Abstract
African Americans have an increased risk of cardiovascular disease partly due to low fruit and vegetable consumption. This article reports the results of an intervention to provide nutrition education and access to fruits and vegetables through community gardens to change dietary behaviors among African Americans in rural Missouri. Cross-sectional surveys evaluated the intervention effect on blood pressure, body mass index (BMI), and perceived fruit and vegetable consumption in this quasi-experimental study with a comparison group. Hypertension (OR = 0.52, 95% CI: 0.38–0.71) and BMI (OR = 0.73, 95% CI: 0.52–1.02) were lower in the intervention county at mid-intervention. Participation in nutrition education (OR = 2.67, 95% CI: 1.63–4.40) and access to fruits and vegetables from a community garden (OR = 1.95, 95% CI: 1.20–3.15) were independently associated with perceived fruit and vegetable consumption. The strongest effect on perceived fruit and vegetable consumption occurred with high participation in nutrition education and access to community gardens (OR = 2.18, 95% CI: 1.24–3.81). Those with access but without education had a reduced likelihood of consuming recommended servings of fruits and vegetables (OR = 0.57, 95% CI: 0.34–0.95). Education plus access interventions may be best at increasing consumption of fruits and vegetables in a rural African American population.
Introduction
Cardiovascular disease (CVD) is a leading cause of morbidity and mortality in rural African American populations [1, 2]. African Americans are twice as likely as non-Hispanic Whites to die of preventable CVD [3]. Obesity and hypertension, two modifiable CVD risk factors, are higher among African Americans [4–8] and those living in rural areas [9, 10]. There is evidence to suggest that fruit and vegetable consumption is associated with decreased body mass index (BMI) [11, 12], hypertension [13, 14] and heart disease [15, 16]. Only 30% of African Americans meet recommendations for fruit consumption (two or more servings a day) and 20% for vegetable consumption (three or more servings a day) [17]. In comparison, 31% of non-Hispanic Whites meet recommendations for fruit consumption and 27% meet recommendations for vegetable consumption [17].
Fruit and vegetable consumption is influenced by individual characteristics and social, cultural and physical environments [18]. Dietary interventions addressing the individual level through nutrition education have shown some success [19–21] yet, a recent review indicates that individual education alone is costly and unlikely to have the desired effects in the absence of policies and environments that enable individuals to make healthy choices [22]. At the environmental level, local access and availability of fruits and vegetables is associated with fruit and vegetable consumption. Areas with greater density of supermarkets, convenience stores and restaurants with availability of a wide variety of fruits and vegetables have higher fruit and vegetable consumption [23–29]. Community gardens [30–32] and farmers’ markets [31, 33] also are associated with higher fruit and vegetable consumption. The Institute of Medicine, the National Institutes of Health and several recent studies all emphasize the importance of interventions that include individual and environmental components to improve dietary behavior [4, 34–38].
Interventions that address individual and environmental factors are particularly important for low income, African American communities which have less access to healthy foods and healthier food that exist are more expensive than energy dense foods high in saturated fat and sugar [39]. However, evidence of the effectiveness of interventions that address individual and environmental factors to support fruit and vegetable consumption is still emerging [21].
The purpose of this study is to present the mid-intervention results of Men on the Move Growing Communities (MOTMGC) an intervention with African Americans in rural Missouri that incorporates nutrition education plus food access. Disseminating mid-intervention findings is important because it provides evidence of participants’ short-term health changes when exposed to a community-wide intervention addressing nutrition education plus food access.
Materials and methods
This study was approved by Saint Louis University and Washington University in St. Louis Institutional Review Boards.
Study setting
Pemiscot County in rural, southeast Missouri has 18 111 residents [40]. It contains two town centers, Caruthersville (6168 residents) and Hayti (3565 residents). A quarter (26.9%) of Pemiscot County residents are African American and approximately 3500 are African American adults aged 18 years or older [40]. Approximately 30% of residents live below poverty, 18% have less than a high school education, and the unemployment rate is 10.4% [40]. Pemiscot County has one of the highest CVD mortality rates in Missouri (348.0 per 100 000 in Pemiscot County versus 196.4 per 100 000 for Missouri) [41]. In 2009, Pemiscot County’s CVD mortality rate was nearly 70% higher than the national rate [1, 41].
Dunklin County was used as a comparison county because it is geographically adjacent to Pemiscot County in the southeast corner of Missouri, and it has similar population sociodemographics and CVD rates. Dunklin has two town centers, Kennett (10 932 residents) and Malden (4275 residents) [40]. Approximately 25% of residents live in poverty, 18% have less than a high school education, and the unemployment rate is 9.5% [40]. Like Pemiscot County, Dunklin County is in Missouri’s worst quintile for CVD mortality (253.7 per 100 000) [41]. The United States Department of Agriculture (USDA) Food Environment Atlas indicates that the number of grocery stores located in Pemiscot (0.4/1000 residents) and Dunklin County (0.5/1000 residents) is similar [42]. No intervention activities were conducted in Dunklin County.
Intervention components
A community-based participatory research approach was used to design, implement and evaluate MOTMGC. Community partners included community advocates, elected officials and church leaders, whereas academic partners represented public health and nutrition. MOTMGC built on community strengths including an existing community garden. All partners were involved in all major project decisions.
