Abstract
IMPORTANCE
Tadalafil is used to treat erectile dysfunction after prostate cancer treatment, but its role as a preventive agent is undefined.
OBJECTIVES
To determine primarily whether tadalafil preserved erectile function in men treated with radiotherapy for prostate cancer, and secondarily to determine whether participant- or partner-reported overall sexual function and sexual and marital satisfaction were affected.
DESIGN, SETTING, AND PARTICIPANTS
Stratified, placebo-controlled, double-blind, parallel-group study with 1:1 randomization at 76 community-based and tertiary medical sites in the United States and Canada. Two hundred forty-two participants with intact erectile function scheduled to receive radiotherapy for prostate cancer were recruited between November 2009 and February 2012 with follow-up through March 2013.
INTERVENTIONS
One hundred twenty-one participants were assigned 5 mg of tadalafil daily and 121 were assigned placebo for 24 weeks starting with external radiotherapy (63%) or brachytherapy (37%). Participant-reported International Index of Erectile Function response before radiotherapy and at weeks 2 and 4, between weeks 20 and 24, between weeks 28 and 30, and 1 year thereafter. Participants and partners could respond also to the Sexual Adjustment Questionnaire and to the Locke Marital Adjustment Test before radiotherapy, between weeks 20 and 24 and weeks 28 and 30, and at 1 year.
MAIN OUTCOMES AND MEASURES
Primary outcome was off-drug spontaneous erectile function 28 to 30 weeks after radiotherapy started. Secondary end points were spontaneous erection at 1 year; overall sexual function and satisfaction; marital adjustment; and partner-reported satisfaction and marital adjustment at 28 to 30 weeks and 1 year, predictors of tadalafil response; and adverse events.
RESULTS
Among 221 evaluable participants, 80 (79%; 95% CI, 70%–88%) assigned to receive tadalafil retained erectile function between weeks 28 and 30 compared with 61 (74%; 95% CI, 63%–85%) assigned to receive placebo (P = .49); an absolute difference of 5% (95% CI, −9% to 19%). A significant difference was also not observed at 1 year (72%; 95% CI, 60%–84% vs 71%; 95% CI, 59%–84%; P = .93). Tadalafil was not associated with significantly improved overall sexual function or satisfaction; a significant difference was not observed in any domain subscale. Partners of men assigned tadalafil noted no significant effect on sexual satisfaction, and marital adjustment was not significantly improved in participants or partners.
CONCLUSIONS AND RELEVANCE
Amongmen undergoing radiotherapy for prostate cancer, daily use of tadalafil compared with placebo did not result in improved erectile function. These findings do not support daily use of tadalafil to prevent erectile dysfunction in these patients.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT00931528
Erectile dysfunction (ED) is a common condition with many causes, including adverse consequencesof prostate cancer treatment.1,2 Forty percent of men report ED after radiotherapy,2 and half of all men use erectile aids thereafter.2 These men may achieve erection with on-demand phosphodiesterase-5 inhibitors,3 but spontaneous erection is not restored and treatment efficacy may wane over time. This may result in patient dissatisfaction with prostate cancer therapy and a decline in psychosocial function among patients and their partners.4
Although the cause of ED after radiotherapy is not understood fully, penile endothelial dysfunction with cavernosal hypoxia and fibrosis is the likely mechanism. The regularly scheduled administration of a phosphodiesterase-5 inhibitor reduces endothelial dysfunction and improves cavernosal vasodilatation and erectile function in a general population of men with ED compared with an episodic on-demand schedule.5,6 Most men report satisfaction with improved erectile function and relationship with partner using tadalafil,7 with this agent comparing favorably with other phosphodiesterase-5 inhibitor medications.7–9 Tadalafil also has unique pharmacokinetic properties well-suited to once-daily dosing, resulting in steady-state exposure of endothelial and erectile tissues to this agent.
