Abstract
Purpose of the Study:
To examine whether compassionate love in both individuals with Alzheimer’s disease (AD) and their spousal caregivers related to less caregiving burden, more positive caregiving appraisals, and less depressive symptoms for caregivers.
Design and Methods:
Fifty-eight individuals with AD and their spousal caregivers participated in interviews in which both partners reported their compassionate love for their partner, and caregivers self-reported burden, positive appraisals of caregiving, and depressive symptoms.
Results:
As hypothesized, both AD individuals’ and caregivers’ compassionate love were associated with less burden and more positive appraisals of caregiving. Also, care givers’ compassionate love mediated the association between AD individuals’ compassionate love and caregivers’ burden as well as the association between AD individuals’ compassionate love and caregivers’ positive appraisals of caregiving. Finally, there was a marginally significant association between caregivers’ compassionate love and less caregiver depressive symptoms.
Implications:
Results suggest that AD individuals’ compassionate love is related to compassionate love in caregivers, which in turn relates to reduced burden but not significantly less depressive symptoms for caregivers. Assessing caregivers’ and AD individuals’ feelings of compassionate love may be useful in identifying caregivers who are resilient and those who are at a heightened risk for caregiving burden. Also, interventions that enhance both partners’ compassionate love may benefit caregivers.
Key words: Compassion, Caregiving, Alzheimer’s disease
It is estimated that there are 5.2 million individuals with Alzheimer’s disease (AD) in the United States with the majority of individuals receiving care from family and friends (Alzheimer’s Association, 2013). A vast literature shows that the stress and burden of providing care to a loved one suffering from dementia can have negative physical and mental health effects on family members, especially spouses (Pinquart & Sörensen, 2003). At the same time, there is a small body of research emphasizing positive aspects of caregiving that may be protective for caregivers’ health, such as self-efficacy, relationship quality, feelings of accomplishment, enriching events in daily life, and a sense of purpose or meaning (Carbonneau, Caron, & Desrosiers, 2010). One positive factor that is receiving increased attention in the close relationships literature but has yet to be considered in the informal caregiving literature is compassionate love. We propose that compassionate love has important implications for the spousal caregivers of individuals with AD in terms of how they view their caregiving role, their feelings of burden, and their depressive symptoms.
What is Compassionate Love?
Compassionate love is “an attitude toward other(s), either close others or strangers or all of humanity; containing feelings, cognitions, and behaviors that are focused on caring concern, tenderness, and an orientation toward supporting, helping, and understanding the other(s), particularly when the other(s) is (are) perceived to be suffering or in need” (Sprecher & Fehr, 2005, p. 630). Although this concept has been applied to a variety of social contexts (Fehr, Sprecher, & Underwood, 2009), little is known about how compassionate love relates to informal caregivers’ psychological health. One exception is a qualitative study of end-of-life patients and their caregivers that highlighted the importance of compassionate love or “compassionate caregiving” during the dying process (Roberts, Wise, & DuBenske, 2009). Roberts and colleagues suggested that compassionate love is manifested in the end-of-life context as care that is other oriented, shows appreciation of the real needs of the patient, and has a warm emotional quality. This is in contrast to care that is self-oriented and stems from obligation, pressure from others, or a desire to get something in return.
Caregiver Compassionate Love and Their Own Psychological Health
No research has examined the association between compassionate love and psychological health in the context of caring for a spouse with dementia. However, research with healthy, young adults shows that compassionate goals and feeling compassionate love in relationships enhances positive emotions (e.g., Canevello & Crocker, 2010; Crocker & Canevello, 2008; Sprecher & Fehr, 2006). For example, young adult roommates who have compassionate goals report feeling peaceful and loving in everyday life (Crocker & Canevello, 2008), and young adults who are high in trait compassionate love expect to feel positive emotions when they help others (Sprecher, Fehr, & Zimmerman, 2007). It has been suggested that this is because people who have compassionate, other-focused goals feel more supported by others than people with more self-focused goals (Crocker & Canevello, 2008). People with compassionate goals see themselves as part of a larger system of individuals whose actions affect the well-being of all. They believe that taking care of others is not inherently costly to the self and that if they take into account the needs of others, they will be able to meet their own needs in a way that is sustainable for the self and others (Crocker & Canevello, 2012). Although the relationships between caregivers and care recipients with dementia are likely to be very different from relationships between young adult college roommates and younger adults in general, we believe these ideas apply to humans in a variety of contexts.
Does Compassionate Love From the Spouse With AD Also Contribute to the Caregiver’s Psychological Health?