MOTMGC used the social cognitive theory (SCT) [43] with emphasis on reciprocal determinism, self-regulation and behavioral capability to guide intervention activities at the individual and environmental levels. At the individual level, community advocates conducted culturally appropriate nutrition education activities to enhance knowledge and skills. These activities were based on REACH [Reach for larger vegetable portions, Eat less salt (sodium), Aim to eat more fruits and vegetables every day, Choose to season your vegetables with less fat and Hunt for a variety of fruits and vegetables—use color as a guide]. The REACH messages were developed by nutrition and public health academic partners with community partner input and integrate information from Dietary Approaches to Stop Hypertension [44], the Therapeutic Lifestyle Change Model [45] and the American Heart Association’s dietary guidelines [46].
The nutrition education activities included cooking demonstrations, goal setting, family dinner nights, taste tests and bulletin boards. Each nutrition education activity incorporated at least one REACH message, information about CVD risk factors and a culturally tailored recipe highlighting the REACH message of the day. Community advocates conducted a series of five REACH cooking demonstrations at churches and community centers. Participants and their family members prepared and ate a REACH-inspired meal during a Family Dinner Night and took ingredients with them to prepare the meal at home. Taste tests provided community members an opportunity to try a REACH recipe at a grocery store or community venue. Bulletin boards displayed REACH messages, tips and recipes in physicians’ offices and community sites around the county. Roughly 10% (n = 360) of the eligible population (n = 3500) [40] participated in at least one cooking demonstration, family dinner night or taste test.
MOTMGC increased access to healthy food at the environmental level by expanding an existing community garden and developing three new production gardens. Community participants grew and harvested fruits and vegetables in the community garden, whereas MOTMGC staff provided maintenance. A trained community advocate and four garden staff developed and maintained the production gardens and distributed the produce. MOTMGC grew over 1800 pounds of produce including green beans, carrots, collard greens, corn, cucumbers, mustard greens, onions, okra, various peppers, sweet potatoes, tomatoes, squash, pumpkins and watermelon by mid-intervention (two growing seasons). Produce from the community garden was free to all community members, whereas produce from the production gardens was sold weekly between June and August at two locations.
Study design to evaluate MOTMGC effect
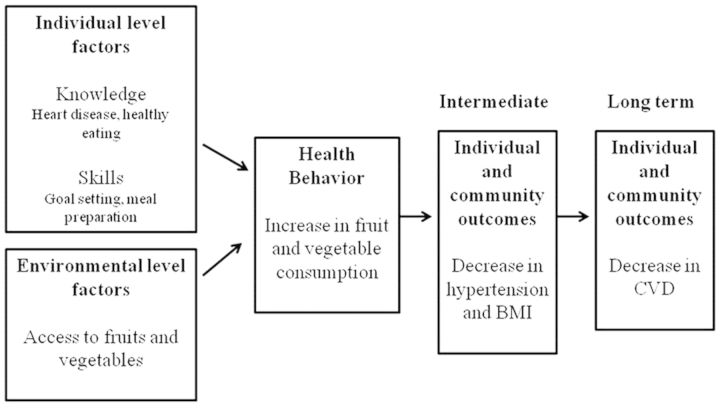
The MOTMGC evaluation was designed as a quasi-experimental study with a comparison group. Cross-sectional surveys of African Americans in both counties measured the effect of MOTMGC on blood pressure, self-reported BMI, perceived fruit and vegetable consumption, and exposure to the individual-level and environmental-level components of the intervention (Fig. 1). Cross-sectional survey data were collected in the Fall of 2008 (baseline) and the Fall of 2010 (mid-intervention). Based on input from community partners including key leaders (e.g. pastors), study participants were recruited from places frequented by African American adults in Pemiscot and Dunklin counties (e.g. community organizations, places of worship). Fliers were posted at survey sites indicating the nature of the study and when surveys were being conducted. Participants were also recruited to participate in the survey at community events (e.g. fall festival). To be eligible to take the survey, a participant had to be an African American adult aged 18 or older residing in Pemiscot County or Dunklin County.
Fig. 1.
MOTMGC logic model.
Measures
Eligible study participants provided informed consent, completed a self-administered survey in a group setting (e.g. church), had their blood pressure measured and were provided a $15 incentive. The measures included in the survey included sociodemographics [47], perceived fruit and vegetable consumption [48], self-reported blood pressure [47], blood pressure measurement [49, 50], individual level intervention exposure, environmental level intervention exposure and behavioral outcomes associated with community garden exposure [51, 52]. Perceived fruit and vegetable consumption measures were based on stages of change. This is considered a valid measure of readiness to change behavior, and appropriate for assessing complex behaviors such as eating [53, 54]. Table I provides more detail about the measures included.
Table I.