We conducted a placebo-controlled, double-blinded, parallel-group study in this context to determine whether tadalafil maintains spontaneous erectile function in men treated with radiotherapy for prostate cancer.
Methods
Participants
Men 18 years or older with clinical stage II (T1b–T2bN0M0)10 prostate adenocarcinoma were eligible if the Gleason score was less than 7 and the serum prostate-specific antigen (PSA) level was less than 20 ng/mL, or if the Gleason score was 7 or higher and the PSA was less than 15 ng/mL. Additional criteria were an ability to achieve erection at least half the time (International Index of Erectile Function11 question 1 response of 3–5), Zubrod Performance Status score less than 2 (0, no physical limitations; 1, unable to perform strenuous activity), serum testosterone within normal limits, and no prior bilateral orchi-ectomy, chemotherapy, external radiotherapy, brachytherapy, surgical, or other ablative therapy for prostate cancer. Patients with another invasive cancer, other than localized basal or squamous cell skin carcinoma, or with a hematological malignancy were not eligible, unless continually free of this other cancer for at least 5 years. Criteria for exclusion also included prostate cancer spread to lymph nodes or metastatic sites, myocardial infarction within the past year, heart failure or stroke within the past 6 months, uncontrolled cardiac arrhythmia or hypertension, hypotension, moderate or severe renal or hepatic insufficiency, AIDS, genital abnormalities precluding intercourse, prior penile implantation, ongoing erectile aid use, or use of nitrate or cytochrome P450-3A4 inhibitor medications. Androgen suppression within the past 6 months or as part of protocol-specified radiotherapy or brachytherapy was not allowed.
After institutional review board approval at each center, participants were recruited by practitioners at 76 community-based and tertiary medical site members in the United States and Canada. Membership was established and maintained through a quality-control system compliant with National Cancer Institute (NCI) guidelines. Before study entry, evaluation required history (including medication record) and physical (including digital rectal) examination, serum PSA and testosterone measurements, and assessment of Zubrod Performance Status score. All participants provided written informed consent before trial registration and were to receive protocol-specified care and follow-up at a member site. Written informed consent also was required for optional participation in the additional quality-of-life study. Participants did not receive compensation for joining the study, and no commercial support was provided to the participant or member site.
Study Design
This was a multicenter, stratified, placebo-controlled, double-blind, parallel-group study with 1:1 randomization. After pre-treatment evaluation was completed and eligibility met, participants were stratified according to type of radiotherapy (external vs brachytherapy) intended and age (≤65 years vs >65 years). Participants were then randomly assigned to receive either tadalafil or placebo with a permuted-block method12 to balance treatment allocation.
Treatment
Tadalafil, 5 mg, and placebo were otherwise identical formulations prepared and supplied by Eli Lilly. Drug use met criteria described under the Title 21 CFR 312.2(b) exemption. Participants started taking either tadalafil or placebo orally within 7 days after the initiation of external radiotherapy or the date of brachytherapy. The requisite number of pills was given to the participant in 3 allotments, which were at the beginning of treatment and at the second and 13th weeks. Administration was to continue for 24 consecutive weeks (168 days).
Either external radiotherapy or low-dose-rate brachytherapy was to start within 6 weeks after randomization. Member sites had met quality assurance guidelines assessed by the Radiological Physics Center (Houston, Texas). External radiotherapy used 3-dimensional conformal or intensity-modulated technique based on computed tomography to identify prostate and pelvic anatomy. International Commission on Radiation Units and Measurements Report No. 50 definitions were used to specify the treatment volume and prescribe dose. The target was the prostate with a 3-dimensional expansion of 0.5 to 1.0 cm, with dose specified such that 98% or more of this volume received between 75.0 and 79.2 Gy in daily dose fractions of between 1.8 and 2.0 Gy administered over 7½ to 9 weeks. Constraints to limit dose to bladder, rectum, femoral heads, and corpus spongiosum were provided, with 50% or less of the corpus spongiosum to receive more than 52.5 Gy. Brachytherapy used permanently implanted, low-dose-rate sealed-source iodine 125 or palladium 103 as an alternative to external radiotherapy. The prostate with a 0.2- to 0.5-cm expansion was to receive 145 Gy (iodine 125) or 125 Gy (palladium 103) prescribed according to the American Association of Physicists in Medicine Task Group No. 40 Report. Computed tomography was obtained within 5 weeks of implantation. The combination of brachytherapy and external radiotherapy and the use of high-dose-rate brachytherapy or of androgen suppression was prohibited.
