Abstract
Despite extensive evidence for cognitive deficits associated with drug use and multiple publications supporting the efficacy of cognitive rehabilitation treatment (CRT) services for drug addictions, there are a few well-structured tools and organized programs to improve cognitive abilities in substance users. Most published studies on cognitive rehabilitation for drug dependent patients used rehabilitation tools, which have been previously designed for other types of brain injuries such as schizophrenia or traumatic brain injuries and not specifically designed for drug dependent patients. These studies also suffer from small sample size, lack of follow-up period assessments and or comprehensive treatment outcome measures. To address these limitations, we decided to develop and investigate the efficacy of a paper and pencil cognitive rehabilitation package called NECOREDA (Neurocognitive Rehabilitation for Disease of Addiction) to improve neurocognitive deficits associated with drug dependence particularly caused by stimulants (e.g. amphetamine type stimulants and cocaine) and opiates. To evaluate the feasibility of NECOREDA program, we conducted a pilot study with 10 opiate and methamphetamine dependent patients for 3 months in outpatient setting. NECOREDA was revised based on qualitative comments received from clients and treatment providers. Final version of NECOREDA is composed of brain training exercises called “Brain Gym” and psychoeducational modules called “Brain Treasures” which is implemented in 16 training sessions interleaved with 16 review and practice sessions. NECOREDA will be evaluated as an add-on intervention to methadone maintenance treatment in a randomized clinical trial among opiate dependent patients starting from August 2015. We discuss methodological features of NECOREDA development and evaluation in this article.
Keywords: Cognitive enhancers, Drug addiction, NECOREDA, Treatment
1. Introduction
Neuroplasticity is defined as an inherent property of neural circuits to alter their structure, function, and connectivity in response to intrinsic or extrinsic stimuli (Cramer et al., 2011). This phenomenon may occur at any age during development, in response to new experiences, during new information learning, in response to disease, or in relation to therapy (Cohen et al., 1997). Such plasticity allows brain to adapt new pattern of neural connectivity in response to different conditions. For example, previous studies show that after CNS injuries such as cerebral infarction, a range of brain events occurred both during spontaneous recovery and as a result of rehabilitation therapy (Cramer et al., 2011). These events may include formation of new synaptic connections (Green, 2003; Grefkes et al., 2008), strengthening of synaptic connections (Langton Hewer, 1990), development of projections from neurons on the undamaged side of the brain to denervated areas (Chen, Goldberg, Kolb, Lanser, & Benowitz, 2002), shifting in inter-hemispheric balance towards the uninjured hemisphere (Landau & Wetzel, 2005) or changing the direction of somatotopic map (Milot & Cramer, 2012). These plasticity pathways are considered as a central factor in returning the normal brain functions or ameliorating cognitive impairments following brain injuries (e.g. cerebral infarction), neurodegenerative conditions (e.g. Alzheimer disease), developmental disorders (e.g. Attention Deficit Hyperactivity Disorder), and other neuropsychiatric disorders (e.g. Schizophrenia, bipolar or major depression and addictive disorders)(Cramer et al., 2011).