Measurement questions for the effect of nutrition education plus fruit and vegetable access on perceived fruit and vegetable consumption in a community-based nutrition intervention in a rural African American community
| Category | Measure | Response | Source | Notes |
|---|---|---|---|---|
| Self-Reported Sociodemographic Data | Age, gender, race, height, weight, education status, current employment status | Varies by measure |
|
|
| Perceived Fruit and Vegetable Consumption |
|
Five response options measuring intent were provided from ‘Yes and I have done this for more than 6 months’ to ‘No and I don’t intend to change this within the next 6 months’ | Trans-Theoretical Model | Examples of serving sizes provided to each participant |
| Self-Reported Blood Pressure | Has participant ever been told by physician that s/he has high blood pressure or heart disease? | Yes/No/Don’t Know | BRFSS | |
| Blood Pressure | Four survey administrators collect blood pressure by sphygmomanometers | Participants were coded as hypertensive if the average of two systolic blood pressure readings was 140 or higher or the average diastolic blood pressure was 90 or higher. | Administrators trained by the local health department | |
| Individual Level Intervention Exposure | The mid-intervention survey included six ‘yes’ or ‘no’ questions about the extent of participation in nutrition education activities | Participants were classified as ‘no participation’ if none of the six activities was endorsed. Participants were classified as ‘medium participation’ if one or two activities were endorsed. Participants were classified as ‘high participation’ if at least three activities were endorsed | The survey items were developed for this project and cognitive response testing was used to develop the items. | |
| Environmental Level Intervention Exposure | ‘Did you ever get fruits and/or vegetables from one of the Men on the Move Growing Communities’ gardens or vegetable stands?’ | Yes/No | N/A | |
| Behavioral Outcomes Associate with Garden Exposure |
|
Using a 5-point Likert Scale, participants were asked how much they agree with each statement | There are no published measures for community garden outcomes that have been tested for validity and reliability; however, The measures included have been used in other community-based studies |
Statistical analysis
The analysis assessed the impact of the intervention on hypertension, BMI, and perceived fruit and vegetable consumption. Chi-square and t-tests were used to statistically test differences between baseline and mid-intervention outcomes. An interaction term in logistic regression was used to determine whether changes in prevalence of hypertension and BMI between baseline and mid-intervention differed between counties. Sociodemographic characteristics (age, education, employment and income) were included in the models to calculate adjusted changes over time between counties.
t-Tests and chi-square statistics were used to determine significant differences by level of participation in nutrition education and access to community gardens in terms of perceived fruit and vegetable consumption and behavioral outcomes (gardens), BMI and hypertension. Linear regression was used to determine significant demographic, participation, and behavior predictors (e.g. perceived fruit and vegetable consumption, behavioral outcomes associated with gardens) of BMI and hypertension. SAS Version 9.2 was used for all analyses. A P-value <0.05 was considered statistically significant.
Results
Table II shows the sociodemographic composition of survey participants in the intervention and comparison counties at baseline and mid-intervention. Annual household incomes and educational attainment were higher among survey participants in the intervention county at baseline (P < 0.01). Average age was slightly higher among survey participants in the intervention county at baseline (P < 0.01) but not mid-intervention (P = 0.06). No differences existed between both communities in gender distribution (P = 0.26) or perceived income adequacy (P = 0.11) at baseline. At mid-intervention, a higher percentage of participants in the intervention county were males compared with the comparison county (P = 0.05). No differences existed in perceived income adequacy (P = 0.72) or educational attainment (P = 0.32) between counties at mid-intervention.
Table II.
Characteristics of African American residents at baseline and mid-intervention by county
| Variable | Baseline |
Mid-intervention |
||||
|---|---|---|---|---|---|---|
| Pemiscot (intervention) | Dunklin (comparison) | P-value | Pemiscot (intervention) | Dunklin (comparison) | P-value | |
| Baseline (n = 397) % | Baseline (n = 397) % | Mid (n = 389) % | Mid (n = 303) % | |||
| Gender | ||||||
| Male | 37.3 | 34.5 | 0.26 | 36.3 | 28.7 | 0.05 |
| Female | 62.7 | 65.0 | 63.2 | 71.3 | ||
| Missing | 0.0 | 0.5 | 0.5 | 0.0 | ||
| Age: Mean (SD) | 41.7 (14.7) | 38.8 (14.6) | 0.01 | 41.1 (16.4) | 38.8 (14.8) | 0.06 |
| Annual household income ($) | ||||||
| 0–9999 | 31.0 | 35.8 | <0.01 | 30.3 | 43.6 | <0.01 |
| 10 000–14 999 | 17.4 | 16.2 | 17.5 | 15.8 | ||
| 15 000–19 999 | 10.3 | 7.7 | 9.0 | 5.9 | ||
| 20 000–24 999 | 5.3 | 3.7 | 8.5 | 2.3 | ||
| 25 000–34 999 | 6.8 | 1.9 | 4.4 | 2.6 | ||
| 35 000–49 999 | 3.8 | 1.9 | 3.9 | 1.3 | ||
| 50 000–74 999 | 2.0 | 0.3 | 1.5 | 0.0 | ||
| 75 000 or more | 2.0 | 0.0 | 0.5 | 0.7 | ||
| Missing | 21.4 | 32.6 | 24.4 | 27.8 | ||
| Perceived income adequacy | ||||||
| Comfortable | 21.4 | 19.1 | 0.11 | 22.4 | 22.8 | 0.72 |
| Have just enough | 44.6 | 47.5 | 47.3 | 43.2 | ||
| Do not have enough | 33.8 | 31.6 | 28.3 | 31.7 | ||
| Missing | 0.3 | 1.9 | 2.1 | 2.3 | ||
| Education | ||||||
| Never attended school | 1.3 | 0.8 | <0.01 | 0.8 | 1.0 | 0.32 |
| Grades 1–8 | 5.5 | 6.6 | 5.7 | 5.0 | ||
| Grades 9–11 | 24.9 | 34.0 | 24.9 | 32.7 | ||
| Grades 12 or GED | 46.6 | 46.4 | 46.3 | 44.9 | ||
| College 1–3 years | 14.6 | 10.3 | 17.5 | 12.9 | ||
| College 4 years or more | 5.8 | 1.1 | 2.8 | 1.3 | ||
| Don’t know | 1.3 | 0.8 | 2.1 | 2.3 | ||
Changes in hypertension and BMI by county from baseline to mid-intervention
Table III shows changes in hypertension and BMI from baseline to mid-intervention in both counties. In the intervention county, 61.0% of participants were hypertensive at baseline compared with 45.0% at mid-intervention (P < 0.01). In the comparison county, there was no change from baseline to mid-intervention in percentage of hypertensives (P = 0.39). The interaction between point of data collection and county (data not shown) was statistically significant (P < 0.01) in unadjusted logistic regression, suggesting that the change in hypertension over time was different between both counties. The interaction remained significant (P < 0.01) in the adjusted model. In this adjusted model, the odds of hypertension declined between baseline and mid-intervention in the intervention county (OR: 0.52; 95% CI: 0.38–0.71) but not in the control county (OR: 1.11; 95% CI: 0.81–1.54).
