Abstract
Oncolytic adenovirus (Ad) vectors present a promising modality to treat cancer. Many clinical trials have been done with either naked oncolytic Ad or combination with chemotherapies. However, the systemic injection of oncolytic Ad in clinical applications is restricted due to significant liver toxicity and immunogenicity. To overcome these issues, Ad has been engineered physically or chemically with numerous polymers for shielding the Ad surface, accomplishing extended blood circulation time and reduced immunogenicity as well as hepatotoxicity. In this review, we describe and classify the characteristics of polymer modified oncolytic Ad following each strategy for cancer treatment. Furthermore, this review concludes with the highlights of various polymer-coated Ads and their prospects, and directions for future research.
Keywords: Oncolytic adenovirus, Clinical trials, Cancer gene therapy, Oncolytic Ad/polymer hybrid vector, Active targeting, Tumor microenvironment targeting, Systemic administration
1. Introduction
Cancer is responsible for about 25% of all deaths in the US, the second most common cause of death in the US, exceeded only by heart disease, and is a major public health problem in many parts of the world. Cancer is one of the most serious diseases and increasing at an alarming rate [1]. Invasive surgical operation and chemotherapy have been used to treat the cancer in the clinic. In spite of the advance in conventional cancer treatment, the overall survival rate of cancer patients is significantly low with unwanted adverse side effects. Thus new strategies are needed to provide better treatment for cancer. Moreover, the Agency for Healthcare research and Quality estimates that the direct medical costs (total of all health care costs) for cancer in the US in 2013 were $91 billion. As a result of these converging influences, we are at a crucial juncture where novel and advanced therapeutic approaches against cancer are solely needed.
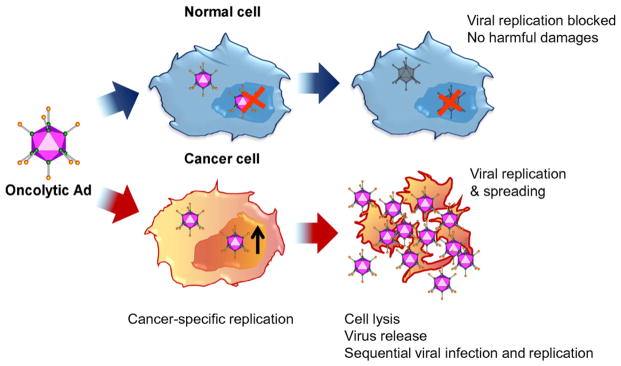
Adenoidal-pharyngeal-conjunctival virus, now named as an adenovirus (Ad) was first discovered by Wallace Rowe and his colleagues in 1953. Following cytopathogenic effects of Ad in tissue culture, the Ad was used in a clinical trial for the treatment of cervical cancer in 1956. After the first clinical gene therapy in 1989, the number of gene therapy clinical trials using an Ad vector worldwide has reached 496 in 2015 —ranking the first place (22.5% of all cases including viral & non-viral vectors) (http://www.wiley.co.uk/genmed/clinical/). Ad vector itself has many outstanding advantages, like an efficient nuclear entry mechanism and high gene transduction efficiency. However, the efficacy and duration of transgene expression with replication-incompetent Ad are limited. Here, cancer-specific replicating Ad (oncolytic Ad) is emerging as a promising new modality for cancer treatment. Oncolytic Ad has the improved efficacy over replication-incompetent Ad and the enhanced expression of therapeutic gene with diminished potential side effects caused by undesired expression of therapeutic gene in normal tissue (Fig. 1).
Fig. 1.
Schematic diagram of the cancer cell-specific killing of oncolytic adenovirus (Ad). Oncolytic Ad can replicate and destroy cancer cells by cancer-specific oncolysis while sparing normal cells.
During two decades, the oncolytic virus has been evolved to generate advanced therapeutic efficacy (Table 1). Most clinical and preclinical studies have focused on oncolytic virus modifications, providing improvements on tumor transduction, tumor targeting, cancer-specific replication, intratumoral dissemination, and modulation of antiviral and antitumor immune responses as well as arming with transgenes [2]. Especially, armed oncolytic virus and hybrid engineering of oncolytic virus promise an emerging approach in cancer treatment. The virotherapy using oncolytic Ad has been widely used in clinical applications due to the high titers that can be achieved, ability to insert larger size of therapeutic genes, and high transduction efficiency in dividing and non-dividing cells. Importantly, when oncolytic Ad replicates, they do not integrate their genome into host, therefore oncolytic Ad does not induce mutagenesis related with oncogene. These unique features give oncolytic Ad potency as gene carrier and increase safety than other oncolytic viruses such as oncolytic retro-, lenti-, and adeno-associated virus [3,4].
Table 1.
Advances in oncolytic virotherapy.
| Conventional genetic engineering | |
| Transduction | |
| Modification of surface proteins with tumor specific markers | [5] |
| Modification of viral envelope proteins | [6] |
| Transcription; tumor-specific promoter/enhancer | [7–10] |
| Engineering of Armed OV | |
| Integration with sequences coding for enzyme, protein, short-hairpin | [11] |
| RNAs tumor suppressor or suicide genes | [12,13] |
| Co-stimulatory molecule; CD ligand | [14] |
| ECM-degrading genes | [15–18] |
| Immunostimulatory cytokines; interleukin, GM-CSF | [19–21] |
| Inhibitor of angiogenesis | [22,23] |
| Increase susceptibility of infected cells to chemo and radiotherapy | [24] |
| miRNA, siRNA | [25,26] |
| Hybrid engineering | |
| Tumor-associated antigen (Oncolytic vaccine) | [27,28] |
| Cell vehicle | |
| Tumor-infiltrating cells; macrophages, myeloid-derived suppressor cells | [29,30] |
| MSC | [31,32] |
| Cytokine gene modified cell | [33] |
| T cell based | [34] |
| Co-administration of chemotherapeutics | [35–38] |
ECM; Extracellular matrix, GM-CSF; Granulocyte macrophage colony-stimulating factor, MSC; Mesenchymal stem cell.
For the therapy in cancer patients, no oncolytic virus is currently licensed by the US Food and Drug Administration and the European Medicines Agency yet (http://www.fda.gov/Drugs, http://ema.europa.eu). In the preclinical and clinical level, Ad is the most extensively investigated oncolytic virus [39–41]. Especially, the Chinese State Food and Drug Administration approved a recombinant Ad encoding human tumor suppressor gene p53 (rAd-p53, Gendicine) in 2003 and a recombinant oncolytic Ad (H101, Oncorine®) for combination treatment with chemotherapy in refractory head and neck cancer patients.
Here, we summarized the recent clinical trials of oncolytic Ad therapy (Table 2). Most phase I clinical trials of oncolytic Ad demonstrated mild, manageable, and transient vector-related toxicities, which is crucial factor for moving on to next phase clinical trials. Moreover, advanced clinical trials of oncolytic Ad have proved clinical responses in tumors that are resistant to chemotherapy or radiotherapy and have distant metastasis [42]. Early clinical trial of oncolytic Ad was evaluated with the administration of oncolytic Ad-alone. In localized prostate cancer phase I clinical trials, CG7870, expressing E1A under control of the rat probasin promoter and E1B under control of the prostate-specific antigen (PSA) promoter–enhancer, and the E3 region genes observed no partial or complete PSA responses [43,44]. Also the intravesical instillation of CG0070 is being studied as a standalone therapy in bladder cancer patients who failed BCG-based immunotherapy [45]. Recently, combined oncolytic Ad and chemotherapy could convey stronger anti-tumor effects by providing synergistic mode of actions by oncolysis and chemotherapeutic mechanism, potentially attenuating cancer cell resistance to virotherapy or chemotherapy [37,38]. GM-CSF coding capsid chimeric Ad, CGTG-102 moves on to the phase I for advanced solid tumors, alone or in combination with cyclophosphamide chemotherapy [40,46]. In a phase III clinical trial, Ad5/3-D24-GMCSF showed efficacy in melanoma patients refractory to other forms of therapy [47]. Ad-OC-TK/VAL is the first in vivo Ad gene therapy used to treat bone metastasis in prostate cancer patients, suggesting potential benefit of combined treatment with docetaxel-based chemotherapy for hormone-refractory metastatic prostate cancer [48,49]. About 50% of all human cancers and over 90% of patients with small cell lung cancer have altered p53 tumor suppressor gene function. Also, dendritic cells are the most potent antigen presenting cells, then most effective in inducing a primary anti-p53 cytotoxic T lymphocytes response. 78.6% of Ad.p53-DC (INGN-225) patients showed positive immune response, followed by better clinical response to second-line chemotherapy and a trend towards improved survival [50]. Ad with 2 cytotoxic gene systems of cytosine deaminase (CD)/5-fluorocytosine (5-FC) and herpes simplex virus thymidine kinase (HSV-1 TK)/valganciclovir (vGCV) has treated the prostate cancer patients, which makes malignant cells sensitive to specific pharmacological agents (cytotoxic gene therapy) and improves the effectiveness of radiation therapy by radiosensitization [51]. This multimodal biological approach to improve the effectiveness of radiation therapy reported a clinically meaningful reduction in positive biopsy results at 2 years in men with intermediate-risk prostate cancer [51]. DNX-2401 (Ad-Δ24) and ICOVIR® (Ad-Δ24-RGD), engineered to replicate only in cells with altered retinoblastoma 1 signaling pathway are being studied in patients with advanced melanoma or other solid tumors as a standalone therapy as well as in patients with recurrent glioblastoma, combined with interferon Gamma or Temozolomide [19,45,52]. VCN-01, Ad expressing human sperm adhesion molecule 1 (SPAM1, PH20 hyaluronidase) is being tested in patients with advanced pancreatic cancer or other solid tumors [45]. See Tables 3 and 4.
Table 2.
