Abstract
Purpose
Cervical cancer is one of the most common causes of cancer mortality for women living in poverty, causing over 28,000 deaths annually in Latin America and 266,000 worldwide. To better understand the molecular basis of the disease we ascertained blood and tumor samples from Guatemala and Venezuela and performed genomic characterization.
Experimental Design
We performed HPV typing and identified somatically mutated genes using exome and ultra-deep targeted sequencing with confirmation in samples from Mexico. Copy number changes were also assessed in the exome sequence.
Results
Cervical cancer cases in Guatemala and Venezuela have an average age-of-diagnosis of 50 years, and 5.6 children. Analysis of 675 tumors revealed activation of PIK3CA and other phosphatidyl inositol (PI3K)/AKT pathway genes in 31% of squamous carcinomas and 24% of adeno- and adenosquamous tumors, predominantly at two sites (E542K, E545K) in the helical domain of the PIK3CA gene. This distribution of PIK3CA mutations is distinct from most other cancer types, and does not result in the in vitro phosphorylation of AKT. Somatic mutations were more frequent in squamous carcinomas diagnosed after age 50. Frequent gain of chromosome 3q was found and low PIK3CA mutation fractions in many tumors suggest that PI3K mutation can be a late event in tumor progression.
Conclusions
PI3K pathway mutation is important to cervical carcinogenesis in Latin America. Therapeutic agents that directly target PI3K could play a role in the therapy of this common malignancy.
Keywords: cervical cancer, Latin America, PIK3CA, human papilloma virus
Introduction
Human papilloma virus (HPV) causes >90% of cervical cancer (CC), one of the most common malignancies in women worldwide (1–3). While 70–90% of infections are cleared by the immune system, persistent HPV infections can lead to high-grade cervical intraepithelial neoplasia and cervical cancer (4). HPV replicates episomally but can integrate; integration is more frequent in late stage lesions and cancer and is associated with genome alteration and instability (5, 6). The viral E6 and E7 oncoproteins inhibit both TP53 and RB1 proteins altering cell cycle control, apoptosis and DNA repair.
The HPV16 and HPV18 types are the most oncogenic and account for 60–70% of cervical cancers, however at least 12 other high risk types can also be found in cervical tumors (7–9). HPV is both highly prevalent and highly infectious, being transmitted through multiple forms of sexual contact, and most males and females acquire one or more infections in their lifetime. Due to the long latency of development of cervical cancer, typically 10–15 years, there is opportunity to identify pre-cancers and eliminate them before the appearance of invasive cancer (4). The use of the Papanicolaou (Pap) test has reduced cervical cancer mortality by up to 80% in countries that have employed screening (3). However, women living in poverty, with inadequate health care, receive either no screening or poorly controlled screening and nearly 90% of cervical cancer mortality occurs in low and middle income countries (LMIC), and within minority populations in higher income countries (3, 10).
Many Latin American countries have high incidence and mortality from cervical cancer (8,414 deaths annually in Brazil; 4,769 in Mexico and 27,000 in the region overall [http://globocan.iarc.fr]). Several Latin American countries have large minority and/or indigenous populations that through poverty, discrimination, rural isolation and/or language barriers suffer from health disparities. Indigenous populations in Guatemala comprise 40% of the inhabitants and speak over 20 languages, Mexico has 75 indigenous groups and Venezuela has 40 recognized indigenous peoples.
Until recently molecular genetic studies of cervical tumors have been limited to candidate gene tests, and studies of cell lines such as HeLa (11). Because the E6 protein of high risk types causes the degradation of TP53, cervical tumors are one of the few cancers with a low level of mutation in the TP53 gene (12). The highly pathogenic HPV16 and HPV18 types can immortalize many cell types but additional lesions are required for transformation (13). The PIK3CA gene and pathway has also been shown to be frequently mutated (14) with a 31% mutation frequency in US cervical tumors. PIK3CA encodes an enzyme converting the signaling molecule phospho-inositol phosphate 2 (PIP2) to PIP3. This molecule can induce the phosphorylation of AKT, a central signaling kinase for many receptor tyrosine kinases. The PTEN protein converts PIP3 back to PIP2 and is a tumor suppressor gene. PIK3CA is one of the most frequently genes mutated in cancer, with most mutations occurring in the kinase domain and resulting in constitutive activation. The helical domain of PIK3CA is also frequently mutated at residues E542 and E545 and this domain is thought to mediate interactions with an inhibitory subunit, and may signal through other kinases such as SGK3 (15, 16).
Genome sequencing of cervical tumors with viral integration revealed wide-spread genome rearrangement and specific sites of integration (17). A comprehensive study of 100 Norwegian and 15 Mexican tumors with genome, exome, and RNA-seq analyses; identified frequent driver genes, common chromosomal alterations and integration sites (18). A genome sequencing study of HPV integration in Chinese cervical tumors revealed diverse integration sites and a study of 15 cervical adenocarcinomas from Hong Kong identified frequently mutated genes (19, 20). To further understand the molecular basis of cervical cancer in high incidence countries we undertook an analysis of cervical cancers in Guatemala and Venezuela with validation from a cohort from Mexico to identify frequently mutated genes and correlate mutations with histological type, HPV type and age of cervical cancer onset.
Materials and Methods
Sample collection
Samples were obtained under Institutional Review Board (IRB) approval with informed consent, a standardized questionnaire on socio-demographic characteristics, reproductive and contraceptive history, smoking and Pap smear history. Protocols were approved by the Ethical Review Committees in Guatemala, Venezuela, and Mexico and the Office of Human Research Subjects, NIH. Subjects from Guatemala (296 FIGO stage I–IV cancers) and Venezuela (39 with FIGO Stage I–IV, and 38 CIN 1–3) were collected from 2011–2013 and from Mexico from 2003–2007. All patients were referred for suspected invasive cervical cancer, all consenting patients were included, and only pregnant subjects and cancer-free women were excluded. Subjects from Venezuela included subjects with a positive Pap smear and biopsy (CIN 1-CIN 3). Surgically resected cervical tumors tissues were stored in RNAlater (QIAGEN) at −20° C until extraction (Supplementary Fig. 1).
DNA and RNA extraction and HPV genotyping
DNA and RNA was extracted from the cervical cancer tissues (5–10 mg) using the AllPrep DNA/RNA Micro Kit (QIAGEN) as described by the manufacturer. For HPV type determination, DNA samples were amplified by PCR using Broad-Spectrum GP5+ (BSGP5+) forward primers with inosine at selected sites, and GP6+ reverse primers along with the β-globin MS3/MS10 primers (226 bp) as a control for DNA quality (21). Four hundred nanomolar of each forward primer were used with ZymoTaq PreMix (Zymo Research). A 10-min denaturation step (95° C) was followed by 40 cycles of amplification (Perkin-Elmer thermocycler). Each cycle was 94° C for 20 s, 38° C for 30 s, and 71° C for 80 s, and final elongation for 5 min. Ramping rates for the Mastercycler were; 1.8°C/s from 94° C to 38° C, 2.0°C/s from 38° C to 71° C, and 2.8° C/s from 71° C to 94° C. Each PCR experiment included HeLa DNA as positive and HEK293 and / or C-33A as negative controls, and sample lacking template DNA. Positive samples by gel electrophoresis were sequenced on an ABI 3730XL and analyzed by assembly and trimming in SeqMan (DNASTAR) followed by BLAST search (NCBI).
