Abstract
Class III malocclusions are considered to be one of the most difficult problems to treat. Establishment of the treatment plan is based on the efficacy and thoughtful application by the clinician and easy acceptance by the patient. We are presenting a case report of an adult male patient with skeletal Class III malocclusion who was treated by orthosurgical approach in Department of Orthodontics in collaboration with Department of Oral and Maxillofacial Surgery. The treatment was complete with a positive overbite and acceptable occlusion and satisfactory facial esthetics using a combination approach.
Keywords: Class III malocclusion, orthodontics, surgical, treatment outcome
INTRODUCTION
Etiologically Class III malocclusions are multifactorial which includes genetic[1,2] and environmental factors. Class III malocclusions are considered to be one of the most difficult problems to treat orthodontically.[3] The presentation of Class III malocclusions are generally classified into two categories: Skeletal and dental. Various features of skeletal Class III malocclusion include either maxillary retrusion or mandibular prognathism or combination of both consummated with vertical and transverse problems apart from sagittal malformations. The features of dental Class III include canines and molars in Class III relation, anterior crossbites, and reverse overjet. The diagnosis is important due to the different treatment approaches.[4,5,6] In general, a dental Class III can be treated with orthodontics alone while a true skeletal Class III with compromised facial esthetics and varying dentofacial deformity and impaired function requires a combination of orthodontics and surgery.[3,7,8] The contribution of jaw bases to malocclusion in all the three-dimensions along with varying degree of dentoalveolar and soft tissue compensations must be thoroughly evaluated.[4,5,9] Establishment of the treatment plan is based on the efficacy and thoughtful application by the clinician and easy acceptance by the patient.
A developing skeletal Class III malocclusion is one of the most challenging problems confronting the practicing orthodontists and the results are controversial. For patients with psuedo Class III malocclusion, early orthopedic treatment can correct the existing or developing skeletal, dentoalveolar, and muscular imbalances and improve the oral environment and facial esthetics.[1,2] In subjects with true Class III malocclusion, however, early orthopedic correction is bound to relapse. Hence in such cases, the orthosurgical approach has to be employed, once the mandibular growth is complete. The mandibular growth continues even after pubertal spurt. Hence, surgery should be deferred to after that phase.[9]
This case report presents orthosurgical management of an adult patient with skeletal Class III malocclusion.
DIAGNOSIS AND ETIOLOGY
A 27-year-old male patient reported to the Department of Orthodontics, BBDCODS, Lucknow with the chief complaint of forwardly placed lower front teeth and impaired speech that has led to low confidence levels in him.
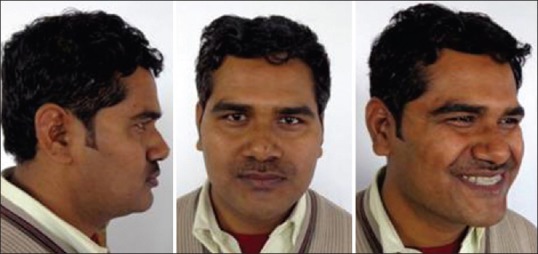
Clinical frontal examination revealed a grossly symmetrical face with mesoprosopic facial form, no incisal show at rest and half of the incisors could be seen on smiling. The profile assessment revealed concave profile with anterior facial divergence, deficient midface, flat cheekbone contour, orthognathic maxilla, and prognathic mandible with protrusive lower lip and low mandibular plane angle. Figure 1 shows extraoral pretreatment photographs whereas Figure 2 shows intraoral photographs. Intraoral examination revealed good periodontal health with symmetrical arches, spacing in the maxillary arch and minor crowding in the mandibular arch with Class III molar and canine relation on both the sides. The mandibular midline was shifted to right by 1 mm and reverse overjet of 3 mm and an overbite of 4 mm were recorded. Scissors bite was observed with respect to 24, 35.
Figure 1.
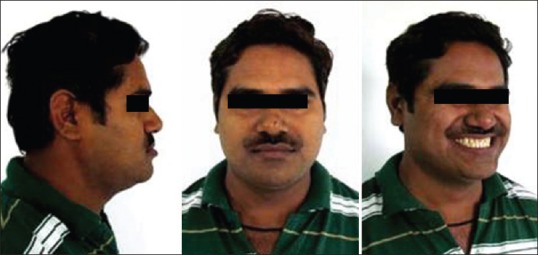
Pretreatment extraoral photographs
Figure 2.

