Abstract
Objective
To determine if community equipoise exists concerning the effectiveness of bracing in adolescent idiopathic scoliosis.
Background Data
Bracing is the standard of care for adolescent idiopathic scoliosis despite the lack of strong reasearch evidence concerning its effectiveness. Thus, some researchers support the idea of a randomized trial, whereas others think that randomization in the face of a standard of care would be unethical.
Methods
A random of Scoliosis Research Society and Pediatric Orthopaedic Society of North America members were asked to consider 12 clinical profiles and to give their opinion concerning the radiographic outcomes after observation and bracing.
Results
An expert panel was created from the respondents. They expressed a wide array of opinions concerning the percentage of patients within each scenario who would benefit from bracing. Agreement was noted concerning the risk due to bracing for post-menarchal patients only.
Conclusions
This study found a high degree of variability in opinion among clinicians concerning the effectiveness of bracing, suggesting that a randomized trial of bracing would be ethical.
Keywords: adolescent idiopathic scoliosis, bracing, concensus, effectiveness, standard of care
Bracing was adopted as the standard of care for non-operative treatment of adolescent idiopathic scoliosis (AIS) long before the application of the current standards of scientific evidence. It is questionable whether a new technology would enjoy such widespread use if it was based on a literature with limitations similar to those noted in bracing: of the multiple published studies of bracing effectiveness, the overwhelming majority are level IV case series, with only a few level III case-control or retrospective cohort studies, and only 1 level II prospective cohort study. Another important limitation of the literature is the paucity of evidence concerning the effect of bracing on surgical rates despite the suggestion that the progression to surgery indicates the ultimate failure of bracing treatment.1 To our knowledge, only 2 studies2,3 have quantified (relative to observation) the risk reduction (RR) in surgical rates due to bracing.
The science of bracing has been hampered, ironically, by the publication of uncontrolled studies to support bracing as the standard of care. Consequently, researchers have hesitated to conduct a randomized trial, stating that it would be unethical to deny treatment (not brace) when bracing is considered an effective therapy that has “stood the test of time”4 even when that test has been less than rigorous. To the proponents of bracing, this may not be bothersome; however, to those who are unconvinced by the evidence, following the standard of care and prescribing a brace can itself be an ethical battle.
More than 50 pediatric orthopaedic surgeons volunteered to participate in a recent randomized trial proposed to compare bracing with the observation on AIS.5 However, several of those approached to participate declined on ethical grounds. Concerned about this objection, we decided to test the validity of the conclusion that a randomized study comparing bracing with observation is unethical using the criteria of clinical equipoise.6 Clinical equipoise has been defined as “the state of honest, professional disagreement in the community of expert practitioners as to the preferred treatment6”. Other similar definitions of equipoise include the state of uncertainty on the part of the pertinent community, the opinion that no one arm of the trial is known to offer greater harm or benefit,7 and the lack of consensus within the expert community about the comparative merits of the treatments being tested. Random assignment of treatments, under the condition of equipoise, is not then a default on the obligation to give the most appropriate treatment because this is unknown.8
Judgments concerning the presence or absence of equipoise can come from 3 sources of information: (1) informal information from the opinions of local clinicians; (2) semiformal information from evidence of different practices across physicians or localities or from differing opinions in the literature; and (3) formal information derived from the specific measurement of expert opinion.8 In the literature, only 2 published natural history studies report a rate of surgery: Bunnell,9 in 1986, reported an overall surgery rate of 16% in curves diagnosed as having an angle of between 16 and 96 degrees, whereas Goldberg et al4 reported a 28% surgery rate in curves with angle ranging from 10 to greater than 60 degrees. Table 1 summarizes the results of bracing outcome studies. Several uncontrolled retrospective case series of braced patients have been published; those reporting surgical rates demonstrate widely varying outcomes ranging from 7% to 43%.10–22 Two studies have simultaneously compared untreated and braced curves.2,3 Fernandez-Feliberti et al2 reported a 26% surgery rate in the braced cases compared with 38% in the observed cases. Miller et al,3 in their case-control study of small curves, found a 2% surgical rate in untreated curves compared with 5% in the braced group. These variations in outcomes are likely caused by different inclusion criteria, including Cobb angle and sex. The literature on surgical rates, then, is extremely variable and does not support the superiority of bracing over observation with any certainty. This variability provides some evidence of equipoise; however, the evidence for a medical intervention does not always equal the degree to which clinicians endorse the intervention or agree on its outcomes.
TABLE 1.
