Abstract
Objectives
Pelvic organ prolapse (POP) is a major cause of morbidity in Nepal, particularly affecting women in the rural communities. Women with POP in Nepal may suffer from symptoms for decades. At present, the Government of Nepal advocates surgical intervention but access to surgical care is inadequate. This report evaluated the feasibility of a non-surgical public health programme in rural Nepal, and describes risk factors associated with POP in this setting.
Design
Prospective monitoring and evaluation study of a new public health programme.
Setting
Baglung district, rural Nepal.
Participants
Women with gynaecological symptoms of POP.
Main outcome measures
Risk factors for disease progression were assessed using Fisher’s exact test, Pearson’s χ2-test and logistic regression analysis.
Results
Of the 74 women included in this analysis, 70.8% were diagnosed with stage 2 POP or greater. The majority of women did not have any further children following the onset of POP symptoms (63.5%). Duration of symptoms ranged from 2 months to 60 years, with 73.4% of women suffering for over 5 years and 28.4% suffering for over 20 years. Univariate analyses identified age at screening, age at onset of symptoms, the duration of symptoms and an associated rectocele as factors associated with increasing POP severity (p < 0.05). Kegel exercises were taught to 25 (33.8%) women with POP and ring pessaries were offered to 47 (63.5%) women with POP.
Conclusions
Non-surgical interventions may provide an opportunity to address the significant burden of POP in rural Nepal.
Keywords: Pelvic organ prolapse, uterine prolapse, vault prolapse, cystocele, rectocele, ring pessary, Kegel exercises, primary prevention, secondary prevention, maternal health, Nepal
Background
Pelvic organ prolapse (POP) is a major cause of morbidity in low-income settings among postmenopausal women as well as women of reproductive age.1 The Global Burden of Disease 2010 report recently estimated the prevalence of POP to be around 9% worldwide.2 In lower income countries, this figure was estimated to be closer to 20%, with wide variations among different populations.3 In Nepal, POP prevalence is estimated at 10% among women of reproductive age (between 15 and 49 years) and 24% among post-menopausal women between 45 and 49 years.4,5
Worldwide, POP risk factors include early marriage, high parity, squatting during delivery, prolonged labour, increasing age, menopause, hysterectomy, smoking, obesity, heavy lifting, and early return to work after parturition.6–14 Symptoms include stress urinary incontinence, urinary voiding problems, bowel changes, vaginal discharge, sexual dysfunction, vaginal bulge and lower abdominal pain.6,15,16
The social and economic repercussions for women with POP are unsettling.7 In Nepal, women have reported urinary incontinence, difficulty working, challenges with sitting down, loss of libido, infidelity among their husbands and domestic violence as a direct consequence of POP.17 A general lack of awareness and understanding perpetuates the stigma associated with this condition. Discrimination by family and society is common,17 and women with POP are often referred to as ‘phokundobhudhi’, meaning ‘women with a ball’ (Surya Bhatta, personal communication, May 2013).
In 2008, the Ministry of Health and Population (MoHP) of Nepal established a small fund to offer surgery to women with POP.18 Although surgery is widely considered as a definitive correction, in rural Nepal, however, the prospect of surgery faces many barriers including costs, limited availability of trained providers, and lack of transportation to district health centres.19 Temporary health camps have been established in some rural areas; however, these services are inadequate to address the burden of disease.20 Over 30% of cases among women aged 15 to 49 years in Nepal are estimated to warrant surgical intervention.4 Independent studies by clinicians from two tertiary referral centres have shown that POP is the primary indication for a vaginal hysterectomy in Kathmandu.21,22
Alternatives to surgery include Kegel’s exercises and ring pessaries.23,24 Non-surgical interventions are effective tools to tackle POP, and ring pessaries also relieve POP symptoms irrespective of stage.25–28 One Heart World-Wide (OHW) and Karuna Shechen (KS), two non-profit organisations with active programmes in rural Nepal, developed a collaborative POP programme offering non-surgical alternatives in order to gather more data on the feasibility of non-surgical interventions in a rural Nepali setting.29
This report has two objectives: the first is to describe and evaluate the feasibility of the joint OHW/KSPOP programme in Baglung district, rural Nepal; the second to describe risk factors associated with POP in rural Nepal.
