0.3 | 98.6 | <1 | 96.7 | <1 |
| Vitamin D | 84.9 | <1 | 87.1 | <1 | 88.4 | <1 | 88.5 | <1 | 80.4b | <1 |
| Iron | 21.1 | 2.4 | 36.7a | 1.7 | 32.8 | 2.7 | 30.1 | 0.3 | 22.2b | 3.3 |
| Zinc | 33.5 | 0.4 | 39.3 | 0.5 | 43.7 | 0.3 | 38.1 | <1 | 26.2b | 1.1 |
*Estimates presented as %. Inadequate or excessive intakes were calculated using EARs and ULs from the 2013 Dietary Reference Intakes for the Chinese Population.
Significantly different between boys vs. girls, Chi square test, P<0.05.
Significantly different between lower vs. middle or higher income, Chi square test, P<0.05.
DISCUSSION
The present study used anthropometric measures, dietary intake data and biochemical parameters to investigate the health and nutritional status of Chinese children over the latest surveyed periods. Our results show that the burden of undernutrition is progressively decreasing although underweight was still prevalent among all children in 2011. The prevalence of stunting was around 4% among the younger age group while wasting was nonexistent in our sample. In parallel, the prevalence of overweight or obesity experienced an important increase since 2009, especially among the younger age groups, among which overweight and obesity overpassed underweight over the period studied. Our results highlight the need for policies and interventions that target the population at risk of nutritional deficiencies while concurrently considering ways to address the increasingly widespread unhealthy dietary and lifestyle patterns to avoid the consequences of obesity and future related complications in China.
Another recent trend study has shown that overweight has been increasing steadily since 1991 among Chinese children and adolescents 2-18-y old, with younger cohorts entering adulthood at higher BMIs than in earlier generations6. Over the last decade (2000-2011), about 8.3% of children 2-6-y old and 11.5% of children 6-11-y old became overweight or obese. Conversely, stunting and underweight have been decreasing gradually among children 6-18-y old from 1991 to 2004, with a higher prevalence of stunting (16%) than underweight (9%) in 2004 5. In contrast, our study showed much smaller prevalences of stunting than underweight in 2009 and 2011 in our sample of children 2-12-y old. However, even though stunting might have been reduced as a result of general improvements in the nutritional status of Chinese children over the past decades32, some nutritional deficiencies might still remain at present to explain the high prevalence of child underweight, even among the higher SES groups.
Our study also documented critical disparities in the prevalence of under- and overweight or obesity between children from different SES backgrounds. As in previous studies5, 32, underweight and stunting was generally more prevalent among children from rural areas and lower incomes households; whereas overweight and obesity was more prevalent among children from urban areas and higher income households. Children 2-6-y old from urban areas and higher income households experienced the highest increase in obesity from 2009 to 2011, although overweight and obesity generally increased among children of all age, gender and SES categories. Previous research suggested that the burden of overweight and obesity might be shifting from the rich to the poor among the Chinese population5, 33-35. With economic development, the burden of obesity turns to lower SES groups as these individuals might be more susceptible to obesogenic environments36. According to Du et al., lower income households in China have experienced the greatest decline in cereal foods but more rapid increases in edible oil consumption33.
Our study highlights that important nutrient inadequacies still exist. Over the past two decades, dietary habits in China have progressively shifted from traditional dietary patterns and cooking methods to a higher intake of fat and animal-sourced foods8, 33, 37. The decreasing proportion of foods cooked in a healthy manner and the increasing intakes of fried food, snacks and away-from-home foods are important dietary behavior changes observed over this period8, 9. Increases in income and decreased prices of edible oils and animal foods partially explain these new patterns in China38, 39. For our study, we also used dietary intake and biochemical markers to investigate if there are nutritional inadequacies by key SES groups and by weight status. We showed several dietary inadequacies in all children in general with a higher proportion of rural children and lower income households not meeting the nutrient recommendations. Also, a high proportion of children across all ranges of body mass index still presented dietary inadequacies of these important nutrients. Following a decreasing trend in the prevalence of anemia showed by Chang et al.,40 we documented a very small prevalence of anemia in 2009 in our sample of 7-12-y old children. Our results revealed that, although childhood nutrition is improving in China, future efforts should focus on these critical nutrients in order to improve the health status of children across different ages and SES background.