Surgery Rates After Bracing Treatment
| Author | Year | Level of Evidence |
Cobb Angle of Sample (degrees) |
Surgical Rate (%) |
|---|---|---|---|---|
| Fernandez-Feliberti et al2 | 1995 | III | <30 with progression, or 30–40 | 26 |
| Miller et al3 | 1984 | III | <30 | 5 |
| Allington and Bowen10 | 1996 | IV | <40 | 31 |
| Emans et al11 | 1986 | IV | 20–59 | 12 |
| Howard12 | 1998 | IV | 19–54 | 18 |
| Karol13 | 2001 | IV | Boys only | 46 |
| Katz et al14 | 1997 | IV | 25–45 | 16 |
| Katz and Durrani15 | 2001 | IV | 36–45 | 31 |
| Korovessis et al16 | 2000 | IV | 25–44 | 13 |
| Little et al17 | 2000 | IV | 25–45 | 43 |
| Piazza and Bassett18 | 1990 | IV | 20–39 | 20 |
| Spoonamore et al19 | 2004 | IV | 25–44 | 30 |
| Upadhyay et al20 | 1995 | IV | 20–45 | 18 |
| Weiss21 | 2001 | IV | 33 (average) | 7 |
| Wiley et al22 | 2000 | IV | 35–45 | 38 |
We therefore sought another source of information, a formal survey of expert opinion concerning the effect of bracing relative to observation on cases of AIS. Sufficient variability and lack of consensus in these estimates would provide additional evidence of community equipoise and would therefore support the ethics of randomization in a trial of bracing on cases of AIS.
METHODS
Expert Panel
With institutional review board approval, we used the membership rosters of the Scoliosis Research Society (SRS) and the Pediatric Orthopaedic Society of North America as the sampling frame for this study. Most members of both societies are practicing physicians, although both include small numbers of nurses, scientists, and other allied health professionals involved in the care of children with orthopaedic conditions. Both societies have official publications that regularly publish research concerning the natural history and treatment outcomes of AIS and include such articles and posters at their national meetings. A sample of 423 members was randomly selected. The responses were anonymous and no attempt was made to follow up the nonresponders. All responses were returned within 3 months after they were mailed.
The members were also asked to supply information concerning the following professional characteristics: number of years in practice, specialty, whether they completed a fellowship in that specialty, percentage of practice devoted to AIS, and a self-rating of their familiarity with the literature concerning bracing and AIS on a scale ranging from 1 to 3.
Surveys
The surveys were designed to gather the opinion of the respondents concerning the radiographic outcomes of bracing and the observation at the endpoint of skeletal maturity. Skeletal maturity was chosen as the endpoint because the risk of continued progression drops significantly after this point is reached.23 The 45-degree-angle outcome was chosen as a proxy for surgical indication, as in the studies by Little et al17 and Upadhyay et al.20
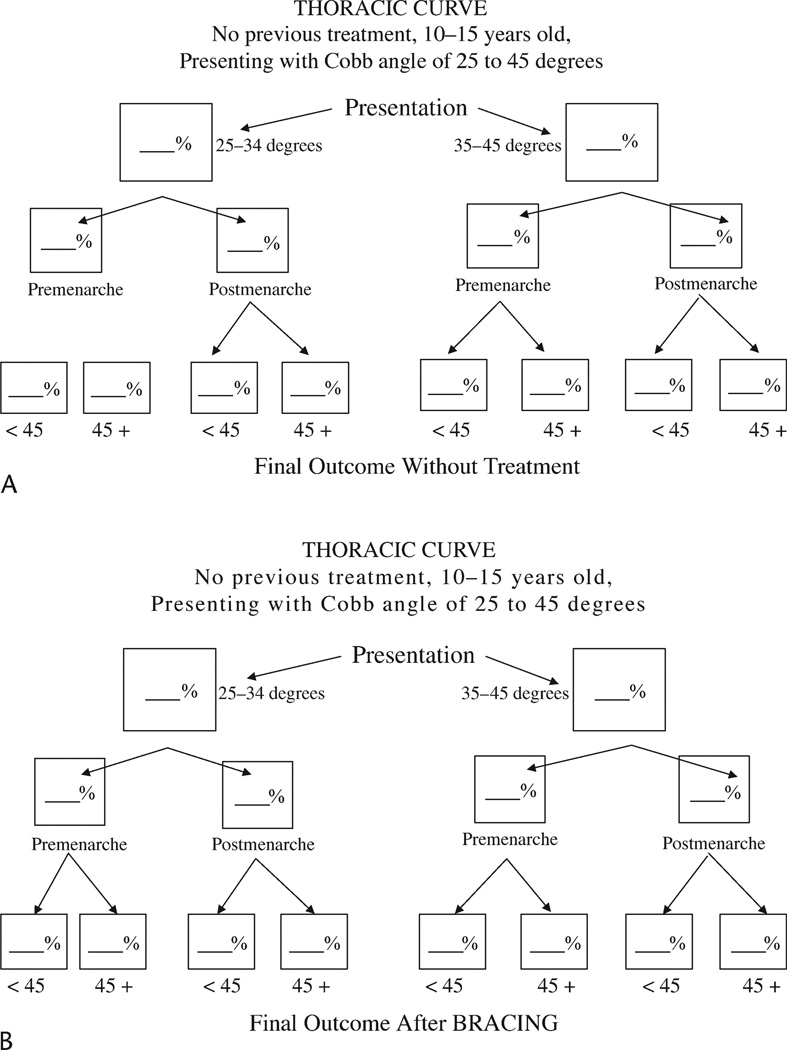
Each member received instructions and examples on how to complete the surveys. The members were asked to imagine patients between the ages of 10 and 15 years with differing clinical profiles who present to their practice for initial evaluation of AIS. The profiles included combinations of 3 curve types (thoracic, thoracolumbar/lumbar, and double major), the presence or absence of menarche, and the size of the Cobb angle (25–34 degrees or 35–45 degrees).