Table III.
Prevalence of hypertension, overweight and obesity for the intervention and comparison counties at baseline and mid-intervention
| Intervention county |
Comparison county |
|||||
|---|---|---|---|---|---|---|
| Baseline | Mid-intervention | P-value | Baseline | Mid-intervention | P-value | |
| Hypertensive (%) | 61.0 | 45.0* | <0.01 | 46.7 | 49.8 | 0.39 |
| BMI | 0.01 | 0.24 | ||||
| Overweight | 28.7 | 26.3 | 30.1 | 25.3 | ||
| Obese | 41.1 | 34.6 | 35.1 | 42.5 | ||
| Overweight and obese | 69.8 | 60.9* | 65.2 | 67.8 | ||
*P < 0.05 between communities.
The prevalence of overweight and obese survey participants declined from 69.8% to 60.9% in the intervention county (P < 0.01), whereas the prevalence remained the same in the comparison county (P = 0.24). The interaction between time of data collection and county was statistically significant (P = 0.01) in unadjusted logistic regression (data not shown), suggesting that the change in BMI over time was different between both counties. The interaction remained significant (P = 0.03) in the adjusted model. In this adjusted model, the odds of being overweight/obese declined between baseline and mid-intervention in the intervention county although the confidence interval included the value of 1 (OR: 0.73; 95% CI: 0.52–1.02). The odds of overweight/obesity did not decline between baseline and mid-intervention in the comparison county (OR: 1.30; 95% CI: 0.89–1.91).
Effect of nutrition education participation on behavior change
In the intervention county, 16.3% of survey participants participated in all six nutrition education activities, and 48.5% did not participate in any. In the comparison county, 9.1% of survey participants participated in all six activities, and 60.2% did not participate in any. In the intervention county, 47.3% of survey participants reported getting fruits and/or vegetables from the MOTMGC garden. This was 19.1% of survey participants in the comparison county. Roughly 30% of comparison county survey participants took part in at least one intervention activity (see Fig. 1). Because some survey participants in the intervention county did not participate in any nutrition education activities whereas some participants in the comparison county did, subsequent analyses examined the effect of participation in nutrition education on perceived fruit and vegetable consumption and behavioral outcomes (gardens) changes, regardless of county. Next, an examination of whether changes in behavior were enhanced by increased access to produce through the gardens, again regardless of county, was conducted.
Table IV shows the prevalence of three behaviors related to perceived fruit and vegetable consumption and the effect of participating in nutrition education. Survey participants who reported high participation had 3.06 times higher odds (95% CI: 1.90–4.95) of eating five servings of fruit and vegetables daily than those who did not participate in any educational activities. Survey participants who reported medium participation also had higher odds of eating five servings of fruit and vegetables daily than those who did not participate in any educational activities (OR = 1.98; 95% CI: 1.42–2.76). Participation was not associated with the other two perceived consumption behaviors (portion and variety).
Table IV.
Prevalence of three behaviors and the effect of participating in nutritional education
| Unadjusted (OR, 95% CI) |
Adjusted for sociodemographics (OR, 95% CI) |
||||
|---|---|---|---|---|---|
| Behaviora | Prevalence (%) | High participation | Medium participation | High participation | Medium participation |
| Currently eat five or more servings of fruits and vegetables daily | 48.3 | 3.06 (1.90–4.95) | 1.98 (1.42–2.76) | 2.67 (1.63–4.40) | 1.88 (1.33–2.65) |
| Currently eat larger portions of vegetables | 63.9 | 1.29 (0.79–2.09) | 1.32 (0.93–1.86) | 1.28 (0.77–2.14) | 1.43 (0.99–2.06) |
| Currently eat greater variety of fruits/vegetables | 65.9 | 1.22 (0.74–2.00) | 0.91 (0.65–1.28) | 1.12 (0.67–1.89) | 0.89 (0.62–1.27) |
Sociodemographics include age, education, employment and income.
aComparing ‘Yes and I have done this for more than 6 months’ and ‘Yes and I started doing this during the last 6 months’ with ‘No but I intend to change this within the next month’, ‘No but I intend to change within the next 6 months’ and ‘No and I don’t intend to change this within the next 6 months’.
Effect of access to community garden on perceived behavioral outcomes
Survey participants getting produce from MOTMGC were more likely to report an increase in several food-related behavior outcomes as a result of the community gardens in unadjusted and adjusted analysis (Table V). Specifically, those that received fruits and vegetables from the MOTMGC gardens were more likely to report that they ate more fruits and vegetables, okra, and peas in adjusted analysis.
Table V.
