Abstract
Given the increasing popularity of dental implants, the number of failures due to late implant fracture is also expected to increase. Hence, the scope for prevention and management needs to be emphasized. The objective of this review article is to analyze the various causes of failure of dental implants due to implant fixture/abutment screw fractures and also to enumerate the management and the preventive options for these failures, thereby aiming to help the clinicians to properly plan the implant-supported prosthesis treatment by considering the important biomechanical aspects of this type of rehabilitation. The present review emphasizes the causes and management of technical complications and not the incidence of such complications.
Keywords: Abutment screw fracture, implant failure, implant fixture fracture
INTRODUCTION
Given the increasing popularity of dental implants, an increase in the number of failures due to late fractures, that is, post successful osseointegration, is expected.
The failure of dental implants is due not only to biological factors, such as unsuccessful osseointegration or the presence of periimplantitis, butthey also result from technical complications thatinvolve implant body/fixture fracture, abutment screw fracture, abutment fracture, fractured prosthesis, etc.
The failure of an implant as a single entity, irrespective of its components, may be classified as early or late. Early failures occur shortly after surgery and are characterized by the lack of osseointegration. In contrast, late failures correspond to those implants that have been regarded as successful for some time, and they occur after prostheticrestoration has been made. There are two main causes for late implant fracture:
Mechanical problems, including fractures— Metal fatigue, due to biomechanical overloading, appears to be the most frequent cause[1,2]
Loss of supporting tissue secondary to infection or periimplantitis— The prevalence of periimplantitis is estimated to be 4-15% among the surviving implant population (i.e., implants still in the mouth).
The present review discusses the various technical/mechanical complications related to the restorative aspect of the dental implant-based restorations. However, to solve these complications, one needs to understand the mechanics of such components. This paper would entail the causes, mechanics, prevention, and management of such component-related complications.
Implant fixture fracture
Various researchers have listed the causes of implant fractures, but there is no universally accepted classification so far. There are two main causes of implant fracture: (a) Mechanical overloads leading to metal fatigue. When the resistance limit is exceeded, it results in a fracture. Overload can also be a consequence of the patient's physiological alterations (e.g., para functional activity). In effect, both centric and eccentric bruxism can lead to implant overload and metal fatigue. Other overload-related factors are of prosthetic origin, including inadequate occlusion, the presence of distal extensions or cantilevers in implant-supported prostheses, and a lack of prosthetic passive fit over the implants.[1,3,4,5,6] (b) Peri implant vertical bone loss is attributable to both chronic peri implant inflammation and occlusal trauma. When vertical bone loss coincides with the apical limit of the screw, thereby joining trans epithelial abutment to implant, the risk of implant fracture increases drastically.[1,3,4,7,8] The implant may also fracture due to defects in implant design and manufacturing.[9] Metal fractures are related to microstructures that influence the material properties. They are related to the localized identification of chemical phases and segregations, frequently associated with failures at interfaces or components, which in turn can cause the fractures.[10]
Incidence/location of implant fracture
The incidence of dental implant fracture is between 0.16-1.5%, as reported in the literature.[2,3,4,9,10,11,12,13,14,15,16] One study reported that the majority of fractured implants are located in the regions of the molars and premolars,[3,9,17] and that the fractures were evenly distributed between the maxilla and the mandible,[9] whereas another study reported more fractures in the maxilla than in the mandible.[17]
Diameter of implant
Implants with small diameters such as 4 mm[17] and 3.75 mm[9,10] tend to fracture more easily than those with large diameters, especially when placed in a posterior location. A study has reported that an implant with a diameter of 5.0 mm is three times stronger than one with a diameter of 3.75 mm, whereas a 6.0-mm implant is six times stronger than a 3.75-mm implant.[18]
Mechanism of implant fracture
The specific bone loss pattern seen in implant fracture cases has been described as a primary cause and a mechanism of fracture.[3,19,20] Coronal bone resorption increases the bending stress of the implant because of the loss of supporting bone,[21] which usually extends to the level corresponding to the end of the abutment screw, there by reducing the resistance to bending in this region. When such reabsorption extends apically beyond the third implant thread, it reaches a structurally weak zone coinciding with the end of the prosthetic screw and the border of the hybrid surface. This contributes to the fatigue at a point of low resistance to torque. The warning signs of such fatigue include loosening, torsion, or fracture of the post screws, and ceramic fractures of the prosthesis.