Methods
Study settings
The OHW-KS POP programme was implemented in Batakachaur and Hatiya, two Village Development Committees (VDC) of Baglung district, Western Nepal. Each VDC is subdivided into nine wards of varying size. Batakachaur VDC has a population of 5351, with 12 female community health volunteers (FCHVs), 2 skilled birth attendants and 1 village health worker at the health post. Hatiya is a larger VDC with a population of 8661, 19 FCHVs, 3 skilled birth attendants and 1 village health worker at the health post. Patients were recruited from the 18 wards across Batakachaur and Hatiya. The study was conducted between January and June 2013.
Study design
This was a cross-sectional study. Women with gynaecological symptoms of POP were invited to participate. Women in the general community known to suffer from POP were actively recruited by the health staff through home visits, whereas women who attended the health post were passively recruited on general attendance. Our analysis focused on 74 women identified with uterine prolapse during the screening programme.
POP was categorised using the Baden-Walker classification system: stage 0 for no prolapse on clinical examination; stage 1 for prolapse into the vagina; stage 2 for prolapse until the introitus of the vagina; stage 3 for prolapse beyond the introitus of the vagina; and stage 4 for procidentia (complete vault eversion outside the vagina). The Baden-Walker classification system was chosen over the POP-Q primarily due to its simplicity in a clinical setting, particularly for non-gynaecological specialists. Uterine prolapse associated with cystocele (n = 36) or rectocele (n = 17) and vaginal vault prolapses post-hysterectomy (n = 2) were also documented.
This programme was ethically approved by the Social Welfare Council under the activities of One Heart World-Wide in Nepal. The clinical protocol, interview questionnaire and training materials were reviewed and approved by the Family Health Division of the Ministry of Health and Population (MoHP) and implemented in collaboration with SWAN (Social Welfare Association of Nepal, www.swannepal.org), One Heart World-Wide’s local partner in Baglung. Funding for the programme was provided by One Heart World-Wide.
Study participants
Skilled birth attendants and village health workers from Batakachaur and Hatiya were trained in the diagnosis, classification and management of POP using non-surgical methods. FCHV were trained on the symptoms, signs, risk factors, danger signs, and prevention of POP and asked to refer women to their local health post. After giving informed consent, the study participants were interviewed and examined by a trained community health worker. Women with stage 1 POP were counselled and consented for training in Kegel’s exercises. Women with stage 2 POP or greater were counselled and consented for silicone ring pessary insertion or referral to a surgical centre, if required. Silicone ring pessaries were distributed in preference to rubber ring pessaries, as they are easier to maintain. POP complications, such as decubitus ulcer, were managed in the community prior to the insertion of a ring pessary. Women were taught how to clean and self-insert the ring pessary, particularly for those living far from the health post.
The OHW-KS team collected data from each participant from 28 January to 16 May 2013 in Hatiya and from 3 March to 12 May 2013 in Batakachaur. Data from demographic and clinical records were anonymised, translated from Nepali to English and included in the analysis.
Statistical analysis
Fisher’s exact test and Pearson’s Chi2-test were used to compare differences between groups of women with varying degrees of POP (stages 1–2 vs. stages 3–4). We assessed risk factors for progression of POP severity.
Univariate logistic regression analysis was performed to assess the relation between the risk factors and severity of POP. Multivariate analysis was not performed due to the small sample size and the focus on a single dependent variable.
The significance for all tests was defined at the 5% level (two-sided p = 0.05). All information was verified, anonymised and entered into a secure database with restricted access to maintain confidentiality. Statistical analysis and generation of figures were performed using Stata software (version 11).
Results
Descriptive statistics
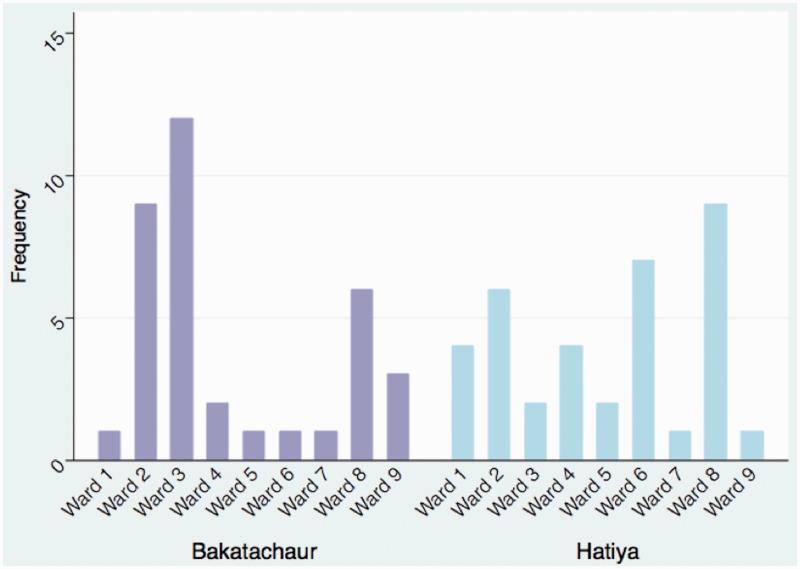
Between January and May 2013, the POP screening programme diagnosed 74 women with POP. The characteristics of the women with POP are presented in Table 1. A total of 36 women (48.6%) were diagnosed with POP in Batakachaur and 38 women (51.4%) in Hatiya. The distribution of these cases according to Ward was unequal (Figure 1), reflecting the transportation barriers to access health care in this region.
