Abstract
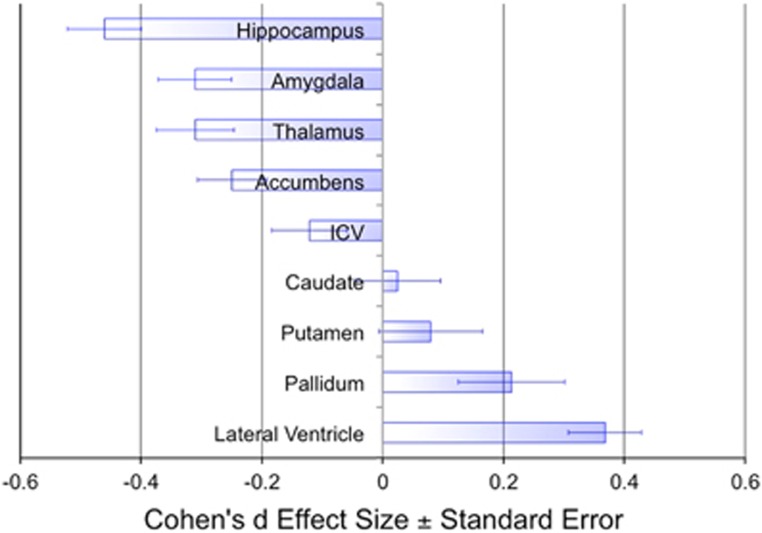
The profile of brain structural abnormalities in schizophrenia is still not fully understood, despite decades of research using brain scans. To validate a prospective meta-analysis approach to analyzing multicenter neuroimaging data, we analyzed brain MRI scans from 2028 schizophrenia patients and 2540 healthy controls, assessed with standardized methods at 15 centers worldwide. We identified subcortical brain volumes that differentiated patients from controls, and ranked them according to their effect sizes. Compared with healthy controls, patients with schizophrenia had smaller hippocampus (Cohen's d=−0.46), amygdala (d=−0.31), thalamus (d=−0.31), accumbens (d=−0.25) and intracranial volumes (d=−0.12), as well as larger pallidum (d=0.21) and lateral ventricle volumes (d=0.37). Putamen and pallidum volume augmentations were positively associated with duration of illness and hippocampal deficits scaled with the proportion of unmedicated patients. Worldwide cooperative analyses of brain imaging data support a profile of subcortical abnormalities in schizophrenia, which is consistent with that based on traditional meta-analytic approaches. This first ENIGMA Schizophrenia Working Group study validates that collaborative data analyses can readily be used across brain phenotypes and disorders and encourages analysis and data sharing efforts to further our understanding of severe mental illness.
Introduction
Achievements based on cooperative analyses of neuroimaging data in severe mental illness trail those in genetics.1, 2, 3 This manuscript presents a first validation of our approach to collectively analyze neuroimaging data via the ENIGMA Schizophrenia Working Group.
Individuals with schizophrenia show significant brain morphological abnormalities, but there is considerable heterogeneity in the effect sizes and patterns of brain differences across studies.4, 5, 6, 7, 8, 9, 10, 11 The study of structural brain abnormalities in schizophrenia can help us understand its causes, progression and even treatment effects. Even so, brain differences are influenced by multiple factors—some with opposing effects. Small studies can yield findings that conflict or are not subsequently replicated. Here, we demonstrate a profile of brain abnormalities based on 15 schizophrenia cohorts worldwide, and rank effect size estimates for subcortical and intracranial brain volume differences between individuals with schizophrenia and healthy controls. We also attempt to identify factors that may contribute to effect size heterogeneity across studies.
Despite early suggestion,6 much collected imaging and associated data does not reside in electronic databases that are easily queried for joint analyses and there are no agreed upon standards for efficient data sharing. Here we report ENIGMA's first analysis of schizophrenia brain morphology using harmonized methods to combine brain volumes across samples. The study provides a proof of concept that prospective analyses of already collected data using similar methods can yield robust findings with sample sizes larger than those achieved via retrospective meta-analyses of published work.
‘Retrospective' meta-analyses—or traditional meta-analyses that pool statistical findings reported in the literature—are invaluable for summarizing the state of research findings and identifying possible sources of heterogeneity; they also yield effect sizes for power calculations. However, in traditional meta-analyses much of the collected data are not fully explored. For instance, Haijma et al.11 identified 119 published studies of schizophrenia that reported on whole brain volumes, but only 9 publications that reported on occipital lobe gray matter volumes. For subcortical structures in particular, 87 publications reported hippocampal volumes, but only 13 reported accumbens volumes. Automated image analysis software, and increasingly efficient global collaborations, now allow for prospective analyses of brain scans worldwide using standardized methods. Prospective mega-analyses require the pooling of individual subject data. In contrast, prospective meta-analyses only require the pooling of specific summary statistics—computed at each participating center. This is highly effective even when participants' consent for individual-level data sharing was not obtained. The power of this approach lies in the consistency of the analyses across data sets rather than the ad hoc aggregation of statistics from the literature. Large-scale analyses using similar methods across cohorts worldwide can also be applied across traditional diagnostic boundaries to yield robust and consistent anatomical fingerprints associated with brain disorders to help formulate improved diagnostic classifications based on both brain and behavioral evaluations.