Clinical trials of oncolytic Ad.
| Cancer | Phase | Ad type | Genetic change | Route | Combination therapy | Response | Ref. |
|---|---|---|---|---|---|---|---|
| Advanced Pancreatic cancer | I | Ad-SPAM1 (VCN-01) | Expressing SPAM1 | IT | Gemcitabine | [45] | |
| Solid tumors | I | IV | Gemcitabine | ||||
| Recurrent GBM | I | Ad-Δ24 (DNX-2401) | Replication only in cells with alterations of the RB1 signaling pathway | CED | Temozolomide ± surgery | [19,45,52] | |
| Recurrent Glioblastoma/Gliosarcoma | I/II | Ad-Δ24-RGD (ICOVIR®) | IT | IFN-γ | |||
| Glioblastoma at first recurrence | I | Ad-Δ24-RGD (ICOVIR®) | IT | Temozolomide | |||
| Advanced Melanoma | I | ICOVIR-5 | IV | – | |||
| Solid tumors | I/II | ICOVIR-5 | IP (via MSC) | – | |||
| Advanced solid tumors | I | Ad5/3-D24-GMCSF (CGTG-102) | Drive the local expression of GM-CSF | IT, IV | cyclophosphamide | [40,46] | |
| I | IT | – | |||||
| Chemotherapy-refractory Melanoma | III | Ad5/3-D24-GMCSF | Armed with GM-CSF coding | – | SD, MR, PD | [47] | |
| Intermediate-risk Prostate cancer | II/III | Ad5-yCD/mutTKSR39rep-ADP | 2 cytotoxic gene systems; CD/5-FC and HSV-1 TK/vGCV | IT | Intensity modulated RTx | Reduction in positive biopsy results at 2 yrs | [51,53–55] |
| Recurrent Ovarian cancer | I | Ad5/3-Δ24 | Selective replication within RB-p16-deficient tumor cells | IP | SD, PD | [56] | |
| Small cell Lung cancer | I/II | Ad.p53-DC (INGN-225) | p53-modified Ad-transduced dendritic cell vaccine | – | [50] | ||
| Refractory Head & Neck cancer | III | Ad5CMV-p53 (INGN-201), Advexin® | Ad-mediated p53 gene therapy | IT | ±CTx ±RTx |
†survival, delayed progression | [57,58] |
| Hormone-refractory metastatic Prostate cancer | I/II | Ad5-OC/TK plus VAL | Osteocalcin promoter-driven HSV thymidine kinase gene | IT | Docetaxel, estramustine | [48,49] | |
| Bladder cancer-failed BCG-based immunotherapy | II, III | Ad-GMCSF (CG0070) | Armed with GM-CSF Preferential replication in RB-deficient tumors |
IV | – | [40,45,59] | |
| Locally recurrent Prostate cancer | I | CG7060 (CV706) | Ad with PSA promoter–enhancer element to control E1A expression | IT | RTx | PR; PSA control | [5,43,60] |
| Metastatic, hormone-refractory Prostate cancer | I | CG7870 (CV787) | Rat probasin-E1A hPSA-E1B E3+ |
IV | – | No PR, CR | [5,43,44,61] |
| Recurrent Head & Neck cancer | Approved (China) | ONYX-015, Oncorine® (H101) | E1B-55 kDa gene deleted, target p53 deficient cancer cells | IT | Cisplatin, 5-FU | [59,62–64] | |
| Hepatobiliary tumor | II | ONYX-015 | Ad5/2, E1B-55 kDa gene deleted | IT | – | [65] | |
| Metastatic colorectal cancer | I/II | IV | – | SD, PR | [61] | ||
| Liver metastasis | I, II | IV | – | [61] |
BCG; Bacillus Calmette–Guérin, CED; convection enhanced delivery, CTx; chemotherapy, DC; dendritic cell, 5-FU; 5-fluorouracil, GBM; glioblastoma multiforme, GM-CSF; granulocyte-macrophage colony-stimulating factor, IP; intraperitoneal, IPleu; intrapleural, IT; intratumoral injection, IV; intravenous, IVe; intravesicular, MSC; mesenchymal stem cell, MR; minimal response, PD; progressive disease, PR; partial response, RB; retinoblastoma signaling pathway, RTx; radiation therapy, SD; stable disease.
Table 3.
Summary of oncolytic Ad/polymers which were complexed by chemical conjugation and electrostatic interaction.
| Methods | Polymer | Oncolytic adenovirus | Efficacy | Application | Ref. |
|---|---|---|---|---|---|
| Chemical conjugation | PEG | Ad-GL |
|
In vitro and in vivo | [82] |
| ABP | YKL-1001 |
|
In vitro and in vivo | [76] | |
| Electrostatic interaction | Reducible PEI | RdB/shMet |
|
In vitro | [91] |
| Bile acid conjugated PEI | KOX |
|
In vitro and in vivo | [92] | |
| PAMAM | E1/AFP-E3/NIS |
|
In vitro and in vivo | [96] | |
| PNLG | ΔB7-U6ShIL8 |
|
In vitro and in vivo | [97] | |
| PPSA | DWP418 |
|
In vitro and in vivo | [98] |
Table 4.
Summary of oncolytic Ad/polymers which were used for active tumor targeting.
| Polymers | Targeting ligand | Oncolytic adenovirus | Efficacy | Targeted cell | Ref. |
|---|---|---|---|---|---|
| CD-PEG-cRGD | cRGD | ΔB7-U6ShIL8 |
|
αβ integrin positive cancer | [110] |
| PEG-HER | Herceptin | DWP418 |
|
Her2/neu overexpressed cancer | [114] |
| chitosan–PEG–FA | Folic acid | HmT |
|
Folate receptor overexpressed cancer | [116] |
| PAMAM-GE11 | GE11 | E1/AFP-RSV/NIS |
|
EGFR positive cancer | [120] |
In recent clinical trials, combined oncolytic Ad and chemotherapy could convey stronger anti-tumor effects by providing synergistic effects by oncolysis and chemotherapeutic mechanism, potentially attenuating cancer cell resistance to virotherapy or chemotherapy [37, 38]. Deeper understanding of complex interactions and molecular mechanisms between the oncolytic Ad, adjuvant chemotherapy or radiation therapy, and tumor must be followed the pros and cons of cancer therapeutics. Also, the consideration for delivery route and delivery method of simultaneous, consequent, or repeated administration with conventional therapy must be taken.
Most of human clinical trials of oncolytic Ad have been limited to local treatment of head and neck cancer, glioblastoma, and melanoma (Table 2). However, systemic administration of oncolytic Ad is required for efficacious treatment of both primary and metastatic cancer. Systemic delivery of oncolytic Ad still needs to overcome three major hurdles that limit its clinical application. First, Ad induces strong innate immune response by interacting with macrophages and dendritic cells which results in production of proinflammatory cytokines and chemokines such as interleukin-6 (IL-6), tumor necrosis factor-α, and interferon γ inducible protein-10 [66–68]. Second, adaptive immune response induced by pre-existing anti-Ad neutralizing antibody (Ab) in the host [69,70]. To this end, individuals who previously have been exposed to Ad produces neutralizing anti-Ad Abs, resulting in rapid clearance of oncolytic Ad which limits Ad’s therapeutic efficacy. Third, nonspecific liver sequestration of systemically administered oncolytic Ad leads to hepatotoxicity [71,72]. These hurdles are caused by nonspecific interaction of oncolytic Ad’s capsid protein, such as hexon, penton base, and fiber, with the host environment. Thus, polymers and other nanomaterials can be used to mask the Ad capsid which can reduce anti-viral immune response, nonspecific liver trafficking, and increase the tumor accumulation of Ad. This review will focus on recent advancements in oncolytic Ad/polymer platform that address some of the critical challenges faced by oncolytic Ad as well as enhancement in therapeutic efficacy and safety of hybrid vector system.
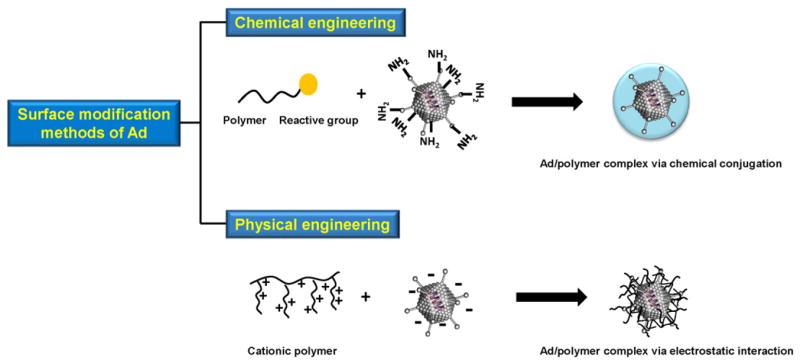
2. Oncolytic Ad complexed with polymers via chemical conjugation
The major purpose of the Ad complexed with polymer is to increase transgene expression, provide protection from the host antiviral immune system, and target the tumor tissues. There are two strategies for surface modification of oncolytic Ad with polymers; chemical conjugation and physical engineering through electrostatic interaction (Fig. 2). These two strategies facilitate evasion of anti-viral immune responses as well as cancer-specific accumulation of Ad [73].
Fig. 2.
Overview of strategies used for surface modification of Ad. The free amines on the viral surface can be easily reacted with functional polymers (top). Ad coated with a cationic polymer effectively interacts with the negatively charged Ad surface (bottom).
Covalent chemical conjugation of polymer to Ad surface can occur through either cross-linker or direct conjugation [74–76]. There are approximately 1800 free amines on the viral surface (hexon, penton, and fiber protein) and they can be reacted with polymers. Direct conjugation modifies several hundred amino acids located on the capsid through single step and can be accomplished more easily than genetic engineering of Ad capsid. Moreover, chemically conjugated oncolytic Ad has high serum stability, enhanced blood circulation time, and ultimately reduced unwanted interactions with blood components, resulting in increased tumor accumulation through enhanced permeability and retention (EPR) effect. In the following sections, various polymer-conjugated Ad complexes will be discussed.
2.1. PEGylation of oncolytic Ad
Initially, poly(ethylene) glycol (PEG) was first chemical to be extensively researched to generate ‘stealth Ad’ system [74]. PEG is a linear synthetic polymer composed of repetitive CH2CH2O subunits. It is a hydrophilic molecule that has neutral charge, non-immunogenic property, and negligible cytotoxicity. PEG has been widely researched as a delivery vehicle for therapeutic peptides and proteins in biomedical applications [77–79]. The covalent conjugation of PEG with proteins or peptides significantly reduces immunogenicity and antigenicity, and increases solubility while maintaining bioactivity as well as serum stability in vivo [80]. PEGylation of Ad prolongs blood circulation and minimizes non-specific uptakes by macrophages and hepatocytes, resulting in increased tumor-specific accumulation and safety [75,81].
Doronin et al. examined the hepatotoxicity and therapeutic efficacy of PEGylated oncolytic Ad using 5-kDa and 20-kDa PEG [82]. Cancer cell killing efficacy of PEGlyated oncolytic Ad increases with increasing molecular weight of the PEG. Only 20-kDa PEG conjugated oncolytic Ad markedly reduced hepatocyte transduction and hepatotoxicity than naked oncolytic Ad after systemic injection. In detail, biodistribution of Ad in prostatic and hepatocarcinoma xenograft tumor models demonstrated that PEGylation with 20-kDa PEG reduced liver uptake by 19- or 90-fold compared with naked oncolytic Ad or 5-kDa PEGylated Ad, respectively. 20-kDa PEGylated oncolytic Ad increased median survival of xenograft-bearing mice by 14 to 31 days in comparison to naked oncolytic Ad-treated mice likely due to passive tumor targeting through EPR effect. The higher molecular weight of 20-kDa PEG likely shields larger area of the Ad surface thereby preventing Ad’s interaction with Kupffer cells in the liver, resulting in decreased hepatotoxicity. These results indicate that conjugation of Ad with high molecular weight PEG can play a pivotal role in increasing anti-tumor efficacy and reducing the hepatotoxicity by efficiently masking Ad’s capsid, resulting in enhanced survival and therapeutic benefits.