NextGen sequencing of HPV
To resolve multiple types on the Ion Torrent PGM, the BSGP6+ primers were tailed with Ion Express barcodes and Ion Torrent A adapter and BSGP5+ primers tailed with the P1 adapter (Supplementary Table S1). β-globin MS3/MS10 primers were included in the reaction to control for amplification, without sequencing adapters or barcodes When samples were PCR negative for HPV, but amplified for β-globin (by gel electrophoresis), a second PCR reaction was performed using 2× DNA input material. Positive PCR products were quantitated on the Caliper GX, normalized and pooled for sequencing on the Ion Torrent PGM as per manufacturer’s instructions. Briefly, normalized, pooled libraries were amplified via emulsion PCR using the One Touch v2, enriched on the ES2, and sequenced for 520 cycles on the PGM. An average of 8000 reads was obtained for each sample.
There was an 83% concordance between the PCR and next-generation (NG) sequencing methods (including both HPV+ and HPV− samples), and another 6% of samples had mixed HPV infection by NG with Sanger sequencing detecting one of the types. A total of 8% of samples had abundant reads of more than one HPV type by NG sequencing.
Exome sequencing
DNA preparation
A 1 μg aliquot of high molecular weight DNA (determined by Picogreen, Invitrogen) was used in TargetSeq exome v2 capture process with enzymatic shearing (Ion Shear Plus Reagents Kit, Life Technologies) to a target size range of 135–165 bp.
Library preparation for TargetSeq exome capture
Sheared genomic DNA followed the TargetSeq protocol for ligation, nick repair, purification, size selection and final amplification. For the ligation and nick repair, a master mix consisting of 10 μL 10× Ligase Buffer, 10 μL A and P1 adapters, 2 μL dNTP mix, 41 μL nuclease free water, 4 μL DNA ligase and 8 μL nick repair polymerase. PCR conditions were as follows: 25° C for 15 min, 98° C for 20 min. and a hold at 4° C. The amplified material was cleaned with Ampure XP reagent (Agencourt) according to the TargetSeq v2 protocol, with DNA elution in 20 μL of Low TE. Amplified sample libraries were size selected (Pippen Prep instrument, Sage Science) and processed according to the TargetSeq protocol. The Pippen Prep was set to elute “Tight” at 220 bp. The eluted size selected samples were cleaned with Ampure XP reagent according to the TargetSeq v2 protocol, and DNA eluted in 30 μL of Low TE. The final amplification of the size selected fragment libraries was performed using a master mix consisting of 200 μL Platinum PCR Supermix High Fidelity and 20 μL Library Amplification Primer Mix. PCR cycling conditions were: 95° C for 5 min, and 8 cycles of 95° C for 15s, 58° C for 15s, 70° C for 1 min. The amplified samples were purified with Ampure XP reagent according to the TargetSeq v2 protocol, with elution in 50 μL of Low TE, and assessment on the Agilent Bioanalyzer (Agilent Technologies).
TargetSeq exome capture
An aliquot of 500 ng of each size selected sample fragment library was used in the TargetSeq Exome enrichment step with 5 μL 1 mg/mL Human Cot-1 DNA, 500 ng of sample, 5 μL each of Ion TargetSeq Blocker P1 and A. The mix was dried at 60° C for 30 min. To each sample we added 7.5 μL TargetSeq Hybridization Solution A (29) and 3 μL TargetSeq Hybridization Enhancer Band incubated for 10 min at 95° C to denature the DNA. The sample was then transferred to a 0.2 mL tube containing 4.5 uL of the TargetSeq Custom Probe Pool and incubated at 47 °C for 72 h, the samples were washed and the probe-hybridized DNA was recovered. After wash and recovery, the samples were eluted in 30 μL of nuclease free water and amplified according to the TargetSeq protocol. A master mix containing 200 μL Platinum PCR Supermix High Fidelity and 20 μL Ion TargetSeq Amplification Primer Mix was added to the 30 μL of TargetSeq capture beads;. PCR cycling conditions were as follows: 95 °C for 5 min, followed by 8 cycles of 95°C for 15s, 58°C for 15s, 70°C for 1min, purified with Ampure XP reagent according to the TargetSeq v2 protocol, eluted in 25 μL of Low TE, quantitated and qualitatively assessed on the Agilent Bioanalyzer.
Ampliseq Exome Sequencing
ALiquots of 100ng of genomic DNA from cervical tumor and normal samples were processed according to the standard protocol for Ampliseq target amplification and library preparation. Each tumor and normal library were pooled for the template emulsion prep and sequenced as a pair using the Proton P1 chip and Ion Torrent Proton Sequencer (Thermo Fisher Scientific). Each run produced over 10 Gb of sequence data and had an average depth of coverage surpassing 100×. The data was aligned using TMAP (https://github.com/iontorrent/TS/tree/master/Analysis/TMAP) and variants were called using Torrent Suite Variant Caller (TSVC) onboard the Proton Sequencer (Thermo Fisher Scientific). The data was processed off-line through a custom analysis workflow utilizing the aligned reads and a dual variant calling process, TSVC and a modified GATK variant caller optimized for Proton data (22).
Copy number analysis
The CNV analysis was performed using tumor and matched normal sequence. A log based 2 ratio between tumor and normal was calculated based on the ngCGH algorithm (https://github.com/seandavi/ngCGH), using the tumor and normal BAM files. Genomic windows are defined from blocks of 1000 reads in the normal sample and thenthe number of reads in the tumor is quantified. A ratio is made between the number of reads in the tumor and the number of reads in the normal. Finally, a log2 transformation is applied to each ratio and the entire vector of the results is centered by subtracting the median to make the median of the log2 ratios zero.
The log2 ratios were imported to Nexus Copy Number Discovery Edition Version 7.5. (BioDiscovery, Inc., Hawthorne, CA http://www.biodiscovery.com). The Fast Adaptive States Segmentation Technique (FASST2) segmentation method (BioDiscovery, Inc.) was used to make CNV calls. A significance threshold of 1.0E-5 was used to adjust the sensitivity of the FASST2 segmentation algorithm. A minimum number of 20 amplicons per segment were used to eliminate small CNVs. Cut offs of 0.2/−0.2 were used for gain/loss; and for high gain/high loss were set to 0.6/−1.0, and the results tabulated (Supplementary Fig. S4).
