ABSTRACT
Objective:
To determine physicians' knowledge of cardiopulmonary resuscitation (CPR) guidelines at the University Hospital of the West Indies (UHWI), Jamaica, and their current certification status in basic life support (BLS), advanced cardiac life support (ACLS), paediatric advanced life support (PALS) and advanced trauma life support (ATLS).
Methods:
This was a cross-sectional study. A 23-item self-administered questionnaire was used to assess physicians practising at the UHWI, from the Departments of Anaesthesia, Surgery, Internal Medicine, Accident and Emergency, Obstetrics and Gynaecology, and Oncology.
Results:
One hundred and forty-three (65%) of the targeted 220 physicians responded. There were 77 (55%) females and 41% of respondents were between ages 26 and 30 years. Knowledge of CPR guidelines was inadequate, as the median score obtained was 4.0 (interquartile range [IQR] 2-5) out of a possible eight. Physician seniority was inversely related to knowledge scores (p < 0.01). While 86% of all respondent physicians had been trained in BLS, only 46% were certified at the time of the study. Fewer (52%) were trained in ACLS with only 36% currently certified. Only 65% had been trained in the use of a defibrillator. Most knew the correct compression rate (78%), but only 46% knew the compressions to breaths ratio for both single and two-rescuer CPR. Only 42% of anaesthetists and 27% of emergency physicians were currently ACLS certified.
Conclusion:
Physician knowledge of CPR protocols was suboptimal and current certification levels were low. Increased training and recertification is necessary to improve physician knowledge which is expected to result in improved performance of CPR.
Keywords: Cardiopulmonary resuscitation (CPR) certification, CPR knowledge, CPR training
RESUMEN
Objetivo:
Determinar el conocimiento de las directrices para la resucitación cardiopulmonar (RCP) en el Hospital Universitario de West Indies (HUWI), Jamaica, y su estado actual de certificación en cuanto a soporte vital básico (SVB), soporte vital cardiovascular avanzado (SVCA), soporte vital pediátrico avanzado (SVPA), y soporte vital avanzado en trauma (SVAT).
Métodos:
Se trató de un estudio transversal. Se utilizó un cuestionario auto-administrado de 23 ítems para evaluar a los médicos que ejercen en el HUWI, en los departamentos de Anestesia, Cirugía, Medicina Interna, Accidentes y Emergencias, Obstetricia y Ginecología y Oncología.
Resultados:
Ciento cuarenta y tres (65%) de los 220 médicos encuestados respondieron. Hubo 77 mujeres (55%) y 41% de los encuestados tenían entre 26 y 30 años. El conocimiento de las directrices para la RCP era insuficiente, ya que la puntuación media obtenida fue 4.0 (rango intercuartílico [IQR] 2-5) de un ocho posible. La antigüedad de los médicos fue inversamente proporcional a las puntuaciones de su conocimiento (p < 0.01). Aunque el 86% de todos los médicos encuestados había recibido entrenamiento en SVB, sólo el 46% habían sido certificado en el momento del estudio. Un número aún menor (52%) estaba entrenado en SVCA, siendo el caso que sólo el 36% poseía certificación. Sólo el 65% habían sido entrenados en el uso del desfibrilador. La mayoría conocía la tasa de compresión correcta (78%), pero sólo el 46% conocía la relación compresión:respiración para la RCP tanto para uno como para dos socorristas. Sólo el 42% de los anestesistas y el 27% de los médicos de urgencias poseían certificaciones actualizadas para SVCA.
Conclusión
El conocimiento médico de los protocolos de RCP distaba de ser óptimo, y los niveles de certificación corriente eran bajos. Se necesita aumentar el adiestramiento y la recertificación a fin de mejorar el conocimiento médico, de modo que se obtengan mejores resultados rendimientos con la RCP.