Although existing research with young adults shows that feeling compassionate love for others seems to have more benefits for the self than receiving compassionate love from others (Sprecher & Fehr, 2006), care recipients’ compassionate love toward the caregiver may also benefit caregivers’ psychological health. In the end-of-life caregiving context, Roberts and colleagues (2009) describe care recipients’ compassionate care for their caregivers as deep recognition of and appreciation for the caregiver, as well as expressions that are genuinely responsive to the caregiver’s emotional needs. They suggest that caregivers who have compassionate spouses are likely to feel more supported than caregivers with spouses who are less compassionate. We suggest that caregivers may also be more likely to feel compassionate love for care recipients when care recipients also feel compassionate love for them. This may be in part because close relationship partners tend to be similar to one another (e.g., Berscheid, Dion, Walster, & Walster, 1971; Sprecher & Duck, 1994) and because responsiveness within close, communal relationships can be mutually reinforcing (Canevello & Crocker, 2010; Clark & Monin, 2006).
Hypotheses
First, we hypothesized that caregivers’ compassionate love would be related to lower caregiving burden (Hypothesis 1a), more positive appraisals of caregiving (Hypothesis 1b), and less depressive symptoms. Second, we hypothesized that compassionate love of individuals with AD and their caregivers would be associated. In other words, when one partner feels compassionate love, the other partner also is likely to feel compassionate love (Hypothesis 2a). Next, we examined whether compassionate love in the individual with AD was also associated with caregivers’ burden, positive appraisals, and depressive symptoms. Based on Roberts and colleagues’ research, we hypothesized that greater compassionate love in the individual with AD would be associated with less caregiver burden (Hypothesis 2b), more positive appraisals of caregiving (Hypothesis 2c), and less depressive symptoms (Hypothesis 2d). We then examined whether caregiver compassionate love or AD individuals compassionate love was more closely related to caregivers’ psychological health. Drawing from Sprecher and Fehr’s (2006) work, we predicted that caregivers’ compassionate love for their partner would be more closely related to caregivers’ own psychological health. In other words, we predicted that caregivers’ compassionate love would mediate potential associations between AD individuals’ compassionate love and caregiver’s burden (Hypothesis 3a), AD individuals’ compassionate love and caregiver’s positive appraisals (Hypothesis 3b), and AD individuals’ compassionate love and caregiver’s depressive symptoms (Hypothesis 3c).
Methods
Participants
Data from 58 individuals with AD and their caregiving spouses were examined. As described in Monin and coworkers (2013), this sample was taken from a parent study of individuals with AD (N = 105) and their family caregivers who were recruited from the Alzheimer’s Disease Research Center at the University of Pittsburgh and the local chapter of the Alzheimer’s Disease Association (Schulz et al., 2010). AD individuals had to (a) be 50 years old or older, (b) have consensus-based diagnosis of probably or possible AD or related dementia, and (c) reside in the community with the primary caregiver. Caregivers had to (a) be a family member/partner (e.g., spouse, child, or fictive kin), (b) be 21 years of age or older, (c) provide a minimum of 3 months of in-home care prior to recruitment, (d) speak English, and (e) self-define as primary caregiver of the AD individual.
Only married couples were selected for the present study so that the nature of the relationship (i.e., similarity of ages of the partners, potential romance in relationship history) was consistent across the sample and because it would be difficult to make comparisons with other relationship types due to low frequencies of other relationship types. We also limited to couples in which the individual with AD had a score of 16 or higher on the Mini-Mental State Examination (Folstein, Folstein, & McHugh, 1975) to ensure more reliable reporting. Reliable reporting was also based on trained interviewers’ ratings of the ability of respondents to answer questions throughout the survey. All participants completed a baseline interview and a 1-year follow-up interview. Because compassionate love was only assessed at the follow-up interview, we used only follow-up variables in our analyses. The final sample size with these selection criteria was 58 couples.
In the present study, the average age was 73.95 (SD = 8.10) for individuals with AD and 71.10 (SD = 7.8) for caregiving spouses at baseline. Eleven (19%) of the individuals with AD were women, and 47 (81%) were men. Fifty-five (94.8%) individuals with AD were white, two were black (3.4%), and one (1.7%) was Asian. This was the same for caregiving spouses. Thirty-eight individuals with AD (66%) and 41 spouses (71%) completed at least some college education.
Measures
Caregiver and AD Individual Characteristics
Standard demographic information was assessed including gender, age, income, education, race/ethnicity, and relationship to the individual with AD.