Table 1.
Characteristics of women with POP.
| Parameter (years) | Descriptive statistics |
|---|---|
| Age (n = 74) | |
| Mean (sd) | 53 ( ± 17.8) |
| Median (iqr) | 53.5 (39–67) |
| Range | 23–90 |
| Age of marriage (n = 73) | |
| Mean (sd) | 16.4 ( ± 4.8) |
| Median (iqr) | 16 (14–19) |
| Range | 6–32 |
| Age at onset of symptoms (n = 64) | |
| Mean (sd) | 35.3 ( ± 13.6) |
| Median (iqr) | 33.75 (25–42.5) |
| Range | 17–71 |
| Duration of symptoms (n = 64) | |
| Mean (sd) | 17.6 ( ± 16.5) |
| Median (iqr) | 11.5 (4–26) |
| Range | 0.2–60 |
| Parity (n = 74) | |
| Mean (sd) | 5 ( ± 2.7) |
| Median (iqr) | 4 (3–6) |
| Range | 1–13 |
| Parity at onset of symptoms (n = 52) | |
| Mean (sd) | 3.4 ( ± 2.4) |
| Median (iqr) | 2.5 (2–2.5) |
| Range | 1–10 |
n: total number; sd: standard deviation; iqr: interquartile range.
Figure 1.
Bar graph showing frequency of POP cases by residential Ward surrounding the Batakachaur and Hatiya birthing centres.
Although the mean age of women with POP was 53 years, 27.0% were under the age of 40 at presentation to the health post. Duration of symptoms ranged from 2 months to 60 years, with 73.4% of study participants suffering for over 5 years and 28.4% over 20 years. The majority of women noticed the symptoms of POP following the delivery of their last child (63.5%). However, a significant proportion (36.5%) continued to have children despite their symptoms.
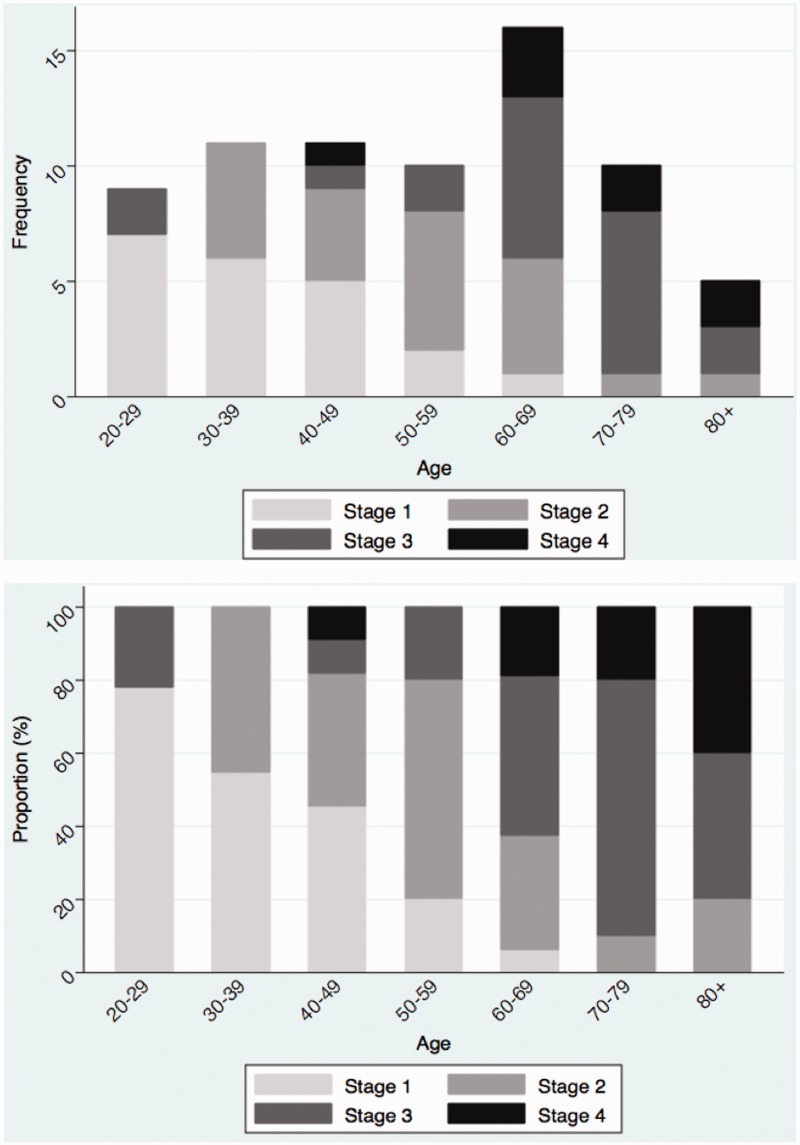
Age and duration of symptoms were positively associated with severity of POP (r = 0.6110 and r = 0.4529, respectively) (Figure 2).