INTRODUCTION
Cardiopulmonary resuscitation (CPR) is performed on victims of cardiac and/or respiratory arrest to maintain flow of oxygenated blood to vital organs (1). This procedure aims to delay tissue death and extend the brief window of opportunity for successful resuscitation without permanent brain damage. It is a fundamental principle of CPR that it should be initiated as soon as possible and hence requires as many trained medical personnel as possible to increase the chance of a rapid response. Although cardiac arrests tend to be more common in particular areas of the hospital, such as the emergency department and the intensive care unit, they may occur on any ward and it is important that the first responders to such an emergency are trained to appropriately manage the situation until expert help arrives. Most hospitals in the United States of America (USA) require either basic life support (BLS) or advanced cardiac life support (ACLS) certification for all their healthcare providers (2).
Success rates of CPR attempts vary widely, with better outcomes seen with in-hospital cardiac arrest and ventricular arrhythmias as the initial cardiac rhythm compared to pulseless electrical activity (PEA) and asystole (3). For in-hospital CPR, a meta-analysis done by Ebell et al reported an immediate survival rate for all adult inpatients of 40% and survival to discharge rate of only 13% (4). Pooled data from four large studies on arrest survival in North America and Europe showed an inpatient survival rate of 17.6% and 6.4% for outpatients (3). A large study of over 84 000 patients from 374 hospitals in the USA with in-hospital cardiac arrest showed that risk adjusted rates of survival to discharge increased from 13.7% in 2000 to 22.3% in 2009 (5).
Recent studies have shown that resuscitation skills by medical personnel are often poor and this may be related to inadequate training and updating (6, 7). In 2002, a study conducted in the United Kingdom reported that 49% of junior doctors participating in a cardiac arrest team had not had ACLS training even though most would have liked to have done so (8). Even when training has been undertaken, it has been shown that the skills acquired decrease within six to twelve months, especially if not used frequently (6, 9, 10). At the University Hospital of the West Indies (UHWI), a survey done between 1991 and 1995 found that only 31% of physicians interviewed knew the ACLS current guidelines (unpublished data).
The Medical Council of Jamaica, at present, does not require certification in resuscitation for practising healthcare workers. In this study, we sought to assess the knowledge of physicians of the ACLS protocols published in 2005, which were the current guidelines at the time of the study. We also determined the level of training and current certification in BLS, ACLS, advanced trauma life support (ATLS) and paediatric advanced cardiac life support (PALS).
SUBJECTS AND METHODS
A single-centre, cross-sectional study was conducted at the UHWI, Kingston, Jamaica, between March 2010 and January 2011. This is a 453-bed urban teaching hospital affiliated to the University of the West Indies. Eligible physicians included all levels of staff (intern to consultant) from anaesthesia, intensive care, internal medicine, surgery, obstetrics, gynaecology, emergency medicine and oncology. Physicians were identified from monthly departmental rotas and a total of 220 doctors fit the inclusion criteria.
A 23-item, self-administered questionnaire was used. A pre-test of the physicians' questionnaire involving thirty physicians was done at the Bustamante Hospital for Children to evaluate the questions for ambiguity. Full confidentiality was maintained and approval for the study obtained from the University Hospital of the West Indies/University of the West Indies/Faculty of Medical Science Ethics Committee. Physician demographics (age, gender, staffing level and speciality) were collected. Eight multiple choice questions were used to assess physicians' knowledge of the current (2005) CPR guidelines. A numerical value of one was given for a correct response and zero for an incorrect response. Respondents could achieve a maximum score of eight. Information regarding previous training in CPR and current certification was also solicited.
Data were entered in Microsoft Excel and analysed using SPSS version 16.0 software. Statistical significance was assessed by the Chi-squared test and a p-value of less than 0.05 was considered significant.
RESULTS
Of the 220 physicians targeted, 154 responded and 143 correctly completed the questionnaire; a valid response rate of 65%. There were 77 (55%) females and 41% of respondents were between 26 and 30 years. Forty-one per cent of respondents were surgeons, 18% were anaesthetists, 15% internists, 11% emergency physicians, 10% obstetricians and gynaecologists and 5% oncologists. Residents accounted for 62% of respondents, house officers 24% and consultants 14%.