The survey was structured as 6 decision trees, each presenting (1) a treatment (bracing or observation); (2) branches for the clinical profiles; and (3) branches for 2 radiographic outcomes (≤45 or >45 degrees). Examples of the decision trees are given in Figures 1A and B. The members were also asked to estimate the percentage of patients from their practice presenting with each clinical profile. These estimates of practice mix were not used in the analysis but were elicited to help the respondents concentrate on each separate profile. Then, they were asked to estimate the percentage of patients in whom they would expect to achieve a curve with an angle less than 45 degrees (success) of 45 degrees or greater (failure) at skeletal maturity after both an observation (natural history) and a full course of bracing. The members were instructed to use their knowledge of the AIS literature and their experience to make these estimates.
Statistical Analysis
Descriptive statistics were calculated for the (1) percentage of patients defined as successes after bracing and after observation, (2) the RR due to bracing (the percentage of failure under observation minus the percentage of failure after bracing), and (3) the number of profiles where the respondents agreed on the RR. Agreement was defined similar to the previous work of Wright et al24 and Dunn et al.25 Agreement was present if greater than 80% of the respondents’ RR estimates were within a given range (low, 0%–39% RR; moderate, 40%–69% RR; and high, 70%–100% RR). The influence of curve type and profile on the outcomes was quantified using analysis of variance and χ2 tests of association.
RESULTS
Sample
A total of 423 surveys were mailed and 92 responses were received. Of these, 10 were from clinicians who declined to participate, and 4 responses were deemed invalid because of bracing failure rates that were uniformly higher than observation failure rates. Therefore, usable data was obtained from 78 respondents (19%). Considering the low response rate and, therefore, the questionable generalizability across all clinicians, we decided instead to use an expert panel approach similar to that used by Latthe et al26 and Lilford27 in their studies of clinical equipoise. From the 78 respondents, we chose an expert panel of those who reportedly devote more than 25% of their practice to AIS and who also consider themselves very familiar with the AIS and bracing literature. Of these 29 experts, 20 (69%) listed pediatric orthopaedics as their subspecialty; 3 (10%), spine; and 4, pediatric spine. On average, the panel had spent 22.55 years in their specialty (range, 6–45 years) and 24 (83%) had completed a fellowship in that specialty. The average percentage of practice devoted to AIS was 49% (range, 28%–100%).
Outcome Estimates
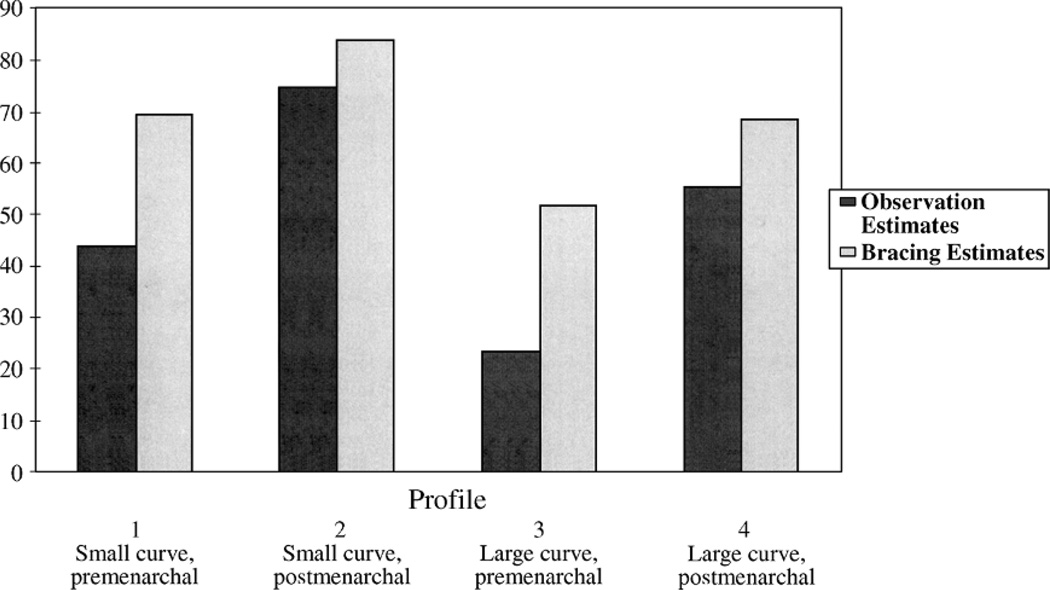
Table 2 summarizes the success estimates (percentage of curves progressing to a Cobb angle less than 45 degrees) for each of the profiles and the treatments (bracing or observation). Although the average estimates indicate that the group felt that bracing demonstrates an advantage over observation in the risk of surgery, the estimates for both bracing and observation varied widely. For example, the panel estimated that anywhere from 20% to 80% of small thoracic curves in immature patients would succeed without treatment. For the same group of curves, the success rates after bracing ranged from 49% to 90%. The type of curve alone had no significant effect on the estimates, but the estimates were higher or lower depending on the profile (a statistical interaction of curve size and menarcheal status; P < 0.0001). This interaction is illustrated by the estimates for thoracic curves. The average success estimate for small thoracic curves in premenarcheal patients without treatment was 44.87% compared with 77.22% for small curves in postmenarcheal patients (difference of approximately 22%), whereas the average success estimate for large thoracic curves was 20.39% in premenarcheal patients and 55.85% in postmenarcheal patients (difference of approximately 35%). Figure 2 summarizes these relationships.