2.2. Arginine-grafted bioreducible polymer (ABP)-conjugated Ad
Despite this evidence demonstrating enhanced safety and efficacy by PEGylated Ad, there are known limitations when compared with naked Ad. 1) The polymer monolayer of PEG is permanently linked to the viral vectors which can interfere between adenoviral fiber and cellular receptor, resulting in reduced transduction efficacy. 2) Neutral surface charge of the complex impedes internalization into negatively charge cellular membrane, resulting in decreased cellular uptake. To this end, enzymatically cleavable linkers and cationic polymers have been studied to overcome these obstacles. In this regard, Kim et al. generated Ad conjugated with positively charged arginine-grafted bioreducible polymer (ABP) [76]. Arginine, frequently used as a cell penetrating peptide, has been grafted onto bioreducible backbone, and it greatly improves the cellular transduction of Ad. Moreover, bioreducible backbone containing disulfide bridge easily degrades and releases the viral vector in the cytoplasm. Thus, conjugation with ABP can lead to higher transduction efficiency and lower cytotoxicity. Ad/ABP showed significantly higher transgene expression than naked Ad in both CAR-positive and -negative cells, implying Ad/ABP is internalized independently of Ad capsid and CAR. Hepatoma-specific oncolytic Ad (YKL-1001) conjugated with ABP enhanced Ad-mediated hepatoma cell killing than either naked YKL-1001 or YKL-1001-DTSSP, indicating that covalent conjugation of ABP does not affect the bioactivity of YKL-1001. ABP-conjugated YKL-1001 induced less innate and adoptive immune response, prolonged blood circulation time, decreased liver accumulation, and exhibited strong anti-tumor efficacy when systemically administered in comparison to naked YKL-1001. These results demonstrate that Ad/ABP is efficient hybrid hepatoma cancer-specific vector that can enhance accumulation in hepatoma via EPR-mediated tumor accumulation.
Polymer conjugated oncolytic Ad can be engineered easily and exhibits high serum stability, resulting in high therapeutic benefits due to reduced host anti-viral immune response and increased tumor accumulation.
3. Oncolytic Ad coating with polymer via electrostatic interaction
The backbone of cationic polymers contains positively charged amine groups. Cationic polymers and anionic surface of Ad can form Ad/polymer complex through electrostatic interaction. Ad/polymer complex with net cationic surface charge exhibits increased cellular uptake and transgene expression of Ad [83]. Additionally, these cationic polymers possess tertiary and secondary amines with high buffering capacity, which facilitate effectively escape from the endosomes and release the virus into the cytosol via the “proton sponge effect” [84]. This strategy has several benefits, such as the easy manipulation of molecular weight and bio-functional group for enhancing anti-cancer efficacy. It is easy and straightforward to generate the Ad/polymer complexes without chemical reaction. However, the main disadvantage of this technique is its non-specific uptake in cells due to the highly positive surface charge, resulting increase cytotoxicity. Ad/polymer complex can rapidly dissociate in the blood stream after intravenous injection due to the negatively charged serum protein, which has a strong interaction with the positively charged polymer. Certain serum proteins can be adsorbed on the Ad/polymer surface, triggering nonspecific interactions between polymer and the membrane receptors of macrophages and monocytes [85].
3.1. Recent engineered poly(ethyleneimine) (PEI)-coated Ad
This electrostatic complexation strategy facilitates conjugation of functional peptide or cholesterol. Furthermore, electrostatic interaction between Ad and polymer can occur in aqueous buffer without cross-linkers and additional preparation. Importantly, Ad/polymer complex maintains its viral activity and intracellular trafficking while transduction efficiency is enhanced through increased membrane binding affinity due to cationic charge of the complex. Among the various cationic polymers that have been developed, PEI (25 kDa) is used as the ‘gold standard’ due to its high transgene expression. However, its clinical application is limited by its systemic cytotoxicity and low serum stability. Therefore, non-toxic polymers (PEG) or cholesterol have been used to modify PEI [86–88] to reduce its toxicity. Alternatively, several bioreducible PEIs have been developed and researched [89,90]. Bioreducible PEI, which carries a disulfide moiety in the block copolymer, can degrade into monomers in the cytoplasm and release the viral vector. These fragments are easily excreted from the body, resulting in low systemic cytotoxicity. Choi et al. developed low molecular weight PEI multi cross-linked to bioreducible disulfide cystamine core (rPEI) [91]. Ad expressing short hairpin RNA against c-Met mRNA was complexed with rPEI (Ad/rPEI) showed higher transduction efficiency than Ad/25 kDa PEI in both CAR-positive and -negative cancer cells. Ad/rPEI exhibited higher cancer cell killing effect, viral production, and suppression of Met and VEGF level than naked Ad. Recently, Lee et al. demonstrated that Ad complexed with bile acid-conjugated PEI (DA3) increases transduction efficiency in both CAR-positive and -negative cancer cells than naked Ad [92]. The cellular uptake mechanism revealed that Ad/DA3 was not internalized through CAR-mediated endocytosis and it rather involved clathrin-, caveolae-, and macropinocytosis-mediated endocytosis. Moreover, VEGF inhibitory gene (KOX) expressing-oncolytic Ad complexed with DA3 (KOX/DA3) complex showed significantly improved therapeutic effects compared with naked KOX in HT1080 tumor xenograft model. The potent antitumor efficacy of the KOX/DA3 complex can be attributed to active replication and amplification of KOX which selectively decreased angiogenesis in the tumor tissues.
3.2. Polyamidoamine (PAMAM) dendrimer-coated Ad
Tomalia et al. first reported the synthesis and characterization of PAMAM dendrimers using ammonium or ethylene diamine as a core molecule [93]. Dendrimers are symmetric, highly branched, synthesized to high generation, and thus it has been investigated as an efficient non-viral carrier [94,95]. Gruanwald et al. examined sodium iodide symporter (NIS)-expressing oncolytic Ad coated with PAMAM G5, which demonstrated enhanced transduction efficacy in CAR-negative cells and protection against neutralizing Abs [96]. Biodistribution result using 123I scintigraphy demonstrated significantly reduced transgene expression and toxicity in the liver by systemically delivered dendrimer-coated Ad5-CMV/NIS whereas transgene expression was enhanced in tumor tissues. These results demonstrate efficient liver detargeting and enhanced tumor targeting by PAMAM-coated oncolytic Ad, which exploits the synergies between oncolytic virotherapy and NIS-mediated radiotherapy.
3.3. Biodegradable/reducible polymers-coated Ad
Recently, Kim et al. assessed therapeutic efficacy and safety of systemically administered biodegradable methoxy poly(ethylene glycol)-b-poly{N-[N-(2-aminoethyl)-2-aminoethyl]-L-glutamate} (PNLG) polymer-coated oncolytic Ad (Ad-ΔB7-U6shIL8) [97]. The PNLG-coated GFP-expressing Ad complex showed increased transgene expression in both high and low CAR-expressing cells than naked Ad, Ad/ABP, or Ad/bPEI. Furthermore, oncolytic Ad coated with PNLG (Ad/PNLG) demonstrated greater cancer killing effect in vitro than Ad, Ad/ABP, or Ad/PEI. Furthermore, enhanced tumor accumulation was observed by Ad/PNLG when compared with naked Ad and Ad/ABP, respectively. Tumor-to-liver ratio of Ad viral particles in Ad/PNLG-treated mice was 1229-fold higher than mice injected with naked Ad or Ad/ABP. Ad/PNLG showed markedly reduced innate and adoptive immune responses than cognate controls. These results indicate that the Ad complexed with biodegradable PNLG polymer increased transduction efficiency, cancer killing ability, and decreased both innate and adoptive immune responses in malignant tumor cells with low or ablated CAR expression.
More recently, Jung et al., demonstrated how oncolytic Ad (DWP418) complexed with cationic polymers containing arginine moieties capable of facilitating cell entry can transduce both CAR-positive and -negative cells [98]. The mPEG-PEI-g-Arg-S-S-Arg-g-PEI-mPEG (PPSA) contains both bioreducible disulfide bond and dual arginine functional moieties to reduce cytotoxicity and enhance transduction efficacy, respectively. The intratumoral delivery of DWP418/PPSA elicited more potent anti-tumor responses in CAR-negative MCF7 xenograft mice compared with naked DWP418 or DWP418/ABP. Innate immune response and production of Ad-specific neutralizing Abs were significantly reduced in the DWP418/PPSA-treated mice compared with DWP418-treated group. The immunohistochemical analysis demonstrated that viral replication and oncolytic Ad-induced apoptosis occurred preferentially in tumor tissues. Together, these results suggest that bioreducible and biodegradable polymer-coated Ads induce cancer cell-specific cytolysis by oncolytic Ad through systemic delivery treating disseminated tumors.
However, oncolytic Ad modified with cationic polymer has several limitations in clinical translation. Targeting cancer cells within the tumor tissues is not always feasible as some nanocomplex cannot diffuse efficiently and positive charged Ad/polymer complex can enter normal tissues or interact with RES, resulting in poor tumor targeting [99,100].
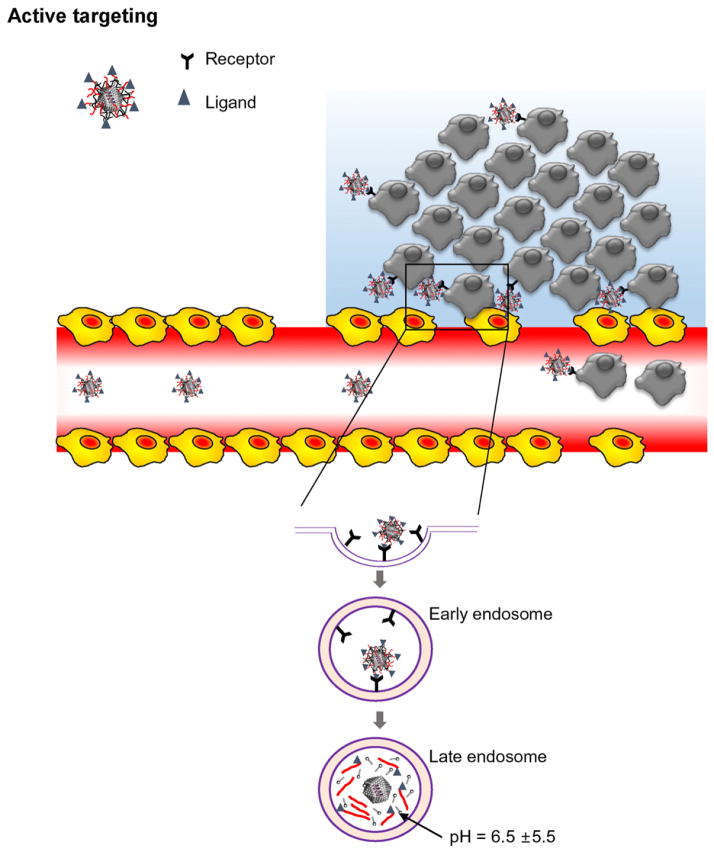
4. Tumor targeting by oncolytic Ad/polymer
One way to overcome the limitations of passive targeting is to introduce affinity ligands to the surface of a polymer, which can provide high binding affinity between the ligand-conjugated polymer and unique receptor overexpressed on the surface of cancer cell membrane (Fig. 3) [101,102]. The backbone of polymer conjugated with a specific tumor-homing moiety such as an antibody, antibody fragment, peptide, aptamer, or polysaccharide can considerably increase selectivity and efficiency of nanocomplex’s accumulation within targeted tumor cells [103–106]. In order to achieve high tumor specificity, targeted receptors should be highly expressed on tumor cells, but not on normal cells. Moreover, multiple factors, such as size and stability of nanoparticles as well as the density and affinity of the targeting moiety, are critical to development of efficient cancer targeting vector [107].