Targeted gene sequencing
A targeted, multiplex PCR primer panel was designed using the custom Ion Ampliseq Designer v1.2 (Life Technologies). The primer panel covered 12kb of sequence including the coding region of 8 genes – HRAS, CTNNB1, KRAS, STK11, CDKN2A, PIK3CA, PTEN, and TP53 (average coverage 99%, average amplicon size 225 bp). Sample DNA (tumor or tumor/normal pairs) was amplified and libraries prepared following the Ion Ampliseq Library Preparation protocol (Life Technologies). Individual samples were barcoded, pooled, applied to chips, and sequenced on the Ion Torrent PGM Sequencer using the Ion PGM Template OT2 200 and Ion PGM Sequencing 200v2 kits. Mean read length after sequencing was 116bp, and 94% of amplicons gave an average coverage of greater than 50 reads/sample.
Sequence alignment and mutation prediction
Resulting sequence reads were aligned to the human reference genome version hg19 using the TMAP aligner (Life Technologies) and single nucleotide variants (SNVs) were called using the Genome Analysis Tool Kit (GATK) (22, 23) and the Torrent Variant Caller (TSVC, Life Technologies) and small insertions and deletions were called using the TSVC. The NIH Biowulf Cluster was used for additional variant annotation. All mutations in Supplementary Tables 1 and 2 were manually examined in IGV (24) to confirm an adequate number of mutant reads in both directions and to eliminate false positives. Selected sites were manually examined to identify potential false negative predictions. For the E542K and E545K sites, a minimum of 100 reads and 3% mutant reads were necessary to call the sample mutation positive. For a subset of samples targeted sequencing was performed on both tumor and normal DNA to confirm that reported mutations were somatic.
PIK3CA Mutation Verification
Primers for the PIK3CA gene were described (25). The amplification (WGA; QIAGEN) required 20 ng cervical cancer tumor or normal blood DNA and standard PCR conditions at an annealing temperature of 63°C 10 cycle and 58°C 30 cycle, respectively. Big Dye v.3.1 chemistry (ABI) sequencing reactions were sequenced on a 3730 Genetic Analyzer (ABI), and chromatograms examined using Sequencher, v.4.8 (GeneCodes) and Mutation Surveyor (Softgenetics). Exons 9 and 20 were sequenced in the majority of the Venezuela and Guatemala tumor samples and selected mutations in other gene regions were also validated.
Quantitative RT-real-time PCR
One microgram of total RNA was reverse transcribed into cDNA using the Transcriptor First Strand cDNA Synthesis Kit (Roche) with oligonucleotide (dT)18 primer according to the manufacturer’s instructions. Real time PCR was performed for E6 and E7 HPV transcripts, using gene and type specific primers, in the presence of SYBR green, in HPV16 and 18 positive tumors. Relative expression levels of E6 and E7 were multiplied by 1000. The E6 primers detect the full-length E6/E7 transcript producing principally E6 protein and the E7 primers detect transcripts expressing E6, E6*1, E6*2 and E7 proteins; (Supplementary Figure 10)(26). For normalization, the expression of a 144 bp β-actin fragment was used. Each experiment included HeLa cDNA and Ca-Ski cDNA as positive and C-33A as negative controls. The relative mRNA expression level of PIK3CA was calibrated with HUC (Human Universal Control from Clontech). Primers and probes for the PIK3CA gene (Hs00907966_m1) and β-actin gene (Hs99999903_m1) were from Applied Biosystems.
Site Directed mutagenesis and phosphorylation determination
Site-directed mutations were introduced into a full length of PIK3CA expression vector (Origene), and confirmed by sequencing, using the QuikChange II XL kit (Agilent). The helical domain mutations E542K, E545K, E542K/E545K, E542Q/E545K, Q546R, D549H of p110α were compared to the kinase domain mutation H1047R. The empty vector, wild-type PIK3CA and mutant PIK3CA expression constructs were transiently transfected into U2OS cells using HyliMax (DojinDo). The U2OS cells were serum starved in DMEM containing 0.5% FBS overnight and treated with 0.1 μM Calyculin A (Cell Signaling Technology) in 0% FBS for 30 minutes prior to lysis cell. Whole cell protein (25 ug) was separated in a 4–12% NuPAGE Bis-Tris gel, transferred to PVDF membrane (Invitrogen). The primary antibodies were monoclonal rabbit-anti-phospho-AKTSer473, phospho-AKTThr308, total AKT (Cell Signaling Technology) at a dilution of 1:8000 to 1:10,000, rabbit-anti-p110α antibody and β-actin was used as a control. HRP-conjugated anti-rabbit IgG was used as secondary antibody (Cell Signaling Technology).
Statistical analyses
Mann-Whitney-U, two-tailed t-test, One Way AVOVA, Kruskal-Wallis, Pearson’s chi-squared test and Fisher’s exact test statistical analyses were performed using GraphPad Prism version 5 for Windows; P<0.05 was regarded to be statistically significant.
Results
Exome and targeted gene sequencing
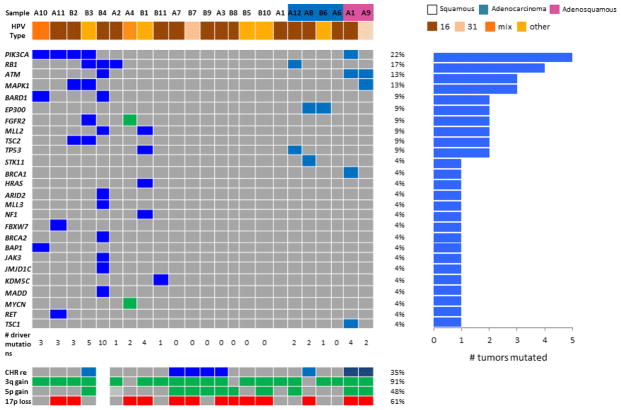
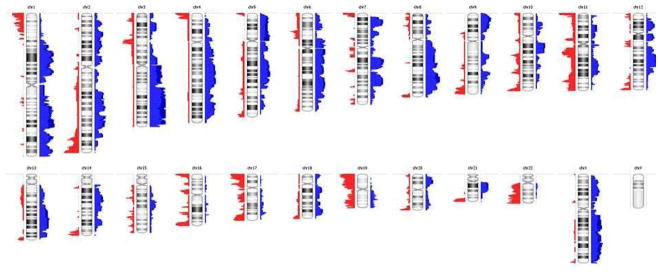
To determine the HPV types and molecular characteristics of Latin American women with cervical tumors, subjects were prospectively enrolled and tumor tissue and blood collected at the Instituto de Cancerologia (Guatemala) and the Hospital Central Universitario (Venezuela). A comparison sample set of 330 subjects from Mexico was also included (Supplementary Fig. 1). There was no significant difference between squamous carcinoma and adeno- and adenosquamous tumors in age at collection, reproductive factors, HPV type, or smoke exposure; however adeno- and adenosquamous tumors are more often diagnosed at Stage I (P=0.061, Table 1). To identify potential cancer genes, 23 Guatemalan CC and corresponding normal blood DNAs were subjected to exome sequencing. Variants in genes predicted to be mutated in two or more tumors, and in known somatic cancer genes (18, 27, 28) are shown (Fig. 1). The tumors contained a predominance of C-T and T-C mutations (Supplementary Fig. 2). Predicted somatic mutations were found in known cancer genes including PIK3CA, RB1, TP53, MAPK1, HRAS, KRAS, TSC1, BRCA1, BRCA2, BAP1, and ATM. The tumor and normal exome sequence was also used for copy number determination and as seen previously (18, 29), nearly all Guatemalan tumors tested have 3–5 copies of chromosome 3q, 43% have gain of 5q and 14/23 (61%) have chromosome loss at 17p containing the TP53 loci (Fig. 1, 2). In total 8/23 cervical tumors show extensive chromosomal rearrangement (>100 chromosome breaks) (Fig. 1). Interestingly one squamous tumor (A4) has amplification of the 2p region containing MYCN, 10q containing the FGFR2 locus, and a region of 6q21 (Fig. 1, Supplementary Fig. S3).