Based on the emerging field of neuroplasticity and the evidence that brain functional impairment can be gradually repaired over time, researchers began exploring ways to improve cognitive functions, and thus the field of cognitive rehabilitation treatment (CRT) was born (Eack, 2013). CRT is a general term for specialized treatment procedures applied to improve cognitive functions such as attention, memory, problem solving, and planning. This approach uses various techniques and methods to restore neurocognitive abilities of patients and compensate their impairments. Recent studies showed that cognitive deficits resulting from chronic substance abuse can be improved in response to CRT, given as an add-on to usual clinical care (Fals-Stewart & Lam, 2010; Sofuoglu, Devito, Waters, & Carroll, 2012; Alam-Mehrjerdi, 2012; Ekhtiari, 2014). Patients with substance use disorders suffer from a wide range of neurocognitive impairments depending on the duration, frequency, routes of administration, amount and types of drug use (Ahmadi-Soleimani et al., 2016). Multiple studies have reported that long-term use of stimulant, especially cocaine or methamphetamine smoking is associated with deficits in cognitive functioning, including decision-making, response inhibition, planning, working memory, and attention (Fernández-Serrano, Perales, Moreno-López, Pérez-García, & Verdejo-García, 2012; Nordahl, Salo, & Leamon, 2003; Sofuoglu et al., 2012). Many studies reported that the prolonged use of opiates, such as heroin, is associated with a deleterious effect on cognitive functioning such as planning, response inhibition, decision-making, planning, memory and learning, visual perception, and attention (Gould, 2010; Prosser et al., 2006). It is notable that these impairments could become even worse after consumption of substitution medications, especially methadone (Davis, Liddiard, & Mcmillan, 2002; Prosser et al., 2006). For these reasons CRT should be considered as a potentially effective treatment method, which could target different neurocognitive domains and improve treatment outcomes in addiction medicine. Few previous studies have reported that the positive effects of adding CRT to standard addiction treatment on not only improved cognitive function but also engagement in treatment, abstinence and retention (Fals-Stewart & Lam, 2010). In a recent review of published studies in the field of addiction medicine and CRT, we found a broad variation in length of time, CRT tools and methods (e.g., restorative exercises versus compensatory strategy), duration and treatment setting (e.g., individual versus group session, inpatient versus outpatient). This variation may be due to lack of acceptable and standard protocols and guidelines for using CRT in drug addictions (Rezapour, DeVito, Sofuoglu & Ekhtiari, 2016). This gap between cognitive neuroscience and addiction medicine encouraged us to focus our efforts on developing a specialized CRT program for substance users seeking for treatment, especially with opiate and stimulant dependencies.
2. NECOREDA Program
During the past two decades burgeoning evidence indicates the potential efficacy of CRT for improving neurocognitive deficits in drug dependent patients, few centers and several treatment have integrated CRT to their standard addiction treatment. The treatment exercises range from solving simple Sudoku exercises to highly sophisticated computerized training programs (Eack, 2013). The CRT approaches that have been applied for addictions are almost identical to those that have been used for other brain injuries such as TBI, Alzheimer’s and Stroke, perhaps due to lack of CRT programs, which are specifically designed for patients with drug dependence.
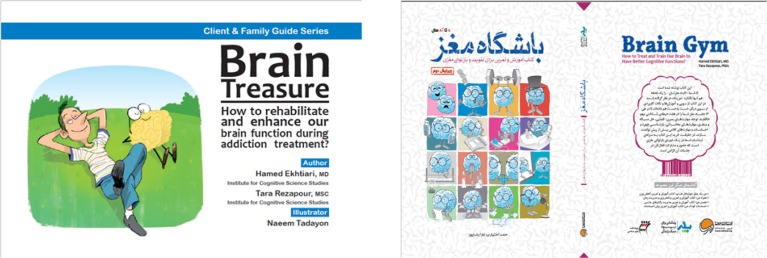
Considering these limitations, we designed NECOREDA as a paper and pencil neurocognitive rehabilitation program for disease of addiction focused stimulants (e.g. AMPH, METH, cocaine) and opiate dependent individuals. NECOREDA is a structured rehabilitation course developed to restore cognitive abilities and compensate cognitive deficits of drug addicted patients. It consists of an array of exercises (mainly game based) designed to target the neurocognitive deficits reported in previous studies on opiate and stimulants dependence. Therefore, NECOREDA has 2 domains: cognitive training exercises named “Brain Gym” and psychoeducational modules called “Brain Treasure” (See both book covers in Figure 1).
Figure 1:.
Covers for two main published materials for clients. NECOREDA has Two main parts: Brain training exercises called “Brain Gym” and psychoeducational modules called “Brain Treasure”.