To validate our approach and address the vast heterogeneity of studies and measures reported, here we estimated and ranked effect sizes for regional brain volume abnormalities in individuals with schizophrenia using the same image analysis, quality assurance and statistical analysis methods across a large number of independently evaluated samples. We also explored effects of available demographics (age at onset, duration of illness, age, chlorpromazine dose equivalents, proportion of second-generation (atypical), first-generation (typical), both or no antipsychotic medication, and severity of positive and negative symptoms) and methodological variables (scanner field strength and FreeSurfer version) on the effect size estimates across studies. Based on the largest schizophrenia brain volume meta-analysis conducted to date,11 we predicted that individuals with schizophrenia would show smaller hippocampus, amygdala, thalamus, accumbens and intracranial volumes (ICVs), as well as larger pallidum and lateral ventricle volumes, compared with healthy controls.
Materials and methods
Study samples
Fifteen worldwide (see Supplementary Figure S1) cross-sectional study samples12, 13, 14, 15, 16, 17, 18, 19, 20, 21 totaling 4568 participants—2028 individuals with schizophrenia and 2540 healthy controls—contributed to the collaborative analysis of subcortical brain volumes via the ENIGMA Schizophrenia Working Group (Supplementary Tables S3a and b). The sample-size-weighted mean age across samples for controls was 31 (range: 23–42) years and for patients 34 (range: 22–43) years. The control and patient samples were on average 52% (range: 38–71%) and 69% male (range: 56–87%). The weighted mean age at onset and duration of illness across the patient groups were 23 (range: 20–29) and 10 (range: 0.8–20) years. The weighted mean total PANSS (Positive and Negative Syndrome Scale), SANS (Scale for the Assessment of Negative Symptoms) and SAPS (Scale for the Assessment of Positive Symptoms) total scores across the samples were 63 (range: 36–90), 24 (range: 15–33) and 18 (range: 8–41) years. For samples that recorded current antipsychotic type and dose, the percentage of patients on second-generation (atypical; 77%), first-generation (typical; 15%), both (3%) or none (5%) was determined and for 11 samples chlorpromazine dose equivalents were computed based on Woods (2005; http://www.scottwilliamwoods.com/files/Equivtext.doc). The size-weighted mean chlorpromazine dose equivalent across the samples was 436 (range: 276–704). Each study sample was collected with participants' written informed consent approved by local Institutional Review Boards. No individual subject imaging or clinical data were shared among the ENIGMA institutions.
Image acquisition and processing
Left and right lateral ventricle, thalamus, caudate, putamen, pallidum, accumbens, hippocampus and amygdala volumes, as well as ICVs, were obtained with FreeSurfer22, 23 (http://surfer.nmr.mgh.harvard.edu) from high-resolution T1-weighted structural brain scans (Supplementary Tables S4 and S4a and o). Details on study type (single site or multisite), scanner vendor/strength/sequence, acquisition parameters and FreeSurfer versions used are provided in Supplementary Table S3b. For quality control, all regions of interest (ROIs) with a volume larger or <1.5 times the interquartile range were identified and visually inspected by overlaying their segmentations on the subjects' anatomical images. Only ROI data for which segmentation was judged accurate upon visual inspection were subjected to statistical analyses (see Supplementary Figure S2 for ROI volume histograms).
Statistical meta-analyses
Group differences for each ROI within each sample were examined using univariate linear regression analysis (R's linear model function lm) predicting the mean of left and right subcortical volumes with group (patient, control). The main analysis (model 1) included sex, age and ICV as covariates. Secondary models excluded ICV (model 2) or ICV, sex and age (model 3; uncorrected means model) covariates. The analysis of ICV was performed with models 2 and 3. Analysis of multiscanner studies (FBIRN, MCIC) included binary dummy covariates for n−1 scanners. For each sample, Cohen's d effect sizes for each ROI and model were computed based on the group contrast t-statistics;24 see Supplementary Information 1 for details. Exploratory analyses examined the effect sizes for left and right hemisphere ROIs separately. Analyses of individual subject data were performed by the site that contributed the sample, using code created within the ENIGMA collaboration. Everyone in the working group had access to statistical results from each site.
Moderator analyses
Meta-regression analyses examined associations between sample demographics (mean age at onset, duration of illness, age, chlorpromazine dose equivalents, proportion of typical, atypical, both or no antipsychotic medication, as well as severity of positive and negative symptoms) and methodology (field strength and FreeSurfer version) and effect sizes across studies. These analyses used a conservative Bonferroni-corrected P-value threshold (P<0.0056). For exploratory purposes and future hypothesis generation, we also report on nominally significant findings (P<0.05; two-tailed, uncorrected).
Power analyses
Sample sizes that achieve 80% power to detect group differences given the presented effect sizes were calculated based on one-tailed t-tests with G*Power Version 3.2.1.25
Results
Ranking group differences in terms of their effect sizes
Compared with controls, individuals with schizophrenia showed significantly smaller hippocampus (mean difference from control mean: −4.10%), amygdala (−3.80%), thalamus (−2.74%), accumbens (−3.69%) and ICVs (−0.30%), as well as larger pallidum (+2.28%) and lateral ventricle volumes (+18.24% see Figure 1 and Table 1). The biggest patient control effect size was observed for smaller hippocampus volume (d=−0.46, P=4.85 × 10−14), followed by larger lateral ventricle volume (d=0.37, P=1.38 × 10-9). Each of these brain structures, except intracranial (P=0.05, two-tailed) and pallidum (P=0.02, two-tailed) volumes, showed group differences at the conservative Bonferroni-corrected threshold of P<0.0056 (two-tailed). Group differences for putamen and caudate volumes were not detectably different from zero. Analysis without ICV as a covariate (model 2) did not substantially alter the effect sizes, or their raking. Analyses of left and right hemisphere volumes showed similar findings as for their mean; removal of age and sex covariates (model 3) lowered all effect sizes (Supplementary Tables S1a and c). Heterogeneity of effect sizes, as measured by the I2 statistic, was moderately high to high for all regions (range: 68–87%). Effect sizes for each sample are provided in Supplementary Figure S3.