Fig. 3.
Active targeting of oncolytic Ad/polymers. Active targeting strategy. Ligands grafted at the surface of polymers, which complexed with oncolytic Ad, bind to receptors overexpressed cancer cells. After endocytosis, Ad/polymer enters into the endosome, then escape from endosome when pH value of endosome becomes acidic.
4.1. Oncolytic Ad complexed CD-PEG-cRGD
Bioreducible cyclic RGD conjugated poly(cystaminebisacrylamine-diaminohexane) [poly(CBA-DAH) (CD)] has been investigated as a polymeric carrier for tumor-targeted oncolytic Ad delivery [108]. CD has lower cytotoxicity than 25 kDa PEI due to disulfide bond which can be easily cleaved by glutathione into innocuous small molecules when exposed to the reductive environment in the cytoplasm. A cyclic RGD peptide is well known as an active targeting moiety for anti-angiogenic gene therapy in tumor [109]. This RGD ligand can recognize and bind with αvβ3 and αvβ5 integrin receptors, which are overexpressed in sprouting tumor vessels and most tumor cells, with high specificity. The oncolytic Ad complexed with cRGD-conjugated CD polymers showed enhanced tumor-specific transduction and greater cancer cell-killing efficacy in a dose-dependent manner when compared with naked oncolytic Ad. Furthermore, a competition assay using anti-CAR or anti-integrin Abs revealed that both CAR and integrin were required for naked Ad to infect and replicate in the cancer cells, but only integrin was needed for effective transduction by oncolytic Ad/CD-PEG-cRGD complex. Cancer cells treated with oncolytic Ad/CD-PEG-cRGD also showed high levels of apoptosis and necrosis as well as decreased IL-8 and VEGF level. Significant tumor-growth inhibition of the polymer-shielded Ad was observed in lung orthotopic tumor model [110]. The shielding effect of the Ad surface with the bioreducible CD-PEG-cRGD polymer allowed evasion of anti-viral immune responses and reduction of hepatotoxicity. Interestingly, CD-PEG2000 Da-cRGD, 2 kDa molecular weight of PEG introduced between CD and cRGD coated oncolytic Ad injected tumor bearing mice showed higher anti-tumor efficacy than CD-PEG500 Da-cRGD coated oncolytic Ad, implying that higher molecular weight of PEG could prong blood circulation and accumulation in the tumor tissues. Together, these results suggest that the infection pathway of CD-PEG-cRGD-complexed Ad is exclusively regulated by the interaction between integrins and tumor homing peptides, cRGD, and CD-PEG-cRGD could be utilized for efficient cancer therapy.
4.2. Her2/neu specific targeting with oncolytic Ad conjugation with Herceptin
Her2/neu is a human EGF 2 receptor that is known to be overexpressed in breast cancer patients [111]. Constitutive activation of Her2/neu led to oncogenesis in these cancers, and drugs that block Her2/neu signaling cascade, such as trastuzumab and lapatinib, are in clinical use [112,113]. Trastuzumab (Herceptin; HER), a Her2/neu-specific monoclonal antibody, is also widely used to treat both metasta-tic breast cancer in clinical settings. Kim et al. covalently conjugated PEG to oncolytic Ad (DWP418) using a bioreducible cross-linker, and subsequently conjugated the Herceptin antibody to the end terminals of PEG for Her2/neu-targeted cancer gene therapy [114]. Systemic injection of Ad-PEG-HER prolonged blood circulation time by 16-fold compared to the naked Ad. Her2/neu-overexpressed SKOV3 and MDA-MB435 xenograft tumor models treated with DWP418-PEG-HER elicited greater antitumor activity than that of naked DWP418 or DWP418-PEG. However, DWP418-PEG-HER-treated Her2/neu-negative MCF7-mot xenograft tumors had similar anti-tumor efficacy compared to DWP418-PEG. The tumor-to-liver ratio for DWP418-PEG-HER was 1010-fold greater than naked DWP418 in Her2/neu-positive tumors, demonstrating that Herceptin-conjugated PEG actively targeted the tumor tissues leading to enhanced intratumoral accumulation. Together, these results clearly demonstrate that the enhanced anti-tumor activity and tumor specific killing efficiency of DWP418-PEG-HER tumors depend upon retargeting of the Ad/polymer to the tumors through specific interaction between Herceptin and Her2/neu on the cell surface.
4.3. Folate receptor overexpressed cancer therapy with oncolytic Ad/chitosan PEG-FA
Folate receptor is widely overexpressed on the surface of cancer cells and has been targeted by folic acid (FA)-conjugated carriers [115]. Recently, GFP-expressing replication-incompetent Ad cross-linked with chitosan–PEG–FA complex was generated through a high capacity encapsulation process known as electrospinning [116,117]. The Ad/chitosan–PEG–FA successfully coated Ad without reducing its biological activity or infectivity. Moreover, the blood clearance assay results revealed 48.9-fold enhanced blood retention time for the oncolytic Ad/chitosan–PEG–FA compared to naked oncolytic Ad. Furthermore, immune response was markedly reduced due to PEGylation and tumor-to-liver ratio of Ad/chitosan–PEG–FA was significantly greater than naked Ad. Moreover, the oncolytic Ad/chitosan–PEG–FA elicited a more potent antitumor efficacy than the oncolytic Ad/chitosan–PEG. These results demonstrated that the efficacy of active tumor targeting is more effective than EPR-mediated passive tumor targeting system.
4.4. EGFR specific targeting with oncolytic Ad/PAMAM-GE11
Epidermal growth factor receptor (EGFR), a family of receptor tyro-sine kinase proteins, such as EGFR, HER2/erbB2, and HER3/erbB3, are overexpressed in various tumors of epithelial origin. EGFR is continually activated in cancer cells resulting in signal cascades that lead to cell growth, drug and radiation resistance, and ligand-independent activation [118]. Thus, anti-EGF Abs or EGFR targeted peptides have been used as an attractive targeting ligand for various diagnostic and therapeutic nanoparticles due to its high affinity binding to EGFR and subsequent cellular internalization by receptor-mediated endocytosis [119]. Grünwald et al. developed an EGFR targeting peptide, GE11-conjugated PAMAM dendrimer-coated oncolytic Ad complex for selective treatment of EGFR-overexpressing tumor cells [120]. 123I scintigraphy after intravenous injection of the dendrimer-coated oncolytic Ad revealed attenuated hepatic transgene expression. Moreover, significant and tumor-specific enhancement in anti-tumor efficacy was observed following systemic delivery of oncolytic Ad/PAMAM-GE11 that was further increased by additional treatment with a therapeutic dose of 131I. These results suggest that retargeting of Ad to specific cells can be achieved by conjugating a cell-specific targeting ligand to the polymer complexed with Ad.
In summary, these results demonstrate that oncolytic Ad complexed with various polymers that have a targeting moiety may overcome the obstacles of conventional oncolytic Ad vectors, such as hepatotoxicity, immunogenicity, and short blood circulation time, while enhancing intratumoral accumulation through active and passive targeting.
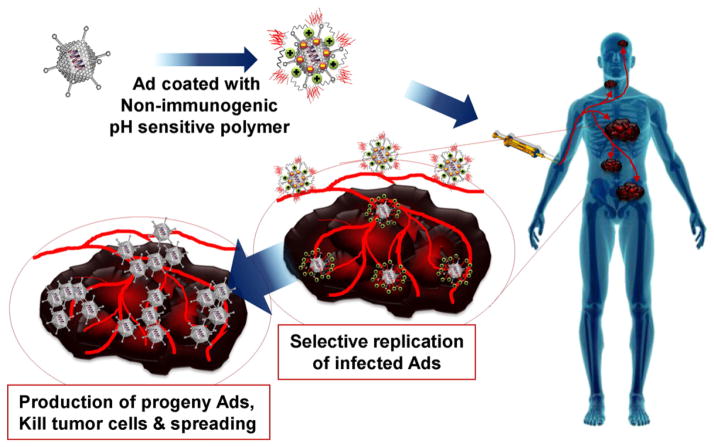
5. Tumor microenvironment targeting
To overcome lack of tumor-specificity of hybrid vectors, many studies utilized targeting moiety conjugated-polymer for complexation with Ad. However, cancer is heterogeneous in cell morphology, phenotype, antigen expression, and inherent or acquired drug resistance. For example, the HER2/neu receptor is only overexpressed in 20 to 30% of breast cancer patients; therefore, the active targeting moiety-conjugated Ad/polymer based platform strategy is ineffective for treating all cancer types. To improve this approach, recently several studies developed a tumor microenvironment targeting strategy that utilizes pH sensitive polymers to target acidic tumor microenvironment [121,122].
In stimuli-responsive delivery systems, the anticancer gene or drug can be released by a certain unique stimulus of tumor microenvironment, such as pH, glucose, and temperature [123]. Among all utilized stimuli, acidic pH status of the internal tumor has been considered as an ideal trigger for the tumor-selective release of anticancer drugs as pH of both primary and metastasized tumors is lower than that of normal tissue. To this end, tumor extracellular pH values of most solid tumors range from pH 6.5 to 7.2 [124]. Lower pH of the tumor microenvironment has been most utilized stimuli in stimulus-sensitive polymeric nano carriers. The pH sensitive polymer may be designed and engineered to display tunable property pH sensitivity and controlled release by the introduction of ionizable amino groups onto the backbones [125]. The pH-sensitive polymer is stable at a physiological condition, yet it can be destabilized in acidic tumor microenvironment to facilitate the release of loaded drugs or gene (Fig. 4).
Fig. 4.
Tumor microenvironment targeting. At normal physiological condition such as blood, oncolytic Ad/pH sensitive polymer complex is stable and deprotonated. PEGylation of pH sensitive polymer prolongs blood retention time of the complex and facilitates intratumoral accumulation. At acidic tumor microenvironment, pH sensitive complex is protonated and net surface charge of the complex becomes cationic and is internalized into the tumor cells through charge-mediated internalization.
In this regard, Moon et al. demonstrated specialized oncolytic Ad/polymer hybrid vectors that take advantage of specific tumor microenvironment property including the tumor’s extracellular pH, resulting in tumor specific delivery of oncolytic Ad [121]. The newly designed and synthesized pH-sensitive polymer with bioreducible disulfide bond (mPEG-PiP-CBA; PPCBA) and pip of polymer backbone can be protonated under acidic conditions resulting in a charge reversal from negative to positive. This charge reversal enhanced cellular uptake and release of oncolytic Ad at the tumor site resulting in greater cellular uptake and killing efficacy at pH 6.4 than pH 7.4. Moreover, intratumorally and intravenously injected oncolytic Ad (RdB/shVEGF)-PPCBA nanocomplexes elicited significantly higher anti-tumor efficacy than naked RdB/shVEGF in U87 tumor xenograft models in mice. These results demonstrate the feasibility of pH-sensitive polymer-coated Ad system to be widely applied to treat solid tumors that are known to have an acidic tumor microenvironment.