Our results highlight the important inequalities in weight status and nutrient intakes among children from different SES, which contribute to expand the double burden of under- and overnutrition and dietary deficiencies between classes as economic and social development progresses in China. However, with urbanization and improved transportation, conservation and storage of foods, new dietary patterns may emerge even among rural areas and lower SES groups. As a consequence of this transition, a dual burden within individuals might be observed. For instance, our study showed that the prevalence of coexisting stunting and overweight was almost as high as the prevalence of stunting itself in 2011. Also, overweight and obese children had higher daily energy intakes than normal weight children but still a high proportion of them had inadequate intakes of selected macro- and micronutrients, such as thiamin, calcium and vitamin D. These patterns might result from an increased caloric intake from energy-dense nutrient poor foods, and, as the nutrition transition advances, healthier dietary and physical activity patterns may continue shifting and contributing to the existing burden of under- and overnutrition within individuals10, 36, 41.
The CHNS is the only longitudinal household-based cohort that captures a wide variability in urbanization and provides an important representation of economic development and health indicators across China16, 21. However, there are several limitations regarding the survey design and others intrinsic to the present study. One is the inability to obtain nationally representative results, although the sampling strategy followed by the CHNS might overcome this issue because the surveys were designed to capture a wide range of demographic and geographical areas, including urban and rural communities and neighborhoods and three mega cities in 201121. In addition, our study could only include one round of biomarker data for the older age group (7-12-y) in 2009. Dietary measurement in the CHNS involved methods that are time consuming, expensive, and require trained field workers. However, it has been shown that these efforts are beneficial as the combination of 24-hr recalls and detailed household food inventory improves the quality of individual dietary data compared to a single 24-hr recall8, 16, 28. Furthermore, although sample sizes of children were generally adequate, further stratification by age, gender and SES might have reduced representativeness and generalizability of our study results, especially for the estimates of prevalence of rare outcomes. Despite these limitations, the CHNS provides a unique framework to understand current dynamics in nutritional and health status over the last surveyed periods, when rapid changes in the social and economic landscape have occurred.
During its nutrition transition, China has progressively evolved from predominant stunting, to simultaneous underweight and overweight and finally to a higher prevalence of overweight and obesity. Among Chinese children <12y, underweight and stunting currently coexist with overweight and obesity. However, overweight and obesity exceeds underweight among children 2-6-y old and those from urban areas and higher income households. Overall trends from 2009 to 2011 have shown decreasing prevalence of underweight and stunting but increasing prevalence of overweight and obesity across all age, gender and income groups. Still, dietary inadequacies of critical nutrients remain across all age, gender and SES groups.
In conclusion, the present study documented critical disparities in the prevalence of under- and overweight and obesity as well as in dietary adequacy of selected nutrients, which reveal that a double burden currently coexists across different SES child groups in China. Our results have implications for policy and targeted interventions. On the one hand, changes in underweight and nutrient deficiencies are positive although some subpopulations of children from rural areas and lower income households will benefit from programs that aim to reduce critical deficiencies in relation to stunting and decreased growth. On the other hand, both rural and more developed areas are also moving towards increased energy intake and less traditional eating patterns, which highlight the need for national programs which help children from all SES groups to maximize the opportunities of the nutrition transition while avoiding the damaging consequences of unhealthy dietary and lifestyle patterns in modernizing China.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Dr. Phil Bardsley for programming assistance; Dr. Alison L. Eldridge for helpful revision, and Ms. Frances L. Dancy for administrative assistance.
FINANCIAL SUPPORT: Funding for this work was provided by the Nestlé Research Center, Lausanne, Switzerland.
ABBREVIATIONS
- AI
Adequate Intakes
- BMI
Body Mass Index
- CHNS
China Health and Nutrition Survey
- DRI
Dietary Reference Intakes
- EAR
Estimated Average Requirements
- EER
Estimated Energy Requirements
- SES
Socio-economic status
- UL
Tolerable Upper Intake Levels
- WC
Waist circumference
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest of any type with respect to this manuscript. The authors alone are responsible for the content and writing of the paper.
AUTHOR CONTRIBUTIONS
C.P., D.W., and B.M.P. designed research; C.P., D.W., S.D., B.Z., Z.W., C.S. and B.M.P. conducted research; C.P. analyzed data; C.P., D.W., and B.M.P. wrote the paper; C.P., D.W., S.D., B.Z., Z.W., C.S. and B.M.P. had primary responsibility for final content. All authors have read and approved the final manuscript.