Compassionate Love
The “close other” version of the compassionate love scale was used to assess caregivers’ and AD individuals’ attitude toward the partner that contained feelings, cognitions, and behaviors focused on caring, concern, tenderness, and an orientation toward supporting, helping, and understanding others, particularly when the other is perceived to be suffering (Sprecher & Fehr, 2005). The scale includes 21 items, such as “When I see my partner feeling sad, I feel a need to reach out to him/her,” “If my partner needs help, I would do almost anything I could do to help him/her,” and “I often have tender feelings toward my partner when he or she seems to be in need.” Participants were asked to rate the extent to which each item was true from 1 (not at all true of me) to 7 (very true of me; α = .96). Mean scores were used.
Caregiver Perceived Burden
A 12-item version of the Zarit Burden Interview assessed caregivers’ burden (Bédard et al., 2001). Caregivers were asked how frequently on a scale from 0 (never) to 4 (nearly always) “that because of the time [they] spend with [the individual with AD] that [they] don’t have enough time for [themselves]?”, “that [their] health has suffered because of [their] involvement with [the individual with AD],” etc. (α = .86). Sum scores were used.
Positive Appraisals of Caregiving
Positive appraisals of caregiving were assessed with 11 items, phrased as statements about the caregiver’s mental-affective state in relation to the caregiving experience (Boerner, Schulz, & Horowitz, 2004). Each item began with the stem “Providing help to (individual with AD) has …,” followed with specific items such as “made me feel useful” and “enabled me to appreciate life more.” Each item was rated on a 5-point Likert scale ranging from 1 (disagree a lot) to 5 (agree a lot; α = .90). Items were based on an earlier measure administered to caregivers of persons with a diagnosis of either physical or cognitive impairment as part of the Caregiver Health Effects Study (Beach, Schulz, Yee, & Jackson, 2000). Higher scores indicated greater caregiving benefit.
Caregiver Depressive Symptoms
The 10-item version of the Center for Epidemiological Studies-Depression scale (Irwin, Artin, & Oxman, 1999) was used to assess the depressive symptoms of the caregiver over the past 7 days. Sum scores were used.
AD Individuals’ Activities of Daily Living and Instrumental Activities of Daily Living
These measures were included as potential covariates. Caregivers were asked about whether the individual with AD needed assistance (“yes” or “no”) with six activities of daily living (ADLs; e.g., grooming, bathing, and toileting) and eight instrumental activities of daily living (IADLs; e.g., housework, laundry, and cooking meals; Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963). Sum scores were used.
Caregiver Physical Conditions
Also used as a potential covariate, 13 items assessed physical conditions experienced by the caregiver, such as arthritis, high blood pressure, diabetes, stroke, chronic lung disease, etc. [responses were 1 (yes) or 0 (no)]. The sum scores were used (Schulz et al., 2003).
Statistical Analysis
Descriptive statistics were calculated for all variables (see Table 1). Next, correlational analyses were conducted to examine potential covariates of compassionate love and the outcome variables (burden, positive appraisals, and depressive symptoms). As shown in Table 2, there were no significant covariates with compassionate love and outcome variables. (We also ran regression models with both partner’s compassionate love predicting each psychological health measure adjusting for theoretically related covariates [caregivers’ age, gender, comorbidity, and care recipients’ ADLs and IADLs]. Including these covariates did not alter the hypothesized findings or show that covariates were significant in the model, so we report the results of the correlational analysis only). Thus, in examining associations between caregiver compassionate love and caregiver psychological health (Hypothesis 1a, 1b, and 1c), caregiver compassionate love and AD compassionate love (Hypothesis 2a), and AD compassionate love and caregiver psychological health (Hypothesis 2b, c, and d), we used correlational analyses.
Table 1.
Descriptive Statistics
| Mean | SD | Range | |
|---|---|---|---|
| CG compassionate love | 6.16 | 0.94 | 2.33–7 |
| AD compassionate love | 6.53 | 1.07 | 3.90–9 |
| AD IADLs | 6.54 | 1.49 | 2–8 |
| AD ADLs | 2.03 | 2.45 | 0–7 |
| CG physical conditions | 2.77 | 1.79 | 0–8 |
| CG burden | 15.97 | 9.33 | 0–43 |
| CG positive appraisals of caregiving | 41.69 | 9.18 | 14–55 |
| CG depressive symptoms | 15.01 | 11.16 | 0–46 |
Note: AD = individual with AD; ADLs = need for assistance with basic activities of daily living; CG = caregiver; IADLs = need for assistance with instrumental activities of daily living; n = 52 for CGs and 50 for ADs.
Table 2.