Association between nutritional behavior and having received fruits and/or vegetables from the MOTMGC
| Behaviora | Prevalence (%) | Unadjusted (OR, 95% CI) | Adjusted (OR, 95% CI) |
|---|---|---|---|
| Eat more fruits and vegetables | 15.2 | 1.79 (1.14–2.83) | 1.95 (1.20–3.15) |
| Eat more greens | 20.0 | 1.50 (1.00–2.24) | 1.30 (0.85–1.99) |
| Eat more tomatoes | 28.0 | 1.65 (1.15–2.38) | 1.40 (0.96–2.06) |
| Eat more apples | 22.1 | 0.95 (0.65–1.38) | 1.03 (0.69–1.53) |
| Eat more watermelon | 27.1 | 1.27 (0.88–1.83) | 1.23 (0.84–1.80) |
| Eat more okra | 32.7 | 2.10 (1.46–3.02) | 1.90 (1.30–2.79) |
| Eat more peas | 33.0 | 2.28 (1.59–3.27) | 2.08 (1.41–3.07) |
| Eat more locally grown food | 29.4 | 2.55 (1.75–3.71) | 2.27 (1.53–3.35) |
| Eat less processed food | 29.5 | 1.72 (1.20–2.47) | 1.70 (1.14–2.44) |
| Eat less fast food | 28.0 | 2.15 (1.48–3.14) | 2.17 (1.46–3.23) |
| Eat more foods that are traditional to my culture | 24.2 | 1.76 (1.20–2.58) | 1.82 (1.21–2.72) |
| Eat new kinds of food | 26.8 | 1.12 (0.78–1.61) | 1.21 (0.83–1.78) |
| Spend less money on food | 35.2 | 1.58 (1.11–2.23) | 1.56 (1.08–2.25) |
| Am better able to provide food for my family and myself | 24.5 | 1.42 (0.97–2.06) | 1.47 (0.99–2.19) |
| Feel better about where my food comes from | 18.4 | 1.55 (1.02–2.35) | 1.54 (0.99–2.39) |
Sociodemographics include age, education, employment and income.
aStem read ‘Because of MOTMGC, I…’ Comparing (strongly) agree with (strongly) disagree.
Effect of participation in nutrition education activities and access to community gardens
After controlling for age, education, employment status and income, those who participated in 3–6 MOTMGC educational activities and received fruits and vegetables from the MOTMGC garden were more likely to perceive that they had started or eaten five or more fruits and vegetables in the past 6 months compared with those who did not participate and did not get fruits and vegetables from the MOTMGC garden (OR = 2.18, 95% CI: 1.24–3.81). Those who participated in 1–2 MOTMGC educational activities and received fruits and vegetables from the MOTMGC garden were also more likely to perceive that they had started or eaten five or more fruits or vegetables in the past 6 months (OR = 1.60, 95% CI: 1.00–2.57). However, those who did not participate in any MOTMGC educational activities but received fruits and vegetables from the MOTMGC garden were less likely to perceive that they had started or eaten five or more fruits and vegetables in the past 6 months than those who did not participate in nutrition education or get fruits and vegetables from the MOTMGC garden (OR = 0.57, 95% CI: 0.34–0.95).
Discussion
This article reports mid-intervention results of a nutrition education plus food access intervention to address dietary risk factors associated with CVD. Participation in nutrition education activities and access to fruits and vegetables through community and production gardens was independently associated with perceived consumption of five or more servings of fruits and vegetables a day.
At the individual level, MOTMGC used SCT to tailor nutrition education information and activities to the cultural experience of the participants and worked with participants to set and monitor small achievable dietary goals. This study shows that dietary interventions are effective when individual behavior change strategies include SCT constructs such as goal setting and identification of barriers [26, 27] and are culturally tailored [20]. However, it should be examined whether behavior change is maintained over time. Although few studies report long-term behavior change outcomes, one multi-behavior study found the greatest increase in diet-related behavior change during the first 6 months of the intervention followed by a slight decline in behavior change over time [55]. The mid-intervention findings were reported for several reasons. First, these findings begin to build the evidence about the effectiveness of nutrition education plus food access interventions to promote fruit and vegetable consumption in rural African American communities. Second, assessment at this stage is important because it determines whether the intervention is proceeding as planned and allows for potential corrections [56]. Third, reporting mid-intervention results provides insight into the time it takes for interventions to have an impact.
At the environmental level, getting fruits and vegetables from a MOTMGC garden was associated with perceived consumption of fruits and vegetables. Our findings add to research that has shown that community gardens are an effective environmental strategy to increase fruit and vegetable consumption in urban settings [30]. Our study also found an association with perceived consumption of specific items grown in the MOTMCG gardens, such as okra and peas, whereas there was no association with items (e.g. apples) not grown in the MOTMGC gardens. This finding suggests that increased consumption may be limited to items grown in gardens. Limited access, poor quality and/or the cost of available produce may limit overall consumption.
The strongest association was found with the highest participation in nutrition education activities and access to fruits and vegetables. However, when an individual did not participate in nutrition education but received fruits and vegetables from a garden they were less likely to perceive that they consumed the recommended servings of fruits and vegetables than those who do not receive nutrition education or produce from the gardens. There could be several explanations for this. First, the cost of fruits and vegetables is a barrier to eating a healthy diet among African Americans [57–59]. The research team compared the price of MOTMGC produce with the price at local stores, MOTMGC produce was less expensive than those sold locally. Perhaps, some participants bought MOTMGC produce as a low-cost way to supplement their food intake but were not able to afford to do so in a way that meets consumption recommendations. Second, knowledge of fruit and vegetable recommendations also was associated with a perceived increase in fruit and vegetable consumption [60]. As participants who did not attend nutrition education sessions did not receive the information delivered, some may not know what the recommendations for consumption are. Third, those who did not receive produce or nutrition education may have access to produce through other food outlets and/or may already have nutrition knowledge. Prior to the start of the intervention, the research team conducted an audit of community gardens in the area. In Pemiscot County, there was only one existing community garden which was included as the community garden in this project. However, the research team did not survey participants to determine whether they had personal gardens which may have affected consumption. Although the Institute of Medicine and others recommend environment and policy change to support the consumption of fruits and vegetables [20, 34], our findings suggest that environmental changes may not have the anticipated effect unless individuals also have the financial resources, knowledge and skills to make use of those changes. The trend toward environmental and policy change to transform the food environment has exploded in the last decade. Systematic reviews indicate that more evaluation of interventions to increase access to healthy food options is needed; however, community gardens have been identified as a promising strategy [61, 62]. Our study adds to what is known by considering nutrition education plus increased access through community gardens.