Physicians' knowledge of CPR guidelines
Out of a total score of eight, the median score was 4.0 (interquartile range [IQR] 2-5) and the modal score was 2.0 (23%). The highest score obtained was seven, achieved by three (2%) physicians. A score of four and above was achieved by 55% of respondents. Speciality was not significantly correlated with knowledge scores obtained (p = 0.487), but 72% of anaesthetists, and 69% of emergency physicians scored ≥ 4. The median score for emergency physicians was 5.0 (IQR 3.0-5.5), anaesthetists 4.0 (IQR 3.0-4.3), internists 3.6 (IQR 3.0-4.8), surgeons 3.5 (IQR 2.0-5.0) and obstetricians/gynaecologists 2.5 (IQR 1.8-5.0). Physician staffing level was inversely related to knowledge scores (p < 0.01). It was found that 83% of interns achieved a knowledge score of four or more, compared to only 25% of consultants and 17% of chief residents. The highest number of correct responses was obtained for the questions on chest compressions rate (77%), importance of compressions with respect to ventilation (54%), and whether or not chest compressions should continue without breaks after securing an advanced airway [52%] (Table 1).
Table 1. Number and proportion of correct responses for knowledge based questions by physicians.
| Knowledge questions | Correct responses (n/%) |
|---|---|
| Rate of chest compressions | 108 (77.7%) |
| New compressions-to-breaths ratio | 64 (46%) |
| Importance of compressions vs ventilation | 75 (54%) |
| Number of shocks to be delivered in VF/VT | 58 (41.7%) |
| Starting energy level for monophasic defibrillators | 27 (19.6%) |
| Timing of securing an advanced airway | 62 (44.6%) |
| Chest compression to breaths ratio after securing advanced airway | 70 (51.5%) |
| Recommended duration of CPR if no response obtained | 61 (43.3%) |
VF/VT: ventricular fibrillation and/or ventricular tachycardia, CPR: cardiopulmonary resuscitation
Only 46% of physicians knew the new compressions to breath ratio for both single and two-rescuer CPR, 20% knew the correct energy level for defibrillation and 42% were aware that only one shock was indicated.
Physician training
Approximately 86% of all respondents indicated that they had training in BLS, 52% in ACLS, 39% in ATLS and only 12% in PALS. Certification was current in only 46% of physicians for BLS, 36% for ACLS, 21% for ATLS and 7% for PALS. Surgeons showed the greatest level of training and current certification (Tables 2 and 3), while only 42% of anaesthetists and 27% of emergency physicians were currently ACLS certified. Recertification rates, which assessed the number of previously trained physicians who were currently certified, were 56% for BLS and 74% for ACLS.
Table 2. Physician training, current certification and recertification rates in basic life support (BLS) by specialty.
| Speciality | Certification | ||
|---|---|---|---|
| BLS trained | BLS current | BLS recertification | |
| Anaesthesia | 17 (68%) | 11 (44%) | 65% |
| Emergency medicine | 12 (80%) | 5 (33%) | 42% |
| Internal medicine | 16 (76%) | 7 (33%) | 44% |
| Obstetrics/gynaecology | 14 (100%) | 5 (36%) | 36% |
| Surgery | 48 (83%) | 31 (53%) | 65% |
| Haematology/oncology | 5 (71%) | 4 (57%) | 80% |
Table 3. Physician training, current certification and recertification rates in advanced cardiac life support (ACLS) by specialty.
| Speciality | Certification | ||
|---|---|---|---|
| ACLS trained | ACLS current | ACLS recertification | |
| Anaesthesia | 11 (44%) | 10 (40%) | 91% |
| Emergency medicine | 5 (33%) | 4 (27%) | 80% |
| Internal medicine | 11 (52%) | 6 (29%) | 55% |
| Obstetrics/gynaecology | 6 (46%) | 2 (14%) | 33% |
| Surgery | 34 (59%) | 27 (47%) | 79% |
| Haematology/oncology | 1 (14%) | 1 (14%) | 100% |
Approximately 62% of physicians knew where the nearest defibrillator was located and 65% stated they had been trained in its use. No correlation was found between defibrillator training and speciality (p = 0.123) or staffing level (p = 0.329).