Correlation Matrix of All Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CG compassionate love | .54** | −.18 | .30* | .12 | −.24 | −.16 | −.08 | .14 | .17 | −.05 | .54** | −.47** | −.25† | |
| 2. AD compassionate love | −.17 | .42** | .24† | −.27 | −.15 | −.22 | .06 | .18 | .00 | .31* | −.39** | −.08 | ||
| 3. CG gender | −.09 | .09 | .10 | .07 | −.07 | .26† | −.04 | .02 | −.13 | .35* | .08 | |||
| 4. CG age | .84** | −.07 | −.03 | −.15 | −.04 | .16 | .15 | .23† | −.23 | −.04 | ||||
| 5. AD age | −.07 | −.04 | −.16 | .04 | .15 | .19 | .06 | .01 | .13 | |||||
| 6. CG education | .63** | .62** | .19 | .12 | −.28* | −.18 | .39** | .03 | ||||||
| 7. AD education | .52** | .23 | .12 | −.12 | −.20 | .30* | .07 | |||||||
| 8. Income | .16 | .09 | .18 | −.18 | .18 | −.05 | ||||||||
| 9. AD IADLs | .36** | .00 | .10 | .25† | .21 | |||||||||
| 10. AD ADLs | .01 | −.09 | .17 | .33* | ||||||||||
| 11. CG physical conditions | −.04 | .21 | .34* | |||||||||||
| 12. CG positive appraisals of caregiving | −.36* | −.36* | ||||||||||||
| 13. CG burden | .53** | |||||||||||||
| 14. CG depressive symptoms |
Note: AD = individual with AD; CG = caregiver; IADLs = need for assistance with instrumental activities of daily living; n = 52 for CGs and 50 for ADs.
*p < .05. **p < .01. † p < .10.
For our analyses testing the pathways that caregiver compassionate love mediates the relationship between AD compassionate love and each of the psychological health indicators (Hypothesis 3a, b, and c), we followed the current recommendations (e.g., Preacher & Hayes, 2004) and used bootstrapping. Bootstrapping evaluates the magnitude of an indirect effect by comparing it to the sampling distribution of multiple resamples of the data set. Because bootstrapping makes no assumptions about normality in the data distribution, it corrects for possible bias in the obtained confidence intervals (CIs), thereby improving the quality of inference in mediation models (MacKinnon, Lockwood, & Williams, 2004). For our bootstrapping analysis, we used separate linear regression models rather than dyadic analyses techniques (e.g., the Actor–Partner Interdependence Model; Kenny, Kashy, & Cook, 2006) because we treated the couple as the unit of analysis and examined only caregiver outcomes. Violation of the assumption of independence primarily occurs within relationship research when individuals are treated as the unit analysis and both partners’ outcomes are being predicted.
Results
Hypothesis 1a, b, and c: Was Caregiver Compassionate Love Related to Caregivers’ Burden, Positive Appraisals, and Depressive Symptoms?
As hypothesized, caregiver compassionate love was significantly associated with less burden and more positive appraisals of caregiving; however, caregiver compassionate love was marginally significantly associated with less depressive symptoms (see Table 2). Also, although not a main hypothesis, we found that greater burden was associated with more depressive symptoms.
Hypothesis 2a: Were AD Individuals’ and Caregivers’ Reports of Compassionate Love Related?
Consistent with the hypothesis, AD individuals’ and care givers’ reports of compassionate love were positively related (see Table 2).
Hypothesis 2b, c, and d: Was AD Individuals’ Compassionate Love for the Caregiver Related to Caregivers’ Burden, Positive Appraisals, and Depressive Symptoms?
As hypothesized, AD individuals’ compassionate love was significantly associated with less caregiver burden and more positive appraisals; however, AD individuals’ compassionate love was not associated with less caregiver depressive symptoms (see Table 2).
Hypothesis 3: Was Caregiver Compassionate Love a Significant Mediator of the Association Between (a) AD Individuals’ Compassionate Love and Caregiver Burden, (b) AD Individuals’ Compassionate Love and Positive Appraisals of Caregiving, and (c) AD Individuals’ Compassionate Love and Caregivers’ Depressive Symptoms?