Recently, Choi et al. investigated tumor microenvironment specific targeting with oncolytic Ad complexed with the pH-sensitive block copolymer, and methoxy poly(ethylene glycol)-b-poly(L-histidine-coLphenylalanine) (PEGbPHF) [122]. Poly(L-histidine) (pHis) is a promising pH-sensitive polybase for stimuli-responsive polymeric carrier due to the imidazole ring of its backbone. At a neutral pH of 7.4, most of the imidazole in the pHis block are not ionized. Conversely at pH 7.0 or lower, the electrons on the unsaturated nitrogen of imidazole ring are protonated and becomes highly cationic. This pH-dependent amphoteric property to the molecule by reversible protonation–deprotonation is ideal attribute for pH sensitive polymeric carrier. pH-dependent change in particle size and surface charge was observed by PEGbPHF coated Ad. The transduction efficiency of Ad/PEGbPHF increased in both CAR-positive and -negative cancers under acidic environment. The oncolytic Ad expressing VEGF promoter-targeting transcriptional repressor (KOX)/PEGbPHF complex significantly attenuated VEGF expression, cancer cell migration, and aorta sprouting at pH 6.4 than pH 7.4, suggesting KOX/PEGbPHF showed pH dependent therapeutic efficacy. The antitumor efficacy of systemically delivered KOX/PEGbPHF in a tumor xenograft model was significantly higher than that of naked KOX. Furthermore, KOX/PEGbPHF exhibited lower hepatotoxicity and immunogenicity. Taken together, these results demonstrate that KOX/PEGbPHF-coated oncolytic Ad complex increases net positive charge upon exposure to acidic tumor microenvironment, allowing efficient intratumoral accumulation of the complex.
Taking advantages of the acidic tumor microenvironment, pH-sensitive polymer coated oncolytic Ads have made a significant impact on tumor specific delivery. These pH-sensitive vectors can overcome certain limitations of the receptor-targeting delivery systems. Multi-functional polymer which combines active targeting and pH-sensitive targeting strategies can be a promising approach which could be addressed in future studies. In conclusion, pH-sensitive polymer complexed oncolytic Ads have been emerging as a fascinating field for precise cancer specific targeting delivery in the foreseeable future.
6. Conclusion
We highlighted recent advances in the modification of oncolytic Ad with diverse polymers for cancer gene therapy. Clinical trials of oncolytic Ad have demonstrated that it is feasible and safe for the cancer treatment in human, but its therapeutic efficacy is insufficient to ensure complete remission. To overcome existing shortcomings of viral vector-based gene therapy, a variety of polymer-based oncolytic Ad hybrid vector systems have been investigated. The chemical conjugation of polymers to oncolytic Ad enhanced stability and successfully protected the oncolytic Ad from innate and adaptive immunity. Furthermore, the polymer-coated oncolytic Ad through an electrostatic interaction increased the transduction efficiency as well as tumor-specific accumulation via passive targeting promoted by the EPR effect. Polymer can also be used as a linker to conjugate the targeting ligand to the surface of oncolytic Ad, resulting in tumor-specific delivery and gene expression of oncolytic Ad. Above all, thorough and tailored strategies of oncolytic Ad/polymer will be necessary for its future application in human clinical trials. Further developments in the multifunctional biomaterial and bioengineering technology can provide better biodegradable vehicles and finally improve the safety and therapeutic efficacy of oncolytic Ad for cancer gene therapy.
Acknowledgments
This work was supported by grants from the National Research Foundation of Korea (2010-0029220, 2013M3A9D3045879 to CO Yun), and the National Institutes of Health, USA (CA177932 to SW Kim).
Footnotes
Conflict of interest
The authors declare no competing financial interests.
References
- 1.Popat K, McQueen K, Feeley TW. The global burden of cancer. Best Pract Res Clin Anaesthesiol. 2013;27:399–408. doi: 10.1016/j.bpa.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Alemany R. Chapter four—design of improved oncolytic adenoviruses. Adv Cancer Res. 2012;115:93–114. doi: 10.1016/B978-0-12-398342-8.00004-5. [DOI] [PubMed] [Google Scholar]
- 3.Cawood R, Hills T, Wong SL, Alamoudi AA, Beadle S, Fisher KD, Seymour LW. Recombinant viral vaccines for cancer. Trends Mol Med. 2012;18:564–574. doi: 10.1016/j.molmed.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Harrop R, John J, Carroll MW. Recombinant viral vectors: cancer vaccines. Adv Drug Deliv Rev. 2006;58:931–947. doi: 10.1016/j.addr.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Russell SJ, Peng KW, Bell JC. Oncolytic virotherapy. Nat Biotechnol. 2012;30:658–670. doi: 10.1038/nbt.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wodrich H, Henaff D, Jammart B, Segura-Morales C, Seelmeir S, Coux O, Ruzsics Z, Wiethoff CM, Kremer EJ. A capsid-encoded PPxY-motif facilitates adenovirus entry. PLoS Pathog. 2010;6:e1000808. doi: 10.1371/journal.ppat.1000808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorer DE, Nettelbeck DM. Targeting cancer by transcriptional control in cancer gene therapy and viral oncolysis. Adv Drug Deliv Rev. 2009;61:554–571. doi: 10.1016/j.addr.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Kim J, Lee B, Kim JS, Yun CO, Kim JH, Lee YJ, Joo CH, Lee H. Antitumoral effects of recombinant adenovirus YKL-1001, conditionally replicating in alpha-fetoprotein-producing human liver cancer cells. Cancer Lett. 2002;180:23–32. doi: 10.1016/s0304-3835(02)00017-4. [DOI] [PubMed] [Google Scholar]
- 9.Kim E, Kim JH, Shin HY, Lee H, Yang JM, Kim J, Sohn JH, Kim H, Yun CO. Ad-mTERT-delta19, a conditional replication-competent adenovirus driven by the human telomerase promoter, selectively replicates in and elicits cytopathic effect in a cancer cell-specific manner. Hum Gene Ther. 2003;14:1415–1428. doi: 10.1089/104303403769211637. [DOI] [PubMed] [Google Scholar]
- 10.Kwon OJ, Kim PH, Huyn S, Wu L, Kim M, Yun CO. A hypoxia- and {alpha}-fetoprotein-dependent oncolytic adenovirus exhibits specific killing of hepatocellular carcinomas. Clin Cancer Res. 2010;16:6071–6082. doi: 10.1158/1078-0432.CCR-10-0664. [DOI] [PubMed] [Google Scholar]
- 11.Cattaneo R, Miest T, Shashkova EV, Barry MA. Reprogrammed viruses as cancer therapeutics: targeted, armed and shielded. Nat Rev Microbiol. 2008;6:529–540. doi: 10.1038/nrmicro1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang WW, Alemany R, Wang J, Koch PE, Ordonez NG, Roth JA. Safety evaluation of Ad5CMV-p53 in vitro and in vivo. Hum Gene Ther. 1995;6:155–164. doi: 10.1089/hum.1995.6.2-155. [DOI] [PubMed] [Google Scholar]
- 13.Shewach DS, Zerbe LK, Hughes TL, Roessler BJ, Breakefield XO, Davidson BL. Enhanced cytotoxicity of antiviral drugs mediated by adenovirus directed transfer of the herpes simplex virus thymidine kinase gene in rat glioma cells. Cancer Gene Ther. 1994;1:107–112. [PubMed] [Google Scholar]
- 14.Hirschowitz EA, Ohwada A, Pascal WR, Russi TJ, Crystal RG. In vivo adenovirus-mediated gene transfer of the Escherichia coli cytosine deaminase gene to human colon carcinoma-derived tumors induces chemosensitivity to 5-fluorocytosine. Hum Gene Ther. 1995;6:1055–1063. doi: 10.1089/hum.1995.6.8-1055. [DOI] [PubMed] [Google Scholar]
- 15.Sanz L, Kristensen P, Blanco B, Facteau S, Russell SJ, Winter G, Alvarez-Vallina L. Single-chain antibody-based gene therapy: inhibition of tumor growth by in situ production of phage-derived human antibody fragments blocking functionally active sites of cell-associated matrices. Gene Ther. 2002;9:1049–1053. doi: 10.1038/sj.gt.3301725. [DOI] [PubMed] [Google Scholar]
- 16.Yun CO, Kim E, Koo T, Kim H, Lee YS, Kim JH. ADP-overexpressing adenovirus elicits enhanced cytopathic effect by induction of apoptosis. Cancer Gene Ther. 2005;12:61–71. doi: 10.1038/sj.cgt.7700769. [DOI] [PubMed] [Google Scholar]
- 17.Kim JH, Lee YS, Kim H, Huang JH, Yoon AR, Yun CO. Relaxin expression from tumor-targeting adenoviruses and its intratumoral spread, apoptosis induction, and efficacy. J Natl Cancer Inst. 2006;98:1482–1493. doi: 10.1093/jnci/djj397. [DOI] [PubMed] [Google Scholar]
- 18.Choi IK, Lee YS, Yoo JY, Yoon AR, Kim H, Kim DS, Seidler DG, Kim JH, Yun CO. Effect of decorin on overcoming the extracellular matrix barrier for oncolytic virotherapy. Gene Ther. 2010;17:190–201. doi: 10.1038/gt.2009.142. [DOI] [PubMed] [Google Scholar]
- 19.Jiang H, Gomez-Manzano C, Rivera-Molina Y, Lang FF, Conrad CA, Fueyo J. Oncolytic adenovirus research evolution: from cell-cycle checkpoints to immune checkpoints. Curr Opin Virol. 2015;13:33–39. doi: 10.1016/j.coviro.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi KJ, Kim JH, Lee YS, Kim J, Suh BS, Kim H, Cho S, Sohn JH, Kim GE, Yun CO. Concurrent delivery of GM-CSF and B7-1 using an oncolytic adenovirus elicits potent antitumor effect. Gene Ther. 2006;13:1010–1020. doi: 10.1038/sj.gt.3302759. [DOI] [PubMed] [Google Scholar]
- 21.Lee YS, Kim JH, Choi KJ, Choi IK, Kim H, Cho S, Cho BC, Yun CO. Enhanced antitumor effect of oncolytic adenovirus expressing interleukin-12 and B7-1 in an immunocompetent murine model. Clin Cancer Res. 2006;12:5859–5868. doi: 10.1158/1078-0432.CCR-06-0935. [DOI] [PubMed] [Google Scholar]
- 22.Neri D, Bicknell R. Tumour vascular targeting. Nat Rev Cancer. 2005;5:436–446. doi: 10.1038/nrc1627. [DOI] [PubMed] [Google Scholar]