Assessments
The International Index of Erectile Function, a 15-item questionnaire with an overall score that ranges from 5 to 75, includes the following domains: erectile function (overall range, 1–30; severe, 1–10; moderate, 11–17; 18–25, mild; and 26–30, no ED),13 orgasmic function (range, 0–10), sexual desire (range, 2–10), intercourse satisfaction (range, 0–15), and overall satisfaction (range, 2–10).11 The Sexual Adjustment Questionnaire is a 20-item questionnaire with an overall score range between 8 and 100 including the following domains: desire, ranging between 5 and 30; dysfunction, 0 and 25; activity, 0 and 10; satisfaction, 1 and 10; and fatigue, 1 and 5.14 The Locke Marital Adjustment Test is a 16-item questionnaire with scores ranging from 48 to 138 for participants and 50 to 138 for partners.15 Higher scores indicate greater sexual function, sexual well-being, or marital adjustment.
Participants were seen with their pill containers and diaries at weeks 2 and 13 to evaluate adherence, record all medications, and assess adverse effects. Any pills not used by each visit were returned to the member site, and the next allotment was dispensed. During the 24-week treatment phase, participants were to complete the International Index of Erectile Function at weeks 2 and 4 and between weeks 20 and 24. The Sexual Adjustment Questionnaire and Locke Marital Adjustment Test results were collected between weeks 20 and 24 from participants who had consented.
After treatment, a pill count was performed between weeks 28 and 30, and the pill diary and any unused pills were collected. The International Index of Erectile Function, Sexual Adjustment Questionnaire, Locke Marital Adjustment Test, serum testosterone levels, all medication usage, and adverse effects were assessed between weeks 28 and 30 and at 1 year. The sexual adjustment and marital adjustment questionnaires were to be completed by consenting partners between weeks 20 and 24 and 28 and 30 and at 1 year.
End Points
The primary end point was to determine whether tadalafil maintained spontaneous erections between weeks 28 and 30 after the start of radiotherapy, which was 4 to 6 weeks after tadalafil was stopped. Participants maintained erectile function if their answer to the question “How often were you able to get an erection during sexual activity?” was “about half the time” or more (score range, 3–5). Those who answered “much less than half the time” were considered to have ED (score range, 0–2). Spontaneous erection at 1 year was a secondary end point. Other secondary end points assessed the men’s overall sexual function, sexual satisfaction, and marital adjustment and their partners’ sexual satisfaction and marital adjustment between weeks 28 and 30 and at 1 year. Patient-related factors predictive of response to tadalafil and adverse events based on the NCI Common Terminology Criteria for Adverse Events version 4 also were assessed between weeks 28 and30 and at 1 year.
Statistical Considerations
Sample size was determined to detect maintenance of spontaneous (off-drug) erectile function of 20% with placebo assignment vs 40% with tadalafil, a doubling of the placebo rate,3 based on a modified intent-to-treat 2-sided Fisher test with α of .05. Assuming 15% attrition, 218 participants accrued over 27 months were needed. Erectile function trends over time were modeled using the generalized estimation equation.16 Missing items were imputed using multiple imputation. The stratification variables were used for planned subgroup analyses. SAS version 9.2 (SAS Institute Inc) software was used for statistical computations.