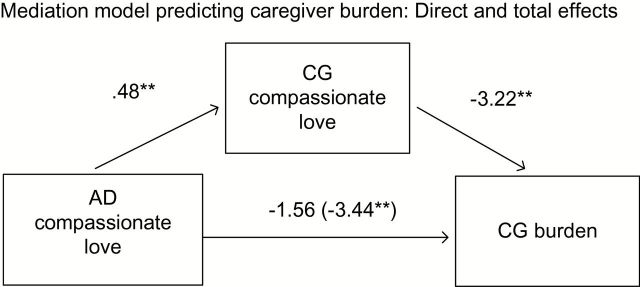
Bootstrapping was used to examine the mediating effect of caregivers’ compassionate love on the association between AD individuals’ compassionate love and caregiver burden. A total of 5,000 resamples and 95% CIs (i.e., establishing that the indirect effects were significant at two-tailed, p < .05) were used. In every case, results were also significant with Sobel tests. As shown in Figure 1, there was a strong overall effect of AD individuals’ compassionate love on burden, a strong effect of AD individuals’ compassionate love on caregiver compassionate love, a strong effect of caregiver compassionate love on burden even after controlling AD individuals’ compassionate love, and a significant reduction in the direct effect when the mediator was included (indirect effect: ab = −1.65, SE = 0.77, 95% CI: [−3.17, −0.13], p < .05; direct effect: b = −1.57, SE = 1.23, t(49) = −1.28, p = .21; We also included an interaction term between both partners’ compassionate love variables in each model predicting burden and positive appraisals. The interaction terms were not significant when included in the models with both main effects, so we examined only main effects in the final analysis according to the guidelines of Jaccard and Turrisi 2003 and Aiken and West 1991). Results of the mediation analysis showed that caregiver compassionate love significantly mediated the relationship between AD individuals’ compassionate love and caregiving burden.
Figure 1.
Mediation model predicting caregiver burden: direct and total effects. Notes: Unstandardized betas are presented. In parentheses is the beta coefficient when the mediator is not included in the model. Standardized betas are .54 for Alzheimer’s disease (AD) compassionate love → CG compassionate love, −.49 for CG compassionate love → burden, and −.39 (−.19 when mediator is included) for AD compassionate love → burden. **p < .01.
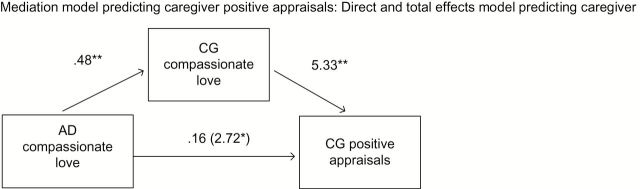
We used the same procedure to test for the mediating effect of caregiver compassionate love on the association between AD individuals’ compassionate love and positive appraisals of caregiving. As shown in Figure 2, there was a strong overall effect of AD individuals’ compassionate love on positive appraisals, a strong effect of AD individuals’ compassionate love on caregiver compassionate love, a strong effect of caregiver compassionate love on positive appraisals even after controlling AD individuals’ compassionate love, and a significant reduction in the direct effect when the mediator was included (indirect effect: ab = 2.55, SE = 0.92, 95% CI: [0.74, 4.36], p < .01; direct effect: b = 0.16, SE = 1.30, t(49) = 0.13, p = .90). Caregiver compassionate love mediated the association between AD individuals’ compassionate love and caregivers’ positive appraisals of caregiving (We also examined the models with caregiver compassionate love predicting AD compassionate love predicting burden [as well as predicting positive appraisals]. Results of these models did not support this pathway [burden: indirect effect = −0.96, SE = 0.80, 95% CI: [0.60, −1.20], p = .22; positive appraisals: indirect effect = 0.10, SE = 0.82, 95% CI: [−1.51, 1.70], p = .90]). Because neither partner’s compassionate love was associated with caregivers’ depressive symptoms, it was not necessary to test for mediation between AD individuals’ compassionate love and caregivers’ depressive symptoms.
Figure 2.
Mediation model predicting caregiver positive appraisals: direct and total effects. Notes: Unstandardized betas are presented. In parentheses is the beta coefficient when the mediator is not included in the model. Standardized betas are .54 for Alzheimer’s disease (AD) compassionate love → CG compassionate love, .54 for CG compassionate love → appraisals, and .31 (.02 when mediator is included) for AD compassionate love → appraisals. **p < .01. *p < .05.
Discussion
The results of this study showed that caregivers who felt more compassionate love for their partners with AD reported less caregiving burden and more positivity in their caregiving role than caregivers who felt less compassionate love for their partners with AD. This is consistent with previous research showing that compassionate love is associated with increased positive emotions and greater psychological well-being in younger adults (Crocker & Canevello, 2008; Sprecher & Fehr, 2006) but extends past research by demonstrating the psychological benefits of compassionate love in the context of dementia caregiving.
In addition, we found that caregivers’ and AD individuals’ compassionate love were highly related to each other, such that caregivers’ who were high in compassionate love were likely to have partners who were also high in compassionate love. This is one of the first studies to examine the association between spouses’ reports of compassionate love. Although studies of close relationships often show that partners are similar in their thoughts, feelings, and behaviors (Shiota & Levenson, 2007) and recent research shows that perceptions of compassionate love are similar for newlyweds (Reis, Maniaci, & Rogge, 2013), it was interesting to see that this held true among older spouses in which one person had dementia. It suggests that mutuality of the spousal relationship may endure after a dementia diagnosis, even when physical and cognitive needs may become unbalanced (Williamson & Shaffer, 2001).