Although our primary focus was the intermediate outcome of perceived fruit and vegetable consumption, hypertension and BMI were significantly lower in our intervention county compared with the comparison county. These differences were not accounted for by demographic characteristics. Although nutrition education plus food access interventions to address CVD are scarce, other community-based interventions addressing individual level risk factors for CVD among an African American population have also found significant pre–post intervention reductions in blood pressure [63, 64] and BMI [65].
As a result of mid-intervention findings several changes were made to the intervention. First, the research team focused on name recognition through branding. For example, adhesive labels with the MOTMGC logo were developed and all production garden produce sold was labeled. Second, the environmental component of our intervention was enhanced by partnering with two local grocery stores to place ‘shelf talkers’ in front of heart healthy items endorsed by MOTMGC.
Limitations
A main limitation is the contamination of the comparison county. The town centers of the intervention and comparison communities are only 22 miles apart. The research team anticipated potential contamination through mass media outlets that serve both counties and therefore used other methods for publicizing activities. Participation by comparison county residents in intervention activities may have occurred because rural Missouri residents often travel farther for fresh produce and family relationships extend beyond county borders. Because this likely resulted in bias toward the null or no difference between counties, the actual difference between both counties is expected to be larger than was observed. Due to this contamination, the research team analyzed those exposed to the intervention regardless of county in the analysis of fruit and vegetable consumption.
Although our cross-sectional survey design cannot establish causality, our results are promising nevertheless. Members of the research team were present on several community boards to stay abreast of environmental or policy-related initiatives during the study period that could affect our findings. Because no such initiatives were developed or implemented during the study period, the research team feels confident that this cannot explain our findings. A randomized cluster design, where survey participants are tracked over time, would make a stronger case for causality. However, such study designs are typically difficult to implement in community-based work such as ours.
Additional limitations include potential for measurement bias and bias toward socially active and mobile residents. Perceived fruit and vegetable consumption, height and weight are self-reported measures and have the potential of bias [66]. Measurement of actual fruit and vegetable consumption can be costly and difficult to attain in a community sample. The measures of outcomes associated with community garden exposure have been used in other work [51, 52], but have not been tested for reliability and validity. Currently, there are no documented reliable and valid measures to assess outcomes associated with community garden exposure. Survey participants were recruited in public venues; therefore, data were only captured from socially active residents. Our sample does not represent less active members of the population. This unlikely affected our findings because participant recruitment was conducted the same way in both counties.
Conclusion
In conclusion, our findings suggest that an intervention incorporating nutrition education plus food access to promote fruit and vegetable consumption can contribute to behavior change in a rural African American population.
Funding
Men on the Move: Growing Communities, R24 MD00 1590-01, National Institute on Minority Health and Health Disparities (NIH).
Conflict of interest statement
None declared.
References
- 1.National Heart, Lung, and Blood Institute. Morbidity and Mortality: 2012 Chart Book on Cardiovascular, Lung, and Blood Disease. National Institutes of Health; Available at: http://www.nhlbi.nih.gov/research/reports/2012-mortality-chart-book. Accessed: 2 March 2015. [Google Scholar]
- 2.Gillum R, Mehari A, Curry B, et al. Racial and geographic variation in coronary heart disease mortality trends. BMC Public Health 2012; 12: 410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Vital signs: avoidable deaths from heart disease, stroke, and hypertensive disease—United States, 2001–2010. MMWR Morb Mortal Wkly Rep 2013; 62: 721–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis 2007; 17: 143–52. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Trends in ischemic heart disease death rates for Blacks and Whites–United States, 1981-1995. MMWR Morb Mortal Wkly Rep 1998; 47: 945–9. [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Available at: http://www.cdc.gov/nchs/data/hus/hus11.pdf. Accessed: 1 March 2015. [Google Scholar]
- 7.Frieden TR. Forward: CDC health disparities and inequalities report - United States, 2011. MMWR Surveill Summ 2011; 60(Suppl.): 1–2. [PubMed] [Google Scholar]
- 8.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Health Stat 2012; 10(252). [PubMed] [Google Scholar]
- 9.O’Connor A, Wellenius G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public Health 2012; 126: 813–20. [DOI] [PubMed] [Google Scholar]
- 10.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005-2008). J Rural Health 2012; 28: 392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Touhill BC, Seymour J, Serdula MK, et al. What epidemiologic studies tell us about the relationship between fruit and vegetable consumption and body weight. Nutr Rev 2004; 62: 365–74. [DOI] [PubMed] [Google Scholar]