TABLE 2.
Summary of Estimates of Success by Curve, Scenario, and Treatment*
| Curve Type | Scenario | Treatment | No. Patients |
Estimates of Success (%) | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Median | Max | ||||
| Thoracic | Premenarcheal, small | Observation | 76 | 44.87 ± 18.97 | 5 | 45 | 80 |
| Bracing | 74 | 70.66 ± 16.05 | 15 | 75 | 95 | ||
| Postmenarcheal, small | Observation | 76 | 77.22 ± 16.56 | 20 | 80 | 95 | |
| Bracing | 74 | 85.65 ± 10.75 | 35 | 90 | 100 | ||
| Premenarcheal, large | Observation | 75 | 20.39 ± 16.66 | 0 | 20 | 85 | |
| Bracing | 73 | 47.95 ± 20.22 | 1 | 50 | 90 | ||
| Postmenarcheal, large | Observation | 75 | 55.85 ± 19.25 | 10 | 50 | 90 | |
| Bracing | 73 | 67.36 ± 17.08 | 10 | 70 | 98 | ||
| Thoracolumbar/Lumbar | Premenarcheal, small | Observation | 76 | 42.99 ± 22.15 | 0 | 40 | 92 |
| Bracing | 72 | 70.96 ± 18.12 | 15 | 75 | 95 | ||
| Postmenarcheal, small | Observation | 76 | 73.29 ± 17.43 | 30 | 80 | 100 | |
| Bracing | 72 | 83.65 ± 12.18 | 50 | 85 | 100 | ||
| Premenarcheal, large | Observation | 76 | 24.92 ± 20.88 | 0 | 20 | 90 | |
| Bracing | 72 | 54.75 ± 19.73 | 5 | 60 | 90 | ||
| Postmenarcheal, large | Observation | 76 | 54.42 ± 21.81 | 1 | 50 | 95 | |
| Bracing | 72 | 69.79 ± 16.60 | 30 | 70 | 95 | ||
| Double major | Premenarcheal, small | Observation | 75 | 44.07 ± 21.73 | 0 | 40 | 90 |
| Bracing | 71 | 66.79 ± 17.70 | 5 | 70 | 95 | ||
| Postmenarcheal, small | Observation | 76 | 73.82 ± 17.28 | 20 | 80 | 100 | |
| Bracing | 72 | 81.53 ± 13.13 | 40 | 85 | 100 | ||
| Premenarcheal, large | Observation | 76 | 24.28 ± 20.85 | 0 | 20 | 100 | |
| Bracing | 72 | 51.49 ± 20.39 | 0 | 50 | 90 | ||
| Postmenarcheal, large | Observation | 76 | 54.69 ± 19.46 | 10 | 50 | 90 | |
| Bracing | 72 | 66.97 ± 16.09 | 20 | 70 | 95 | ||
Success indicates a Cobb angle less than 45 degrees at the end of treatment.
FIGURE 2.
Percentage of successes by profile and treatment.