Figure 1.
Cohen's d effect sizes±s.e. for regional brain volume differences between Individuals with schizophrenia and healthy controls. Effect sizes for all subcortical volumes depicted were corrected for sex, age and intracranial volume (ICV). The effect size for ICV was corrected for sex and age. The number of independent data points (NSz and NHV) for each region are listed in Table 1.
Table 1. Cohen's d effect sizes by region.
| Cohen's d | P-value | 95% CI | % Difference | N80 | I2 | NSz | NHV | |
|---|---|---|---|---|---|---|---|---|
| Hippocampus | −0.46 | 4.85 × 10−14 | −0.58 to −0.34 | −4.10 | 25 | 71 | 2021 | 2531 |
| Amygdala | −0.31 | 3.59 × 10−7 | −0.43 to −0.19 | −3.80 | 60 | 71 | 2024 | 2535 |
| Thalamus | −0.31 | 1.31 × 10−6 | −0.44 to −0.18 | −2.74 | 60 | 74 | 2022 | 2533 |
| Accumbens | −0.25 | 1.54 × 10−5 | −0.36 to −0.14 | −3.69 | 95 | 68 | 2018 | 2535 |
| ICV | −0.12 | 0.05 | −0.24 to 0.00 | −0.30 | 425 | 73 | 2028 | 2539 |
| Caudate | 0.02 | 0.73 | −0.12 to 0.16 | −0.20 | 15 450 | 79 | 2024 | 2540 |
| Putamen | 0.08 | 0.36 | −0.09 to 0.25 | 0.20 | 962 | 86 | 2023 | 2536 |
| Pallidum | 0.21 | 0.02 | 0.04 to 0.39 | 2.28 | 136 | 87 | 2015 | 2538 |
| Lateral ventricle | 0.37 | 1.38 × 10–9 | 0.25 to 0.49 | 18.24 | 41 | 71 | 2028 | 2539 |
Abbreviations: CI, confidence interval; HV, healthy volunteer; I2, heterogeneity index; ICV, intracranial volume; N80, number of subjects needed in each group for 80% power to detect significant group differences (P<0.05, one-tailed); NSz and NHv, the number of subjects with schizophrenia and healthy volunteers included in the analysis, respectively.
Group contrast (Sz−HV) effect sizes for mean ((left+right)/2) volumes controlling for age, sex and ICV. Effect size for ICV controlling for age and sex.58 % Difference=mean weighted percent difference in volume between patients and controls ((Sz−HV)/HV) × 100%.
Moderator analyses
Moderator analyses use meta-regressions, which examine the effects of moderator variables on meta-analysis effect sizes using regression techniques. Our moderator analyses found that sample means for duration of illness and age were positively associated with putamen (P=0.002, P=0.002, respectively) and pallidum (P=0.0002; P=0.002, respectively) group contrast effect sizes. The sample proportions of medication-naive patients were negatively (P=0.0004) associated with hippocampus group contrast effect sizes (Table 2, Supplementary Tables S2a and m and Supplementary Figure S4).
Table 2. Moderator (meta-regression) analysis P-values.
| Duration of illness | Age | Proportion of unmedicated patients | Difference (Sz−HV), proportion of males | Proportion of second-generation antipsychotics | CPZ dose equivalents | Age of onset | PANSS negative | Scanner field strength | FreeSurfer version | |
|---|---|---|---|---|---|---|---|---|---|---|
| Putamen | 0.002 | 0.001 | 0.49 | 0.11 | 0.14 | 0.48 | 0.53 | 0.34 | 0.24 | 0.23 |
| Pallidum | 0.0002 | 0.002 | 0.58 | 0.69 | 0.52 | 0.68 | 0.15 | 0.96 | 0.82 | 0.10 |
| Hippocampus | 0.57 | 0.11 | 0.003 | 0.22 | 0.52 | 0.20 | 0.02 | 0.49 | 0.54 | 0.16 |
| Lat. ventricle | 0.30 | 0.16 | 0.28 | 0.65 | 0.04 | 0.03 | 0.28 | 0.01 | 0.43 | 0.61 |
| Thalamus | 0.84 | 0.32 | 0.43 | 0.96 | 0.81 | 0.08 | 0.09 | 0.15 | 0.72 | 0.87 |
| Caudate | 0.22 | 0.22 | 0.99 | 0.69 | 0.19 | 0.46 | 0.73 | 0.58 | 0.34 | 0.12 |
| Amygdala | 0.43 | 0.26 | 0.35 | 0.01 | 0.66 | 0.26 | 0.78 | 0.35 | 0.04 | 0.93 |
| Accumbens | 0.15 | 0.13 | 0.40 | 0.007 | 0.30 | 0.21 | 0.66 | 0.073 | 0.17 | 0.22 |
| ICV | 0.78 | 0.89 | 0.43 | 0.70 | 0.85 | 0.06 | 0.40 | 0.087 | 0.19 | 0.45 |
Abbreviations: CPZ, chlorpromazine; HV, healthy volunteers; ICV, intracranial volume; Sz, schizophrenia.
Italic P-values are significant at the Bonferroni-corrected threshold of P<0.0056. Bolded P-values are significant at a nominal P-value of P<0.05 (two-tailed).