Missing Sexual Adjustment Questionnaire values were imputed using the average of completed items. Differences in overall sexual function and satisfaction and marital adjustment scores were assessed with a 2-sided t test or Wilcoxon rank sum (with small samples) at .05 significance, and trends over time used the general linear mixed model adjusting for covariates.17 Spearman correlation with bootstrap18 to adjust for multiple assessments was used to identify associations between patient and partner sexual satisfaction and marital adjustment within and across treatment assignment. Factors potentially associated with spontaneous erectile function were evaluated with logistic regression. No adjustments were made to address secondary hypotheses.
Results
Demographic Characteristics
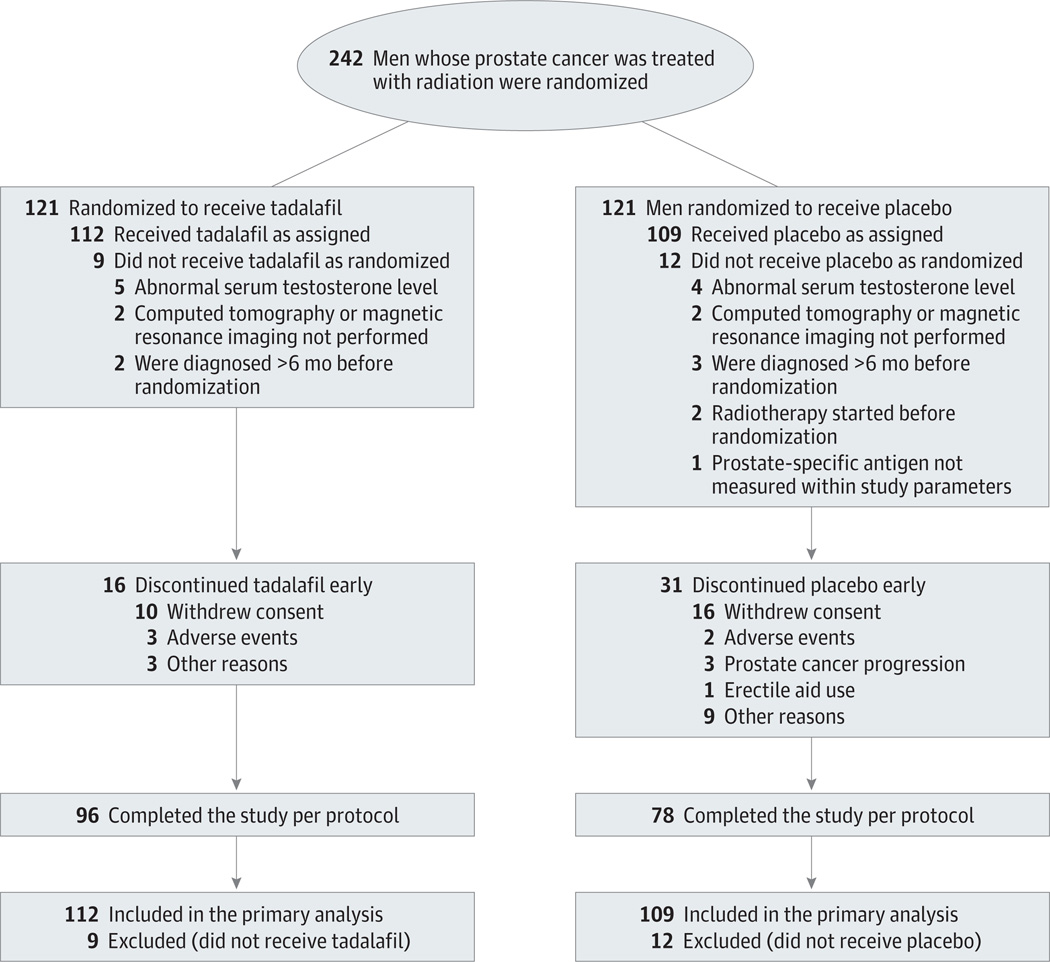
Between November 2009 and February 2012, 242 participants enrolled with 121 allocated to each assignment, as shown in Figure 1. Exclusions were mainly for testing not performed within the required time frame (48%) or an abnormal serum testosterone level (43%). The baseline characteristics of 221 fully eligible participants (112 tadalafil and 109 placebo) are provided in Table 1. Fourteen percent were actively smoking tobacco. Baseline characteristics were balanced well, with no significant between-group differences. Intensity modulation was used in 98% of those treated with external radiotherapy; the median dose administered was 78.0 Gy (range, 75–81 Gy). The median dose to 50% of the corpus spongiosum was 14.6 Gy (range, 0–80.8 Gy) for tadalafil and 24.0 Gy (range, 0–80.2 Gy) for placebo. Iodine 125 was used in 85% of brachytherapy-treated participants with palladium 103 used for the remainder.The median brachytherapy dose to 50% of the corpus spongiosum was 22.6 Gy (range, 0–256.3 Gy for tadalafil) and 25.0 Gy (range, 0–239.6 Gy for placebo).