NECOREDA is a 2-month course provided for CRT and consists of 16 steps that each step has 2 interrelated sections namely enhancement and consolidation. Enhancement section is a class work exercise, which should be completed in a group session with a therapist or a skilled coach. Parallel to each enhancement section, we designed a homework (for outpatient settings) or inter-session (for residential settings) exercise to consolidate the skills learned in classroom session. The homework will be completed individually. We developed these two basically similar sections according to the theory that repetition of training as an efficient way to enhance neuroplasticity and reshaping of neural networks (Kaneko & Keshavan, 2012). Enhancement sessions are conducted 2 times a week and each takes 1 hour. Each session consisted of two 30-minute training session and 10-minute break in between.
As the most effective CRT programs target broad cognitive domains, NECOREDA is designed as a multiple-component package that organized in 6 modules, addressing those cognitive deficits following long-term opioid abuse. These cognitive deficits are attention, calculation, visuospatial process, memory, verbal skills and logic/problem solving.
Attention Module: Because of the importance of attention deficits in stimulants and opiates users, 11 steps involve exercises that focus on different types of attention, including sustained/selective attention, divided attention, and shifting attention through exercises such as spot the differences, finding hidden objects, working on the Stroop test, finding similar or odd objects, trial making and letter(s), number(s), and object(s) cancellation.
Calculation: This module include training to improve numerical skills through different types of mathematical puzzles enhances the speed of mental processing that is considered as one of basic building blocks of cognition. This cognitive module is applied in 7 steps.
Visuospatial process: This module has been designed to enhance visual attention, spatial imagination, and the ability to mentally manipulate visual information through 7 steps. Exercises such as determining spatial direction, mental rotation, maze, drawing symmetrical figures, and visual puzzles are provided in this cognitive module.
Memory: The aim of this module is to improve both long-term and working memory. Multiple dimensions of working memory, including verbal rehearsal and visuospatial sketchpad are targeted through picture and word recalling exercises. The other type of memory emphasized in NECOREDA is semantic memory, which is stimulated through solving crosswords. Memory module is embedded in 7 steps of NECOREDA.
Verbal skills: This module is designed to improve patient’s verbal fluency and to make more social interaction between participants during sessions. In this module, clients should write a text based on pictures or presented words during a short time (at most 4 minutes) and then read it aloud for others.
Logic/Problem solving: We have targeted different high order cognitive functions to stimulate the ability of clients to logically solve problems. Exercises such as Tower of Hanoi, Sudoku, finding logical relation between objects and numbers as well as story sequencing are provided in this module during 7 steps.
Each step targets at most, 3 cognitive modules in a hierarchical fashion from lower-order (e.g. attention) to higher order cognitive functions (e.g. problem solving). For example, the main focus of step 1 is on attention and calculation, step 2 on attention and visuospatial process and step 3 on memory, verbal fluency, and logic/problem solving. This architecture of cognitive training is followed through 16 steps with gradual increase in the difficulty of exercises from level 1 to level 5. It means that all exercises begin with simpler levels and progress to more complex ones during 14 steps. The last two steps (steps 15 and 16) are considered as review section and include all training domain with the highest level of difficulty (5). Table 1 shows the architecture of NECOREDA exercises for 16 steps.
Table 1.
Architecture of NECOREDA Exercises for 16 Steps.
| Steps | Cognitive Modules | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Attention | Calculation | Visuospatial process | Memory | Verbal skills | Logic and Problem solving | |||||||||||||||
| Spotthe differences | Finding hidden objects | Stroop | Cancellation | Finding similar, odd objects | Trial making | Math ematical puzzles | Spatial direction | Mental rotation | Puzzle | Drawing symmetrical | Maze | Word recalling | Picture recalling | Crosswords | Writing story | Tower of Hanoi | Sudoku | Finding logical relation | Story sequencing | |
| 1st | 1 | 1 | 1 | 1 | ||||||||||||||||
| 2ed | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||
| 3th | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||
| 4th | 2 | 2 | 2 | 2 | ||||||||||||||||
| 5th | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | ||||||||||||
| 6th | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | ||||||||||||
| 7th | 3 | 3 | 3 | 3 | ||||||||||||||||
| 8th | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | ||||||||||||
| 9th | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | ||||||||||||
| 10th | 4 | 4 | 4 | 4 | ||||||||||||||||
| 11th | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | ||||||||||||
| 12th | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | ||||||||||||
| 13th | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | |||||||||
| 14th | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | |||||||||||
| 15th | Review | |||||||||||||||||||
| 16th | Review | |||||||||||||||||||
In addition to brain exercise program, NECOREDA has been designed to incorporate psychoeducation section by considering 3 main components:
Metacognitive Education: It consists of two parts; general and specific information. General part offers clients some information about brain structure and cognitive functions while specific part is devoted to more customized information for drug addicted patients such as the effects of drug use on nervous system and process, symptoms of cognitive deficits, and the ways that patients can be aware of their deficits. Metacognition part in NECOREDA assists patients to know about their status of brain performance as a result of drug use and to perceive the necessity of using CRT as one of their therapeutic service. Better metacognitive abilities will help clients to transfer their enhanced abilities during cognitive exercise to real life tasks.