At an uncorrected statistical threshold (P<0.05), differences in sample proportions of males (Sz−HV) were negatively associated with accumbens (P=0.007) and amygdala (P=0.01) group contrast effect sizes, sample proportions of patients treated with second-generation antipsychotics were negatively associated with lateral ventricle group contrast effect sizes (P=0.04), sample means of current chlorpromazine dose equivalents were positively associated with lateral ventricle volume group contrast effect sizes (P=0.03), sample means for age of onset were negatively associated with hippocampus group contrast effect sizes (P=0.02), sample means for PANSS-negative symptom severity were negatively associated with lateral ventricle group contrast effect sizes (P=0.01) and scanner field strength (1.5/3 T) was negatively associated with amygdala group contrast effect sizes (P=0.03).
There were no detectable effects of proportion of typical/both antipsychotics, or FreeSurfer version on any of the group contrast effect sizes (all P>0.05; Supplementary Tables S2a and m).
Power analyses
Our sample of 2028 individuals with schizophrenia and 2540 healthy controls provided 80% power to detect Cohen's d effect sizes of 0.084 at P<0.05 (two-tailed) and 0.108 at the conservative Bonferroni-corrected threshold of P<0.0056 (two-tailed). Estimated sample sizes needed, in each group, to achieve 80% power to detect group differences at P<0.05 (one-tailed) across ROIs range from 25 to 15 450 (Table 1).
Discussion
In the largest cooperative analysis to date of brain MRI scans from individuals with schizophrenia, we found that: (1) individuals with schizophrenia, compared with healthy controls, have significantly smaller hippocampus, amygdala, thalamus, accumbens and ICVs, and significantly larger and pallidum and lateral ventricle volumes; (2) the heterogeneity of effect sizes across samples was moderately high to high; (3) putamen and pallidum volume enlargements were associated with duration of illness and age and (4) hippocampal volume deficits were more severe in samples with a higher proportion of unmedicated patients.
The percent volume differences and effect sizes for ICV and subcortical volume abnormalities were small to moderate (−4.10 to 18.24%, Cohen's d=−0.46 to 0.37); patients and controls substantially overlapped in their distributions. The reported effect sizes provide important information for power estimates in schizophrenia imaging studies. The rank order and magnitude of effect sizes across regions here agrees with the largest retrospective meta-analysis performed to date,11 which examined 38 brain structures, analyzed using a variety of different methods, across 382 samples (317 studies) combining data from over 18 000 subjects. The biggest effect size was observed for smaller hippocampus volumes (d=−0.46) followed by larger lateral ventricle volumes (d=0.37) in patients versus controls. Despite FreeSurfer's relatively crude measure of intracranial brain volume, based on registration scaling parameters, our findings agree with other reports of smaller average intracranial brain volumes in individuals with schizophrenia versus controls.4, 11 This is consistent with a role for disturbed brain development in the disorder. The lack of detectable differences in caudate and putamen volumes among individuals with schizophrenia on antipsychotic medications also corroborates the findings by Haijma et al.11 who observed smaller caudate volumes only in medication-naive individuals with schizophrenia compared with controls.
The effect size estimates based on analyses excluding ICV (model 2) as compared to including ICV (model 1) showed the exact same pattern (Supplementary Tables S1a and c). As expected from the lower ICV in patients compared with controls, when not covarying for ICV, the negative effect sizes were slightly more negative and the positive effect sizes were slightly less positive. All effect sizes significant in model 1 remained significant in model 2. Subcortical brain abnormalities are therefore largely independent of intracranial volume. Removing age and sex from the analysis rendered group contrasts for intracranial volume nonsignificant and lowered subcortical volume effect sizes. This is not surprising: removing covariates that explain variance increases error variance, and reduces effect size.
Despite using similar imaging, quality assurance and analysis methods, effect size heterogeneity across the samples was moderately high to high for all regions (I2 range: 60–87%). Indeed, the heterogeneity is even larger than that observed in the largest retrospective meta-analysis.11 Although unexpected, this finding may suggest that prospective meta-analyses, compared with retrospective meta-analyses, show more true variation in effect sizes owing to unselective reporting; the latter may show more restricted variance owing to publication bias.
We found significant positive associations between duration of illness as well as age and putamen and pallidum volume exacerbations in schizophrenia. We also found that hippocampal volume deficits showed a significant negative association with the proportion of unmedicated patients. Meta-regression analyses must be interpreted cautiously, owing to possible confounds (e.g., Simpson's paradox26), but can be useful for hypothesis generation. The positive association between duration of illness and the volumes of the putamen and pallidum may reflect, in part, the cumulative effects of antipsychotic medication treatment on basal ganglia volumes; the association for caudate volume was also positive, although not significant. Several longitudinal studies report that antipsychotic treatments normalize caudate volume deficits observed in medication-naive patients11 and increase putamen volumes.27, 28, 29, 30, 31, 32 Few studies report medication effects in the pallidum. Caudate, putamen and pallidum volume–ICV ratios may predict risperidone treatment effects in individuals with schizophrenia.33 One retrospective meta-analysis suggests that cumulative exposure to antipsychotic treatments is associated with gray matter volume loss,34 but the field would benefit from a prospective meta-analysis of longitudinal studies examining how antipsychotic medications affect brain morphology over time, especially because many studies only report data from a select set of regions.