SUPPLEMENTARY INFORMATION
Supplementary information is available at EJCN's website: Supplemental Tables 1-5
BIBLIOGRAPHY
- 1.Popkin BM. Urbanization, lifestyle changes and the nutrition transition. World Development. 1999;27(11):1905–1916. [Google Scholar]
- 2.Popkin BM. The nutrition transition and obesity in the developing world. The Journal of nutrition. 2001;131(3):871S–873S. doi: 10.1093/jn/131.3.871S. [DOI] [PubMed] [Google Scholar]
- 3.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutrition reviews. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adair LS, Gordon-Larsen P, Du SF, Zhang B, Popkin BM. The emergence of cardiometabolic disease risk in Chinese children and adults: consequences of changes in diet, physical activity and obesity. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2014;15(Suppl 1):49–59. doi: 10.1111/obr.12123. doi: 10.1111/obr.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dearth-Wesley T, Wang H, Popkin BM. Under- and overnutrition dynamics in Chinese children and adults (1991-2004). European journal of clinical nutrition. 2008;62(11):1302–1307. doi: 10.1038/sj.ejcn.1602853. doi: 10.1038/sj.ejcn.1602853. [DOI] [PubMed] [Google Scholar]
- 6.Gordon-Larsen P, Wang H, Popkin BM. Overweight dynamics in Chinese children and adults. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2014;15(Suppl 1):37–48. doi: 10.1111/obr.12121. doi: 10.1111/obr.12121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutrition reviews. 1997;55(2):31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 8.Zhai FY, Du SF, Wang ZH, Zhang JG, Du WW, Popkin BM. Dynamics of the Chinese diet and the role of urbanicity, 1991-2011. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2014;15(Suppl 1):16–26. doi: 10.1111/obr.12124. doi: 10.1111/obr.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Z, Zhai F, Zhang B, Popkin BM. Trends in Chinese snacking behaviors and patterns and the social-demographic role between 1991 and 2009. Asia Pacific journal of clinical nutrition. 2012;21(2):253. [PMC free article] [PubMed] [Google Scholar]
- 10.Ng SW, Howard AG, Wang H, Su C, Zhang B. The physical activity transition among adults in China: 1991–2011. Obesity Reviews. 2014;15(S1):27–36. doi: 10.1111/obr.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tzioumis E, Adair LS. Childhood dual burden of under-and overnutrition in low-and middle-income countries: A critical review. Food & Nutrition Bulletin. 2014;35(2):230–243. doi: 10.1177/156482651403500210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. The American journal of clinical nutrition. 2002;75(6):971–977. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 13.Popkin BM, Conde W, Hou N, Monteiro C. Is there a lag globally in overweight trends for children compared with adults? Obesity. 2006;14(10):1846–1853. doi: 10.1038/oby.2006.213. [DOI] [PubMed] [Google Scholar]
- 14.Popkin BM. Recent dynamics suggest selected countries catching up to US obesity. The American journal of clinical nutrition. 2010;91(1):284S–288S. doi: 10.3945/ajcn.2009.28473C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Social science & medicine. 2010;71(8):1436–1446. doi: 10.1016/j.socscimed.2010.07.027. doi: 10.1016/j.socscimed.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989-2011. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2014;15(Suppl 1):2–7. doi: 10.1111/obr.12119. doi: 10.1111/obr.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.International Food Policy Research Institute . Global Nutrition Report: Actions and Accountability to Accelerate the World's Progress on Nutrition. International Food Policy Research Institute; Washington DC: 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Labadarios D, Steyn NP. Nutritional disorders in Africa: the triple burden. Nutrition. 2005;21(1):2–3. doi: 10.1016/j.nut.2004.09.002. doi: 10.1016/j.nut.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Doak C, Adair L, Bentley M, Fengying Z, Popkin B. The underweight/overweight household: an exploration of household sociodemographic and dietary factors in China. Public health nutrition. 2002;5(1A):215–221. doi: 10.1079/PHN2001296. doi: 10.1079/PHN2001296. [DOI] [PubMed] [Google Scholar]