Table 1.
Patient Demographics and Disease Characteristics
| Characteristic | Total (n=531) | Squamous (n=466) | Adenocarcinoma/Adenosquamous (n=65) | P value |
|---|---|---|---|---|
| Mean age at collection | 52 ±13.2 | 52.3 ±13.3 | 49.8 ±12.4 | 0.055a |
| Mean age menarche | 13.3 ±1.5 | 13.3 ±1.5 | 13.4 ±1.6 | |
| Mean pregnancies | 5.9 ±3.3 | 6.0 ±3.3 | 5.3 ±3.0 | |
| Mean age at first birth | 18.5 ±2.7 | 18.6 ±2.6 | 17.7 ±2.9 | |
| Human Papiloma Virus | 0.21b | |||
| HPV 16 | 252 (51.5) | 221 (51.5) | 31 (51.7) | |
| HPV 18 | 48 (9.8) | 38 (8.9) | 10 (16.7) | |
| HPV 45 | 38 (7.8) | 33 (7.7) | 5 (8.3) | |
| All others | 151 (30.8) | 137 (31.9) | 14 (23.3) | |
| Grade | 0.0061b | |||
| I | 122 (23.3) | 96 (20.8) | 26 (40.6) | |
| II | 213 (40.7) | 193 (41.9) | 20 (31.2) ** | |
| III | 173 (33.0) | 157 (34.1) | 16 (25.0) ** | |
| IV | 16 (3.0) | 14 (3.0) | 2 (3.1) | |
| Country | 0.010c | |||
| Guatemala | 208 (39.2) | 192 (41.2) | 16 (24.6) | |
| Mexico | 323 (60.8) | 274 (58.8) | 49 (75.4) | |
| Cooking Method | 0.75b | |||
| Gas | 57 (22.3) | 25 (22.1) | 3 (27.3) | |
| Wood | 155 (60.6) | 74 (65.5) | 6 (54.6) | |
| Gas&Wood | 44 (17.2) | 14 (12.4) | 2 (18.2) |
P <0.001
Mann-Whitney test
Pearson’s chi-squared test
Fisher’s exact test
Included are all samples with known pathology that are either squamous carcinoma, adenocarcinoma or adenosquamous carcinoma. Means are followed by standard deviation and numbers by percentages.
Figure 1.
Driver gene mutations in 23 Guatemalan cervical cancers. Genes frequently mutated or amplified in other cancers are indicated, with their gene names at the left and the mutation percentages (%) on the right. The predominant HPV type and pathology is indicated at the top (unlabeled tumors are squamous cell carcinomas). Below the main section, the presence of chromosome rearrangement (>100 chromosome breaks, CHR re), gain of chromosome 3q and loss of 17p are shown.
Figure 2.
Copy number changes in cervical tumors. The predicted copy number changes from 23 tumors analyzed by AmpliSeq Exome were combined. Deletions are displayed by red bars to the left of the chromosome ideograms, and gains by blue bars to the right. The height of the bars indicates the combined effect of the CNV. Darker shades of red and blue indicate CNVs above a cutoff of log2 ratio value of above 0.6 and below −1.0, respectively.
To further explore the role of the major genes identified in this study and previously reported in at least 5% of tumors in the Catalogue of Somatic Mutations in Cancer (COSMIC) database, an eight-gene targeted sequencing panel was developed (CDKN2A, HRAS, KRAS, CTNNB1, PIK3CA, PTEN, STK11 and TP53 genes). The targeted panel was applied to 280 CC from Guatemala, 75 CC and pre-malignant lesions from Venezuela, and a replication set of 330 CC from Mexico, with up to 1000× coverage of targeted nucleotides (500× average, Supplementary Figs. 1 and 4). Predicted variants are shown (Supplementary Tables S2 and S3). Mutations in HRAS, KRAS, CDKN2A, and CTNNB1 were infrequent; however, genes in the phosphatidyl inositol (PI3K) pathway were frequently mutated. Specifically, activating mutations were common in PIK3CA, and inactivating mutations in PTEN and STK11 were also found (Table 2 and Supplementary Tables S2 and S3).
Table 2.
Summary of mutations in targeted gene panel
| Gene | Guat. | % | Venez. CIN | % | Venez. CC | % | Mexico | % | Total |
|---|---|---|---|---|---|---|---|---|---|
| PIK3CA | 91/280 | 33% | 2/30 | 7% | 11/40 | 28% | 91/325 | 28% | 30% |
| TP53 | 15/280 | 5.4% | 0/30 | 0% | 2/40 | 5% | 15/325 | 5% | 5.0% |
| STK11 | 11/280 | 3.9% | 0/30 | 0% | 2/40 | 5% | 6/325 | 2% | 2.9% |
| PTEN | 14/280 | 5.0% | 0/24 | 0% | 2/40 | 5% | 22/325 | 7% | 5.9% |
| KRAS | 2/280 | 0.7% | 0/24 | 0% | 1/40 | 3% | 12/325 | 4% | 2.3% |
| HRAS | 2/280 | 07% | 0/24 | 0% | 0/40 | 0% | 5/325 | 2% | 1.1% |
| CDKN2A | 0/280 | 0% | 1/24 | 3% | 1/40 | 32% | 0/325 | 0% | 0.2% |
| CTNNB1 | 0/280 | 0% | 1/24 | 3% | 1/40 | 3% | 0/325 | 0 | 0.2% |
| PIK3CA+PTEN | 105/280 | 38% | 13/40 | 33% | 108/325 | 33% | 35% | ||
| All PI3K | 111/280 | 40% | 15/40 | 38% | 104/325 | 32% | 36% |
Mutations in targeted genes are shown for each country along with the percentage and sum of PIK3CA and PTEN (PIK3CA+PTEN) and PIK3CA< PTEN and STK11 (All PI3K). CIN, cervical intraepithelial neoplasia; CC, cervical cáncer, Guat., Guatemala, Venez., Venezuela. Total excludes Venezuela CIN.