The fact that caregivers’ compassionate love mediated the relationship between AD individual’s compassionate love and reduced burden and positive appraisals provides support for past research showing that feeling compassionate love for others may be more directly beneficial for psychological health than receiving compassionate love from others (Sprecher & Fehr, 2006). However, a partners’ compassionate love is still important. Our findings suggest that compassionate love in one partner can facilitate compassionate love in the other partner, with compassionate love being mutually reinforced (Canevello & Crocker, 2010; Clark & Monin, 2006). Consistent with this idea, Roberts and coworkers (2009) found in their qualitative study of caregivers and end-of-life patients that compassionate love seemed to be most easily supported and maintained when it was experienced as a process of mutual give and take between partners. They described that caregivers opened patients to new levels of gratitude, love, and compassion, and similarly the patient’s ability to act out of compassion opened the caregiver to continuing self-sacrifice, patience, and tending, a “self-reinforcing feedback loop” (Roberts et al., 2009, p. 336).
Finally, although compassionate love was associated with less caregiving burden and more positive appraisals of caregiving, and caregiving burden was associated with less depressive symptoms (also reported in Schulz et al., 2010), compassionate love was only marginally associated with less depressive symptoms. One possible explanation for only finding a trend is that compassionate love may be a double edged sword for some caregivers coping with dementia, where psychological distance with the partner and the threat of death are salient. On the one hand, compassionate love reduces the burden of caring for a loved one, but on the other hand, it represents increased psychological closeness or empathy, which may make caregivers more vigilant to their partner’s suffering and cause depression to persist (Monin & Schulz, 2009). The fact that compassionate love is not significantly associated with a reduction in depressive symptoms is also consistent with theory and research indicating that despair is a common reaction to impending loss (Bowlby, 1980).
Limitations and Future Directions
Future research should continue to examine issues of mutuality of compassionate love in the context of dementia caregiving by examining both partners’ compassionate love and well-being simultaneously. For example, dyadic models such as the Actor–Partner Interdependence Model could examine the influence of both partners’ compassionate love on both partners’ psychological health as well as their marital satisfaction. In our study, we did not have the same type of measures of psychological health for care givers and care recipients. Future research should examine other potential mediators for the association between both partners’ compassionate love and both partners’ psychological health, such as care recipients’ feelings about receiving support from their partners and caregivers’ perceptions of support in their social networks. Another limitation of the present study is that it was cross-sectional so we were not able to detect directionality or causality of effects. Future research should examine these associations longitudinally. Related to this, although our mediational analysis showed that caregiver compassionate love mediated the relationship between AD individuals compassionate love and caregiver psychological health, we cannot determine whether caregivers’ compassionate love leads to care recipients’ compassionate love or vice versa. Rather we showed that caregivers’ compassionate love is more closely related to their own psychological health. This may be in part because the same person is reporting on both measures. Partner associations are usually weaker due to differences in perception and communication (Reis et al., 2013).
Also, because our sample was small and caregivers were predominantly women, we were not able to examine gender differences in spouses’ feelings of compassionate love or whether there were moderating effects of gender on the links between compassionate love and psychological health. We might hypothesize that female caregivers benefit more than male caregivers when female caregivers report greater compassionate love. There is a consistent finding among younger adults that women report greater compassionate love and altruism than men (Perlman & Aragon, 2009). Also, research by Neff and Karney (2009) suggests that among newlywed husbands and wives who report feelings of compassionate love for their spouses, only for wives does feeling compassionate love predict positive outcomes (e.g., supportive behaviors, marital efficacy, and likelihood of divorce). Future research should examine gender differences in the context of spouses caring for their partners with dementia. Likewise it will be important to collect information from more diverse samples so that we can examine cultural differences in compassionate love in caregiving.