- 20.Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. International journal of obesity. 2005;29(1):129–136. doi: 10.1038/sj.ijo.0802824. doi: 101038/sj.ijo.0802824. [DOI] [PubMed] [Google Scholar]
- 21.Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989-2011. International journal of epidemiology. 2010;39(6):1435–1440. doi: 10.1093/ije/dyp322. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Golden MH. Specific deficiencies versus growth failure: type I and type II nutrients. Journal of Nutritional and Environmental Medicine. 1996;6(3):301–308. [Google Scholar]
- 23.de Onis M, Blössner M, Borghi E, Frongillo E, Morris R. WHO global database on child growth and malnutrition. WHO; Geneva: 2003. [DOI] [PubMed] [Google Scholar]
- 24.De Onis M, Organization WH. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. 2006 [Google Scholar]
- 25.de Onis M. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization. 2007;85(09):660–667. doi: 10.2471/BLT.07.043497. doi: 102471/blt.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cole T, Lobstein T. Extended international (IOTF) body mass index cut - offs for thinness, overweight and obesity. Pediatric obesity. 2012;7(4):284–294. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 27.Zhai F, Guo X, Popkin BM, Ma L, Wang Q, Yu W, Jin S, Ge., Keyuo Evaluation of the 24-hour individual recall method in China. Food and NUtrition Bulletin. 1996;17:154–161. [Google Scholar]
- 28.Popkin BM, Lu B, Zhai F. Understanding the nutrition transition: measuring rapid dietary changes in transitional countries. Public health nutrition. 2002;5(6A):947–953. doi: 10.1079/PHN2002370. [DOI] [PubMed] [Google Scholar]
- 29.Yang Y, Wang G, Pan X. China food composition 2002. Peking University Medical Press; Beijing: 2002. p. 136. [Google Scholar]
- 30.Chinese Nutrition Society . Chinese Dietary Reference Intakes (version 2013) Science Press; Beijing: 2014. [Google Scholar]
- 31.Murphy SP, Guenther PM, Kretsch MJ. Using the dietary reference intakes to assess intakes of groups: pitfalls to avoid. Journal of the American Dietetic Association. 2006;106(10):1550–1553. doi: 10.1016/j.jada.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 32.Wang X, Hojer B, Guo S, Luo S, Zhou W, Wang Y. Stunting and 'overweight' in the WHO Child Growth Standards - malnutrition among children in a poor area of China. Public health nutrition. 2009;12(11):1991–1998. doi: 10.1017/S1368980009990796. doi: 10.1017/S1368980009990796. [DOI] [PubMed] [Google Scholar]
- 33.Du S, Mroz TA, Zhai F, Popkin BM. Rapid income growth adversely affects diet quality in China—particularly for the poor! Social science & medicine. 2004;59(7):1505–1515. doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 34.Dearth-Wesley T, Wang H, Popkin B. Obesity dynamics in China: the poor are catching up. European journal of clinical nutrition. 2007;18:1–6. [Google Scholar]
- 35.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Emerging disparities in overweight by educational attainment in Chinese adults (1989-2006). Int J Obes. 2011 doi: 10.1038/ijo.2011.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. International journal of obesity. 2004;28(9):1181–1186. doi: 10.1038/sj.ijo.0802716. [DOI] [PubMed] [Google Scholar]
- 37.Wang Z, Zhai F, Du S, Popkin B. Dynamic shifts in Chinese eating behaviors. Asia Pac J Clin Nutr. 2008;17(1):123–130. [PubMed] [Google Scholar]
- 38.Popkin BM, Du S. Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. The Journal of nutrition. 2003;133(11):3898S–3906S. doi: 10.1093/jn/133.11.3898S. [DOI] [PubMed] [Google Scholar]
- 39.Ng SW, Zhai F, Popkin BM. Impacts of China's edible oil pricing policy on nutrition. Social Science & Medicine. 2008;66(2):414–426. doi: 10.1016/j.socscimed.2007.09.015. doi: http://dx.doi.org/10.1016/j.socscimed.2007.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chang Y, Zhai F, Li W, Ge K, Jin D, De Onis M. Nutritional status of preschool children in poor rural areas of China. Bulletin of the World Health Organization. 1994;72(1):105. [PMC free article] [PubMed] [Google Scholar]
- 41.Pinhas-Hamiel O, Newfield R, Koren I, Agmon A, Lilos P, Phillip M. Greater prevalence of iron deficiency in overweight and obese children and adolescents. International journal of obesity. 2003;27(3):416–418. doi: 10.1038/sj.ijo.0802224. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.