Distribution of mutations in the PIK3CA gene
Somatic PIK3CA mutations were detected in 33% (91 of 280) of carcinomas from Guatemala, 28% (11 of 40) from Venezuela, and 28% (91 of 325) from Mexico. Only 2 of 27 cervical intraepithelial neoplasia (CIN) grade 1, 2, or 3 lesions from Venezuela (one CIN 2 and one CIN 3) had PIK3CA mutations (8%), indicating that these mutations occur predominantly in malignant tumors. When tumors were divided by histological type 155/499 squamous cell carcinomas (31%), 16/67 adenocarcinomas (24%) and 5/21 adenosquamous carcinomas (24%) have a PIK3CA mutation. A total of 95% of all PIK3CA mutations were located in the ABD, ABD-RBD linker, C2, and helical domains of PIK3CA, whereas mutations in the kinase domain were rare (Fig. 3A and B). In fact, two specific mutations (E542K, E545K) account for 81% of the PIK3CA mutations in Mexico and 76% in Guatemala (Fig. 3), and helical domain mutations are significantly more common in squamous cell versus adenocarcinomas (P=0.017, Supplementary Fig. S5). Helical PIK3CA mutations are more frequent in cervical and bladder cancer as compared to breast, endometrial or intestinal tumors (P< 0.0001) (Fig. 3C). Several tumors had more than one PIK3CA or PTEN mutation. For adjacent mutations their presence on either the same DNA strand (cis) or different strands (trans) could be determined, and both cis and trans examples were found (Supplementary Fig. S6).
Figure 3.
The distribution of somatic PIK3CA mutations. A). Mutations in patients from Guatemala (red triangles), Venezuela (black triangles), and Mexico (green triangle) are shown relative to functional domains (ABD, p85 binding domain; RBD, RAS binding domain; C2 domain; Helical domain; and Kinase domain) of the PIK3CA protein. The percentage of mutations detected within each region and the amino acid positions are indicated below. Blue indicates novel mutations from this study and purple indicates mutations without published functional analyses. * indicates the patient with ≥1 PIK3CA mutation. B) Proportion of PIK3CA mutations in cervical cancer in different countries. The domain location of PIK3CA mutations are shown in comparison with the cervical tumors in this study. The brackets denote comparison of helical versus kinase domain in Latin American cervical tumors to breast, endometrial and intestinal tumors (****= P<0.0001). The frequency of PIK3CA mutations is noted above and details are in Supplementary Table 6C) The frequency and location of PIK3CA mutations from colon, breast, endometrial, intestine, ovary, bladder from the literature and the COSMIC Catalogue of Somatic Mutations in Cancer; http://www.sanger.ac.uk/cosmic) database and cervical cancers from this study are displayed (14, 18, 33).
Interestingly, despite tumors having 70% or greater tumor cells by pathological examination, many tumors with PIK3CA mutations have a low percentage of mutant reads. A total of 79% of tumors with a PIK3CA mutation have between 4 and 33% mutant reads, and this is constant across grades I–IV (78–83%); suggesting that there is considerable tumor heterogeneity. Targeted sequence on tumor and normal DNA and Sanger sequencing was used to confirm selected PIK3CA mutations were somatic variants and the approximate mutated allele fraction was comparable to that obtained from next-generation sequencing (Supplementary Fig. S7). The high frequency of E542K and E545K mutations allowed the determination of the mutation fraction of each individual mutation and for double mutants (Supplementary Fig. S8A, S8B). E542K is found 31% of the time at a mutation fraction greater than 20%, whereas 51% of E545K-containing tumors have >20% mutant reads (X2=5.5; P=0.019). However, for the six E542K/E545K double mutants, the two mutations are always on different haplotypes and E542K is usually more prevalent (Supplementary Fig. S8B).
Several PIK3CA mutations described here have not previously been reported (delN107, E1034Q in Venezuela; T229I, Q861R, K942M and V952G in Guatemala and V146I, M299V, delH419_C420 and G914R in Mexican tumors), whereas the R38H, R88Q, K111E, K111N, E453K, E542K, E545K, and H1047R variants are documented somatic gain-of-function alleles (25, 30–32) (Fig. 3A). Both combined PIK3CA mutations and overall mutations are statistically significantly increased in patients diagnosed at a later age and are less common in HPV18− and HPV45-positive tumors (P=0.0016) (Supplementary Fig. 9, Supplementary Table 4). While adenocarcinomas occur with a younger average age, and a lower tumor stage and may confound these relationships, squamous cell subjects diagnosed before age 50 have significantly fewer PIK3CA mutations (P=0.0001). Comparison of our Latin American data with data from other countries [(14, 18, 33), COSMIC database] demonstrates differences in frequency of PIK3CA mutations in individual domains, as well as the E542K, E545K, and H1407H sites (Fig. 3C; Supplementary Table S5).
HPV type and PIK3CA gene expression
It has been shown that the HPV E6 and E7 proteins can activate the PI3K/AKT pathway (34). We determined the mRNA expression levels of the PIK3CA, and HPV E6 and E7 transcripts in 65 HPV16+ tumors. The mRNA levels for PIK3CA were higher in PIK3CA mutation-positive tumors compared to PIK3CA WT tumors (P = 0.029), and HPV E6 and E7 expression was also elevated in PIK3CA mutant tumors (P=0.040, Supplementary Fig. S10A, B).
Phosphorylation of AKT by specific PIK3CA mutations
To determine whether specific PIK3CA mutations lead to increased AKT phosphorylation in vitro, U2OS cells were transfected with mutant constructs and used for WB analysis. Total PIK3CA (p110α), AKT, β-actin and p-AKT (Ser473) were constant. However, the kinase domain mutation H1047R led to increased p-AKT at Thr308, however neither E542K, E545K nor the double mutant significantly increased p-AKT at Thr308 levels (Fig. 4).
Figure 4. PIK3CA mutation effect on AKT phosphorylation.
Expression and analysis of the phosphorylation of AKT in U2OS transfected with empty vector, wild type and mutant PIK3CA constructs. The H1047R constructs showed a significant increase in p110α and Thr308 levels compared with wild type (WT) control, but the 3 helical domain mutations E542K, E545K and E542K/E545K showed a minimal level at Thr308. A H1047R mutant was used as a positive control. Densitometric analysis of specific signals using Image J software, on three independent blots, were quantitated and normalized to actin. One Way AVOVA and Kruskal-Wallis Statistical method was performed using GraphPad Prism version 5 (P<0.05).