Implications
Results of this study have a number of implications. First, assessing caregivers’ and care recipients’ feelings of compassionate love for their partners may identify caregivers who are resilient and those who are at heightened risk for negative mental health consequences. It may also identify caregivers who are at risk for being abusive toward the care recipient, as lack of gratification in the caregiving role has been linked to a heightened risk of this type of behavior (Nolan, Grant, & Keady, 1996). Second, interventions that foster caregiver’s and care recipients’ compassionate love for their partners may be particularly beneficial for caregivers’ mental health (Martire, Schulz, Helgeson, Small, & Saghafi, 2010). Pinquart and Sörensen (2003) have suggested that psychosocial interventions for caregivers should focus on enhancement of the positive aspects of caring. Enhancing feelings of compassionate love may reinforce caregiver’s psychological well-being and reduce caregiving stress and burden. This may also contribute to maintaining caregivers’ involvement (Carbonneau et al., 2010), which could be especially important for spousal caregivers of individuals with dementia who may feel they are slowly losing an intimate partner during the disease process. De Vugt and colleagues (2003) have noted that although caregivers often experience deterioration in their relationships with their loved ones, a sense of closeness can remain. Finally, this research adds to the body of work emphasizing positive aspects of caregiving and how they may be protective for caregivers’ health. Theoretical frameworks that focus on caregiving stress only may limit the ability to understand the antecedents and consequences of positive aspects of caregiving (Carbonneau et al., 2010). Findings from the present study highlight the importance of focusing on one such positive aspect, compassionate love, especially in dementia caregiving, as it has important consequences for caregivers’ mental health.
Funding
Preparation of this manuscript was in part supported by grants from the Alzheimer’s Association (IIRG-07-59784) and the National Institute on Aging (P50 AG05133, AG015321, AG026010, K01 AG042450-01, P30AG021342).
References
- Aiken L. S., West S. G. (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage. [Google Scholar]
- Alzheimer’s Association. (2013). 2013 Alzheimer’s disease facts and figures Retrieved from http://www.alz.org/downloads/facts_figures_2013.pdf
- Beach S. R., Schulz R., Yee J. L., Jackson S. (2000). Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the caregiver health effects study. Psychology and Aging, 15, 259–271. 10.1037//0882-7974.15.2.259 [DOI] [PubMed] [Google Scholar]
- Bédard M., Molloy D. W., Squire L., Dubois S., Lever J. A., O’Donnell M. (2001). The Zarit Burden Interview: A new short version and screening version. The Gerontologist, 41, 652–657. 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- Berscheid E., Dion K., Walster E., Walster G. W. (1971). Physical attractiveness and dating choice: A test of the matching hypothesis. Journal of Experimental Social Psychology, 7, 173–189.10.1016/0022-1031(71)90065-5 [Google Scholar]
- Boerner K., Schulz R., Horowitz A. (2004). Positive aspects of caregiving and adaptation to bereavement. Psychology and Aging, 19, 668–675. 10.1037/0882-7974.19.4.668 [DOI] [PubMed] [Google Scholar]
- Bowlby J. (1980). Loss: Sadness and depression (Vol. 3). New York: Basic Books Classics. [Google Scholar]
- Canevello A., Crocker J. (2010). Creating good relationships: Responsiveness, relationship quality, and interpersonal goals. Journal of Personality and Social Psychology, 99, 78–106. 10.1037/a0018186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonneau H., Caron C., Desrosiers J. (2010). Development of a conceptual framework of positive aspects of caregiving in dementia. Dementia, 9, 327–353. 10.1177/1471301210375316 [Google Scholar]
- Clark M. S., Monin J. K. (2006). Giving and receiving communal responsiveness as love. In Sternberg R. J., Weis K. (Eds.), The new psychology of love (2nd ed.). New Haven, CT: Yale University Press. [Google Scholar]
- Crocker J., Canevello A. (2008). Creating and undermining social support in communal relationships: The role of compassionate and self-image goals. Journal of Personality and Social Psychology, 95, 555–575. 10.1037/0022-3514.95.3.555 [DOI] [PubMed] [Google Scholar]
- Crocker J., Canevello A. (2012). Egosystem and ecosystem: Motivational perspectives on caregiving. In Brown S. L., Brown R. M., Penner L. A. (Eds.), Moving beyond self-interest: Perspectives from evolutionary biology, neuroscience, and the social sciences (pp. 211–223). [Google Scholar]
- De Vugt M. E., Stevens F., Aalten P., Lousberg R., Jaspers N., Winkens I, … Verhey F. (2003). Behavourial disturbances in dementia patients and quality of marital relationship. International Journal of Geriatric Psychiatry, 18, 149–154. 10.1002/gps.807 [DOI] [PubMed] [Google Scholar]