Clinical manifestations
Patients may often report spontaneous bleeding and mobility. Exploration (manually or electronically) confirms increased mobility, increased pocket depth, and gingival indexes, and occasionally, also, plaque accumulation resulting from the patient's fear of the pain is triggered by brushing. Radiologically, separation of the fragments and bone loss may be seen. It has been reported that marginal bone reabsorption seems to be the most important risk factor indicating the start of an implant fracture, and may often extend beyond the actual fracture line.[9] Thus, an x-ray study is very useful.
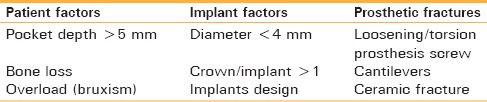
For diagnostic purposes, the fracture risk factors[22] have been grouped into three main categories [Table 1]. In the presence of more than three factors pertaining to one or more of these categories, the risk of fracture is high.
Table 1.
Clinical findings frequently documented in the literature and related to implant fracture, grouped by categories
MANAGEMENT
There are three management options in the event of an implant fracture:[9,23]
Complete removal of the fractured implant using explantation trephines.[9,23] After the removal of the fractured implant, a new larger diameter implant can be installed at the same surgical bed or at another placeto achieve primary stability.[20] Their complete removal is considered to be the best solution to the problem
Removal of the coronal portion of the fractured implant with the purpose of placing a new prosthetic post.[9,23] It is essential to radiologically confirm the absence of radio transparency and to electronically determine the mobility of the fragment. A prosthetic post should be considered only if there is still sufficient remaining internal thread retention[9]
Removal of the coronal portion of the fractured implant, leaving the remaining apical part integrated in the bone.[9,23] and the missing tooth/teeth can be restored using conventional prosthodontic procedures like removable partial denture, fixed partial denture etc.
A recent study described “apicoectomy” as a suitable technique for removing fractured implants and inserting new implants at the same clinical session. This technique was based on opening a hole in the bone in order to improve the visualization of the apical fragments of the fractured implants and to remove those fragments through this hole. Afterward, a new implant is placed in a conventional manner, and the hole is closed by using the same bone that is removed from the patient.[24]
Preventive measures
The following preventive measures have been suggested:
Avoid placing hybrid-type implant fixtures
Carefully control occlusal forces: Eliminate all posterior contacts in mandibular eccentric movements
Perform staggered placement of implants: Avoid a straight-line configuration
Avoid or minimize posterior cantilevers and buccolingual offsets, particularly in partially edentulous patients
During the chronic loosening of gold or abutment screws or the fracture of components, critically reassess the prosthesis, retighten the abutment or usea gold screw, and check the fit
Pronounced bruxers or clenchers who have experienced multiple implant fractures should be managed by the placement of additional implants fractures[17]
Ensure perfect fit: Resolder and assess passive fit.[25]
Implant-abutment connection system
The misfit at the abutment-implant interface and the absence of a passive adaptation between the prosthesis and the abutment can lead to fracture and the most common technical complication in implants is a fracture of the abutment screw.
The stability of the implant abutment connection is influenced by factors such as internal connection versus external connection, screw head design, screw geometry, materials, screw diameter, preload, joint separating force, settling effect, and overall screw mechanics.