Discussion
Our study combines exome and targeted sequencing to examine the relationship between genetic mutations and cervical cancer in tumors in three countries with high incidence and mortality. We identified frequent PIK3CA gene mutations in Latin American cervical tumors that had a distinct distribution from those found in most other cancers (25, 30). Latin American tumors have a similar PIK3CA mutation frequency as US tumors (33% vs. 31%), and display a somewhat higher prevalence in squamous carcinomas (Supplementary Table 5). However, the PIK3CA mutation frequency is significantly lower in Swedish tumors (8.2 %; X2= 35, 2.89 × 10−08) (14, 18). Most PIK3CA mutations are located in the ABD and ABD-RBD linker, and helical domain, especially in the Arg532 and Arg535 residues in the helical domain, particularly in squamous carcinomas. Recent structural studies of the PIK3CA protein (p110α) indicate that the helical domain of PIK3CA acts as a scaffold for the assembly of p110α domains and for interactions with the inhibitory p85α (35–37). While E545K mutations are also common in colorectal, breast, intestine, ovary, and endometrial cancers (25, 30, 38)(COSMIC database), these tumors also have frequent mutations in the kinase domain. In contrast, we found only six mutations within the kinase domain in cervical cancer. The most common PIK3CA mutation in all tumors, H1047R, which has been associated with an increased response rate to PI3K/AKT/mTOR inhibitors (39), is very rare in our study, consistent with US tumors (14). The distribution of mutations in PIK3CA/p110α suggests that there is a selective advantage to disrupting the ABD and ABD-RBD linker interactions in cervical cancers. Interestingly a similar pattern was recently identified in bladder and HPV+ oral cancer with more helical domain mutations than kinase domain mutations, and a role for APOBEC has been proposed (38, 40–42).
Our study has several limitations: 1) the small size of the mutation discovery cohort (24 tumors of different histology and HPV type) would not allow the discovery of all frequently mutated genes or copy number changes, and without paired-end whole genome sequence we cannot fully evaluate the high rearrangement tumors for chromothripsis or chromoplexy (43); 2) we lack a cancer-free cohort to explore risk factors for invasive cancer (apart from HPV infection); 3) our data on tumor mutation heterogeneity lack a direct assessment of tumor purity and would require a detailed microdissection, immunohistochemistry, and/or single cell sequencing component to fully explore; 4) to date we have limited treatment outcome data to understand how molecular events may predict survival. However we feel that data on tumors from high prevalence countries is important in understanding cervical cancer worldwide.
PI3K signaling has been shown to be important in HPV transformation (44). In this study, we show that PIK3CA mRNA expression is (41) elevated in tumors with PIK3CA mutations, and associated with upregulated E7 mRNA expression at least in HPV16-positive tumors. The PIK3CA gene is on chromosome 3q, in a region known to be duplicated in most invasive cervical cancers and in 19/22 of the tumors we report (29). Our data indicate that in approximately 20% of tumors with PIK3CA mutation (5% of all tumors), mutation is an early event and the 3q duplication involves the mutant PIK3CA allele, whereas in the remaining tumors the mutation occurs on the non-duplicated allele, or after duplication (Supplementary Fig. S11).
The presumed late occurring PIK3CA mutations could represent tumor evolution or represent the accumulation of somatic passenger mutations driven perhaps by HPV induction of APOBEC enzymes (42). Given the roles of PI3K in cellular proliferation, metastasis, cell cycle, and cell survival, PIK3CA mutations may impart a more aggressive and treatment-resistant phenotype (44, 45). However, it should be pointed out that our study is limited in having few early stage lesions, no normal cervical tissue control, and exome and targeted sequencing can miss mutations, especially insertions/deletions (46). Sampling of multiple areas of the same tumor as well as primary and metastatic lesions from the same patients could address this issue.
While kinase domain mutations in PIK3CA have been shown to result in elevated AKT phosphorylation and mTOR activation, consistent with other reports, helical domain mutations do not (47). Several groups have documented that the AKT-related kinase SGK3 is activated by PIK3CA helical domain mutations (15, 16). Interestingly, in a clinical trial of AKT inhibitors, cervical and other cancers patients with the E542K mutation had a shorter median progression-free survival than those with the H1047R mutation (14, 39); suggesting that this subtype may be more refractory to therapy. And a recent trial showed PIK3CA to be a marker of poor response (48). The data from our study and others would suggest that agents directly targeting PIK3C would have the best chance of benefit.
Our data are consistent with data (18) that cervical tumors have a relatively low level of driver gene mutations and group with glioblastoma, ovarian, breast, kidney, and acute myelogenous leukemia as tumors with an average of 2–4 driver gene mutations (28). Given that HPV expresses the two viral oncogenes, E6 and E7, this is expected. However, RB1 and TP53 are mutated in a subset of tumors suggesting that further inactivation of these genes is sometimes required. In squamous tumors these additional drivers are more frequently found in tumors in older women.
While HPV infection is the dominant risk factor in cervical cancer, tobacco use is a major co-factor in developed countries, (49) and is variable within the subjects in this study. Interestingly, tobacco use is very low in Guatemala, but exposure to wood smoke is high (Table 1). Whether cooking with wood in the home contributes to cervical cancer similar to tobacco will require further study. We find that the distribution of HPV types is similar in the three populations studied, but that the PIK3CA and overall mutation load is higher in patients diagnosed after age 50 and in HPV16+ patients (Supplementary Fig. S9, data not shown). HPV18 and HPV45 negative tumors are also more common in older patients (Supplementary Fig. S9B).
In summary, Latin American cervical tumors have a high frequency of mutations in the PIK3CA gene, especially at the E542 and E545 residues in the helical domain. PIK3CA kinase domain mutations more extensively phosphorylate AKT and are independent of RAS activity (47, 50). Furthermore, clinical trials of PI3K/AKT/mTOR inhibitors have shown that patients with the H1047R mutation in the PIK3CA kinase domain had better response (39). Therefore these two classes of PIK3CA mutations, while both displaying activating/gain-of-function properties denote functionally distinct classes of cancers. Our data adds to the literature published to date demonstrating that although PIK3CA mutations are common in cervical cancer, they are not predicted to respond well to AKT/mTOR targeted agents. However, comprehensive surveys of other high prevalence countries are needed to fully understand the worldwide heterogeneity of this disease.
Supplementary Material
Statement of translational relevance.
Cervical cancer is one of the most common cancers in women worldwide with over 80% of deaths occurring in women living in poverty. Although pre-cancerous lesions and local malignancy is curable, invasive and/or metastatic tumors have poor survival. In invasive tumors from three Latin American countries we identify common activation of the phosphotidyl-inositol 3 (PI3K) kinase pathway. Up to 33% of tumors have mutations in the PIK3CA gene, predominantly at two specific helical domain sites, E542K and E545K, and rarely in the kinase domain. The PI3K pathway can signal through the AKT1 and MTOR serine-threonine kinases, however PIK3CA helical mutations may activate alternative pathway(s). Our data are relevant to the development and application of therapeutic strategies for invasive cervical tumors.