Figure 2.
Bar graph showing the positive relationship between age and degree of POP by frequency (top) and proportion (bottom) (n = 72). Two patients were excluded as the stage of POP was unknown.
The age of marriage ranged widely from 6 to 32 years with 78.0% married before the legal age of 18. No statistically significant differences were detected between Brahmin and Chhetri castes and other castes.
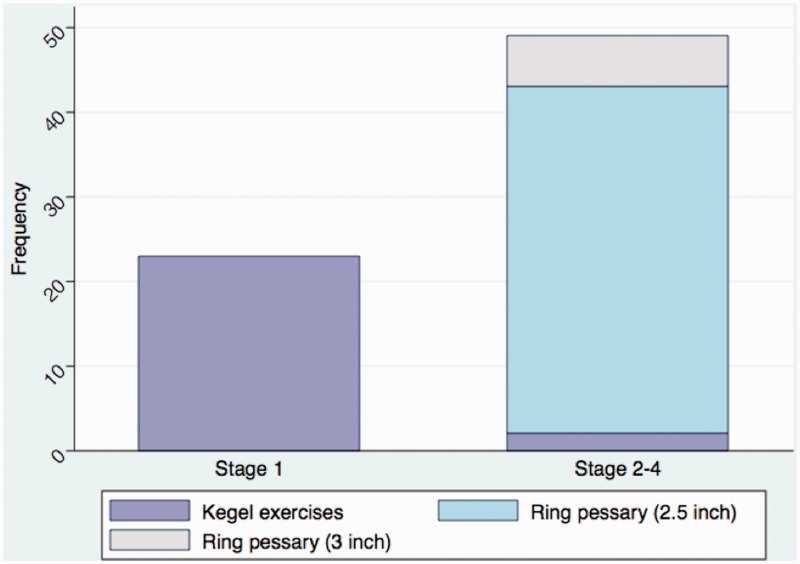
The distribution of the severity of POP was as follows: stage 1 (28.4%), stage 2 (29.7%), stage 3 (28.4%), and stage 4 (10.8%). The stage was unknown in two women. Figure 3 shows the prescribed primary management, Kegel exercises or ring pessary, regardless of stage. POP was associated with cystocele in 48.4%, rectocele in 23.0%, and a vault prolapse in 2.7% of women.
Figure 3.
Bar graph showing primary management according to degree of POP (n = 72). Kegel exercises (n = 25); Ring pessary 2.5-inch (n = 41); Ring pessary 3-inch (n = 6). Two patients were excluded as the stage of POP was unknown.
As shown in Figure 3, ring pessaries were offered to women with stages 2–4 POP (63.5%), with 87.2% of women receiving the 2.5-inch pessary. One woman (1.4%) refused intervention following diagnosis and counselling, and one woman (1.4%) was being treated for a decubitus ulcer prior to the insertion of a ring pessary at a later date.
Complications following intervention were reported in nine women with ring pessaries (19.1%). Pessary extrusion was the leading complication comprising four out of nine cases. Larger pessaries were available for women receiving the 2.5-inch pessary. Pain was reported in two patients (4.3%), discharge in two patients (4.3%) and urinary symptoms in one patient (2.1%). Staff at the health post managed all cases: antibiotics were prescribed to one patient, the pessary was reinserted in four patients (8.5%), and the pessary was removed in four patients (8.5%).