Compensatory Trainings: Compensatory approaches attempt to recruit intact cognitive process to bypass cognitive impairments and improve targeted behaviors and functional outcomes. This training approach emphasizes on teaching mnemonic, attention, speed, and problem solving strategies that could be easily applied in daily life activities. The importance of teaching compensatory strategies lies in their durability which is significantly longer than that of restorative approaches (Twamley et al., 2008).
Lifestyle Trainings: Teaching the clients with the most influential lifestyle skills that improve and promote brain functions is considered in the third component of psychoeducational part. Encouraging healthy eating habits, daily physical exercise, regular sleep pattern, feeling positive emotion, performing neurobic exercises, and making positive social interaction are considered in this component.
Psychoeducational modules have been organized for 32 parts (parallel to enhancement and consolidation sections) that are presented to patients by an instructional booklet. Table 2 shows the architecture of educational titles of NECOREDA. Most of these trainings are supported with cartoons in the educational booklet (See sample cartoons in Figure 2).
Table 2.
Architecture of Psychoeducational Titles Presented during NECOREDA Program.
| Session | Title |
|---|---|
| 1 | Introduction about Psychoeducation in Brain Injuries |
| 2 | What Is Brain and Its Function? |
| 3 | The Effects of Drug Abuse on My Brain? |
| 4 | What Are the Symptoms of Drug Abuse on My Brain? |
| 5 | Am I Suffer from Brain Injury? |
| 6 | How Can I Diagnose My Brain Injury? |
| 7 | How Should I Face with My Brain Injury? |
| 8 | What Is Cognitive Rehabilitation? |
| 9 | Why Do I Need Cognitive Rehabilitation? |
| 10 | What Is the Role of Sleep in Cognitive Rehabilitation? |
| 11 | What Is the Healthy Diet for Improving Cognitive Functions? |
| 12 | How Can Stress and Anxiety Affect My Brain? |
| 13 | What Is the Effect of Fatigue and Depression on My Brain? |
| 14 | What Is the Effect of Regular Exercise on My Brain? |
| 15 | How Can Positive Leisure Activities Affect My Brain? |
| 16 | What Type of Mental Games Can Help My Brain? |
| 17 | How Can Painting and Drawing Help My Brain? |
| 18 | Does Writing Diaries Help My Brain? |
| 19 | How Can Daily Programming Help My Brain? |
| 20 | Does Reading Book Help My Brain? |
| 21 | How Can I Help My Brain by Recalling Old Memories? |
| 22 | How Can Learning New Skills Help My Brain? |
| 23 | How Can I Help My Brain with Social Interaction? |
| 24 | What Is Neurobic Exercises? |
| 25 | How Can I Improve My Memory? |
| 26 | How Can I Improve My Attention? |
| 27 | How Can I Speed up My Performance? |
| 28 | How Can I Make Better Decisions? |
| 29 | How Can I Efficiently Use My Mental Energy during Cognitive Rehabilitation? |
| 30 | Can I Control My Craving with My Cognitive Abilities? |
| 31 | What Is the Importance of Brain in Controlling Drug Craving? |
| 32 | Conclusion and Review |
Figure 2.