As duration of illness is highly correlated with age (r14=0.91, P<0.001), we cannot exclude the possibility of disease-related age effects on these regions. The latter interpretation is consistent with independently replicated findings of larger pallidum volumes in unmedicated, non-ill relatives of individuals with schizophrenia. Hence, larger pallidum volumes may be associated with familial (possibly genetic) liability35, 36 (but see Honea et al.37 for a conflicting finding, perhaps reflecting confounding factors). Longitudinal studies of clinically and/or genetically at-risk individuals are needed to examine whether subcortical abnormalities, such as larger pallidum volumes, reflect abnormal developmental trajectories, in the absence of confounding factors (e.g., medications), as suggested by abnormal associations of subcortical volumes with age in adolescents at familial risk for schizophrenia.38
The finding that a larger proportion of unmedicated patients was associated with larger hippocampal volume deficits is surprising and warrants replication. This finding suggests that untreated psychosis may be associated with more severe hippocampus volume deficits and perhaps that hippocampal volume deficits may be partially ameliorated by (atypical) antipsychotic medications. This interpretation is supported by a longitudinal study finding that schizophrenia patients on a cumulative higher dose of atypical antipsychotics showed less decrease or even small increases in hippocampus volumes over time39 and findings of neurogenic effects of atypical but not typical antipsychotics in the hippocampus subgranular zone.40 Notably, the 11 samples included in this meta-regression were predominantly treated with atypical antipsychotics (sample-size-weighted mean=77%).
Our exploratory findings include smaller accumbens (P=0.007) and amygdala (P=0.01) deficits among samples with larger proportions of males in the schizophrenia compared with the control sample. Most neuroimaging studies equate sex distributions between comparison groups and our findings indicate that this may be particularly important when examining accumbens and amygdala volumes. We also found that sample proportions of patients treated with second-generation antipsychotics were associated with smaller lateral ventricle volume enlargement (P=0.04); a finding perhaps consistent with observations of smaller decreases in brain volumes in patients taking second- compared with first-generation antipsychotic medications.41 In contrast, current chlorpromazine dose equivalents were positively associated with lateral ventricle volume exacerbations (P=0.03); the nature of this association remains to be determined. Most unexpected, and in contrast to early findings,42 higher severity of negative symptoms was associated with smaller lateral ventricle volumes (P=0.01). However, we believe that associations between symptom severity and subcortical volumes are best studied within site, followed by between site meta-analyses of the observed within-site beta-weights in particular because no reliability for symptom ratings was established between sites. Such analyses are currently under development for cortical thickness and possible findings for the subcortical volumes will be reported in the planned manuscript. Also unexpected, given prior findings showing opposite effects, is that higher mean age of onset was associated with larger hippocampal volume deficits. This finding may be consistent with larger hippocampus volume deficits in patients with a longer duration of untreated psychosis;43 an interpretation consistent with this study's finding that hippocampal deficits scale with the proportion of unmedicated patients. The only methodological effect observed was that of larger amygdala deficits at higher scanner field strength (3 versus 1.5 T). Brain volume estimates may be more reliable at 3 versus 1.5 T, perhaps due to reduced partial volume effects associated with smaller voxels used at 3T;44 reliabilities for amygdala volumes at 1.5 and 3 T are comparable when the same voxel size is used.45
Strengths of this study include sample sizes of over 2018 patients and 2533 controls for each brain region (Table 1). For measures other than intracranial and hippocampal volumes, this study constitutes the largest meta-analysis of subcortical brain volumes in schizophrenia to date. A second strength is the use of similar image analysis, quality assurance and statistical analysis methods across all brain regions from all 15 contributing studies. Individual studies can maximize their statistical power by restricting analyses to a smaller number of a priori regions of interest, but in prospective meta-analyses participating sites are free to include brain measures that would otherwise remain unexplored.
A similar strategy to the one used in this study has been used in an international mega-analysis of structural imaging in bipolar disorder46 as well as in parallel ENIGMA—Bipolar Disorder (BD) and Major Depressive Disorder Working Group studies, which found significantly smaller hippocampus, amygdala and thalamus, and significantly larger lateral ventricle volumes in bipolar disorder47 and smaller hippocampus volumes in major depressive disorder compared with controls with the latter effect mainly present in individuals with recurrent major depressive disorder and/or with an illness onset before age 22 years.48 Our prospective meta-analyses strategy generates highly significant findings and may be particularly useful in areas where study samples are traditionally small or for which no comprehensive regional assessment of brain morphology has been pursued—for example, high-risk, medication-naive first-episode, longitudinal medication studies, and comparisons across diagnostic boundaries.
This study has some weaknesses. We used the same image analysis package across all samples (FreeSurfer), but a recent study showed effects of FreeSurfer version, workstation vendor and operating system version on brain volume and cortical thickness estimates.49 Here, however, FreeSurfer version did not predict effect sizes across studies for any of the regions examined. Second, the overall sample included a higher proportion of males in the patient (69%) compared with the control group (52%). It is however unlikely that this discrepancy affects our findings because (a) they replicate those of Haijma et al.11 who included only studies matched for sex distribution, and (b) meta-regression predicting effect sizes with group difference in the proportion of males only showed a significant effect for the accumbens and the amygdala, for which a higher proportion of males in the schizophrenia compared with the control group was negatively associated with group contrast effect sizes (P=0.007 and P=0.01, respectively; Table 2 and Supplementary Tables S2a and m). Third, our analysis only examined cross-sectional studies of individuals with schizophrenia and healthy controls and only examined subcortical and intracranial brain volumes. Fourth, apart from disease-related biological factors, numerous confounding environmental factors can influence the volume of brain structures, including fetal hypoxia,50 nutritional and hydration status,51, 52, 53 exercise,54 medications,11 smoking,55 cannabis use,41 social isolation56 and the stress associated with severe mental illness.57 Parsing the contributions of such factors is an ongoing effort within as well as outside the consortium. This is, however, a first validation study for which significant efforts were put forward to grow the consortium and develop a first robust analyses allowing for validation of the approach. Plans for additional analyses of patients' relatives, relationship to more detailed clinical symptoms and the study of additional brain measures (e.g., volume and thickness of cortical ROIs) are under development.