Factors affecting the implant-abutment connection system are as follows:
Internal connection versus external connection
The implant-abutment interface connection is generally described as an internal or external connection. Relative to external connections, the internal implant-abutment connections have been shown to present a higher stability and improved force distribution as a result of not only their ability to dissipate lateral loads deeply within the implant, there by shielding the abutment screw better from stress, but also due to the longer internal wall engagement that creates a stiff, unified body to resist joint opening (micro movement).[26,27,28,29] However, there is another aspect to stronger internal abutment connection after cyclic loading relative to external connections.[30,31,32] While mechanical strength is gained, the thinner lateral fixture wall at the connecting part of the internal connections may lead to a higher absolute strain value at the cervical area.[31] Such stress shift has raised concerns regarding an increased risk of marginal bone resorption or fixture fracture.[31]
Although there are studies that show that the fracture strength in implant systems with an external fixation is equal or superior to those with internal fixation.[33,34]
The literature supports a gold alloy screw with a flat head, internal hex or square, and a high tightening force (torque driver) as having the greatest ability to produce the best results.[35]
Screw head design
To maximize the preload and minimize the loss of input torque to friction, the head of the screw should be wider than the thread diameter. An abutment head most often should be flat. A tapered head design reduces the clamping effect and reduces the tensile force in the threads of the screw. The tapered screw head distorts and aligns non passive components and gives a non passive casting the appearance of proper fit. However, the superstructure is not deformed permanently and leads to stress in the system. A flat-head screw distributes forces more evenly within the threads and the head of the screw, and is also less likely to distort a non passive casting. As such, the abutment head should also be flat on top to increase the clamping force in the screw head and the tensile force in the threads.[36]
Screw material
The most commonly used retaining screws are either of gold or titanium. Gold screws are designed to be the most “flexible” portion of the implant assembly. Due to their higher modulus of elasticity than titanium, they permit an adequate micro movement to distribute force to the implant body.[37] Implant posts, that are retained with gold or gold coated screws, show a reduction of screw loosening and improved clamping force in comparison with titanium screws.[38,39,40]
Titanium alloy has four times the bending fracture resistance of grade 1 titanium. Therefore, abutment screws made of grade 1 titanium will deform and fracture more easily than the alloy. A higher torque magnitude can be used on the titanium alloy abutment screw and female component (implant body).[36] Titanium retaining screws are stronger than gold, but have a lower modulus of elasticity; metal fatigue will produce a gold screw fracture before the titanium retaining screw is affected.[37] The major disadvantage of titanium retaining screws is their tendency to cause galling, which results in excessive friction between the two mating surfaces there by causinga localized welding with a further roughening of the mating surfaces.[41] Galling occurs in the following manner: Titanium of the retainings crew slides in contact with the titanium of the implant body, the coefficient of friction increases whereby titanium molecules transfer from the mating surfaces.[42] This has been described as the adhesive wear mechanism[43] which causes slight damage to both the implant body and the retaining screw threads.
Screw diameter
The greater the diameter, the higher the preload that may be applied and the greater the clamping force on the screw joint. As a general rule, abutment screws loosen less often and can take a higher preload than coping screws.[44]
Preload
The screw joint has been described as two parts tightened together by a screw, such as an abutment and implant being held together by a screw. A screw is tightened by applying torque. The applied torque develops a force within the screw called the preload.[40] As a screw is tightened, it elongates, thereby producing tension. Elastic recovery of the screw pulls the two parts together, creating a clamping force.[45] Excessive forces cause slippage between the threads of the screw and the threads of the bone, resulting in the loss of the preload.[46]
Adequate preload of the screw creates less micromotion of the implant-abutment screw interface and less screw loosening.[45,47,48,49] Pre loading the screw improves the fatigue resistance and the locking effect of the abutment/implant connection. The preload should fluctuate as little as possible to prevent loosening. Occlusal forces, which result in the loading of implant supported prostheses, will cause changes in the preload of the abutment screws that may result in loosening of the screws.[50]
Joint separating forces
Intra oral separating forces may include off-axis occlusal contacts, lateral excursive contacts, interproximal contacts between natural teeth and implant restorations, protrusive contacts, para functional forces, and non passive frameworks that attach to the implants. Opposing the clamping force is a joint-separating force, which attempts to separate the screw joint. Screw loosening occurs when the joint-separating forces acting on the screw joint are greater than the clamping forces holding the screw unit together.[40]