Sample Cartoons in the Psychoeducational Booklet of NECOREDA.
3.3. CRT with NECOREDA: Protocols for a clinical trial
To evaluate the feasibly of NECOREDA in the context of clinical application and also to plan for full scale clinical trial in the field of addiction medicine, we conducted a pilot study with 10 addicted patients with opiate and/or methamphetamine dependence who had entered to MMT course for opiates and Matrix program for methamphetamine in outpatient setting. We implemented CRT with NECOREDA as a supplementary treatment section. Patients received NECOREDA twice a week as “group therapy” sessions interleaved with homework individual sessions during two months.
The aim of the pilot study was to evaluate the level of comprehensibility of exercises and education materials which were presented by trained therapist. During this phase, we collected therapists and patient’s suggestions related to the NECOREDA and revised the content of the package based on these quantitative feedbacks. Although we did not use cognitive assessments for this pilot study, we asked our clients to write us about their attitude, perceived changes, and satisfaction from participating in the CRT course. According to their letters, we found much satisfaction among clients with their experiences during the course and high levels of willingness to continue it after termination of the NECOREDA sessions. They also noticed some obvious changes in their daily life activities such as improvements in their attention, working memory, spatial perception, and the speed of information processing. After this pilot study, we planned for our main RCT in a sample of 120 clients.
The RCT study is designed as a comparative, evaluator-blinded, randomized, and parallel clinical trial to determine the efficacy of cognitive rehabilitation with NECOREDA for opiate dependent (OD) patients as a supplementary treatment during MMT. In the trial, patients who enter medium term (two months) residential care during specific time and meet our inclusion criteria (age 20–40, ability to read and speak in Farsi, meet DSV-IV-TR criteria for opiate dependence, to give written informed consent) will be selected to participate in the trial. Our exclusion criteria are suffering from serious chronic mental disease, demonstration of withdrawal symptoms at the end of first 2-weeks admission, or a history of a suicide attempt during last month.
All recruited clients with OD will be interviewed by an expert drug counselor based on a structured form, including demographic information, history of type and frequency of substance use and previous treatment experiences. With regard to the collected information and the scores of withdrawal symptoms monitored during the first two weeks of MMT induction process, 120 male patients will be chosen and randomly classified into two groups; intervention (n=60) or control group (n=60). Process of sampling and classification of participants will be performed every two months with 40 admitted patients to form 4 parallel 10-patients groups. The baseline cognitive assessments are administered individually for all patients with an experienced and skilled psychologist.
These assessments include the Digit Span Test (forward and backward), the Trail Making Task (part B), the Auditory Verbal Learning Test (AVLT), Digit-Symbol Substitution (DSS), the Verbal Fluency Task (VFT), and the Stroop task. Following the pre-assessment sessions, control groups receive treatment as usual (TAU) with MMT program and intervention group assign in cognitive rehabilitation course plus receiving TAU for 2 months.
Participants in the CR group are scheduled for 16 one-hour group sessions (enhancement section) and 16 one-hour individual sessions (consolidation section), four times a week. After each training session, participants will be asked to rate their fatigue and happiness level as well as their craving intensity with scale ranging from 0–100. Barratt Impulsiveness Scale (BIS-11) will also be used in baseline and during follow-ups to study the relation between impulsiveness and the effect of CRT on patients. The midterm assessment, after the end of 16th step, will be administered as the same as baseline from both groups and will be redone after the end of 32nd step (before discharging from the residential center).
All subjects will be followed up after termination of 2-month residential MMT program for 1 month in an outpatient MMT center. Two alternative forms of assessment tests will be used consecutively during 4 times of assessments (baseline, midterm, end of the treatment, and first month of follow up). In addition to these comprehensive evaluations, we will use backward digit span as dynamic cognitive measure every other 2-week from both groups to monitor the long-term effect of CRT on cognitive performance. We also consider therapist’s attitude through the effect of CRT with a questionnaire that asks about patient’s participation in TAU (from both group) and their satisfaction from CRT (from intervention group) with scales ranging from 1–5.