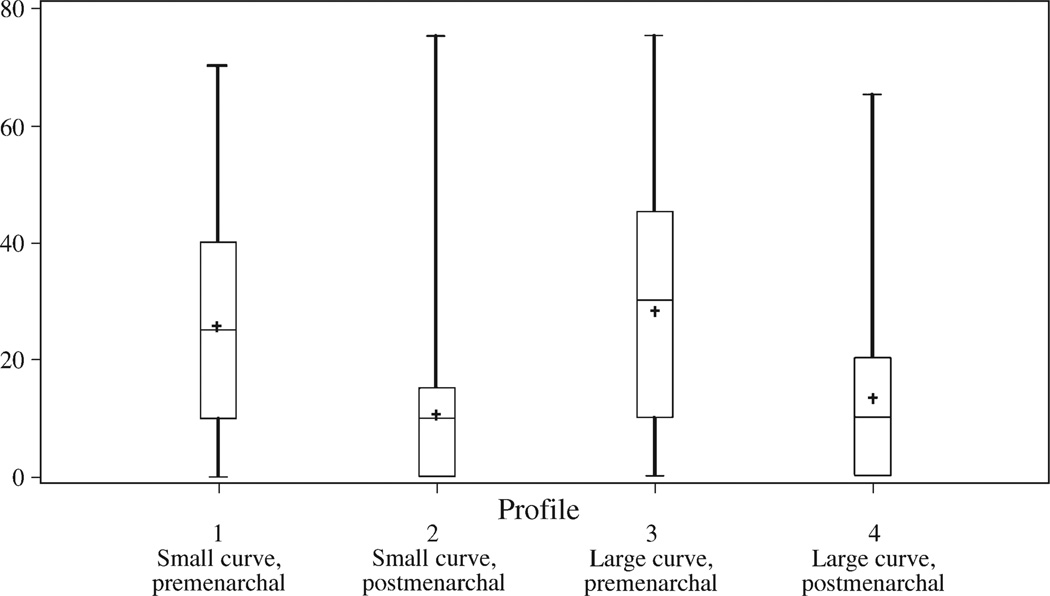
Table 3 summarizes the RR estimates for each clinical profile. The RR estimates were obtained by subtracting the bracing failure rates from the observation failure rates. Like the raw success rate estimates, there was wide variation in the RR estimates. The minimum RR was 0% for all profiles, and the maximum ranged from 55% (small curves in postmenarcheal patients with thoracolumbar/lumbar curves) to 75% (small thoracic curves in postmenarcheal patients and large thoracic curves in premenarcheal patients). Another way to demonstrate the variability between the raters is to look at the median estimates. For example, the median RR for post-menarcheal patients with large thoracic curves was 30%; therefore, one half of the panel thought that the RR due to bracing was 0% to 30%, whereas the other half thought that it was 30% to 75%.
TABLE 3.
Summary of Attributable RR Estimates (Bracing Compared With Observation) by Curve and Scenario
| Attributable RR Estimates (%) | ||||||
|---|---|---|---|---|---|---|
| Curve | Scenario | N | Mean ± SD | Minimum | Median | Maximum |
| Thoracic | Premenarcheal, small | 73 | 26.71 ± 18.59 | 0 | 25 | 70 |
| Postmenarcheal, small | 73 | 10.26 ± 13.83 | 0 | 5 | 75 | |
| Premenarcheal, large | 72 | 28.21 ± 19.37 | 0 | 30 | 75 | |
| Postmenarcheal, large | 72 | 11.92 ± 14.44 | 0 | 10 | 60 | |
| Thoracolumbar/Lumbar | Premenarcheal, small | 71 | 28.21 ± 18.50 | 0 | 25 | 70 |
| Postmenarcheal, small | 71 | 12.15 ± 13.67 | 0 | 10 | 55 | |
| Premenarcheal, large | 71 | 29.27 ± 20.90 | 0 | 30 | 75 | |
| Postmenarcheal, large | 71 | 14.70 ± 15.49 | 0 | 10 | 65 | |
| Double major | Premenarcheal, small | 70 | 22.33 ± 17.74 | 0 | 20 | 60 |
| Postmenarcheal, small | 71 | 10.00 ± 12.45 | 0 | 10 | 60 | |
| Premenarcheal, large | 71 | 26.79 ± 20.07 | 0 | 30 | 65 | |
| Postmenarcheal, large | 71 | 12.96 ± 14.18 | 0 | 10 | 60 | |
The RR estimates did not significantly differ across curve types, but they were significantly different between profiles (P < 0.0001). This is expected considering the interaction observed for the raw success estimates. The interaction suggests that on average, the panel thought that the impact of bracing was dependent on both the curve size and the menarcheal status of the patient. Consistently, however, the RR estimates for premenarcheal patients were greater than those for the postmenarcheal patients. Thus, the panel responses suggest that bracing has a greater positive impact for premenarcheal patients than for postmenarcheal patients. Boxplots summarizing the RR estimates are provided in Figure 3.
FIGURE 3.
Boxplots of RR d/t bracing (%) by profile.
Agreement
We divided the range of RR estimates into 3 intervals: small effect (0%–39% fewer failures with bracing), medium effect (40%–69% fewer failures with bracing), and large effect (70%–100% fewer failures with bracing). Clinical agreement was present if more than 80% of the experts’ estimates were within 1 of the 3 intervals. We evaluated whether there was clinical agreement on the outcomes of each of the 12 profiles.