Pretreatment intraoral photographs
Temporomandibular joint examination did not reveal any discrepancy between centric relation and/centric occlusion and patient did not complain of pain or clicking in the joint.
Cephalometric examination revealed retrognathic maxilla, prognathic mandible, with horizontal growth pattern and proclined maxillary incisors and retroclined mandibular incisors. Table 1 gives details of cephalometeric examination. Mild vertical deficiency was evident. Soft tissue examination on lateral cephalogram revealed concave profile, increased nasal prominence, normal nasolabial angle, increased upper lip thickness, and protrusive lower lip. Good soft tissue thickness camouflaged the retrognathic maxilla. Figure 3 shows pretreatment radiographs of the patient.
Table 1.
Cephalometric summary
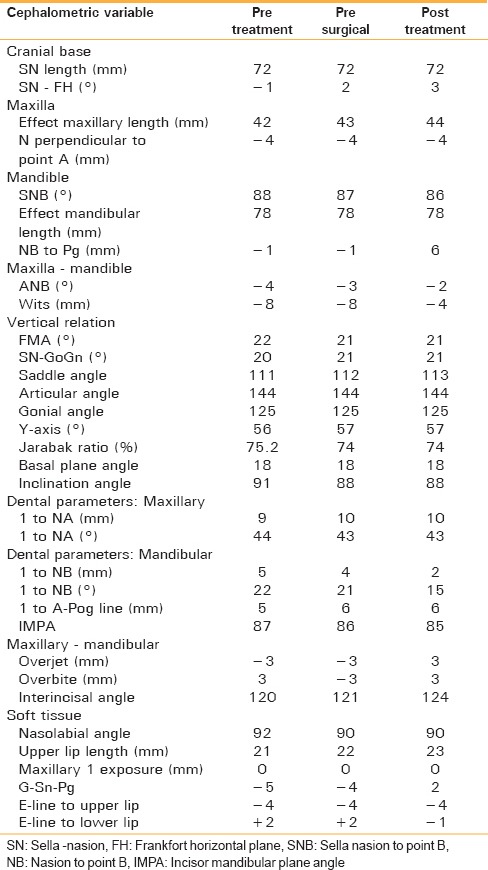
Figure 3.