In conclusion, this study shows a robust pattern of subcortical brain abnormalities, suggests that that larger putamen and pallidum volumes may be associated with duration of illness in schizophrenia and suggests that treatment with predominantly second-generation (atypical) antipsychotics may ameliorate hippocampal volume deficits. The consistency between the reported prospective meta-analysis findings and those from traditional retrospective meta-analyses validate the prospective meta-analysis approach. We are in the process applying similar methods to cortical thickness and surface, as well as less well-studied subcortical shape measures. For a review of ongoing efforts and to join the collaborative see http://enigma.ini.usc.edu.
Acknowledgments
For grant support and acknowledgments see Supplementary Information 2.
Author Contributions
Protocol design, quality testing and meta-analysis: DPH, TGMvE, JMR. Data collection, processing, analysis and funding: TGMvE, DPH, JMR, DCG, GDP, OAA, IA, LTW, UKH, AMD, IM, CBH, OG, BK, DZ, GD, SK, CM, DWM, DMC, AC, MWJM, LK, LdH, DJV, TDS, DHW, RCG, REG, SGP, DHM, BAM, AP, FM, SE, EW, JH, VDC, HJB, SRS, JMS, NEMvH, HEHP, RAO, RSK, RR-S, BC-F, LW, KIA, EGJ, RD, CB, HCW, AMM, SML, PMT, JAT; manuscript preparation: TGMvE, JAT and PMT. All authors contributed edits and approved the contents of the manuscript.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Molecular Psychiatry website (http://www.nature.com/mp)
Supplementary Material
References
- Ripke S, Sanders AR, Kendler KS, Levinson DF, Sklar P, Holmans PA et al. Genome-wide association study identifies five new schizophrenia loci. Nat Genet 2011; 43: 969–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoller JW, Craddock N, Kendler K, Lee PH, Neale BM, Nurnberger JI et al. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 2013; 381: 1371–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ripke S, Wray NR, Lewis CM, Hamilton SP, Weissman MM, Breen G et al. A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry 2013; 18: 497–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward KE, Friedman L, Wise A, Schulz SC. Meta-analysis of brain and cranial size in schizophrenia. Schizophr Res 1996; 22: 197–213. [DOI] [PubMed] [Google Scholar]
- Nelson MD, Saykin AJ, Flashman LA, Riordan HJ. Hippocampal volume reduction in schizophrenia as assessed by magnetic resonance imaging: a meta-analytic study. Arch Gen Psychiatry 1998; 55: 433–440. [DOI] [PubMed] [Google Scholar]
- Wright IC, Rabe-Hesketh S, Woodruff PW, David AS, Murray RM, Bullmore ET. Meta-analysis of regional brain volumes in schizophrenia. Am J Psychiatry 2000; 157: 16–25. [DOI] [PubMed] [Google Scholar]
- Zakzanis KK, Poulin P, Hansen KT, Jolic D. Searching the schizophrenic brain for temporal lobe deficits: a systematic review and meta-analysis. Psychol Med 2000; 30: 491–504. [DOI] [PubMed] [Google Scholar]
- Vita A, De Peri L, Silenzi C, Dieci M. Brain morphology in first-episode schizophrenia: a meta-analysis of quantitative magnetic resonance imaging studies. Schizophr Res 2006; 82: 75–88. [DOI] [PubMed] [Google Scholar]
- Adriano F, Spoletini I, Caltagirone C, Spalletta G. Updated meta-analyses reveal thalamus volume reduction in patients with first-episode and chronic schizophrenia. Schizophr Res 2010; 123: 1–14. [DOI] [PubMed] [Google Scholar]
- Shepherd AM, Laurens KR, Matheson SL, Carr VJ, Green MJ. Systematic meta-review and quality assessment of the structural brain alterations in schizophrenia. Neurosci Biobehav Rev 2012; 36: 1342–1356. [DOI] [PubMed] [Google Scholar]
- Haijma SV, Van Haren N, Cahn W, Koolschijn PC, Hulshoff Pol HE, Kahn RS. Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects. Schizophr Bull 2012; 39: 1129–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo-Facorro B, Roiz-Santianez R, Perez-Iglesias R, Tordesillas-Gutierrez D, Mata I, Rodriguez-Sanchez JM et al. Specific brain structural abnormalities in first-episode schizophrenia. A comparative study with patients with schizophreniform disorder, non-schizophrenic non-affective psychoses and healthy volunteers. Schizophr Res 2009; 115: 191–201. [DOI] [PubMed] [Google Scholar]
- Pelayo-Teran JM, Perez-Iglesias R, Ramirez-Bonilla M, Gonzalez-Blanch C, Martinez-Garcia O, Pardo-Garcia G et al. Epidemiological factors associated with treated incidence of first-episode non-affective psychosis in Cantabria: insights from the Clinical Programme on Early Phases of Psychosis. Early Interv Psychiatry 2008; 2: 178–187. [DOI] [PubMed] [Google Scholar]
- Machielsen MW. Schizophrenia and Comorbid Cannabis Use Disorders. Ph.D. Thesis University of Amsterdam: Amsterdam, Netherlands, 2014. [Google Scholar]
- McIntosh AM, Job DE, Moorhead TW, Harrison LK, Forrester K, Lawrie SM et al. Voxel-based morphometry of patients with schizophrenia or bipolar disorder and their unaffected relatives. Biol Psychiatry 2004; 56: 544–552. [DOI] [PubMed] [Google Scholar]