- 12.Goss J, Grubbs L. Comparative analysis of body mass index, consumption of fruits and vegetables, smoking, and physical activity among Florida residents. J Community Health Nurs 2005; 22: 37–46. [DOI] [PubMed] [Google Scholar]
- 13.Miura K, Greenland P, Stamler J, et al. Relation of vegetable, fruit, and meat intake to a 7-year blood pressure change in middle-aged men: the Chicago Western Electric study. Am J Epidemiol 2004; 159: 572–80. [DOI] [PubMed] [Google Scholar]
- 14.Reddy KS, Katan MB. Diet, nutrition, and the prevention of hypertension and cardiovascular diseases. Public Health Nutr 2004; 7: 167–86. [DOI] [PubMed] [Google Scholar]
- 15.He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: meta analysis of cohort studies. Lancet 2006; 367: 320–6. [DOI] [PubMed] [Google Scholar]
- 16.Dauchet L, Amouyel P, Hercber S, et al. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr 2006; 136: 2588–93. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. State-Specific Trends in Fruit and Vegetable Consumption among Adults - United States, 2000-2009. MMWR Morb Mortal Wkly Rep 2010; 59: 1125–9. [PubMed] [Google Scholar]
- 18.Seymour JD, Yaroch AL, Serdula M, et al. Impact of nutrition environmental interventions on point-of-purchase behavior in adults: a review. Am J Prev Med 2004; 39(Suppl. 2): S108–36. [DOI] [PubMed] [Google Scholar]
- 19.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 2010; 122: 406–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stuart Shor EM, Berra KA, Kamau MW, et al. Behavioral strategies for cardiovascular risk reduction in diverse and underserved racial/ethnic groups. Circulation 2012; 125: 171–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Walton-Moss B, Samuel L, Nyugen T et al. Community-based cardiovascular health interventions in vulnerable populations: a systematic review. J Cardiovasc Nurs 2014; 29: 293–307. [DOI] [PMC free article] [PubMed]
- 22.Leeman J, Sommers J, Vu M, et al. An evaluation framework for obesity prevention policy interventions. Prev Chronic Dis 2012; 9: 110322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health 2001; 22; 309–35. [DOI] [PubMed] [Google Scholar]
- 24.Glanz K, Lankenau B, Foerster S, et al. Environmental and policy approaches to cardiovascular disease prevention through nutrition: opportunities for state and local action. Health Educ Q 1995; 22: 512–27. [DOI] [PubMed] [Google Scholar]
- 25.Jeffery RW, French SA. Epidemic obesity in the United States: are fast foods and television viewing contributing? Am J Public Health 1998; 88: 277–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamphuis CB, Giskes K, De bruijn GJ, et al. Environmental determinants of fruit and vegetable consumption among adults: a systematic review. Br J Nutr 2006; 96: 620–35. [PubMed] [Google Scholar]
- 27.Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study . Am J Public Health 2002; 92: 1761–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raine K. Determinates of healthy eating in Canada: an overview and synthesis. Can J Public Health 2005; 96(Suppl. 3): S8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morland K, Wing S, Diez Roux A, et al. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med 2002; 22: 23–9. [DOI] [PubMed] [Google Scholar]
- 30.Litt JS, Soobader MJ, Turbin MS, et al. The influence of social involvement, neighborhood aesthetics, and community garden participation on fruit and vegetable consumption. Am J Public Health 2011; 101: 1466–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCormack LA, Laska MN, Larson NI, et al. Review of the nutritional implications of farmers’ markets and community gardens: a call for evaluation and research efforts. J Am Diet Assoc 2010; 110: 399–408. [DOI] [PubMed] [Google Scholar]
- 32.Barnidge E, Hipp PR, Estlund E, et al. Association between community garden participation and fruit and vegetable consumption in rural Missouri. Int J Behav Nutr Phys Act 2013; 10: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freedman DA, Choi SK, Hurley T, et al. A farmers’ market at a federally qualified health center improves fruit and vegetable intake among low-income diabetics. Am J Prev Med 2013; 56: 288–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Institute of Medicine. Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making . Washington, DC: The National Academies Press, 2010. [PubMed] [Google Scholar]
- 35.National Heart, Lung, and Blood Institute (NHLBI). Working Group Report on Future Research Directions in Childhood Obesity Prevention and Treatment. Available at: http://www.nhlbi.nih.gov/research/reports/2007-child-obesity. Accessed: 2 March 2015. [Google Scholar]
- 36.Golley RK, Hendrie GA, Slater A, et al. Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns—what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obes Rev 2011; 12: 114–30. [DOI] [PubMed] [Google Scholar]
- 37.Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009; 28: 690–701. [DOI] [PubMed] [Google Scholar]
- 38.Story M, Kaphingst K, Robinson-O’Brien R, et al. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health 2008; 29: 253–72. [DOI] [PubMed] [Google Scholar]
- 39.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004; 79: 6–16. [DOI] [PubMed] [Google Scholar]
- 40.Auslander WF, Haire-joshu D, Houston CA, et al. Community organization to reduce the risk of non-insulin-dependent diabetes among low-income African-American women. Ethn Dis 1992; 2: 176–84. [PubMed] [Google Scholar]
- 41.U. S. Census Bureau. American FactFinder. U.S. Census Bureau. Available at: http://factfinder2.census.gov. Accessed: 15 July 2013. [Google Scholar]