Univariate analysis
The results of a univariate analysis of risk factors by severity of POP are presented in Table 2. Women married under the age of 20, those over the age of 55 years at screening, over the age of 40 years at start of symptoms, suffering from POP for over 5 years, and those with a rectocele were at high risk of developing severe disease (stages 3–4 POP). Multivariate analysis could not be performed due to the small sample size.
Table 2.
Effect of potential risk factors and univariate odds ratio of relations between risk factors and severity of POP (stages 1–2 vs. stages 3–4).
| Variables | Degree of POP |
|||||
|---|---|---|---|---|---|---|
| Stage 1–2 | Stage 3–4 | Chi-squared | Univariate analysis |
|||
| n (%) | n (%) | p | OR | 95% CI | p | |
| Caste | ||||||
| Brahmin or chhetri | 30 (41.7) | 25 (34.7) | 0.090 | 2.71 | 0.78–9.36 | 0.115 |
| Other | 13 (18.1) | 4 (5.6) | 1 | |||
| Age of marriage | ||||||
| <20 years | 29 (40.8) | 26 (36.6) | 0.037 | 3.76 | 0.96–14.64 | 0.057 |
| ≥20 years | 13 (18.3) | 3 (4.2) | 1 | |||
| Age at screening | ||||||
| ≥55 years | 12 (16.7) | 23 (31.9) | 0.000 | 9.90 | 3.24–30.31 | 0.000 |
| <55 years | 31 (43.1) | 6 (8.3) | 1 | |||
| Age at onset of symptoms | ||||||
| ≥40 years | 6 (9.4) | 14 (21.9) | 0.004 | 5.00 | 1.59–15.75 | 0.006 |
| <40 years | 30 (46.9) | 14 (21.9) | 1 | |||
| Duration of symptoms | ||||||
| ≥5 years | 22 (34.4) | 25 (39.1) | 0.011 | 5.30 | 1.34–20.92 | 0.017 |
| <5 years | 14 (21.9) | 3 (4.7) | 1 | |||
| Parity at screening | ||||||
| 4 + | 27 (37.5) | 21 (29.2) | 0.278 | 1.56 | 0.56–4.32 | 0.397 |
| 1–3 | 16 (22.2) | 8 (11.1) | 1 | |||
| Parity at onset of symptoms | ||||||
| Last child | 20 (40.0) | 12 (24.0) | 0.579 | 0.94 | 0.29–3.09 | 0.923 |
| First-penultimate child | 11 (22.0) | 7 (14.0) | 1 | |||
| Birthing centre | ||||||
| Hatiya | 21 (29.2) | 15 (20.8) | 0.500 | 1.12 | 0.4–42.88 | 0.810 |
| Batakachaur | 22 (30.6) | 14 (19.4) | 1 | |||
| Cystocele | ||||||
| Yes | 24 (34.8) | 12 (17.4) | 0.099 | 0.47 | 0.18–1.24 | 0.129 |
| No | 16 (23.2) | 17 (24.6) | 1 | |||
| Rectocele | ||||||
| Yes | 6 (8.7) | 11 (15.9) | 0.029 | 3.46 | 1.10–10.91 | 0.034 |
| No | 34 (49.3) | 18 (26.1) | 1 | |||
n: total number; %: proportion of total; p: p value; OR: odds ratio; 95% CI: 95% confidence intervals. p < 0.05 considered statistically significant.
Conclusions
The present study highlights the opportunity to provide effective and safe non-surgical interventions to address the burden of POP in rural Nepal. As the women screened in this programme may represent the tip of the iceberg, further outreach and expansion of the screening programme is warranted.
The severity of the disease in rural communities is extremely concerning. Stages 2, 3 or 4 POP were diagnosed in 70.8% of women at screening. The long duration of symptoms, ageing of the women, and the young age of marriage in this region mean that the status quo is unlikely to change without appropriate interventions.
Age is a known risk factor for POP and the data in this screening programme support the Nepali and international literature.3,7 However, our study demonstrates that POP is not limited to the elderly population. A significant proportion of cases at screening were in young women (27.0% under the age of 40 years) and 70.0% of POP symptoms started in women under the age of 40 years (range 17–71 years). In addition, the duration of symptoms is a critical consideration in this population of women. On average, women waited 17.6 years (sd ± 16.5) with symptoms before accessing the screening programme (range 0.2–60 years). These findings highlight that POP is a major health burden among women of reproductive age in rural Nepal.