According to this definition, there was clinical agreement on only 4 of the 12 profiles, all of which proposed a small RR due to bracing in postmenarcheal patients. These agreements are highlighted in Table 4. More than 80% of the experts indicated that bracing would have a small effect on postmenarcheal patients with thoracic curves (for both small and large curves), postmenarcheal patients with small thoracolumbar/lumbar curves, and postmenarcheal patients with small double major curves. The respondents were very close to agreement (77% and 79%) that bracing would have only a small effect on postmenarcheal patients with either large thoracolumbar/lumber curves or double major curves.
TABLE 4.
Attributable RR (Percentage of Responses Within 3 Categories)*
| Scenario/Cobb Angle (degrees) |
Attributable RR (%) | ||
|---|---|---|---|
| 0–39 | 40–69 | 70–100 | |
| Thoracic curve | |||
| Premenarcheal, 25–34 | 47 | 36 | 6 |
| Postmenarcheal, 25–34 | 93 | 4 | 3 |
| Premenarcheal, 35–45 | 47 | 42 | 11 |
| Postmenarcheal, 35–45 | 85 | 7 | 8 |
| Thoracolumbar/Lumbar curve | |||
| Premenarcheal, 25–34 | 45 | 34 | 21 |
| Postmenarcheal, 25–34 | 82 | 7 | 11 |
| Premenarcheal, 35–45 | 45 | 44 | 11 |
| Postmenarcheal, 35–45 | 77 | 17 | 6 |
| Double major curve | |||
| Premenarcheal, 25–34 | 58 | 28 | 14 |
| Postmenarcheal, 25–34 | 90 | 6 | 4 |
| Premenarcheal, 35–45 | 48 | 22 | 30 |
| Postmenarcheal, 35–45 | 79 | 17 | 4 |
Bold font indicates estimates greater than 80% within a single category.
DISCUSSION
This study used the experts’ opinion of radiographic outcomes to estimate the surgical rates after observation and bracing for cases of AIS. These rates varied widely within the panel for both treatments, as did the consequent RR due to bracing. The reported RR ratios indicate a wide spectrum of opinion, from substantial benefit from brace use to no benefit at all. Agreement, defined as greater than 80% endorsement, existed in about one third of the profiles. These data demonstrate significant uncertainty within this expert group concerning the outcomes of observation and bracing. Consequently, we think that there is evidence of community equipoise for most clinical profiles contained in this survey and that the equipoise requirement for an ethical randomized trial has been met.
The method of expert group input has been widely used in other health research applications, including technology assessment, education and training, priorities and information, and development of clinical practice.28 The design used here allowed a panel of geographically dispersed experts to be surveyed efficiently and confidentially.29 All clinicians reviewed exactly the same material, with no uncertainty concerning Cobb angle measurement or other evaluations that might occur in actual practice. In addition, because these estimates reflect the initial clinical judgments in the absence of knowledge of the estimates of other clinicians, they provide an indication of the extent of interclinician variation that might occur in actual practice. Some might argue that the contrived situation of this research design does not reflect clinical practice. However, would the outcomes be any less variable if it was a parent, rather than a researcher, asking “Of children like mine, how many will need surgery without treatment? How many will need surgery after treatment?” It seems very unlikely that the results of this exercise overestimate the extent of interclinician variation in predicting the effectiveness of bracing in this population.
Several recent articles have reported on the clinical agreement concerning the indications and the outcomes of medical treatment for other purposes in addition to clinical trial planning.24–26,30,31 Two of these papers involve orthopaedics and each defined agreement similarly to this paper. Wright et al24 demonstrated disagreement similar to that shown in this article in their survey concerning the indications and the outcomes of total knee replacement. For example, their respondents indicated that anywhere from 1% to 95% of patients would require a revision within 10 years of their primary replacement. Dunn et al25 also found a significant variation in decision making and a lack of clinical agreement concerning the indications for rotator cuff surgery.
To our knowledge, there have been only 3 published reports measuring community equipoise to specifically assess the ethics and the feasibility of conducting randomized clinical trials. Young et al32 mailed surveys to all members of a vascular surgery professional organization and asked the members to rate several common clinical scenarios describing 2 alternative treatments for the same condition. The respondents showed great variability in their responses, and each treatment was endorsed to some degree in all of the scenarios. There were only 1 in 6 scenarios where more than 70% of the respondents agreed that the same treatment was preferable. The authors conclude that this variation indicates equipoise within the membership and, therefore, that randomized clinical trials would be ethically justified. Lilford27 surveyed the expectations of a 10-member expert panel concerning the probable relative risk of morbidity resulting from immediate or delayed delivery in scenarios involving at-risk fetuses. For each scenario the average result was no relative RR, but the range in estimates for each scenarios was large. In 1 scenario, the estimates ranged from a 75% decrease to a 25% increase in the risk to a fetus delivered early. Lambert et al33 investigated the perceptions of the parents and the members of the Pediatric Ophthalmology and Strabismus Society concerning the treatment for infants with congenital cataracts. On a scale ranging from 1 to 10, with 1 strongly favoring an intraocular implant and 10 strongly favoring a contact lens, the median score of the respondents was 7.5. This range of opinions also manifested itself as a support for randomized controlled trials because 61% of the respondents indicated that they would be willing to randomize children to one of these 2 treatments.