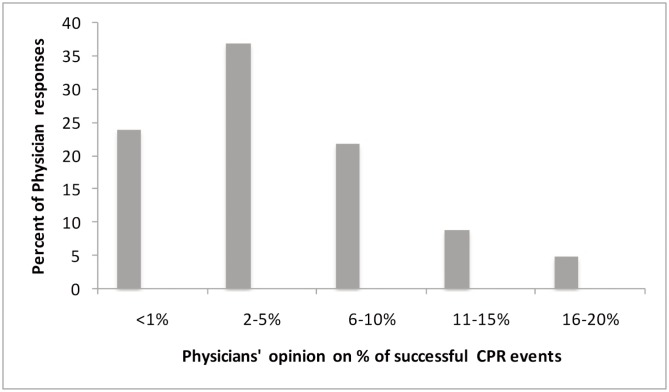
Approximately 92% of physicians surveyed indicated that they had been involved in a resuscitation attempt where spontaneous return of circulation occurred initially. However, 37% thought only between 2% and 5% of all their resuscitation attempts had been successful and 24% thought CPR was effective < 1% of the time in their experience (Figure).
Figure. Physicians' perception of percentage of patients they had successfully resuscitated.
DISCUSSION
The knowledge of physicians at the UHWI of 2005 CPR guidelines (which were the current guidelines at the time of data collection) was inadequate, with just over half (55%) giving correct responses for four or more of eight questions. In addition, current certification was very poor, below 50% of all respondents for all protocols combined. This would suggest that at any given resuscitation attempt, there is a significant possibility that none of the physicians present would have received training in current life support algorithms. This was reflected in the high number of incorrect responses to the questions regarding current CPR guidelines. However, there was a discrepancy between the levels of knowledge demonstrated by anaesthetists and emergency physicians, which were the highest of all specialities, and their poor training rates. This could suggest that the doctors with the most contact with patients needing resuscitation may rely on clinical training on the job and hence not seek formal instruction and certification. It is interesting to note that the recertification rate was greater than 50%, suggesting that training engenders a desire to remain up to date with the current practice.
The results for certification in PALS needs to be viewed in light of the fact that not all the physicians who participated in the study would be regularly involved in the care of paediatric patients and hence would not consider it necessary. Those for whom PALS is relevant would include physicians in emergency care (n = 15) and anaesthesia (n = 25). Using this total number as the denominator (n = 40), PALS certification would be 43% trained, 59% of whom have remained current, which is similar to the other protocols.
There may be several reasons why our study population as a whole performed so poorly. There has not been a significant focus on CPR training outside of the need for continuing medical education credits (CME) for annual registration with the national medical council. Cardio-pulmonary resuscitation training can be quite costly, though there are now subsidized courses provided in Jamaica through the Ministry of Health. However, spaces are limited. Additionally, many physicians may feel that CPR training is not as important compared to other academic interests, for example, attending a surgical specialist workshop. Also, there is a significantly greater time commitment that has to be made to CPR training as compared with other seminars and courses.
Studies have shown the erosion of skills and knowledge with time and suggest a need for regular updates. Stross found a difference in knowledge between physicians who received interventions designed to provide reinforcement of previously mastered knowledge and skills and those who did not. Of those who had not received interventions, knowledge scores were approximately 52% compared to > 75% for those who had (11). This attrition of knowledge may also have contributed to the poor performance of our res-pondents, as most of them had never received training or were not currently certified. This would have meant that the last course attended would have been greater than two years previously.
Our findings revealed that physicians in emergency medicine and anaesthesia achieved the highest mean scores. This is most likely because these are the specialities that teach resuscitation and are most involved in actual resuscitation attempts. Consultants and chief residents were not as well informed about new CPR guidelines compared to more junior staff. This may be explained by the fact that the more junior staff would have been more likely to have had training in the most recent guidelines, while the more senior staff would need to attend refresher courses to remain current. In addition, the junior staff is usually the first call person and responsible for carrying out the majority of acute emergencies which may require resuscitation. Training, and frequent refresher courses, with financial subsidies to encourage participation, are needed to improve the knowledge base of all physicians in the future.