Acknowledgments
The authors thank the staff and health professionals from the Instituto de Cancerologia, Guatemala City, Guatemala, and Hospital Central Universitario “Dr. Antonio M Pineda”, Barquisimeto, Lara State, Venezuela, as well as Patricia Zaid, Martha Balsells de Sechel, Keyla Guerra, Esther Avila and Lineth Boror for sample and data collection and shipping, Russ Hanson for approvals, and the BSP-CCR Genetics Core for technical support.
Funding Information
The work was supported in part by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Center for Cancer Research, and by Leidos Biomedical Research, Inc., under contract # HHSN261200800001E and the National University of Mexico (www.unam.mx), grant number SDI.PTID.05.2 (to JB). The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
Footnotes
The authors have no conflicts of interest to report.
References
- 1.de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. The lancet oncology. 2010;11:1048–56. doi: 10.1016/S1470-2045(10)70230-8. [DOI] [PubMed] [Google Scholar]
- 2.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. The Journal of pathology. 1999;189:12–9. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 3.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA: a cancer journal for clinicians. 2015 doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 4.Schiffman M, Castle PE. The promise of global cervical-cancer prevention. The New England journal of medicine. 2005;353:2101–4. doi: 10.1056/NEJMp058171. [DOI] [PubMed] [Google Scholar]
- 5.Wentzensen N, Vinokurova S, von Knebel Doeberitz M. Systematic review of genomic integration sites of human papillomavirus genomes in epithelial dysplasia and invasive cancer of the female lower genital tract. Cancer Res. 2004;64:3878–84. doi: 10.1158/0008-5472.CAN-04-0009. [DOI] [PubMed] [Google Scholar]
- 6.Xu B, Chotewutmontri S, Wolf S, Klos U, Schmitz M, Durst M, et al. Multiplex Identification of Human Papillomavirus 16 DNA Integration Sites in Cervical Carcinomas. PloS one. 2013;8:e66693. doi: 10.1371/journal.pone.0066693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khan MJ, Castle PE, Lorincz AT, Wacholder S, Sherman M, Scott DR, et al. The elevated 10-year risk of cervical precancer and cancer in women with human papillomavirus (HPV) type 16 or 18 and the possible utility of type-specific HPV testing in clinical practice. Journal of the National Cancer Institute. 2005;97:1072–9. doi: 10.1093/jnci/dji187. [DOI] [PubMed] [Google Scholar]
- 8.Burk RD, Harari A, Chen Z. Human papillomavirus genome variants. Virology. 2013;445:232–43. doi: 10.1016/j.virol.2013.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guan P, Howell-Jones R, Li N, Bruni L, de Sanjose S, Franceschi S, et al. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. International journal of cancer Journal international du cancer. 2012;131:2349–59. doi: 10.1002/ijc.27485. [DOI] [PubMed] [Google Scholar]
- 10.Rositch AF, Nowak RG, Gravitt PE. Increased age and race-specific incidence of cervical cancer after correction for hysterectomy prevalence in the United States from 2000 to 2009. Cancer. 2014;120:2032–8. doi: 10.1002/cncr.28548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adey A, Burton JN, Kitzman JO, Hiatt JB, Lewis AP, Martin BK, et al. The haplotype-resolved genome and epigenome of the aneuploid HeLa cancer cell line. Nature. 2013;500:207–11. doi: 10.1038/nature12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tommasino M, Accardi R, Caldeira S, Dong W, Malanchi I, Smet A, et al. The role of TP53 in Cervical carcinogenesis. Human mutation. 2003;21:307–12. doi: 10.1002/humu.10178. [DOI] [PubMed] [Google Scholar]
- 13.zur Hausen H, de Villiers EM. Human papillomaviruses. Annual review of microbiology. 1994;48:427–47. doi: 10.1146/annurev.mi.48.100194.002235. [DOI] [PubMed] [Google Scholar]
- 14.Wright AA, Howitt BE, Myers AP, Dahlberg SE, Palescandolo E, Van Hummelen P, et al. Oncogenic mutations in cervical cancer: genomic differences between adenocarcinomas and squamous cell carcinomas of the cervix. Cancer. 2013;119:3776–83. doi: 10.1002/cncr.28288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bruhn MA, Pearson RB, Hannan RD, Sheppard KE. AKT-independent PI3-K signaling in cancer - emerging role for SGK3. Cancer management and research. 2013;5:281–92. doi: 10.2147/CMAR.S35178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vasudevan KM, Barbie DA, Davies MA, Rabinovsky R, McNear CJ, Kim JJ, et al. AKT-independent signaling downstream of oncogenic PIK3CA mutations in human cancer. Cancer cell. 2009;16:21–32. doi: 10.1016/j.ccr.2009.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akagi K, Li J, Broutian TR, Padilla-Nash H, Xiao W, Jiang B, et al. Genome-wide analysis of HPV integration in human cancers reveals recurrent, focal genomic instability. Genome Res. 2014;24:185–99. doi: 10.1101/gr.164806.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ojesina AI, Lichtenstein L, Freeman SS, Pedamallu CS, Imaz-Rosshandler I, Pugh TJ, et al. Landscape of genomic alterations in cervical carcinomas. Nature. 2013 doi: 10.1038/nature12881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chung TK, Van Hummelen P, Chan PK, Cheung TH, Yim SF, Yu MY, et al. Genomic aberrations in cervical adenocarcinomas in Hong Kong Chinese women. International journal of cancer Journal international du cancer. 2015 doi: 10.1002/ijc.29456. [DOI] [PubMed] [Google Scholar]
- 20.Hu Z, Zhu D, Wang W, Li W, Jia W, Zeng X, et al. Genome-wide profiling of HPV integration in cervical cancer identifies clustered genomic hot spots and a potential microhomology-mediated integration mechanism. Nat Genet. 2015;47:158–63. doi: 10.1038/ng.3178. [DOI] [PubMed] [Google Scholar]
- 21.de Roda Husman AM, Walboomers JM, van den Brule AJ, Meijer CJ, Snijders PJ. The use of general primers GP5 and GP6 elongated at their 3′ ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. The Journal of general virology. 1995;76 ( Pt 4):1057–62. doi: 10.1099/0022-1317-76-4-1057. [DOI] [PubMed] [Google Scholar]
- 22.McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome research. 2010;20:1297–303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nature genetics. 2011;43:491–8. doi: 10.1038/ng.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robinson JT, Thorvaldsdottir H, Winckler W, Guttman M, Lander ES, Getz G, et al. Integrative genomics viewer. Nat Biotechnol. 2011;29:24–6. doi: 10.1038/nbt.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samuels Y, Wang Z, Bardelli A, Silliman N, Ptak J, Szabo S, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304:554. doi: 10.1126/science.1096502. [DOI] [PubMed] [Google Scholar]