A significant proportion of women (63.5%) developed symptoms after the birth of their last child. Although there is a peak after the third child among these women, the range of parity remains wide (range 1–10 children). Repeated pregnancy was reported in this study and in the published literature.30 However, our findings suggest that the new onset of POP symptoms may lead to a decrease in future reproduction (either due to biological or psychosocial factors).
Our findings show the population differences in access to the screening programme. There is a clear trend showing greater utilisation of the programme among women who are geographically closer to the rural health post (Figure 1). It is essential for the screening programme to be as accessible as possible to all members of the community.
In total, nine complications were documented (six in Batakachaur, three in Hatiya). Although the complications are generally minor, the documentation of complications highlights the need for the availability of follow up at the local health care facility. The sub-health post managed all complications successfully and none required referral to a secondary health facility.
Surgery is an essential component for the continuum of care for women with POP. A recent study demonstrated an improvement in the quality of life among 166 women with POP after surgical intervention in a temporary facility in Nepal.31 However, these studies should be interpreted with caution. Data is scarce but post-operative complications and loss to follow-up are considered extremely high in women undergoing surgery in temporary health camps.31–34 Published evidence suggests complications, such as post-operative haemorrhage, infection, wound dehiscence and vault prolapse, can be as high as 43.5%.18 Women may also require further revision surgeries at a later date, which is currently difficult to provide in this setting.
The evaluation of the OHW-KS POP screening programme highlights the critical need to review the role of non-surgical interventions in Nepal, with a particular focus on the rural districts. Kegel exercises can play an essential role in asymptomatic, low stage POP, whereas ring pessaries can play an important role in more severe POP for women who prefer not to have surgery, due to high cost, travel barriers and difficulty leaving work in the community. In this screening programme, only 1 woman refused a ring pessary following diagnosis and counselling, because she was awaiting surgical intervention. All the women with stage 2 POP or greater preferred having the option of a ring pessary versus surgery.
Local cultural factors also shape health-related beliefs, behaviours, and values.34 In Nepal, many women require the permission from a family member, such as their husband or mother-in-law, to seek health care.35 Typically, women are responsible for heavy manual labour and return to work soon after a vaginal delivery, contributing to the development of POP.
We identify several limitations to this study. Firstly, this paper provides an overview and evaluation of a new public health programme in rural Nepal. The effectiveness of ring pessaries on symptomatology or quality of life is yet to be assessed in this setting, and a firm recommendation for adoption of ring pessaries cannot be made. However, the study provides first stage experience of the feasibility of rolling out non-surgical interventions in a geographically and socioeconomically challenging setting. Further limitations include the short duration of the follow-up period for the purposes of this evaluation. This paper is part of an ongoing programme collecting further data on an annual basis. Finally, the sample size is relatively small and due to geographical barriers there may be a selection bias for women further away from the health posts. Combining recruitment with FCHVs was adopted to reduce selection bias to a minimum, but it is likely to have remained considering the burden of POP in rural Nepal. The programme is currently expanding to provide greater access to care.
In summary, POP results in limitations to physical, psychological, and socioeconomic wellbeing.6,16,36 Recommendations by the screening programme implementation team and by members of the Batakachaur and Hatiya communities are presented in Table 3. We call for the delivery of freely available POP services in the community, the promotion of training in self-insertion and care of ring pessaries, and the integration of education of risk factors in the maternal and child health national programme. Non-surgical interventions will need to be assessed with a clear monitoring and evaluation strategy. We urge researchers to work closely with policy makers to design effective screening programmes and promote access to care in rural and marginalised communities.
Table 3.
Recommendations by the implementation team and community members.
| Recommendation | Responsible parties | |
|---|---|---|
| 1 | Outreach to disadvantaged, hard-to-reach and marginalised groups to access the POP programme | MoHP Local health facility |
| 2 | Community-wide promotion of POP awareness using innovative media, such as the local radio. | NGO partners Local health facility |
| 3 | Education initiatives should target both men and adolescent populations to promote a supportive environment for women with POP and address key risk factors. | MoHP/MoE NGO partners |
| 4 | Education initiatives should be integrated into the adolescent curriculum (school education and peer education) | MoHP/MoE NGO partners |
| 5 | Include silicone ring pessaries to the essential supply list for the local health facilities | MoHP Local health facility |
| 6 | Refocus policy from surgical management to preventive measures, such as Kegel’s exercise and ring pessaries | MoHP Donor organisations |
| 7 | Include POP in the Nepal Demographic Health Survey to quantify the burden of disease | MoHP |
| 8 | Regular monitoring and evaluation of the skills of the local health staff and FCHVs and data reporting systems | MoHP NGO partners |
| 9 | Health staff should maintain confidentiality in order to gain women’s trust and not deter them from seeking help | Local health facility Women with POP |
| 10 | Refresher training for health staff and FCHVs to build local capacity | MoHP NGO partners |
MoHP: ministry of health and population; MoE: ministry of education; NGO: nongovernmental organisation; FCHV: female community health volunteer.