- Gollub RL, Shoemaker JM, King MD, White T, Ehrlich S, Sponheim SR et al. The MCIC collection: a shared repository of multi-modal, multi-site brain image data from a clinical investigation of schizophrenia. Neuroinformatics 2013; 11: 367–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulshoff Pol HE, Schnack HG, Bertens MG, van Haren NE, van der Tweel I, Staal WG et al. Volume changes in gray matter in patients with schizophrenia. Am J Psychiatry 2002; 159: 244–250. [DOI] [PubMed] [Google Scholar]
- Boos HB, Cahn W, van Haren NE, Derks EM, Brouwer RM, Schnack HG et al. Focal and global brain measurements in siblings of patients with schizophrenia. Schizophr Bull 2012; 38: 814–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trost S, Platz B, Usher J, Scherk H, Wobrock T, Ekawardhani S et al. DISC1 (disrupted-in-schizophrenia 1) is associated with cortical grey matter volumes in the human brain: a voxel-based morphometry (VBM) study. J Psychiatr Res 2013; 47: 188–196. [DOI] [PubMed] [Google Scholar]
- Gruber O. Neuroimaging markers: their role for differential diagnosis and therapeutic decisions in personalized psychiatry. Nervenarzt 2011; 82: 1404, 1406, 1408, passim. [DOI] [PubMed] [Google Scholar]
- Wang L, Kogan A, Cobia D, Alpert K, Kolasny A, Miller MI et al. Northwestern University Schizophrenia Data and Software Tool (NUSDAST). Front Neuroinform 2013; 7: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 2002; 33: 341–355. [DOI] [PubMed] [Google Scholar]
- Fischl B. FreeSurfer. Neuroimage 2012; 62: 774–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa S, Cuthill IC. Effect size, confidence interval and statistical significance: a practical guide for biologists. Biol Rev Camb Philos Soc 2007; 82: 591–605. [DOI] [PubMed] [Google Scholar]
- Erdefelder E, Faul F, Buchner A. GPOWER: a general power analysis porgram. Behav Res Methods Instrum Comput 1996; 28: 1–11. [Google Scholar]
- Goltz HH, Smith ML. Yule–Simpson's paradox in research. Pract Assess Res Eval 2010; 15: 1–9. [Google Scholar]
- Gur RE, Maany V, Mozley PD, Swanson C, Bilker W, Gur RC. Subcortical MRI volumes in neuroleptic-naive and treated patients with schizophrenia. Am J Psychiatry 1998; 155: 1711–1717. [DOI] [PubMed] [Google Scholar]
- Glenthoj A, Glenthoj BY, Mackeprang T, Pagsberg AK, Hemmingsen RP, Jernigan TL et al. Basal ganglia volumes in drug-naive first-episode schizophrenia patients before and after short-term treatment with either a typical or an atypical antipsychotic drug. Psychiatry Res 2007; 154: 199–208. [DOI] [PubMed] [Google Scholar]
- Hulshoff Pol HE, Kahn RS. What happens after the first episode? A review of progressive brain changes in chronically ill patients with schizophrenia. Schizophr Bull 2008; 34: 354–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M, Chen Z, Deng W, He Z, Wang Q, Jiang L et al. Volume increases in putamen associated with positive symptom reduction in previously drug-naive schizophrenia after 6 weeks antipsychotic treatment. Psychol Med 2011; 42: 1475–1483. [DOI] [PubMed] [Google Scholar]
- Boonstra G, van Haren NE, Schnack HG, Cahn W, Burger H, Boersma M et al. Brain volume changes after withdrawal of atypical antipsychotics in patients with first-episode schizophrenia. J Clin Psychopharmacol 2011; 31: 146–153. [DOI] [PubMed] [Google Scholar]
- Ho BC, Andreasen NC, Ziebell S, Pierson R, Magnotta V. Long-term antipsychotic treatment and brain volumes: a longitudinal study of first-episode schizophrenia. Arch Gen Psychiatry 2011; 68: 128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutcheson NL, Clark DG, Bolding MS, White DM, Lahti AC. Basal ganglia volume in unmedicated patients with schizophrenia is associated with treatment response to antipsychotic medication. Psychiatry Res 2014; 221: 6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Smieskova R, Kempton MJ, Ho BC, Andreasen NC, Borgwardt S. Progressive brain changes in schizophrenia related to antipsychotic treatment? A meta-analysis of longitudinal MRI studies. Neurosci Biobehav Rev 2013; 37: 1680–1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oertel-Knochel V, Knochel C, Matura S, Rotarska-Jagiela A, Magerkurth J, Prvulovic D et al. Cortical-basal ganglia imbalance in schizophrenia patients and unaffected first-degree relatives. Schizophr Res 2012; 138: 120–127. [DOI] [PubMed] [Google Scholar]
- Yang Y, Nuechterlein KH, Phillips OR, Gutman B, Kurth F, Dinov I et al. Disease and genetic contributions toward local tissue volume disturbances in schizophrenia: a tensor-based morphometry study. Hum Brain Mapp 2012; 33: 2081–2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honea RA, Meyer-Lindenberg A, Hobbs KB, Pezawas L, Mattay VS, Egan MF et al. Is gray matter volume an intermediate phenotype for schizophrenia? A voxel-based morphometry study of patients with schizophrenia and their healthy siblings. Biol Psychiatry 2008; 63: 465–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty MK, Gu H, Bizzell J, Ramsey S, Gerig G, Perkins DO et al. Differences in subcortical structures in young adolescents at familial risk for schizophrenia: a preliminary study. Psychiatry Res 2012; 204: 68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koolschijn PC, van Haren NE, Cahn W, Schnack HG, Janssen J, Klumpers F et al. Hippocampal volume change in schizophrenia. J Clin Psychiatry 2010; 71: 737–744. [DOI] [PubMed] [Google Scholar]