Pretreatment radiographs
A panoramic radiograph showed that all teeth were present including the third molars. There were no supernumerary teeth. The crown-root ratios were normal with good alveolar bone levels, no bone pathology, mandibular condyles, nasal floor, and maxillary sinuses appeared normal.
TREATMENT OBJECTIVES
Attain a pleasing profile by reducing the prominence of lower jaw
To relieve post-crossbite
Alignment of both the arches with proper angulations of all the teeth
Achieving acceptable static and functional occlusion
To correct inadequate incisor show.
TREATMENT ALTERNATIVES
As per prediction tracing, on dental decompensation of the respective arches, reverse overjet was increased to 8 mm, suggesting a combination of maxillary advancement and mandibular setback being the first treatment option. Since the soft tissue camouflage was excellent in the maxillary anterior region, hence maxillary advancement procedure was not considered
The mandibular setback alone by bilateral sagittal split osteotomy was ruled out due to good buccal occlusion, that would have disturbed thereafter
Mandibular subapical osteotomy with extraction of first premolars and setting the anterior back in that space would be the third alternative that will not disturb posterior occlusion
This option was selected for the patient and was discussed with him before finalizing the treatment plan with Department of Oral and Maxillofacial Surgery of our college.
TREATMENT PROGRESS
This will be discussed under three headings as follows:
Presurgical orthodontic phase
Surgical phase
Postsurgical orthodontic phase.
Presurgical orthodontic phase
The presurgical phase was initiated with bonding brackets and banding first molars with 0.022 inch slot MBT preadjusted edgewise appliance. The nonextraction treatment approach was follwed initially and the maxillary and mandibular arches were aligned using 0.016 inch Ni-Ti arch wires, which were followed by progressively heavier archwires, such as 0.018 inch self-esteem. For this reason, 0.017 inch × 0.025 inch stainless steel and finally 0.019 inch × 0.025 inch and 0.021 × 0.025 stainless steel. Minor spaces in maxillary arch were consolidated during the course of treatment. Crossbite with respect to 24 and 35 was corrected.
Before surgery upper and lower co-ordinated 0.019 inch × 0.025 inch stainless steel wires were left passively in place for 4 weeks following which presurgical records were taken.
The mock surgery was performed after removing mandibular first premolars on the cast and setting the mandibular anterior segment back so as to evaluate postsurgical results.
Figure 4 shows patients model mounted for mock surgery. Figure 5 shows presurgical radiographs of the patient.
Figure 4.
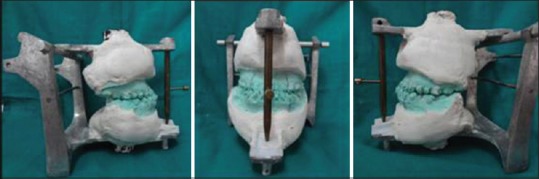
Patients model mounted for mock surgery
Figure 5.

Presurgical radiographs
Surgical orthodontic phase
The surgery was done in Department of Oral and Maxillofacial Surgery. During surgery, mandibular first premolars were extracted and mandibular subapical osteotomy was done in the anterior segment, then mandible was set back in the extraction space to achieve positive overjet. The mandible was stabilized with surgical bone plates that were placed at the osteotomy site. The intermaxillary fixation was done with the help of stabilizing wires. Figure 6a shows the photograph of the surgical site with a bone plate in place whereas Figure 6b shows the chunk of bone removed to set the mandible back.
Figure 6.
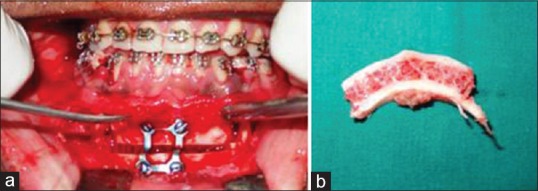
(a) Surgical site with bone plates, (b) Chunk of removed bone
Postsurgical orthodontic phase
Figures 7–9 shows postsurgical records of the patient. Four weeks postsurgery, the stabilizing arch wires were removed. Minor extraction spaces that were left were closed. Postsurgical leveling and final detailing were achieved with 0.014 inch stainless steel archwires and settling elastics. Total treatment time was 28 months. As the molar tube was broken for a right mandibular first molar, single tooth crossbite was seen on that side as patient had to shift to Delhi, he was not ready for its correction. After taking consent from the patient, he was debonded and records were taken. The upper and lower retainers were fitted. Figures 10 and 11 shows debonded extraoral and intraoral photographs of the patient. Figure 12 shows radiographs of the patient taken after debonding.
Figure 7.
Post surgical extraoral photographs
Figure 9.

Postsurgical radiographs
Figure 10.

Posttreatment extraoral photographs
Figure 11.

Posttreatment intraoral photographs
Figure 12.

Posttreatment radiographs
Figure 8.