Settling effect
Settling occurs as the rough spot interfaces flatten under load/micro movements, since they are the only contacting surfaces when the initial tightening torque is applied.[51] It has been reported that 2-10% of the initial preload is lost as a result of settling.[52] This reduction effect is known as embedment relaxation.[53]
Process of screw loosening
The process of screw loosening has been described in two stages.[54] Initially, external forces such as mastication applied to the screw joint causes slippage, contributing to the release of preload of the screw. The second stage of loosening involves continual preload reduction below critical level, allowing threads to turn and the loss of intended screw joint junction.[55]
Incidence of screw loosening
A literature review of clinical complications of osseo integrated implants showed that screw loosening or screw fracture varied 2-45% of the implant restorations, with the highest amount in single crowns.[4] In one of the systematic reviews that evaluated the 5-year survival rates of implant-supported single crowns, it was observed that from the 26 clinical studies included, the cumulative incidence of abutment screw or abutment loosening was 7.3% after 5 years of clinical service in both external and internal connections.[56]
Location of screw loosening
Posterior abutment screws loosen at a higher percentage than anterior implants. This supports the project of eliminating unnecessary occlusal and off-axial forces on implant-supported restorations.[35] One of the studies have reporteda 38% loosening of single implant restorations in the posterior maxilla and mandible,[57] but such studies do not take into account various important factors.
Preventive management
It is recommended in clinical practice that in order to reduce the settling effect, the implant screws should be retightened 10 min after the initial torque application.[50,58,59,60,61]
Mechanical torque gauges should be used instead of hand drivers to ensure a consistent tightening of the implant components to recommended torque values.[51]
The use of sealers to fill in the gaps between thes crews and implant threads and adhesives to in creasethe frictional resistance has been suggested to reduce screw loosening. (Ceka Bond, Preat, San Mateo, CA) is listed as an adhesive paste on the package insert.[50]
One study of screw loosening supported the following clinical recommendations: (a) Ensure that implants are placed perpendicular to the occlusal plane; (b) frameworks should have minimal cantilever lengths; (c) use components with low tolerance levels for component misfit; and (d) use components with anti rotational features for single tooth restorations.[35]
Management of fractured abutment screw
This mainly involves two options: Either retrieve the fractured screw, or remove the old implant and insert a new implant in one sitting.
The retrieval of the fractured abutment screw can be done by the following means:
Artery forceps: If the fractured part is above the head of the implant, then it can be unscrewed with the help of artery forceps[62]
Ultrasonic scaler: If the fractured part cannot be grasped with any instrument, then use ultrasonic vibrations to disengage the threads. The oscillations from an ultrasonic scaler can gradually reverse the screw out by placing a thin tip of an ultrasonic scaler directly on the top of the screw[63]
Lubricant: Lubricate the damaged screw before unscrewing it. Add a few drops of eugenol, handpiece lubricant, or even mineral oil in the area, and then try to remove the screw with a probe or ultrasonic scaler in a counter clockwise direction
Contra angle low speed: Using a 1/4 round bur in a contra angle low speed running in a reverse mode could help spin the screw out. The small round drill acts as a screwdriver and holds the head of the fragment[63]
Repair or rescue kit: Used when the site of the abutment fracture is deep. The kit consists of drills, drill guides, and tapping instruments. Some kits repair the implant by unscrewing the fractured fragment, while others cut into splinters
Be indigenous: If the fractured end is not too deep then prepare a 1-mm slot across the most occlusal portion of the broken screw fragment with the help of a diamond bur and handpiece. Hold the handpiece firmly to avoid having the bur inadvertently jump into the implant body. Use an appropriate-sized “mini” screwdriver available at local hardware stores to remove the screw.
A clinical report describes utilizing the non retrievable fractured abutment screw by fabricating the post/core. For this, modify the screw hole and fabricate a post crown after radiographically checking the osseo integration status of the implant.[64]
CONCLUSION
In the present review, in order to present a complete picture, various clinical as well as in vitro studies on the mechanics of implant fixture fracture and abutment screw loosening/fracture of a single implant-abutment connection have been reviewed. The incidence of such complications is very small and the literature is still not conclusive concerning the choice of connection and/or crown-retaining system. However, understanding the mechanics of these failures will help the clinicians in formulating a more predictable treatment.