- 23.Yoo JY, Kim JH, Kim J, Huang JH, Zhang SN, Kang YA, Kim H, Yun CO. Short hairpin RNA-expressing oncolytic adenovirus-mediated inhibition of IL-8: effects on antiangiogenesis and tumor growth inhibition. Gene Ther. 2008;15:635–651. doi: 10.1038/gt.2008.3. [DOI] [PubMed] [Google Scholar]
- 24.Qiao J, Wang H, Kottke T, White C, Twigger K, Diaz RM, Thompson J, Selby P, de Bono J, Melcher A, Pandha H, Coffey M, Vile R, Harrington K. Cyclophosphamide facilitates antitumor efficacy against subcutaneous tumors following intravenous delivery of reovirus. Clin Cancer Res. 2008;14:259–269. doi: 10.1158/1078-0432.CCR-07-1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelly EJ, Russell SJ. MicroRNAs and the regulation of vector tropism. Mol Ther. 2009;17:409–416. doi: 10.1038/mt.2008.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoo JY, Kim JH, Kwon YG, Kim EC, Kim NK, Choi HJ, Yun CO. VEGF-specific short hairpin RNA-expressing oncolytic adenovirus elicits potent inhibition of angiogenesis and tumor growth. Mol Ther. 2007;15:295–302. doi: 10.1038/sj.mt.6300023. [DOI] [PubMed] [Google Scholar]
- 27.Elsedawy NB, Russell SJ. Oncolytic vaccines. Expert Rev Vaccines. 2013;12:1155–1172. doi: 10.1586/14760584.2013.836912. [DOI] [PubMed] [Google Scholar]
- 28.Woller N, Gurlevik E, Ureche CI, Schumacher A, Kuhnel F. Oncolytic viruses as anticancer vaccines. Front Oncol. 2014;4:188. doi: 10.3389/fonc.2014.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Satoh T, Saika T, Ebara S, Kusaka N, Timme TL, Yang G, Wang J, Mouraviev V, Cao G, Fattah MA, Thompson TC. Macrophages transduced with an adenoviral vector expressing interleukin 12 suppress tumor growth and metastasis in a preclinical metastatic prostate cancer model. Cancer Res. 2003;63:7853–7860. [PubMed] [Google Scholar]
- 30.Alberti MO, Roth JC, Ismail M, Tsuruta Y, Abraham E, Pereboeva L, Gerson SL, Curiel DT. Derivation of a myeloid cell-binding adenovirus for gene therapy of inflammation. PLoS One. 2012;7:e37812. doi: 10.1371/journal.pone.0037812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garcia-Castro J, Alemany R, Cascallo M, Martinez-Quintanilla J, del Arriero MM, Lassaletta A, Madero L, Ramirez M. Treatment of metastatic neuroblastoma with systemic oncolytic virotherapy delivered by autologous mesenchymal stem cells: an exploratory study. Cancer Gene Ther. 2010;17:476–483. doi: 10.1038/cgt.2010.4. [DOI] [PubMed] [Google Scholar]
- 32.Mader EK, Maeyama Y, Lin Y, Butler GW, Russell HM, Galanis E, Russell SJ, Dietz AB, Peng KW. Mesenchymal stem cell carriers protect oncolytic measles viruses from antibody neutralization in an orthotopic ovarian cancer therapy model. Clin Cancer Res. 2009;15:7246–7255. doi: 10.1158/1078-0432.CCR-09-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brenner MK, Heslop H, Krance R, Horowitz M, Strother D, Nuchtern J, Grilley B, Martingano E, Cooper K. Phase I study of chemokine and cytokine gene-modified autologous neuroblastoma cells for treatment of relapsed/refractory neuroblastoma using an adenoviral vector. Hum Gene Ther. 2000;11:1477–1488. doi: 10.1089/10430340050057549. [DOI] [PubMed] [Google Scholar]
- 34.Ilett EJ, Prestwich RJ, Kottke T, Errington F, Thompson JM, Harrington KJ, Pandha HS, Coffey M, Selby PJ, Vile RG, Melcher AA. Dendritic cells and T cells deliver oncolytic reovirus for tumour killing despite pre-existing anti-viral immunity. Gene Ther. 2009;16:689–699. doi: 10.1038/gt.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kottke T, Thompson J, Diaz RM, Pulido J, Willmon C, Coffey M, Selby P, Melcher A, Harrington K, Vile RG. Improved systemic delivery of oncolytic reovirus to established tumors using preconditioning with cyclophosphamide-mediated Treg modulation and interleukin-2. Clin Cancer Res. 2009;15:561–569. doi: 10.1158/1078-0432.CCR-08-1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kurozumi K, Hardcastle J, Thakur R, Yang M, Christoforidis G, Fulci G, Hochberg FH, Weissleder R, Carson W, Chiocca EA, Kaur B. Effect of tumor microenvironment modulation on the efficacy of oncolytic virus therapy. J Natl Cancer Inst. 2007;99:1768–1781. doi: 10.1093/jnci/djm229. [DOI] [PubMed] [Google Scholar]
- 37.Bressy C, Benihoud K. Association of oncolytic adenoviruses with chemotherapies: an overview and future directions. Biochem Pharmacol. 2014;90:97–106. doi: 10.1016/j.bcp.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 38.Forbes NE, Krishnan R, Diallo JS. Pharmacological modulation of anti-tumor immunity induced by oncolytic viruses. Front Oncol. 2014;4:191. doi: 10.3389/fonc.2014.00191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bradbury J. Oncolytic viral anti-cancer therapy: a magic bullet? Lancet. 2001;357:614. doi: 10.1016/S0140-6736(05)71407-0. [DOI] [PubMed] [Google Scholar]
- 40.Vacchelli E, Eggermont A, Sautes-Fridman C, Galon J, Zitvogel L, Kroemer G, Galluzzi L. Trial watch: oncolytic viruses for cancer therapy. Oncoimmunology. 2013;2:e24612. doi: 10.4161/onci.24612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cerullo V, Vaha-Koskela M, Hemminki A. Oncolytic adenoviruses: a potent form of tumor immunovirotherapy. Oncoimmunology. 2012;1:979–981. doi: 10.4161/onci.20172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eager RM, Nemunaitis J. Clinical development directions in oncolytic viral therapy. Cancer Gene Ther. 2011;18:305–317. doi: 10.1038/cgt.2011.7. [DOI] [PubMed] [Google Scholar]
- 43.Small EJ, Carducci MA, Burke JM, Rodriguez R, Fong L, van Ummersen L, Yu DC, Aimi J, Ando D, Working P, Kirn D, Wilding G. A phase I trial of intravenous CG7870, a replication-selective, prostate-specific antigen-targeted oncolytic adenovirus, for the treatment of hormone-refractory, metastatic prostate cancer. Mol Ther. 2006;14:107–117. doi: 10.1016/j.ymthe.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 44.Yu DC, Chen Y, Seng M, Dilley J, Henderson DR. The addition of adenovirus type 5 region E3 enables calydon virus 787 to eliminate distant prostate tumor xenografts. Cancer Res. 1999;59:4200–4203. [PubMed] [Google Scholar]
- 45.Pol >J, Bloy N, Obrist F, Eggermont A, Galon J, Cremer I, Erbs P, Limacher JM, Preville X, Zitvogel L, Kroemer G, Galluzzi L. Trial Watch: oncolytic viruses for cancer therapy. Oncoimmunology. 2014;3:e28694. doi: 10.4161/onci.28694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kanerva A, Nokisalmi P, Diaconu I, Koski A, Cerullo V, Liikanen I, Tahtinen S, Oksanen M, Heiskanen R, Pesonen S, Joensuu T, Alanko T, Partanen K, Laasonen L, Kairemo K, Kangasniemi L, Hemminki A. Antiviral and antitumor T-cell immunity in patients treated with GM-CSF-coding oncolytic adenovirus. Clin Cancer Res. 2013;19:2734–2744. doi: 10.1158/1078-0432.CCR-12-2546. [DOI] [PubMed] [Google Scholar]
- 47.Bramante S, Kaufmann JK, Veckman V, Liikanen I, Nettelbeck DM, Hemminki O, Vassilev L, Cerullo V, Oksanen M, Heiskanen R, Joensuu T, Kanerva A, Pesonen S, Matikainen S, Vaha-Koskela M, Koski A, Hemminki A. Treatment of melanoma with a serotype 5/3 chimeric oncolytic adenovirus coding for GM-CSF: results in vitro, in rodents and in humans. 2015. [DOI] [PubMed] [Google Scholar]
- 48.Shirakawa T, Terao S, Hinata N, Tanaka K, Takenaka A, Hara I, Sugimura K, Matsuo M, Hamada K, Fuji K, Okegawa T, Higashihara E, Gardner TA, Kao C, Chung LW, Kamidono S, Fujisawa M, Gotoh A. Long-term outcome of phase I/II clinical trial of Ad-OC-TK/VAL gene therapy for hormone-refractory metastatic prostate cancer. Hum Gene Ther. 2007;18:1225–1232. doi: 10.1089/hum.2007.074. [DOI] [PubMed] [Google Scholar]
- 49.Hinata N, Shirakawa T, Terao S, Goda K, Tanaka K, Yamada Y, Hara I, Kamidono S, Fujisawa M, Gotoh A. Progress report on phase I/II clinical trial of Ad-OC-TK plus VAL therapy for metastatic or locally recurrent prostate cancer: initial experience at Kobe University. Int J Urol. 2006;13:834–837. doi: 10.1111/j.1442-2042.2006.01418.x. [DOI] [PubMed] [Google Scholar]
- 50.Chiappori AA, Soliman H, Janssen WE, Antonia SJ, Gabrilovich DI. INGN-225: a dendritic cell-based p53 vaccine (Ad.p53-DC) in small cell lung cancer: observed association between immune response and enhanced chemotherapy effect. Expert Opin Biol Ther. 2010;10:983–991. doi: 10.1517/14712598.2010.484801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Freytag SO, Stricker H, Lu M, Elshaikh M, Aref I, Pradhan D, Levin K, Kim JH, Peabody J, Siddiqui F, Barton K, Pegg J, Zhang Y, Cheng J, Oja-Tebbe N, Bourgeois R, Gupta N, Lane Z, Rodriguez R, DeWeese T, Movsas B. Prospective randomized phase 2 trial of intensity modulated radiation therapy with or without oncolytic adenovirus-mediated cytotoxic gene therapy in intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2014;89:268–276. doi: 10.1016/j.ijrobp.2014.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang H, Gomez-Manzano C, Lang FF, Alemany R, Fueyo J. Oncolytic adenovirus: preclinical and clinical studies in patients with human malignant gliomas. Curr Gene Ther. 2009;9:422–427. doi: 10.2174/156652309789753356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Freytag SO, Rogulski KR, Paielli DL, Gilbert JD, Kim JH. A novel three-pronged approach to kill cancer cells selectively: concomitant viral, double suicide gene, and radiotherapy. Hum Gene Ther. 1998;9:1323–1333. doi: 10.1089/hum.1998.9.9-1323. [DOI] [PubMed] [Google Scholar]
- 54.Freytag SO, Stricker H, Pegg J, Paielli D, Pradhan DG, Peabody J, DePeralta-Venturina M, Xia X, Brown S, Lu M, Kim JH. Phase I study of replication-competent adenovirus-mediated double-suicide gene therapy in combination with conventional-dose three-dimensional conformal radiation therapy for the treatment of newly diagnosed, intermediate- to high-risk prostate cancer. Cancer Res. 2003;63:7497–7506. [PubMed] [Google Scholar]