Post surgical intraoral photographs
TREATMENT RESULTS
Most of the treatment objectives were achieved and facial esthetics definitely improved and lower lip attained normal profile anterior crossbite was corrected. Figure 13 shows superimposition of stage radiographs.
Figure 13.
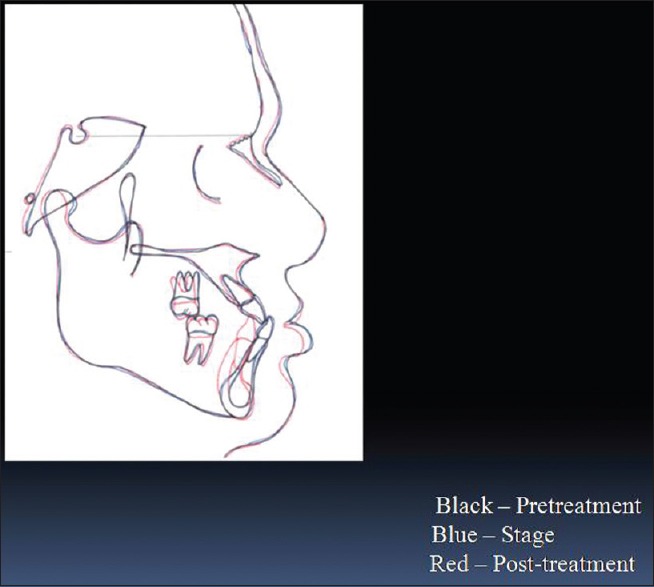
Cephalometric superimposition
DISCUSSION
In cases of severe dentofacial deformity in skeletal Class III malocclusion, orthosurgical approach is must.[3,7,8] The final facial profile after surgery is of great significance as it results in a dramatic change in the appearance of the patient that can psychologically boost up or deteriorate his self-esteem. For this reason, diagnosis and proper treatment planning must be given added weightage.[4,5,6]
There is a paradigm shift in diagnosis with stress on soft tissue examination in whose light hard tissue deviations must be viewed.[1]
In this patient, a nonextraction treatment approach was used presurgically so as to achieve alignment and leveling of the arches leaving less of correction to be done orthodontically during postsurgical phase.
Clinically after surgery, patient should be satisfied, with normal static and functional occlusion, patient should be comfort able while chewing, and should possess stability of results achieved.
CONCLUSION
The carefully planned presurgical phase with skillfully done surgery and adequate detailing during postsurgical phase, keeping patients expectations in mind will bring desired results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Footnotes
Source of Support: Nil.
Conflicts of Interest: None declared.
REFERENCES
- 1.Profit WR. Profit WR, White RP, Jr, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St Louis: CV Mosby; 2003. The development of dentofacial deformity: Influence and etiological factor. [Google Scholar]
- 2.Litton SF, Ackermann LV, Isaacson RJ, Shapiro BL. A genetic study of Class 3 malocclusion. Am J Orthod. 1970;58:565–77. doi: 10.1016/0002-9416(70)90145-4. [DOI] [PubMed] [Google Scholar]
- 3.Mendiratta A, Mesquita AA, Kamat NV, Dhupar V. Orthosurgical management of severe class III malocclusion. J Indian Orthod Soc. 2014;48:273–9. [Google Scholar]
- 4.Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod Dentofacial Orthop. 1993;103:299–312. doi: 10.1016/0889-5406(93)70010-L. [DOI] [PubMed] [Google Scholar]
- 5.Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning – Part II. Am J Orthod Dentofacial Orthop. 1993;103:395–411. doi: 10.1016/s0889-5406(05)81791-3. [DOI] [PubMed] [Google Scholar]
- 6.Epker BN, Stella JP, Fish LC, editors. St Louios, MO: Mosby Year Book; 1986. Dentofacial Deformities. Integrated Orthodontic and Surgical Correction. [Google Scholar]
- 7.Stojanovic LS, Mileusnic I, Mileusnic B, Cutovic T. Orthodontic-surgical treatment of the skeletal class III malocclusion: A case report. Vojnosanit Pregl. 2013;70:215–20. doi: 10.2298/vsp1302215s. [DOI] [PubMed] [Google Scholar]
- 8.Khan MB, Karra A. Severe skeletal class III orthosurgical correction. J Orofac Res. 2013;3:274–9. [Google Scholar]
- 9.Graber TM. 3rd ed. Philadelphia: WB Saunders Company; 2001. Orthodontic Principle and Practice. [Google Scholar]