Footnotes
Source of Support: Nil.
Conflicts of Interest: None declared.
REFERENCES
- 1.Piattelli A, Scarano A, Piattelli M, Vaia E, Matarasso S. Hollow implants retrieved for fracture: A light and scanning electron microscope analysis of 4 cases. J Periodontol. 1998;69:185–9. doi: 10.1902/jop.1998.69.2.185. [DOI] [PubMed] [Google Scholar]
- 2.Tolman DE, Laney WR. Tissue-integrated prosthesis complications. Int J Oral Maxillofac Implants. 1992;7:477–84. [PubMed] [Google Scholar]
- 3.Rangert B, Krogh PH, Langer B, Van Roekel N. Bending overload and implant fracture: A retrospective clinical analysis. Int J Oral Maxillofac Implants. 1995;10:326–34. [PubMed] [Google Scholar]
- 4.Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999;81:537–52. doi: 10.1016/s0022-3913(99)70208-8. [DOI] [PubMed] [Google Scholar]
- 5.Kronström M, Svenson B, Hellman M, Persson GR. Early implant failures in patients treated with Brånemarksystem titanium dental implants: A retrospective study. Int J Oral Maxillofac Implants. 2001;16:201–7. [PubMed] [Google Scholar]
- 6.Flanagan D. External and occlusal trauma to dental implants and a case report. Dent Traumatol. 2003;19:160–4. doi: 10.1034/j.1600-9657.2003.00144.x. [DOI] [PubMed] [Google Scholar]
- 7.Sánchez-Gárces MA, Gay-Escoda C. Periimplantitis. Med Oral Patol Oral Cir Bucal. 2004;9(Suppl):63–74. [PubMed] [Google Scholar]
- 8.Uribe R, Peñarrocha M, Sanchis JM, García O. Marginal peri-implantitis due to occlusal overload. A case report. Med Oral. 2004;9:159–62. [PubMed] [Google Scholar]
- 9.Balshi TJ. An analysis and management of fractured implants: A clinical report. Int J Oral Maxillofac Implants. 1996;11:660–6. [PubMed] [Google Scholar]
- 10.Eckert SE, Meraw SJ, Cal E, Ow RK. Analysis of incidence and associated factors with fractured implants: A retrospective study. Int J Oral Maxillofac Implants. 2000;15:662–7. [PubMed] [Google Scholar]
- 11.Jemt T, Lekholm U. Oral implant treatment in posterior partially edentulous jaws: A 5-year follow-up report. Int J Oral Maxillofac Implants. 1993;8:635–40. [PubMed] [Google Scholar]
- 12.Naert I, Quirynen M, van Steenberghe D, Darius P. A study of 589 consecutive implants supporting complete fixed prostheses. Part II: Prosthetic aspects. J Prosthet Dent. 1992;68:949–56. doi: 10.1016/0022-3913(92)90557-q. [DOI] [PubMed] [Google Scholar]
- 13.Gunne J, Jemt T, Lindén B. Implant treatment in partially edentulous patients: A report on prostheses after 3 years. Int J Prosthodont. 1994;7:143–8. [PubMed] [Google Scholar]
- 14.Lekhom U, van Steenberghe D, Herrmann I, Bolender C, Folmer T, Gunne J, et al. Osseo integrated implants in the treatment of partially edentulous jaws: A prospective 5-year multicenter study. Int J Oral Maxillofac Implant. 1994;9:627–35. [Google Scholar]
- 15.Pylant T, Triplett RG, Key MC, Brunsvold MA. A retrospective evaluation of endosseous titanium implants in the partially edentulous patient. Int J Oral Maxillofac Implants. 1992;7:195–202. [PubMed] [Google Scholar]
- 16.Piattelli A, Scarano A, Piattelli M. Histologic observations on 230 retrieved dental implants: 8 years’ experience (1989-1996) J Periodontol. 1998;69:178–84. doi: 10.1902/jop.1998.69.2.178. [DOI] [PubMed] [Google Scholar]