- 55.Freytag SO, Khil M, Stricker H, Peabody J, Menon M, DePeralta-Venturina M, Nafziger D, Pegg J, Paielli D, Brown S, Barton K, Lu M, Aguilar-Cordova E, Kim JH. Phase I study of replication-competent adenovirus-mediated double suicide gene therapy for the treatment of locally recurrent prostate cancer. Cancer Res. 2002;62:4968–4976. [PubMed] [Google Scholar]
- 56.Kim KH, Dmitriev IP, Saddekni S, Kashentseva EA, Harris RD, Aurigemma R, Bae S, Singh KP, Siegal GP, Curiel DT, Alvarez RD. A phase I clinical trial of Ad5/3-Delta24, a novel serotype-chimeric, infectivity-enhanced, conditionally-replicative adenovirus (CRAd), in patients with recurrent ovarian cancer. Gynecol Oncol. 2013;130:518–524. doi: 10.1016/j.ygyno.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang B, Zhang Y, Wang J, Zhang Y, Chen J, Pan Y, Ren L, Hu Z, Zhao J, Liao M, Wang S. Screening and identification of a targeting peptide to hepatocarcinoma from a phage display peptide library. Mol Med. 2007;13:246–254. doi: 10.2119/2006-00115.Zhang. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gabrilovich DI. INGN 201 (Advexin): adenoviral p53 gene therapy for cancer. Expert Opin Biol Ther. 2006;6:823–832. doi: 10.1517/14712598.6.8.823. [DOI] [PubMed] [Google Scholar]
- 59.Miest TS, Cattaneo R. New viruses for cancer therapy: meeting clinical needs. Nat Rev Microbiol. 2014;12:23–34. doi: 10.1038/nrmicro3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.DeWeese TL, van der Poel H, Li S, Mikhak B, Drew R, Goemann M, Hamper U, DeJong R, Detorie N, Rodriguez R, Haulk T, DeMarzo AM, Piantadosi S, Yu DC, Chen Y, Henderson DR, Carducci MA, Nelson WG, Simons JW. A phase I trial of CV706, a replication-competent, PSA selective oncolytic adenovirus, for the treatment of locally recurrent prostate cancer following radiation therapy. Cancer Res. 2001;61:7464–7472. [PubMed] [Google Scholar]
- 61.Ferguson MS, Lemoine NR, Wang Y. Systemic delivery of oncolytic viruses: hopes and hurdles. Adv Virol. 2012;2012:805629. doi: 10.1155/2012/805629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shilpa P, Kaul R, Bhat S, Sultana N, Pandeshwar P. Oncolytic viruses in head and neck cancer: a new ray of hope in the management protocol. Ann Med Health Sci Res. 2014;4:S178–S184. doi: 10.4103/2141-9248.141953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nemunaitis J, Khuri F, Ganly I, Arseneau J, Posner M, Vokes E, Kuhn J, McCarty T, Landers S, Blackburn A, Romel L, Randlev B, Kaye S, Kirn D. Phase II trial of intratumoral administration of ONYX-015, a replication-selective adenovirus, in patients with refractory head and neck cancer. J Clin Oncol. 2001;19:289–298. doi: 10.1200/JCO.2001.19.2.289. [DOI] [PubMed] [Google Scholar]
- 64.Khuri FR, Nemunaitis J, Ganly I, Arseneau J, Tannock IF, Romel L, Gore M, Ironside J, MacDougall RH, Heise C, Randlev B, Gillenwater AM, Bruso P, Kaye SB, Hong WK, Kirn DH. A controlled trial of intratumoral ONYX-015, a selectively-replicating adenovirus, in combination with cisplatin and 5-fluorouracil in patients with recurrent head and neck cancer. Nat Med. 2000;6:879–885. doi: 10.1038/78638. [DOI] [PubMed] [Google Scholar]
- 65.Makower D, Rozenblit A, Kaufman H, Edelman M, Lane ME, Zwiebel J, Haynes H, Wadler S. Phase II clinical trial of intralesional administration of the oncolytic adenovirus ONYX-015 in patients with hepatobiliary tumors with correlative p53 studies. Clin Cancer Res. 2003;9:693–702. [PubMed] [Google Scholar]
- 66.Muruve DA, Barnes MJ, Stillman IE, Libermann TA. Adenoviral gene therapy leads to rapid induction of multiple chemokines and acute neutrophil-dependent hepatic injury in vivo. Hum Gene Ther. 1999;10:965–976. doi: 10.1089/10430349950018364. [DOI] [PubMed] [Google Scholar]
- 67.Schnell MA, Zhang Y, Tazelaar J, Gao GP, Yu QC, Qian R, Chen SJ, Varnavski AN, LeClair C, Raper SE, Wilson JM. Activation of innate immunity in non-human primates following intraportal administration of adenoviral vectors. Mol Ther. 2001;3:708–722. doi: 10.1006/mthe.2001.0330. [DOI] [PubMed] [Google Scholar]
- 68.Zhang Y, Chirmule N, Gao GP, Qian R, Croyle M, Joshi B, Tazelaar J, Wilson JM. Acute cytokine response to systemic adenoviral vectors in mice is mediated by dendritic cells and macrophages. Mol Ther. 2001;3:697–707. doi: 10.1006/mthe.2001.0329. [DOI] [PubMed] [Google Scholar]
- 69.Yang Y, Li Q, Ertl HC, Wilson JM. Cellular and humoral immune responses to viral antigens create barriers to lung-directed gene therapy with recombinant adenoviruses. J Virol. 1995;69:2004–2015. doi: 10.1128/jvi.69.4.2004-2015.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Molnar-Kimber KL, Sterman DH, Chang M, Kang EH, ElBash M, Lanuti M, Elshami A, Gelfand K, Wilson JM, Kaiser LR, Albelda SM. Impact of preexisting and induced humoral and cellular immune responses in an adenovirus-based gene therapy phase I clinical trial for localized mesothelioma. Hum Gene Ther. 1998;9:2121–2133. doi: 10.1089/hum.1998.9.14-2121. [DOI] [PubMed] [Google Scholar]
- 71.Xu Z, Tian J, Smith JS, Byrnes AP. Clearance of adenovirus by Kupffer cells is mediated by scavenger receptors, natural antibodies, and complement. J Virol. 2008;82:11705–11713. doi: 10.1128/JVI.01320-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Smith JS, Xu Z, Byrnes AP. A quantitative assay for measuring clearance of adenovirus vectors by Kupffer cells. J Virol Methods. 2008;147:54–60. doi: 10.1016/j.jviromet.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 73.Myhre S, Henning P, Granio O, Tylo AS, Nygren PA, Olofsson S, Boulanger P, Lindholm L, Hong SS. Decreased immune reactivity towards a knobless, affibody-targeted adenovirus type 5 vector. Gene Ther. 2007;14:376–381. doi: 10.1038/sj.gt.3302875. [DOI] [PubMed] [Google Scholar]
- 74.O’Riordan CR, Lachapelle A, Delgado C, Parkes V, Wadsworth SC, Smith AE, Francis GE. PEGylation of adenovirus with retention of infectivity and protection from neutralizing antibody in vitro and in vivo. Hum Gene Ther. 1999;10:1349–1358. doi: 10.1089/10430349950018021. [DOI] [PubMed] [Google Scholar]
- 75.Croyle MA, Chirmule N, Zhang Y, Wilson JM. “Stealth” adenoviruses blunt cell-mediated and humoral immune responses against the virus and allow for significant gene expression upon readministration in the lung. J Virol. 2001;75:4792–4801. doi: 10.1128/JVI.75.10.4792-4801.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kim PH, Kim J, Kim TI, Nam HY, Yockman JW, Kim M, Kim SW, Yun CO. Bioreducible polymer-conjugated oncolytic adenovirus for hepatoma-specific therapy via systemic administration. Biomaterials. 2011;32:9328–9342. doi: 10.1016/j.biomaterials.2011.08.066. [DOI] [PubMed] [Google Scholar]
- 77.Delgado C, Francis GE, Fisher D. The uses and properties of PEG-linked proteins. Crit Rev Ther Drug Carrier Syst. 1992;9:249–304. [PubMed] [Google Scholar]
- 78.Parveen S, Sahoo SK. Nanomedicine: clinical applications of polyethylene glycol conjugated proteins and drugs. Clin Pharmacokinet. 2006;45:965–988. doi: 10.2165/00003088-200645100-00002. [DOI] [PubMed] [Google Scholar]
- 79.Kumar TR, Soppimath K, Nachaegari SK. Novel delivery technologies for protein and peptide therapeutics. Curr Pharm Biotechnol. 2006;7:261–276. doi: 10.2174/138920106777950852. [DOI] [PubMed] [Google Scholar]
- 80.Knop K, Hoogenboom R, Fischer D, Schubert US. Poly(ethylene glycol) in drug delivery: pros and cons as well as potential alternatives. Angew Chem. 2010;49:6288–6308. doi: 10.1002/anie.200902672. [DOI] [PubMed] [Google Scholar]
- 81.Wortmann A, Vohringer S, Engler T, Corjon S, Schirmbeck R, Reimann J, Kochanek S, Kreppel F. Fully detargeted polyethylene glycol-coated adenovirus vectors are potent genetic vaccines and escape from pre-existing anti-adenovirus antibodies. Mol Ther. 2008;16:154–162. doi: 10.1038/sj.mt.6300306. [DOI] [PubMed] [Google Scholar]
- 82.Doronin K, Shashkova EV, May SM, Hofherr SE, Barry MA. Chemical modification with high molecular weight polyethylene glycol reduces transduction of hepatocytes and increases efficacy of intravenously delivered oncolytic adenovirus. Hum Gene Ther. 2009;20:975–988. doi: 10.1089/hum.2009.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pack DW, Hoffman AS, Pun S, Stayton PS. Design and development of polymers for gene delivery. Nat Rev Drug Discov. 2005;4:581–593. doi: 10.1038/nrd1775. [DOI] [PubMed] [Google Scholar]
- 84.Varkouhi AK, Scholte M, Storm G, Haisma HJ. Endosomal escape pathways for delivery of biologicals. J Control Release. 2011;151:220–228. doi: 10.1016/j.jconrel.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 85.Moghimi SM, Hunter AC, Murray JC. Long-circulating and target-specific nanoparticles: theory to practice. Pharmacol Rev. 2001;53:283–318. [PubMed] [Google Scholar]
- 86.Yockman JW, Kastenmeier A, Erickson HM, Brumbach JG, Whitten MG, Albanil A, Li DY, Kim SW, Bull DA. Novel polymer carriers and gene constructs for treatment of myocardial ischemia and infarction. J Control Release. 2008;132:260–266. doi: 10.1016/j.jconrel.2008.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Furgeson DY, Cohen RN, Mahato RI, Kim SW. Novel water insoluble lipoparticulates for gene delivery. Pharm Res. 2002;19:382–390. doi: 10.1023/a:1015166806366. [DOI] [PubMed] [Google Scholar]