These studies indicate that clinical disagreement is a reality across specialties and interventions. Three possible explanations for clinical disagreement demonstrated by studies such as these include the limitations of available knowledge, the controversy within the research literature, and the inadequate dissemination or adoption of available information.24 A recent article by the SRS Bracing Committee34 addresses these issues by calling for completeness and uniformity in the subjects, endpoints, and outcomes of bracing studies to maximize the likelihood of developing a coherent, accepted body of knowledge concerning this disease. If future articles adopt this approach, disagreements may diminish.
It has been suggested that progression to surgery indicates the ultimate failure of bracing treatment.1 The key question of any future study of bracing, randomized or not, must be “How many patients avoided surgery because of bracing treatment?” This study found a high degree of variability in opinion among experts concerning the effectiveness of bracing. Yet, bracing is the standard of care for AIS, and all 362 respondents to a recent survey from the SRS35 indicated that they advocate its use. This implies a major disconnect between opinions of effectiveness and endorsement of bracing by the community. Patients considering their treatment options need to be aware of this disconnect; instead of considering bracing as the only option, they should take this variation into account along with their personal goals and tolerance for risk. In addition, these results indicate that a randomized trial of bracing would not only be ethical but also necessary.
FIGURE 1.
Examples of survey. A, Estimates of observation outcomes. B, Estimates of bracing outcomes.
Acknowledgments
Supported by a National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases Clinical Trials Planning grant (S.L.W.) and by the Children’s Miracle Network (S.L.W.).
Footnotes
This study was performed at the Department of Orthopaedics and Rehabilitation, University of Iowa Health Care, Iowa City, IA.
REFERENCES
- 1.Gavin TM, Bunch WH, Patwardhan AG, et al. Orthotic treatment for spinal disorders. In: Weinstein SL, editor. The Pediatric Spine: Principles and Practice. 2nd ed. New York, NY: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 2.Fernandez-Feliberti R, Flynn J, Ramirez N, et al. Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr Orthop. 1995;15:176–181. [PubMed] [Google Scholar]
- 3.Miller JA, Nachemson AL, Schultz AB. Effectiveness of braces in mild idiopathic scoliosis. Spine. 1984;9:632–635. doi: 10.1097/00007632-198409000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg CJ, Moore DP, Fogarty EE, et al. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine. 2001;26:42–47. doi: 10.1097/00007632-200101010-00009. [see comment]. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein SL, Dolan LA, Morcuende JA. BrAIST: The Bracing in Adolescent Idiopathic Scoliosis Trial. University of Iowa: 2005. [Google Scholar]
- 6.Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987;317:141–145. doi: 10.1056/NEJM198707163170304. [DOI] [PubMed] [Google Scholar]
- 7.Alderson P. Equipoise as a means of managing uncertainty: personal, communal and proxy. J Med Ethics. 1996;22:135–139. doi: 10.1136/jme.22.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lilford RJ, Jackson J. Equipoise and the ethics of randomization. J R Soc Med. 1995;88:552–559. [PMC free article] [PubMed] [Google Scholar]
- 9.Bunnell WP. The natural history of idiopathic scoliosis before skeletal maturity. Spine. 1986;11:773. doi: 10.1097/00007632-198610000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Allington NJ, Bowen JR. Adolescent idiopathic scoliosis: treatment with the Wilmington brace. A comparison of full-time and part-time use. J Bone Joint Surg Am. 1996;78:1056–1062. [PubMed] [Google Scholar]
- 11.Emans J, Kaelin A, Bancel P, et al. The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine. 1986;11:792–801. doi: 10.1097/00007632-198610000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Howard A, Wright JG, Hedden D. A comparative study of TLSO, Charleston, and Milwaukee braces for idiopathic scoliosis. Spine. 1998;23:2404–2411. doi: 10.1097/00007632-199811150-00009. [DOI] [PubMed] [Google Scholar]
- 13.Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine. 2001;26:2001–2005. doi: 10.1097/00007632-200109150-00013. [DOI] [PubMed] [Google Scholar]