After discharging from residential center, during their 1-month follow up, patients (both groups) will give urine test for opiates, every 3 days to monitor the abstinence and perform cognitive assessments at the end of this period to examine the durability of CRT effects. The follow-up assessments will be done during outpatient MMT program. The trial will be conducted in the line with previous studies associated with CRT in addiction, to evaluate the effect of using NECOREDA as a specifically developed CRT package for substance users on cognitive improvements as well as addiction treatment outcomes.
4. Discussion
To summarize, cognitive rehabilitation could be considered as an efficient supplementary treatment approach that can be used addiction medicine, which neglected neurocognitive impairments in substance users. These neurocognitive impairments not only affect the quality of patient’s life, but also make abstinence and recovery process more difficult. As reviewed in this article, NECOREDA package would be one of the first CRT packages that have been developed specifically to target the cognitive deficits and educational needs for rehabilitation of people with stimulant and opiates abuse disorders. We hope future clinical trials will define the efficacy of this package in both addiction treatment outcomes i.e. treatment retention and negative urine tests and cognitive improvement terms.
Acknowledgements
The authors would like to acknowledge the invaluable contributions and helpful suggestions provided by Dr. Peyman Hassani-Abharian from Institute for Cognitive Sciences Studies (ICSS) and Dr. Schwann Shariatirad from Tehran University of Medical Sciences (TUMS).
We would also like to thank the outstanding contribution of Mrs. Gita Saeedi from Omid-e-Novin Clinical Center in Karaj, Iran during the pilot phase of the study. TR and AF have received supports from Cognitive Science and Technologies Council (CSTS) of Iran and Tehran University of Medical Sciences (TUMS) for the ongoing Clinical Trial with NECOREDA. HE has received funds from Tehran University of Medical Sciences for development of NECOREDA.
References
- Ahmadi-Soleimani A., Ekhtiari H., Cadet J. L. (2016). Drug-induced neurotoxicity Q1 in addiction medicine: From prevention to harm reduction. Progress in Brain Research. Advance online publication. doi: 10.1177/0268355513518912. [DOI] [PubMed]
- Alam-Mehrjerdi Z., Noroozi A., Barr A. M., Ekhtiari H. (2012). Attention deficits in chronic methamphetamine users as a potential target for enhancing treatment efficacy. Basic and Clinical Neuroscience, 3( 4), 5– 14. [Google Scholar]
- Chen P., Goldberg D. E., Kolb B., Lanser M., Benowitz L. I. (2002). Inosine induces axonal rewiring and improves behavioral outcome after stroke. Proceedings of the National Academy of Sciences of the United States of America, 99( 13), 9031– 9036. doi: 10.1073/pnas.132076299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen L. G., Celnik P., Pascual-Leone A, Corwell B., Falz L., Dambrosia J., et al. (1997). Functional relevance of cross-modal plasticity in blind humans. Nature, 389( 6647), 180– 183. doi: 10.1038/38278. [DOI] [PubMed] [Google Scholar]
- Cramer S. C., Sur M., Dobkin B. H., O’Brien Ch., Sanger T. D., Trojanowski J. Q., et al. (2011). Harnessing neuroplasticity for clinical applications. Brain, 134( 6), 1591– 1609. doi: 10.1093/brain/awr039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis P. E., Liddiard H., Mcmillan T. M. (2002). Neuropsychological deficits and opiate abuse. Drug Alcohol Dependence., 67( 1), 105– 108. [DOI] [PubMed] [Google Scholar]