- 88.Ahn CH, Chae SY, Bae YH, Kim SW. Biodegradable poly(ethylenimine) for plasmid DNA delivery. J Control Release. 2002;80:273–282. doi: 10.1016/s0168-3659(01)00547-8. [DOI] [PubMed] [Google Scholar]
- 89.Fang G, Zeng F, Yu C, Wu S. Low molecular weight PEIs modified by hydrazone-based crosslinker and betaine as improved gene carriers. Colloids Surf B: Biointerfaces. 2014;122:472–481. doi: 10.1016/j.colsurfb.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 90.Akinc A, Thomas M, Klibanov AM, Langer R. Exploring polyethylenimine-mediated DNA transfection and the proton sponge hypothesis. J Gene Med. 2005;7:657–663. doi: 10.1002/jgm.696. [DOI] [PubMed] [Google Scholar]
- 91.Choi JW, Nam JP, Nam K, Lee YS, Yun CO, Kim SW. Oncolytic adenovirus coated with multidegradable bioreducible core-cross-linked polyethylenimine for cancer gene therapy. Biomacromolecules. 2015;16:2132–2143. doi: 10.1021/acs.biomac.5b00538. [DOI] [PubMed] [Google Scholar]
- 92.Lee CH, Kasala D, Na Y, Lee MS, Kim SW, Jeong JH, Yun CO. Enhanced therapeutic efficacy of an adenovirus-PEI-bile-acid complex in tumors with low coxsackie and adenovirus receptor expression. Biomaterials. 2014;35:5505–5516. doi: 10.1016/j.biomaterials.2014.03.060. [DOI] [PubMed] [Google Scholar]
- 93.Tomalia DA. Dendrimer research. Science. 1991;252:1231. doi: 10.1126/science.252.5010.1231-b. [DOI] [PubMed] [Google Scholar]
- 94.Haensler J, Szoka FC., Jr Polyamidoamine cascade polymers mediate efficient transfection of cells in culture. Bioconjug Chem. 1993;4:372–379. doi: 10.1021/bc00023a012. [DOI] [PubMed] [Google Scholar]
- 95.Kukowska-Latallo JF, Bielinska AU, Johnson J, Spindler R, Tomalia DA, Baker JR., Jr Efficient transfer of genetic material into mammalian cells using Starburst polyamidoamine dendrimers. Proc Natl Acad Sci U S A. 1996;93:4897–4902. doi: 10.1073/pnas.93.10.4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Grunwald GK, Vetter A, Klutz K, Willhauck MJ, Schwenk N, Senekowitsch-Schmidtke R, Schwaiger M, Zach C, Wagner E, Goke B, Holm PS, Ogris M, Spitzweg C. Systemic image-guided liver cancer radiovirotherapy using dendrimer-coated adenovirus encoding the sodium iodide symporter as theranostic gene. J Nucl Med. 2013;54:1450–1457. doi: 10.2967/jnumed.112.115493. [DOI] [PubMed] [Google Scholar]
- 97.Kim J, Li Y, Kim SW, Lee DS, Yun CO. Therapeutic efficacy of a systemically delivered oncolytic adenovirus–biodegradable polymer complex. Biomaterials. 2013;34:4622–4631. doi: 10.1016/j.biomaterials.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 98.Jung SJ, Kasala D, Choi JW, Lee SH, Hwang JK, Kim SW, Yun CO. Safety profiles and antitumor efficacy of oncolytic adenovirus coated with bioreducible polymer in the treatment of a CAR negative tumor model. Biomacromolecules. 2015;16:87–96. doi: 10.1021/bm501116x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jain RK. Barriers to drug delivery in solid tumors. Sci Am. 1994;271:58–65. doi: 10.1038/scientificamerican0794-58. [DOI] [PubMed] [Google Scholar]
- 100.Sriraman SK, Aryasomayajula B, Torchilin VP. Barriers to drug delivery in solid tumors. Tissue Barriers. 2014;2:e29528. doi: 10.4161/tisb.29528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ogris M, Wagner E. Targeting tumors with non-viral gene delivery systems. Drug Discov Today. 2002;7:479–485. doi: 10.1016/s1359-6446(02)02243-2. [DOI] [PubMed] [Google Scholar]
- 102.Byrne JD, Betancourt T, Brannon-Peppas L. Active targeting schemes for nanoparticle systems in cancer therapeutics. Adv Drug Deliv Rev. 2008;60:1615–1626. doi: 10.1016/j.addr.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 103.Ansell SM, Harasym TO, Tardi PG, Buchkowsky SS, Bally MB, Cullis PR. Antibody conjugation methods for active targeting of liposomes. Methods Mol Med. 2000;25:51–68. doi: 10.1385/1-59259-075-6:51. [DOI] [PubMed] [Google Scholar]
- 104.Manjappa AS, Goel PN, Gude RP, Ramachandra Murthy RS. Anti-neuropilin 1 antibody Fab’ fragment conjugated liposomal docetaxel for active targeting of tumours. J Drug Target. 2014;22:698–711. doi: 10.3109/1061186X.2014.910792. [DOI] [PubMed] [Google Scholar]
- 105.Wu X, Chen J, Wu M, Zhao JX. Aptamers: active targeting ligands for cancer diagnosis and therapy. Theranostics. 2015;5:322–344. doi: 10.7150/thno.10257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhang N, Wardwell PR, Bader RA. Polysaccharide-based micelles for drug delivery. Pharmaceutics. 2013;5:329–352. doi: 10.3390/pharmaceutics5020329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yu MK, Park J, Jon S. Targeting strategies for multifunctional nanoparticles in cancer imaging and therapy. Theranostics. 2012;2:3–44. doi: 10.7150/thno.3463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kim J, Nam HY, Kim TI, Kim PH, Ryu J, Yun CO, Kim SW. Active targeting of RGD-conjugated bioreducible polymer for delivery of oncolytic adenovirus expressing shRNA against IL-8 mRNA. Biomaterials. 2011;32:5158–5166. doi: 10.1016/j.biomaterials.2011.03.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ge Z, Chen Q, Osada K, Liu X, Tockary TA, Uchida S, Dirisala A, Ishii T, Nomoto T, Toh K, Matsumoto Y, Oba M, Kano MR, Itaka K, Kataoka K. Targeted gene delivery by polyplex micelles with crowded PEG palisade and cRGD moiety for systemic treatment of pancreatic tumors. Biomaterials. 2014;35:3416–3426. doi: 10.1016/j.biomaterials.2013.12.086. [DOI] [PubMed] [Google Scholar]
- 110.Kim J, Nam HY, Choi JW, Yun CO, Kim SW. Efficient lung orthotopic tumor-growth suppression of oncolytic adenovirus complexed with RGD-targeted bioreducible polymer. Gene Ther. 2014;21:476–483. doi: 10.1038/gt.2014.18. [DOI] [PubMed] [Google Scholar]
- 111.Iqbal N, Iqbal N. Human epidermal growth factor receptor 2 (HER2) in cancers: overexpression and therapeutic implications. Biochem Mol Biol Int. 2014;2014:852748. doi: 10.1155/2014/852748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gajria D, Chandarlapaty S. HER2-amplified breast cancer: mechanisms of trastuzumab resistance and novel targeted therapies. Expert Rev Anticancer Ther. 2011;11:263–275. doi: 10.1586/era.10.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Alba E, Albanell J, de la Haba J, Barnadas A, Calvo L, Sanchez-Rovira P, Ramos M, Rojo F, Burgues O, Carrasco E, Caballero R, Porras I, Tibau A, Camara MC, Lluch A. Trastuzumab or lapatinib with standard chemotherapy for HER2-positive breast cancer: results from the GEICAM/2006-14 trial. Br J Cancer. 2014;110:1139–1147. doi: 10.1038/bjc.2013.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kim PH, Sohn JH, Choi JW, Jung Y, Kim SW, Haam S, Yun CO. Active targeting and safety profile of PEG-modified adenovirus conjugated with herceptin. Biomaterials. 2011;32:2314–2326. doi: 10.1016/j.biomaterials.2010.10.031. [DOI] [PubMed] [Google Scholar]
- 115.Zhao XB, Lee RJ. Tumor-selective targeted delivery of genes and antisense oligodeoxyribonucleotides via the folate receptor. Adv Drug Deliv Rev. 2004;56:1193–1204. doi: 10.1016/j.addr.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 116.Kwon OJ, Kang E, Choi JW, Kim SW, Yun CO. Therapeutic targeting of chitosan–PEG–folate-complexed oncolytic adenovirus for active and systemic cancer gene therapy. J Control Release. 2013;169:257–265. doi: 10.1016/j.jconrel.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 117.Park Y, Kang E, Kwon OJ, Hwang T, Park H, Lee JM, Kim JH, Yun CO. Ionically crosslinked Ad/chitosan nanocomplexes processed by electrospinning for targeted cancer gene therapy. J Control Release. 2010;148:75–82. doi: 10.1016/j.jconrel.2010.06.027. [DOI] [PubMed] [Google Scholar]
- 118.Yewale C, Baradia D, Vhora I, Patil S, Misra A. Epidermal growth factor receptor targeting in cancer: a review of trends and strategies. Biomaterials. 2013;34:8690–8707. doi: 10.1016/j.biomaterials.2013.07.100. [DOI] [PubMed] [Google Scholar]
- 119.Master AM, Sen Gupta A. EGF receptor-targeted nanocarriers for enhanced cancer treatment. Nanomedicine. 2012;7:1895–1906. doi: 10.2217/nnm.12.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Grunwald GK, Vetter A, Klutz K, Willhauck MJ, Schwenk N, Senekowitsch-Schmidtke R, Schwaiger M, Zach C, Wagner E, Goke B, Holm PS, Ogris M, Spitzweg C. EGFR-targeted adenovirus dendrimer coating for improved systemic delivery of the theranostic NIS gene. Mol Ther–Nucleic Acids. 2013;2:e131. doi: 10.1038/mtna.2013.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Moon CY, Choi JW, Kasala D, Jung SJ, Kim SW, Yun CO. Dual tumor targeting with pH-sensitive and bioreducible polymer-complexed oncolytic adenovirus. Biomaterials. 2015;41:53–68. doi: 10.1016/j.biomaterials.2014.11.021. [DOI] [PubMed] [Google Scholar]
- 122.Choi JW, Jung SJ, Kasala D, Hwang JK, Hu J, Bae YH, Yun CO. pH-sensitive oncolytic adenovirus hybrid targeting acidic tumor microenvironment and angiogenesis. J Control Release. 2015;205:134–143. doi: 10.1016/j.jconrel.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Payne SJ, Jones L. Influence of the tumor microenvironment on angiogenesis. Future Oncol. 2011;7:395–408. doi: 10.2217/fon.11.13. [DOI] [PubMed] [Google Scholar]
- 124.Tannock IF, Rotin D. Acid pH in tumors and its potential for therapeutic exploitation. Cancer Res. 1989;49:4373–4384. [PubMed] [Google Scholar]
- 125.Midoux P, Pichon C, Yaouanc JJ, Jaffres PA. Chemical vectors for gene delivery: a current review on polymers, peptides and lipids containing histidine or imidazole as nucleic acids carriers. Br J Pharmacol. 2009;157:166–178. doi: 10.1111/j.1476-5381.2009.00288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]