- Fehr B., Sprecher S., Underwood G. (Eds.). (2009). The science of compassionate love: Theory, research, and applications. Malden, MA: Blackwell. [Google Scholar]
- Folstein M. F., Folstein S. E., McHugh P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. [DOI] [PubMed] [Google Scholar]
- Irwin M., Artin K. H., Oxman M. N. (1999). Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Archives of Internal Medicine, 159, 1701–1704. 10.1001/archinte.159.15.1701 [DOI] [PubMed] [Google Scholar]
- Jaccard J., Turrisi R. (Eds.). (2003). Interaction effects in multiple regression (Vol. 72). Newbury Park: Sage. [Google Scholar]
- Katz S., Ford A. B., Moskowitz R. W., Jackson B. A., Jaffe M. W. (1963). Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA, 185, 914–919. 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- Kenny D. A., Kashy D. A., Cook W. L. (2006). Dyadic data analysis. New York: The Guilford Press. [Google Scholar]
- MacKinnon D. P., Lockwood C. M., Williams J. (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99. 10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire L. M., Schulz R., Helgeson V. S., Small B. J., Saghafi E. M. (2010). Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine, 40, 325–342. 10.1007/s12160-010-9216-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin J. K., Schulz R. (2009). Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging, 24, 681–695. 10.1037/a0016355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin J. K., Schulz R., Kershaw T. S. (2013). Caregiving spouses’ attachment orientations and the physical and psychological health of individuals with Alzheimer’s disease. Aging & Mental Health, 17, 508–516. 10.1080/13607863.2012. 747080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff L. A., Karney B. R. (2009). Compassionate love in early marriage. In Fehr B., Sprecher S., Underwood L. G. (Eds.), The science of compassionate love: Theory, research, and applications (pp. 201–222). Malden, MA: Wiley-Blackwell. [Google Scholar]
- Nolan M., Grant G., Keady J. (1996). Understanding family care. Buckingham, UK: Open University Press. [Google Scholar]
- Perlman D., Aragon R. S. (2009). Compassionate love: Concluding reflections. In Fehr B., Sprecher S., Underwood L. G. (Eds.), The science of compassionate love: Theory, research, and applications (pp. 433–452). Malden, MA: Wiley-Blackwell. [Google Scholar]
- Pinquart M., Sörensen S. (2003). Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. Journal of Gerontology: Psychological Sciences, 58, 112–126. 10.1093/geronb/58.2.P112 [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731. 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- Reis H. T., Maniaci M. R., Rogge R. D. (2013). The expression of compassionate love in everyday compassionate acts. Journal of Social and Personal Relationships. Advance online publication. 10.1177/0265407513507214 [Google Scholar]
- Roberts L. J., Wise M., DuBenske L. L. (2009). Compassionate family caregiving in the light and shadow of death. In Fehr B., Sprecher S., Underwood L. G., Fehr B., Sprecher S., Underwood L. G. (Eds.), The science of compassionate love: Theory, research, and applications (pp. 311–344). Malden, MA: Wiley-Blackwell. [Google Scholar]
- Schulz R., Belle S. H., Czaja S. J., Gitlin L., Wisniewski S., Ory M. G. (2003). Introduction to the special section on Resources for Enhancing Alzheimer’s Caregiver Health (REACH). Psychology and Aging, 18, 357–360. 10.1037/0882-7974.18.3.357 [DOI] [PubMed] [Google Scholar]
- Schulz R., Monin J. K., Czaja S. J., Lingler J. H., Beach S. R., Martire L. M, … Cook T. B. (2010). Measuring the experience and perception of suffering. The Gerontologist, 50, 774–784. 10.1093/geront/gnq033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiota M. N., Levenson R. W. (2007). Birds of a feather don’t always fly farthest: Similarity in Big Five personality predicts more negative marital satisfaction trajectories in long-term marriages. Psychology and Aging, 22, 666–675. 10.1037/0882-7974.22.4.666 [DOI] [PubMed] [Google Scholar]
- Sprecher S., Duck S. (1994). Sweet talk: The importance of perceived communication for romantic and friendship attraction experienced during a get-acquainted date. Personality and Social Psychology Bulletin, 20, 391–400. 10.1177/0146167294204006 [Google Scholar]
- Sprecher S., Fehr B. (2005). Compassionate love for close others and humanity. Journal of Social and Personal Relationships, 22, 629–651. 10.1177/0265407505056439 [Google Scholar]
- Sprecher S., Fehr B. (2006). Enhancement of mood and self-esteem as a result of giving and receiving compassionate love. Current Research in Social Psychology, 11, 227–242. [Google Scholar]
- Sprecher S., Fehr B., Zimmerman C. (2007). Expectation for mood enhancement as a result of helping: The effects of gender and compassionate love. Sex Roles, 56, 543–549. 10.1007/s11199-007-9192-6 [Google Scholar]
- Williamson G. M., Shaffer D. R. (2001). Relationship quality and potentially harmful behaviors by spousal caregivers: How we were then, how we are now. Psychology and Aging, 16, 217–226. 10.1037/0882-7974.16.2.217 [PubMed] [Google Scholar]