- 17.Kwon K, Sim K, Cha J, Kim E, Lee J. Clinical and scanning electron microscopic analysis of fractured dental implants: A retrospective clinical analysis. J Korean Assoc Oral Maxillofac Surg. 2012;38:371–8. [Google Scholar]
- 18.Proceedings of the 4th International Symposium on Implant Dentistry: Focus on Esthetics. San Diego, California, January 27-29, 1994. Abstracts. J Prosthet Dent. 1994;72:623–34. [PubMed] [Google Scholar]
- 19.Muroff FI. Removal and replacement of a fractured dental implant: Case report. Implant Dent. 2003;12:206–10. doi: 10.1097/01.id.0000084168.57434.f1. [DOI] [PubMed] [Google Scholar]
- 20.Gargallo Albiol J, Satorres-Nieto M, Puyuelo Capablo JL, Sánchez Garcés MA, Pi Urgell J, Gay Escoda C. End osseous dental implant fractures: An analysis of 21 cases. Med Oral Patol Oral Cir Bucal. 2008;13:E124–8. [PubMed] [Google Scholar]
- 21.Morgan MJ, James DF, Pilliar RM. Fractures of the fixture component of an osseo integrated implant. Int J Oral Maxillofac Implants. 1993;8:409–14. [PubMed] [Google Scholar]
- 22.Sánchez-Pérez A, Moya-Villaescusa MJ, Jornet-Garcia A, Gomez S. Etiology, risk factors and management of implant fractures. Med Oral Patol Oral Cir Bucal. 2010;15:e504–8. doi: 10.4317/medoral.15.e504. [DOI] [PubMed] [Google Scholar]
- 23.Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991;6:270–6. [PubMed] [Google Scholar]
- 24.Gealh WC, Mazzo V, Barbi F, Camarini ET. Osseo integrated implants fracture: Causes and treatment. J Oral Implantol. 2010;37:499–503. doi: 10.1563/AAID-JOI-D-09-00135.1. [DOI] [PubMed] [Google Scholar]
- 25.Santos MD, Pfeifer AB, Silva MR, Sendyk CL, Sendyk WR. Fracture of abutment screw supporting a cemented implant-retained prosthesis with external hexagon connection: A case report with sem evaluation. J Appl Oral Sci. 2007;15:148–51. doi: 10.1590/S1678-77572007000200015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Binon PP. Implants and components: Entering the new millennium. Int J Oral Maxillofac Implants. 2000;15:76–94. [PubMed] [Google Scholar]
- 27.Finger IM, Castellon P, Block M, Elian N. The evolution of external and internal implant/abutment connections. Pract Proced Aesthet Dent. 2003;15:625–32. quiz 634. [PubMed] [Google Scholar]
- 28.Sailer I, Sailer T, Stawarczyk B, Jung RE, Hämmerle CH. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int J Oral Maxillofac Implants. 2009;24:850–8. [PubMed] [Google Scholar]
- 29.Da Silva EF, Pellizzer EP, QuinelliMazaro JV, Garcia Júnior IR. Influence of the connector and implant design on the implant-tooth-connected prostheses. Clin Implant Dent Relat Res. 2010;12:254–62. doi: 10.1111/j.1708-8208.2009.00161.x. [DOI] [PubMed] [Google Scholar]
- 30.Khraisat A, Stegaroiu R, Nomura S, Miyakawa O. Fatigue resistance of two implant/abutment joint designs. J Prosthet Dent. 2002;88:604–10. doi: 10.1067/mpr.2002.129384. [DOI] [PubMed] [Google Scholar]
- 31.Maeda Y, Satoh T, Sogo M. In vitro differences of stress concentrations for internal and external hex implant-abutment connections: A short communication. J Oral Rehabil. 2006;33:75–8. doi: 10.1111/j.1365-2842.2006.01545.x. [DOI] [PubMed] [Google Scholar]
- 32.Steinebrunner L, Wolfart S, Ludwig K, Kern M. Implant-abutment interface design affects fatigue and fracture strength of implants. Clin Oral Implants Res. 2008;19:1276–84. doi: 10.1111/j.1600-0501.2008.01581.x. [DOI] [PubMed] [Google Scholar]