- 14.Katz DE, Richards BS, Browne RH, et al. A comparison between the Boston brace and the Charleston bending brace in adolescent idiopathic scoliosis. Spine. 1997;22:1302–1312. doi: 10.1097/00007632-199706150-00005. [DOI] [PubMed] [Google Scholar]
- 15.Katz DE, Durrani AA. Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine. 2001;26:2354–2361. doi: 10.1097/00007632-200111010-00012. [DOI] [PubMed] [Google Scholar]
- 16.Korovessis P, Kyrkos C, Piperos G, et al. Effects of thoracolumbosacral orthosis on spinal deformities, trunk asymmetry, and frontal lower rib cage in adolescent idiopathic scoliosis. Spine. 2000;25:2064–2071. doi: 10.1097/00007632-200008150-00010. [DOI] [PubMed] [Google Scholar]
- 17.Little DG, Song KM, Katz D, et al. Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls. J Bone Joint Surg. 2000;82-A:685–693. doi: 10.2106/00004623-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Piazza MR, Bassett GS. Curve progression after treatment with the Wilmington brace for idiopathic scoliosis. J Pediatr Orthop. 1990;10:39–43. [PubMed] [Google Scholar]
- 19.Spoonamore MJ, Dolan LA, Weinstein SL. Use of the Rosenberger brace in the treatment of progressive adolescent idiopathic scoliosis. Spine. 2004;29:1458–1464. doi: 10.1097/01.brs.0000128756.89367.9e. [DOI] [PubMed] [Google Scholar]
- 20.Upadhyay SS, Nelson IW, Ho EK, et al. New prognostic factors to predict the final outcome of brace treatment in adolescent idiopathic scoliosis. Spine. 1995;20:537–545. doi: 10.1097/00007632-199503010-00006. [DOI] [PubMed] [Google Scholar]
- 21.Weiss HR. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine. 2001;26:2058–2059. doi: 10.1097/00007632-200109150-00024. [DOI] [PubMed] [Google Scholar]
- 22.Wiley JW, Thomson JD, Mitchell TM, et al. Effectiveness of the Boston brace in treatment of large curves in adolescent idiopathic scoliosis. Spine. 2000;25:2326–2332. doi: 10.1097/00007632-200009150-00010. [DOI] [PubMed] [Google Scholar]
- 23.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg. 1983;65-A:447–455. [PubMed] [Google Scholar]
- 24.Wright JG, Coyte P, Hawker G, et al. Variation in orthopaedic surgeons’ perceptions of the indications for and outcomes of knee replacement. CMAJ. 1995;152:687–697. [PMC free article] [PubMed] [Google Scholar]
- 25.Dunn WR, Schackman BR, Walsh C, et al. Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am. 2005;87-A:1978–1984. doi: 10.2106/JBJS.D.02944. [DOI] [PubMed] [Google Scholar]
- 26.Latthe PM, Braunholtz DA, Hills RK, et al. Measurement of beliefs about effectiveness of laparoscopic uterosacral nerve ablation. BJOG. 2005;112:243–246. doi: 10.1111/j.1471-0528.2004.00304.x. [DOI] [PubMed] [Google Scholar]
- 27.Lilford R. The Fetal Compromise Group. Formal measurement of clinical uncertainty: prelude to a trial in perinatal medicine. BMJ. 1994;308:111–112. doi: 10.1136/bmj.308.6921.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scott EA, Black N. When does consensus exist in expert panels? J Public Health Med. 1991;13:35–39. doi: 10.1093/oxfordjournals.pubmed.a042575. [DOI] [PubMed] [Google Scholar]
- 30.Jacka MJ, Cohen MM, To T, et al. The appropriateness of the pulmonary artery catheter in cardiovascular surgery. Can J Anaesth. 2002;49:276–282. doi: 10.1007/BF03020527. [DOI] [PubMed] [Google Scholar]
- 31.Moore K, Bokey L, Chapuis P, et al. Clinician opinion on the management of patients with hepatic colorectal metastases. J Gastroenterol Hepatol. 2001;16:1120–1124. doi: 10.1046/j.1440-1746.2001.02550.x. [DOI] [PubMed] [Google Scholar]
- 32.Young J, Harrison J, White G, et al. Developing measures of surgeons’ equipoise to assess the feasibility of randomized controlled trials in vascular surgery. Surgery. 2004;136:1070–1076. doi: 10.1016/j.surg.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 33.Lambert SR, Lynn M, Drews-Botsch C, et al. Intraocular lens implantation during infancy: perceptions of parents and the American Association for Pediatric Ophthalmology and Strabismus members. J AAPOS. 2003;7:400–405. doi: 10.1016/j.jaapos.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Richards BS, Bernstein RM, D’Amato CR, et al. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30:2068–2075. doi: 10.1097/01.brs.0000178819.90239.d0. discussion 2076–2067. [DOI] [PubMed] [Google Scholar]
- 35.Scoliosis Research Society. Bracing Survey Responses. 2001 [Google Scholar]