Acknowledgements
We are grateful to the patients and community members of Batakachaur and Hatiya for their support, openness and hospitality. We are grateful to the local community health staff and the female community health volunteers for their clinical outreach work in a resource-limited setting. We thank our project partners, the Ministry of Health and Population and the Social Welfare Association of Nepal (SWAN), for their constructive collaboration. We are grateful to Karuna-Schechen for their generous financial support. Thank you to Professor Emeritus Louis G Keith and Nancy Sullivan for their insightful comments on earlier versions of the manuscript.
Declarations
Competing interests
None declared
Funding
We are grateful to Karuna-Schechen for their generous financial support of the POP programme. Thank you to Wellbeing of Women for supporting travel costs of JRF and EJAF.
Ethical approval
This programme was ethically approved by the Social Welfare Council under the activities of One Heart World-Wide in Nepal. The clinical protocol, interview questionnaire and training materials were reviewed and approved by the Family Health Division of the Ministry of Health and Population (MoHP).
Guarantor
SK
Contributorship
SB, SK and AS designed the programme. BSM, EJAF and JRF collated the data with assistance from the health post staff. JRF analysed the data, wrote up the results and created the graphs with input from TYS, EJAF and SB. SK supervised the data analysis and the drafting of the manuscript. JRF and SB contributed equally to this paper. All authors reviewed and approved the final version.
Provenance
Not commissioned; peer-reviewed by Ian Watt.
References
- 1.Gunasekera P, Sazaki J, Walker G. Pelvic organ prolapse: don’t forget developing countries. Lancet 2007; 369: 1789–1790. [DOI] [PubMed] [Google Scholar]
- 2.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990--2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012; 5380: 2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker GJA, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J 2011; 22: 127–135. [DOI] [PubMed] [Google Scholar]
- 4.UNFPA. Status of reproductive morbidities in Nepal, 2006. Kathmandu United Nations Popul Fund, www.advocacynet.org/modules/fck/upload/file/upa/Status of Reproductive Morbidities in Nepal.pdf (accessed 13 June 2013).
- 5.Gurung G, Rana A, Amatya A, Bista KD, Joshi AB, Sayami J. Pelvic organ prolapse in rural Nepalese women of reproductive age groups: what makes it so common? Nepal J Obstet Gynaecol 2008; 2: 35–41. [Google Scholar]
- 6.Fritel X, Varnoux N, Zins M, Breart G, Ringa V. Symptomatic pelvic organ prolapse at midlife, quality of life, and risk factors. Obstet Gynecol 2009; 113: 609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL. Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol 2007; 109: 1396–1403. [DOI] [PubMed] [Google Scholar]
- 8.Lien Y-S, Chen G-D, Ng S-C. Prevalence of and risk factors for pelvic organ prolapse and lower urinary tract symptoms among women in rural Nepal. Int J Gynaecol Obstet 2012; 119: 185–188. [DOI] [PubMed] [Google Scholar]
- 9.Gautam S, Adhikari RK, Dangol A. Associated factors for uterine prolapse. J Nepal Health Res Counc 2012; 10: 1–4. [PubMed] [Google Scholar]
- 10.Duong TH, Korn A. Predictors of advanced pelvic organ prolapse in Asian women. J Reprod Med 2009; 54: 488–492. [PubMed] [Google Scholar]
- 11.Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford family planning association study. Br J Obstet Gynaecol 1997; 104: 579–585. [DOI] [PubMed] [Google Scholar]
- 12.Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the women’s health initiative: gravity and gravidity. Am J Obstet Gynecol 2002; 186: 1160–1166. [DOI] [PubMed] [Google Scholar]
- 13.Swift S, Woodman P, O’Boyle A, et al. Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 2005; 192: 795–806. [DOI] [PubMed] [Google Scholar]