Physician's perception of the success rate of CPR in the resuscitations they had been involved in (2-5%) was less than international studies would suggest (18-40%) but more in keeping with local data. A prospective study of 200 cardiopulmonary arrests at the UHWI in 1986 reported an initial success rate of 18%, but only 7% of survivors were discharged from hospital (12).
The main limitation of this study was that a self-administered questionnaire was used and there might have been incorrect responses due to misunderstanding of questions.
CONCLUSIONS
Physician knowledge of CPR protocols was inadequate and current certification rates poor. Increased training and recertification is necessary to improve physician knowledge which is expected to result in improved performance of CPR performed within the hospital. We recommend that all medical staff at the UHWI should be certified in at least ACLS with regular recertification; it was noted in this study, from responses to questions regarding their opinion on CPR effectiveness, that all had been involved in at least one resuscitation event. Greater subsidy for CPR training and time allowed from work for the two-day training exercise are also needed to promote compliance. Further study to determine physicians' perception of the importance of CPR training and maintaining current certification, as well as barriers (and facilitators) to training is recommended.
REFERENCES
- 1.Eisenberg MS, Mengert TJ. Cardiac resuscitation. N Engl J Med. 2001;344:1304–1313. doi: 10.1056/NEJM200104263441707. [DOI] [PubMed] [Google Scholar]
- 2.Sutton RM, Nadkarni V, Abella BS. “Putting it all together” to improve resuscitation quality. Emerg Med Clin North Am. 2012;30:105–122. doi: 10.1016/j.emc.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper JA, Cooper JD, Cooper JM. Cardiopulmonary resuscitation: history, current practice, and future direction. Circulation. 2006;114:2839–2849. doi: 10.1161/CIRCULATIONAHA.106.610907. [DOI] [PubMed] [Google Scholar]
- 4.Ebell MH, Becker LA, Barry HC, Hagen M. Survival after in-hospital cardiopulmonary resuscitation. A meta-analysis. J Gen Intern Med. 1998;13:805–816. doi: 10.1046/j.1525-1497.1998.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang CW, Yen ZS, McGowan JE, Chen HC, Chiang WC, Mancini ME, et al. A systematic review of retention of adult advanced life support knowledge and skills in healthcare providers. Resuscitation. 2012;83:1055–1060. doi: 10.1016/j.resuscitation.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 7.Broomfield R. A quasi-experimental research to investigate the retention of basic cardiopulmonary resuscitation skills and knowledge by qualified nurses following a course in professional development. J Adv Nurs. 1996;23:1016–1023. doi: 10.1111/j.1365-2648.1996.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 8.Morgan R, Westmoreland C. Survey of junior hospital doctors' attitudes to cardiopulmonary resuscitation. Postgrad Med J. 2002;78:413–415. doi: 10.1136/pmj.78.921.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith KK, Gilcreast D, Pierce K. Evaluation of staff's retention of ACLS and BLS skills. Resuscitation. 2008;78:59–65. doi: 10.1016/j.resuscitation.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Pantazopoulos I, Aggelina A, Barouxis D, Papapanagiotou P, Troupis G, Kotsiomitis E, et al. Cardiologists' knowledge of the 2005 American Heart Association Resuscitation Guidelines: the Athens Study. Heart Lung. 2011;40:278–284. doi: 10.1016/j.hrtlng.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 11.Stross JK. Maintaining competency in advanced cardiac life support skills. JAMA. 1983;249:3339–3341. [PubMed] [Google Scholar]
- 12.Ballin NC. A prospective study of 200 cardiopulmonary arrests at the University Hospital of the West Indies. West Indian Med J. 1986;35:88–91. [PubMed] [Google Scholar]