- Newton SS, Duman RS. Neurogenic actions of atypical antipsychotic drugs and therapeutic implications. CNS Drugs 2007; 21: 715–725. [DOI] [PubMed] [Google Scholar]
- Van Haren NE, Cahn W, Hulshoff Pol HE, Kahn RS. Confounders of excessive brain volume loss in schizophrenia. Neurosci Biobehav Rev 2013; 37: 2418–2423. [DOI] [PubMed] [Google Scholar]
- Pearlson GD, Garbacz DJ, Breakey WR, Ahn HS, DePaulo JR. Lateral ventricular enlargement associated with persistent unemployment and negative symptoms in both schizophrenia and bipolar disorder. Psychiatry Res 1984; 12: 1–9. [DOI] [PubMed] [Google Scholar]
- Penttila M, Jaaskelainen E, Haapea M, Tanskanen P, Veijola J, Ridler K et al. Association between duration of untreated psychosis and brain morphology in schizophrenia within the Northern Finland 1966 Birth Cohort. Schizophr Res 2010; 123: 145–152. [DOI] [PubMed] [Google Scholar]
- Brouwer RM, Hulshoff Pol HE, Schnack HG. Segmentation of MRI brain scans using non-uniform partial volume densities. Neuroimage 2010; 49: 467–477. [DOI] [PubMed] [Google Scholar]
- Jovicich J, Czanner S, Han X, Salat D, van der Kouwe A, Quinn B et al. MRI-derived measurements of human subcortical, ventricular and intracranial brain volumes: Reliability effects of scan sessions, acquisition sequences, data analyses, scanner upgrade, scanner vendors and field strengths. Neuroimage 2009; 46: 177–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallahan B, Newell J, Soares JC, Brambilla P, Strakowski SM, Fleck DE et al. Structural magnetic resonance imaging in bipolar disorder: An International Collaborative Mega-analysis of Individual Adult Patient Data. Biol Psychiatry 2011; 69: 326–335. [DOI] [PubMed] [Google Scholar]
- Hibar DP Robust subcortical volumetric reductions in bipolar disorder: findings from the ENIGMA bipolar disorder working group including 1,745 cases and 2,613 controls. Proc Natl Acad Sci USA (submitted).
- Schmaal L Subcortical brain volume abnormalities in major depressive disorder: prospective meta-analytic findings from the ENIGMA Major Depressive Disorder Working Group including 1,808 cases and 7,223 controls. Proc Natl Acad Sci USA (submitted).
- Gronenschild EH, Habets P, Jacobs HI, Mengelers R, Rozendaal N, van Os J et al. The effects of FreeSurfer version, workstation type, and Macintosh operating system version on anatomical volume and cortical thickness measurements. PLoS One 2012; 7: e38234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Erp TG, Saleh PA, Rosso IM, Huttunen M, Lonnqvist J, Pirkola T et al. Contributions of genetic risk and fetal hypoxia to hippocampal volume in patients with schizophrenia or schizoaffective disorder, their unaffected siblings, and healthy unrelated volunteers. Am J Psychiatry 2002; 159: 1514–1520. [DOI] [PubMed] [Google Scholar]
- King JA, Geisler D, Ritschel F, Boehm I, Seidel M, Roschinski B et al. Global cortical thinning in acute anorexia nervosa normalizes following long-term weight restoration. Biol Psychiatry 2014; 77: 624–632. [DOI] [PubMed] [Google Scholar]
- Duning T, Kloska S, Steinstrater O, Kugel H, Heindel W, Knecht S. Dehydration confounds the assessment of brain atrophy. Neurology 2005; 64: 548–550. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Brown RA, Araujo D, Narayanan S, Arnold DL. Correlation between brain volume change and T2 relaxation time induced by dehydration and rehydration: implications for monitoring atrophy in clinical studies. Neuroimage Clin 2014; 6: 166–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajonk FG, Wobrock T, Gruber O, Scherk H, Berner D, Kaizl I et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry 2010; 67: 133–143. [DOI] [PubMed] [Google Scholar]
- Schneider CE, White T, Hass J, Geisler D, Wallace SR, Roessner V et al. Smoking status as a potential confounder in the study of brain structure in schizophrenia. J Psychiatr Res 2014; 50: 84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabricius K, Helboe L, Steiniger-Brach B, Fink-Jensen A, Pakkenberg B. Stereological brain volume changes in post-weaned socially isolated rats. Brain Res 2010; 1345: 233–239. [DOI] [PubMed] [Google Scholar]
- Mondelli V, Pariante CM, Navari S, Aas M, D'Albenzio A, Di Forti M et al. Higher cortisol levels are associated with smaller left hippocampal volume in first-episode psychosis. Schizophr Res 2010; 119: 75–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.