- 14.Bodner-Adler B, Shrivastava C, Bodner K. Risk factors for uterine prolapse in Nepal. Int Urogynecol J Pelvic Floor Dysfunct 2007; 18: 1343–1346. [DOI] [PubMed] [Google Scholar]
- 15.Barber MD. Symptoms and outcome measures of pelvic organ prolapse. Clin Obstet Gynecol 2005; 48: 648–661. [DOI] [PubMed] [Google Scholar]
- 16.Samuelsson EC, Victor FT, Tibblin G, Svärdsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 1999; 180: 299–305. [DOI] [PubMed] [Google Scholar]
- 17.Bonetti TR, Erpelding A, Pathak LR. Listening to “felt needs”: investigating genital prolapse in western Nepal. Reprod Health Matters 2004; 12: 166–175. [DOI] [PubMed] [Google Scholar]
- 18.Chhetry DB, Upreti SR, Dangal G, Subedi PK, Khanal MN. Impact evaluation of uterine prolapse surgery in nepalese women. J Nepal Health Res Counc 2012; 10: 167–171. [PubMed] [Google Scholar]
- 19.Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 2013; 4: CD004014–CD004014. [DOI] [PubMed] [Google Scholar]
- 20.Dangal G. A study of reproductive morbidity of women in the Eastern Terai region of Nepal. Nepal J Obstet Gynaecol 2008; 3: 29–34. [Google Scholar]
- 21.Jha R, Pant AD, Jha A, Adhikari RC, Sayami G. Histopathological analysis of hysterectomy specimens. J Nepal Med Assoc 2006; 45: 283–290. [PubMed] [Google Scholar]
- 22.Shrestha NS, Saha R, Karki C. Changing routes of hysterectomy: a cross sectional and comparative study. Nepal Med Coll J 2010; 12: 176–179. [PubMed] [Google Scholar]
- 23.Bø K. Pelvic floor muscle training in treatment of female stress urinary incontinence, pelvic organ prolapse and sexual dysfunction. World J Urol 2012; 30: 437–443. [DOI] [PubMed] [Google Scholar]
- 24.Bugge C, Adams EJ, Gopinath D, Reid F. Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev 2013; 2: CD004010–CD004010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fitz FF, Costa TF, Yamamoto DM, et al. Impact of pelvic floor muscle training on the quality of life in women with urinary incontinence. Rev Assoc Med Bras 2012; 58: 155–159. [PubMed] [Google Scholar]
- 26.Culligan PJ. Nonsurgical management of pelvic organ prolapse. Obstet Gynecol 2012; 119: 852–860. [DOI] [PubMed] [Google Scholar]
- 27.Lamers BHC, Broekman BMW, Milani AL. Pessary treatment for pelvic organ prolapse and health-related quality of life: a review. Int Urogynecol J 2011; 22: 637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manchana T. Ring pessary for all pelvic organ prolapse. Arch Gynecol Obstet 2011; 284: 391–395. [DOI] [PubMed] [Google Scholar]
- 29.Radl CM, Rajwar R, Aro AR. Uterine prolapse prevention in Eastern Nepal: the perspectives of women and health care professionals. Int J Womens Health 2012; 4: 373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pantha S. Repeated pregnancy in a woman with uterine prolapse from a rural area in Nepal. Reprod Health Matters 2011; 19: 129–132. [DOI] [PubMed] [Google Scholar]
- 31.Dhital R, Otsuka K, Poudel KC, Yasuoka J, Dangal G, Jimba M. Improved quality of life after surgery for pelvic organ prolapse in Nepalese women. BMC Womens Health 2013; 13: 22–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schaaf JM, Dongol A, van der Leeuw-Harmsen L. Follow-up of prolapse surgery in rural Nepal. Int Urogynecol J Pelvic Floor Dysfunct 2008; 19: 851–855. [DOI] [PubMed] [Google Scholar]
- 33.Rana A. Reducing morbidity from uterovaginal prolapse in Nepalese women through surgical camps: an ambitious approach. Nepal J Obstet Gynaecol 2009; 1: 1–3. [Google Scholar]
- 34.Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med 2006; 3: e294–e294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shrestha AD. Prevalence of uterine prolapse amongst gynecology OPD patients in Tribhuvan University Teaching Hospital in Nepal and its socio-cultural determinants. Kuala Lumpur, Malaysia Asian-pacific resour. Res Cent Women, http://arrow.org.my/publications/ICPD+15Country&ThematicCaseStudies/Nepal.pdf (2009, accessed 1 October 2015).
- 36.Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol 2006; 194: 1455–1461. [DOI] [PubMed] [Google Scholar]