- 33.Balfour A, O’Brien GR. Comparative study of anti rotational single tooth abutments. J Prosthet Dent. 1995;73:36–43. doi: 10.1016/s0022-3913(05)80270-7. [DOI] [PubMed] [Google Scholar]
- 34.Möllersten L, Lockwandt D, Lindén LA. Comparison of strength and failure mode of seven implant systems: An in vitro test. J Prosthet Dent. 1997;78:582–91. doi: 10.1016/s0022-3913(97)70009-x. [DOI] [PubMed] [Google Scholar]
- 35.Cho SC, Small PN, Elian N, Tarnow D. Screw loosening for standard and wide diameter implants in partially edentulous cases: 3- to 7-year longitudinal data. Implant Dent. 2004;13:245–50. doi: 10.1097/01.id.0000140459.87333.f8. [DOI] [PubMed] [Google Scholar]
- 36.Shetty M, Krishna Prasad D, Shetty NH, Jaiman R. Implant abutment connection: Biomechanical Perspectives. NUJHS. 2014;4:47–53. [Google Scholar]
- 37.Weinberg LA. The biomechanics of force distribution in implant-supported prostheses. Int J Oral Maxillofac Implants. 1993;8:19–31. [PubMed] [Google Scholar]
- 38.Scholander S. A retrospective evaluation of 259 single-tooth replacements by the use of Brånemark implants. Int J Prosthodont. 1999;12:483–91. [PubMed] [Google Scholar]
- 39.Jörnéus L, Jemt T, Carlsson L. Loads and designs of screw joints for single crowns supported by osseointegrated implants. Int J Oral Maxillofac Implants. 1992;7:353–9. [PubMed] [Google Scholar]
- 40.McGlumphy EA, Mendel DA, Holloway JA. Implant screw mechanics. Dent Clin North Am. 1998;42:71–89. [PubMed] [Google Scholar]
- 41.AlJabbari Y, Fournelle R, Ziebert G, Toth J, Iacopino A. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 2: Metallurgical and micro hardness analysis. J Prosthodont. 2008;17:181–91. doi: 10.1111/j.1532-849X.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 42.Martin WC, Woody RD, Miller BH, Miller AW. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J Prosthet Dent. 2001;86:24–32. doi: 10.1067/mpr.2001.116230. [DOI] [PubMed] [Google Scholar]
- 43.AlJabbari Y, Fournelle R, Ziebert G, Toth J, Iacopino AM. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 1: Characterization of adhesive wear and structure of retaining screws. J Prosthodont. 2008;17:168–80. doi: 10.1111/j.1532-849X.2007.00265.x. [DOI] [PubMed] [Google Scholar]
- 44.Misch C. Principles for abutment and prosthetic screws and screw-retained components and prostheses. In: Misch CE, editor. Dental Implant Prosthetics. 2nd ed. San Luis: Elsevier Mosby; 2014. 730 pp. [Google Scholar]
- 45.Haack JE, Sakaguchi RL, Sun T, Coffey JP. Elongation and preload stress in dental implant abutment screws. Int J Oral Maxillofac Implants. 1995;10:529–36. [PubMed] [Google Scholar]
- 46.Lang JA, May KB, Wang RF. The effect of the use of a counter-torque device on the abutment-implant complex. J Prosthet Dent. 1999;81:411–7. doi: 10.1016/s0022-3913(99)80007-9. [DOI] [PubMed] [Google Scholar]
- 47.Patterson EA, Johns RB. Theoretical analysis of the fatigue life of fixture screws on osseo integrated dental implants. Int J Oral Maxillofac Implants. 1992;7:26–33. [PubMed] [Google Scholar]
- 48.Burquete RL, Johns RB, King T, Patterson EA. Tightening characteristics for screwed joints in osseo integrated dental implants. J Prosthet Dent. 1994;71:592–9. doi: 10.1016/0022-3913(94)90443-x. [DOI] [PubMed] [Google Scholar]