- 42.Missouri Department of Health and Senior Services. Chronic Disease Data Queries. Missouri Department of Health and Senior Services; Available at: http://health.mo.gov/data/mica/ChronicDiseaseMICAs/. Accessed: 2 March 2015. [Google Scholar]
- 43.Economic Research Service (ERS), U.S. Department of Agriculture (USDA). Food Environment Atlas. U.S. Department Agriculture; Available at: http://www.ers.usda.gov/data-products/food-environment-atlas/go-to-the-atlas.aspx. Accessed: 28 April 2015. [Google Scholar]
- 44.Baranowski T, Perry C, Parcel GS. How individuals, environments, and health behavior interact: social cognitive theory. In: Glanz K, Rimer B, Lewis F. (eds). Health Behavior and Health Education, 3rd edn. San Francisco, CA: Jossey Bass, 2002. [Google Scholar]
- 45.National Heart, Lung, and Blood Institute. Guide to lowering blood pressure. NIH Publication No. 06-4082. National Institutes of Health. Available at: http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf. Accessed: 2 March 2015. [Google Scholar]
- 46.Krauss RM, Eckel RH, Howard B, et al. AHA Dietary Guidelines Revision 2000: A statement for health care professionals from the nutrition committee of the American Heart Association Circulation 2000; 102: 2284–99. [DOI] [PubMed] [Google Scholar]
- 47.American Heart Association Nutrition Committee, Lichtenstein AH, Appel LJ, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006; 114: 82–96. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Questionnaire. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/brfss/questionnaires.htm. Accessed: 2 March 2015. [Google Scholar]
- 49.Prochaska JO, Redding CA, Viswanath K. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Lewis FM. (eds). Health Behavior and Health Education, Theory, Research, and Practice, 4th edn. San Francisco, CA: Jossey-Bass, 2009. [Google Scholar]
- 50.White WB, Berson AS, Robbins C, et al. National standard for blood pressures with automated sphygmomanometers. Hypertension 1993; 21: 504–9. [DOI] [PubMed] [Google Scholar]
- 51.Anwar YA, Giacco S, McCabe EJ, et al. Evaluation of the efficacy of the Omron HEM-737 IntelliSense Device for use on adults according to recommendations of the Association for the Advancement of Medical Instrumentation. Blood Press Monit 1998; 3: 261–5. [PubMed] [Google Scholar]
- 52.Baker EA, Motton F, Seiler R, Duggan K, Brownson R. Creating community gardens to improve access among African Americans: a partnership approach. J Hunger Environ Nutr 2013; 8: 1–17.23935771 [Google Scholar]
- 53.National Research Center, Community Food Security Coalition. Community Food Project Evaluation Handbook and Toolkit, 3rd edn. Boulder, CO: National Research Center, 2006. [Google Scholar]
- 54.Kristal AR, Glanz K, Curry S, et al. How can stages of change be best used in dietary interventions? J Am Diet Assoc. 1999; 99: 679–84. [DOI] [PubMed] [Google Scholar]
- 55.Robinson AH, Norman GJ, Sallis JF, et al. Validating stage of change measures for physical activity and dietary behaviors for overweight women. Int J Obes 2008; 32: 1137–44. [DOI] [PubMed] [Google Scholar]
- 56.Toobert DJ, Strycker LA, Barrera M, et al. Seven-year follow-up of a multiple-health-behavior diabetes intervention. Am J Health Behav 2010; 34: 680–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rossi P, Lipsley M, Freeman H. Evaluation: A Systematic Approach. Thousand Oaks, CA: Sage Publications, 2004. [Google Scholar]
- 58.Hargreaves M, Schlundt D, Buchowski M. Contextual factors influencing the eating behaviors of African American women: a focus group investigation. Ethn Health 2002; 7: 133–47. [DOI] [PubMed] [Google Scholar]
- 59.James D. Factors influencing food choices, dietary intake, and nutrition-related attitudes among African Americans: application of a culturally sensitive model. Ethn Health 2004; 9: 349–67. [DOI] [PubMed] [Google Scholar]
- 60.Mushi-Brunt C, Haire-Joshu D, Elliot M. Food spending behaviors and perceptions are associated with fruit and vegetable intake among parents and their preadolescent children. J Nutr Educ Behav 2007; 39: 26–30. [DOI] [PubMed] [Google Scholar]
- 61.Watters J, Satia J, Galanko J. Associations of psychosocial factors with fruit and vegetable intake among African Americans. Public Health Nutr 2007; 10: 701–11. [DOI] [PubMed] [Google Scholar]
- 62.Brennan LK, Brownson R, Orleans T. Childhood obesity policy research and practice evidence for policy and environmental strategies. Am J Prev Med 2014; 46: e1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kumanyaki SK, Swank M, Stachecki MC, et al. Examining the evidence for policy and environmental strategies to prevent childhood obesity in black communities: new directions and next steps. Obes Rev 2014; S4: 177–203. [DOI] [PubMed] [Google Scholar]
- 64.Paschal AM, Lewis RK, Martin A, et al. Evaluating the impact of a hypertension program for African Americans. J Natl Med Assoc 2006; 98: 607–15. [PMC free article] [PubMed] [Google Scholar]
- 65.Resnick B, Shaughnessy M, Galik E, et al. Pilot testing of the PRAISEDD intervention among African American and low income older adults. J Cardiovasc Nurs 2009; 24: 352–61. [DOI] [PubMed] [Google Scholar]
- 66.Steinhardt MA, Mamerow MM, Brown SA, et al. A resilience intervention in African American adults with type 2 diabetes: a pilot study of efficacy. Diabetes Educ 2009; 35: 274–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gorber CS, Tremblay M, Moher D, et al. A comparison of direct vs. self-report measure for assessing height, weight and body mass index: a systematic review. Obes Rev 2007; 8: 307–26. [DOI] [PubMed] [Google Scholar]