- Eack S. M. (2013). Cognitive Remediation: A New Generation of Psychosocial Interventions for People with Schizophrenia. Social Work, 57( 3), 235– 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekhtiari H. (2014). Alcohol and Cognition; From Neurotoxicity Prevention to Cognitive Rehabilitation. Asia Pacific Journal of Medical Toxicology, 3( 1), 7– 7. [Google Scholar]
- Fals-Stewart W., Lam W. K. K. (2010). Computer-assisted cognitive rehabilitation for the treatment of patients with substance use disorders: a randomized clinical trial. Experimental and Clinical Psychopharmacology, 18( 1), 87– 98. doi: 10.1037/a0018058. [DOI] [PubMed] [Google Scholar]
- Fernández-Serrano M. J., Perales J. C., Moreno-López L., Pérez-García M., Verdejo-García A. (2012). Neuropsychological profiling of impulsivity and compulsivity in cocaine dependent individuals. Psychopharmacology, 219( 2), 673– 683. doi: 10.1007/s00213-011-2485-z. [DOI] [PubMed] [Google Scholar]
- Gould T. J. (2010). Addiction and Cognition, Addiction Science & Clinical Practice, 5(2), 4– 14. [PMC free article] [PubMed] [Google Scholar]
- Green J. B. (2003). Brain reorganization after stroke. Topics in Stroke Rehabilitation, 10( 3), 1– 20. doi: 10.1310/H65X-23HWQL1G-KTNQ. [DOI] [PubMed] [Google Scholar]
- Grefkes C., Nowak D. A., Eickhoff S. B., Dafotakis M., Küst J., Karbe H., et al. (2008). Cortical connectivity after subcortical stroke assessed with functional magnetic resonance imaging. Annals of Neurology, 63( 2), 236– 246. doi: 10.1002/ana.21228. [DOI] [PubMed] [Google Scholar]
- Kaneko Y., Keshavan M. (2012). Cognitive remediation in schizophrenia. Clinical Psychopharmacology and Neuroscience, 10( 3), 125– 135. doi: 10.9758/cpn.2012.10.3.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landau W. M., Wetzel R. D. (2005). Influence of somatosensory input on motor function in patients with chronic stroke. Annals of Neurology, 57( 3), 465– 466; author reply 466–467. [DOI] [PubMed] [Google Scholar]
- Langton-Hewer R. (1990). Rehabilitation after stroke. The Quarterly Journal of Medicine, 76( 279), 659– 674. doi: 10.1056/NEJM-cp043511. [DOI] [PubMed] [Google Scholar]
- Milot M. H., Cramer C. S. (2012). Biomarkers of recovery after stroke. Current Opinion in Neurology, 29( 6), 997– 1003. doi: 10.1016/j.biotechadv.2011.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordahl T. E., Salo R., Leamon M. (2003). Neuropsychological effects of chronic methamphetamine use on neurotransmitters and cognition: a review. The Journal of Neuropsychiatry and Clinical Neurosciences, 15( 3), 317– 325. doi: 10.1176/appi.neuropsych.15.3.317. [DOI] [PubMed] [Google Scholar]
- Prosser J., Cohen L. J., Steinfeld M., Eisenberg D., London E. D., Galynker I. I. (2006). Neuropsychological functioning in opiate-dependent subjects receiving and following methadone maintenance treatment. Drug and Alcohol Dependence, 84( 3), 240– 247. doi: 10.1016/j.drugalcdep.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezapour T., DeVito E. E., Sofuoglu M., Ekhtiari H. (2016). Perspectives on neurocognitive rehabilitation as an adjunct treatment for addictive disorders; from cognitive improvement to relapse prevention (unpublished). Progress in Brain Research, 1– 21. doi:http://dx.doi.org/10.1016/bs.pbr.2015.07.022 [DOI] [PubMed] [Google Scholar]
- Sofuoglu M., DeVito E. E., Waters A. J., Carroll K. M. (2012). Neuropharmacology cognitive enhancement as a treatment for drug addictions. Neuropharmacology, 64, 452– 463. doi: 10.1016/j.neuropharm.2012.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twamley E. W., Savla G. N., Zurhellen C. H., Heaton R. K., Jeste D. V. (2008). Development and pilot testing of a novel compensatory cognitive training intervention for people with psychosis. American Journal of Psychiatric Rehabilitation, 11(2), 144– 163. [DOI] [PMC free article] [PubMed] [Google Scholar]