- 49.Gratton DG, Aquilino SA, Stanford CM. Micromotion and dynamic fatigue properties of the dental implant-abutment interface. J Prosthet Dent. 2001;85:47–52. doi: 10.1067/mpr.2001.112796. [DOI] [PubMed] [Google Scholar]
- 50.Breeding LC, Dixon DL, Nelson EW, Tietge JD. Torque required to loosen single-tooth implant abutment screws before and after simulated function. Int J Prosthodont. 1993;6:435–9. [PubMed] [Google Scholar]
- 51.Winkler S, Ring K, Ring JD, Boberick KG. Implant screw mechanics and the settling effect: An over view. J Oral Implantol. 2003;29:242–5. doi: 10.1563/1548-1336(2003)029<0242:ISMATS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 52.Sakaguchi RL, Borgersen SE. Nonlinear contact analysis of preload in dental implant screws. Int J Oral Maxillofac Implants. 1995;10:295–302. [PubMed] [Google Scholar]
- 53.Shigley IE, Mischkc CR. 1st ed. New York: McGraw Hill; 1986. Standard Handbook of Machine Design; pp. 23–26. [Google Scholar]
- 54.Bickford JH. New York: Marcel Dekker; 1981. An introduction to the Design and Behaviour of Bolted Joints; pp. 175–268. [Google Scholar]
- 55.Wiskott HW, Nicholls JI, Belser UC. Stress fatigue: Basic principles and prosthodontic implications. Int J Prosthodont. 1995;8:105–16. [PubMed] [Google Scholar]
- 56.Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res. 2008;19:119–30. doi: 10.1111/j.1600-0501.2007.01453.x. [DOI] [PubMed] [Google Scholar]
- 57.Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: A retrospective study. J Prosthet Dent. 1995;74:51–5. doi: 10.1016/s0022-3913(05)80229-x. [DOI] [PubMed] [Google Scholar]
- 58.Fugazzotto PA, Kirsch A, Ackermann KL, Neuendorff G. Implant/Tooth connected restorations utilizing screw -fixed attachements: A survey of 3,096 sites in function for 3 to 14 years. Int J Oral Maxillofac Implants. 1999;14:819–23. [PubMed] [Google Scholar]
- 59.Begoña Ormeachea M, Millstein P, Hirayama H. Tube angulation effect on radiographic analysis of the implant-abutment interface. Int J Oral Maxillofac Implants. 1999;14:77–85. [PubMed] [Google Scholar]
- 60.Bakaeen LG, Winkler S, Neff PA. The effect of implant diameter, restoration design, and occlusal table variations on screw loosening of posterior single-tooth implant restorations. J Oral Implantol. 2001;27:63–72. doi: 10.1563/1548-1336(2001)027<0063:TEOIDR>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 61.Siamos G, Winkler S, Boberick KG. Relationship between implant preload and screw loosening on implant-supported prostheses. J Oral Implantol. 2002;28:67–73. doi: 10.1563/1548-1336(2002)028<0067:TRBIPA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 62.Reyhanian A, Parker S, Moshonov J, Fuhrman N. The use of Er: YAG in laser-assisted broken abutment screw treatment. Case report_Er: YAG. Lasers. 2010;3:6–11. [Google Scholar]
- 63.Pow EH, Leung KC. Prosthodontic complications in dental implant therapy. Hong Kong Dent J. 2008;5:79–83. [Google Scholar]
- 64.Pow EH, Wat PY. A technique for salvaging an implant-supported crown with a fractured abutment screw. J Prosthet Dent. 2006;95:169–70. doi: 10.1016/j.prosdent.2005.12.005. [DOI] [PubMed] [Google Scholar]