- 26.Rosty C, Sheffer M, Tsafrir D, Stransky N, Tsafrir I, Peter M, et al. Identification of a proliferation gene cluster associated with HPV E6/E7 expression level and viral DNA load in invasive cervical carcinoma. Oncogene. 2005;24:7094–104. doi: 10.1038/sj.onc.1208854. [DOI] [PubMed] [Google Scholar]
- 27.Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Jr, Kinzler KW. Cancer genome landscapes. Science. 2013;339:1546–58. doi: 10.1126/science.1235122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kandoth C, McLellan MD, Vandin F, Ye K, Niu B, Lu C, et al. Mutational landscape and significance across 12 major cancer types. Nature. 2013;502:333–9. doi: 10.1038/nature12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heselmeyer K, Schrock E, du Manoir S, Blegen H, Shah K, Steinbeck R, et al. Gain of chromosome 3q defines the transition from severe dysplasia to invasive carcinoma of the uterine cervix. Proc Natl Acad Sci U S A. 1996;93:479–84. doi: 10.1073/pnas.93.1.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rudd ML, Price JC, Fogoros S, Godwin AK, Sgroi DC, Merino MJ, et al. A unique spectrum of somatic PIK3CA (p110alpha) mutations within primary endometrial carcinomas. Clin Cancer Res. 2011;17:1331–40. doi: 10.1158/1078-0432.CCR-10-0540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burke JE, Perisic O, Masson GR, Vadas O, Williams RL. Oncogenic mutations mimic and enhance dynamic events in the natural activation of phosphoinositide 3-kinase p110alpha (PIK3CA) Proc Natl Acad Sci U S A. 2012;109:15259–64. doi: 10.1073/pnas.1205508109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gymnopoulos M, Elsliger MA, Vogt PK. Rare cancer-specific mutations in PIK3CA show gain of function. Proc Natl Acad Sci U S A. 2007;104:5569–74. doi: 10.1073/pnas.0701005104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cui B, Zheng B, Zhang X, Stendahl U, Andersson S, Wallin KL. Mutation of PIK3CA: possible risk factor for cervical carcinogenesis in older women. International journal of oncology. 2009;34:409–16. [PubMed] [Google Scholar]
- 34.Menges CW, Baglia LA, Lapoint R, McCance DJ. Human papillomavirus type 16 E7 up-regulates AKT activity through the retinoblastoma protein. Cancer Res. 2006;66:5555–9. doi: 10.1158/0008-5472.CAN-06-0499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang CH, Mandelker D, Schmidt-Kittler O, Samuels Y, Velculescu VE, Kinzler KW, et al. The structure of a human p110alpha/p85alpha complex elucidates the effects of oncogenic PI3Kalpha mutations. Science. 2007;318:1744–8. doi: 10.1126/science.1150799. [DOI] [PubMed] [Google Scholar]
- 36.Mandelker D, Gabelli SB, Schmidt-Kittler O, Zhu J, Cheong I, Huang CH, et al. A frequent kinase domain mutation that changes the interaction between PI3Kalpha and the membrane. Proc Natl Acad Sci U S A. 2009;106:16996–7001. doi: 10.1073/pnas.0908444106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miled N, Yan Y, Hon WC, Perisic O, Zvelebil M, Inbar Y, et al. Mechanism of two classes of cancer mutations in the phosphoinositide 3-kinase catalytic subunit. Science. 2007;317:239–42. doi: 10.1126/science.1135394. [DOI] [PubMed] [Google Scholar]
- 38.Cancer Genome Atlas Research N. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature. 2014;507:315–22. doi: 10.1038/nature12965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Janku F, Wheler JJ, Naing A, Falchook GS, Hong DS, Stepanek VM, et al. PIK3CA mutation H1047R is associated with response to PI3K/AKT/mTOR signaling pathway inhibitors in early-phase clinical trials. Cancer Res. 2013;73:276–84. doi: 10.1158/0008-5472.CAN-12-1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo G, Sun X, Chen C, Wu S, Huang P, Li Z, et al. Whole-genome and whole-exome sequencing of bladder cancer identifies frequent alterations in genes involved in sister chromatid cohesion and segregation. Nat Genet. 2013;45:1459–63. doi: 10.1038/ng.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roberts SA, Lawrence MS, Klimczak LJ, Grimm SA, Fargo D, Stojanov P, et al. An APOBEC cytidine deaminase mutagenesis pattern is widespread in human cancers. Nat Genet. 2013;45:970–6. doi: 10.1038/ng.2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Henderson S, Chakravarthy A, Su X, Boshoff C, Fenton TR. APOBEC-mediated cytosine deamination links PIK3CA helical domain mutations to human papillomavirus-driven tumor development. Cell reports. 2014;7:1833–41. doi: 10.1016/j.celrep.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 43.Lawrence MS, Stojanov P, Mermel CH, Robinson JT, Garraway LA, Golub TR, et al. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature. 2014;505:495–501. doi: 10.1038/nature12912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Henken FE, Banerjee NS, Snijders PJ, Meijer CJ, De-Castro Arce J, Rosl F, et al. PIK3CA-mediated PI3-kinase signalling is essential for HPV-induced transformation in vitro. Mol Cancer. 2011;10:71. doi: 10.1186/1476-4598-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schwarz JK, Payton JE, Rashmi R, Xiang T, Jia Y, Huettner P, et al. Pathway-specific analysis of gene expression data identifies the PI3K/Akt pathway as a novel therapeutic target in cervical cancer. Clin Cancer Res. 2012;18:1464–71. doi: 10.1158/1078-0432.CCR-11-2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boland JF, Chung CC, Roberson D, Mitchell J, Zhang X, Im KM, et al. The new sequencer on the block: comparison of Life Technology’s Proton sequencer to an Illumina HiSeq for whole-exome sequencing. Human genetics. 2013;132:1153–63. doi: 10.1007/s00439-013-1321-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhao L, Vogt PK. Helical domain and kinase domain mutations in p110alpha of phosphatidylinositol 3-kinase induce gain of function by different mechanisms. Proc Natl Acad Sci U S A. 2008;105:2652–7. doi: 10.1073/pnas.0712169105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de la Rochefordiere A, Kamal M, Floquet A, Thomas L, Petrow P, Petit T, et al. PIK3CA pathway mutations predictive of poor response following Standard radio chemotherapy +/− Cetuximab in cervical cancer patients. Clinical cancer research : an official journal of the American Association for Cancer Research. 2015 doi: 10.1158/1078-0432.CCR-14-2368. [DOI] [PubMed] [Google Scholar]
- 49.Roura E, Castellsague X, Pawlita M, Travier N, Waterboer T, Margall N, et al. Smoking as a major risk factor for cervical cancer and pre-cancer: Results from the EPIC cohort. International journal of cancer Journal international du cancer. 2013 doi: 10.1002/ijc.28666. [DOI] [PubMed] [Google Scholar]
- 50.Zhao L, Vogt PK. Hot-spot mutations in p110alpha of phosphatidylinositol 3-kinase (pI3K): differential interactions with the regulatory subunit p85 and with RAS. Cell cycle. 2010;9:596–600. doi: 10.4161/cc.9.3.10599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.