Figure 1. Enrollment, Randomization, and Follow-up of the Study Participants.
The number of patients screened and assessed for eligibility was not recorded.
Table 1.
Baseline Demographic and Clinical Characteristics of Participantsa
| Characteristic | No. (%) of Men | |
|---|---|---|
| Tadalafil + Radiotherapy (n = 112) |
Placebo + Radiotherapy (n = 109) |
|
| Age, median (range), y | 63 (45–80) | 63 (48–79) |
| ≤65 | 76 (68) | 71 (65) |
| Zubrod Performance Status scoreb | ||
| 0 | 106 (95) | 104 (95) |
| 1 | 6 (5) | 5 (5) |
| Race | ||
| Black | 22 (20) | 29 (27) |
| Asian | 1 (1) | 2 (2) |
| White | 87 (78) | 73 (67) |
| Other | 2 (2) | 5 (5) |
| Tumor stage | ||
| T1c | 87 (78) | 89 (82) |
| T2 | 25 (22) | 20 (18) |
| Gleason score | ||
| 2–6 | 80 (71) | 73 (67) |
| >6 | 32 (29) | 36 (33) |
| Serum PSA, median (range), ng/mL | 5.8 (0.4–19.2) | 5.7 (0.5–19.0) |
| Prior PDE5-i use | 24 (21) | 23 (21) |
| Erectile function score at baselinec | ||
| Overall score, mean (95% CI) | 60.8 (58.6–63.0) | 60.8 (58.7–62.9) |
| Sometimesd | 25 (22) | 22 (20) |
| Most timesd | 27 (24) | 24 (22) |
| Almost always/alwaysd | 60 (54) | 63 (58) |
| Radiotherapy | ||
| External | 72 (64) | 67 (62) |
| Brachytherapy | 40 (36) | 42 (38) |
Abbreviations: PDE5-i, phosphodiesterase-5 inhibitor; PSA, prostate-specific antigen.
Differences in baseline characteristics between groups were not significant (P > .05) based on χ2 test or Wilcoxon rank sum test.
Score 0 indicates fully active without restriction; score 1, restricted in physically strenuous activity.
International Index of Erectile Function assessment.
Response to International Index of Erectile Function question 1: “How often were you able to get an erection during sexual activity?”
Adherence
Radiotherapy details were available for 96% of participants. Radiotherapy was completed per protocol in 98% of participants assigned to tadalafil and in 97% assigned to placebo. Five participants refused or selected other treatments. Ninety-six participants (86%) completed tadalafil, 10 withdrew consent, and 6 did not complete tadalafil because of adverse effects or other reasons. Seventy-eight participants (72%) completed placebo, 15 did not, and 16 withdrew consent. The average number of pills taken was 158 (95% CI, 142–174) for the tadalafil group and 163 (95% CI, 147–179) for the placebo group. Participant adherence with completing the erectile function, sexual satisfaction, and marital adjustment assessment instruments over time is shown in Table 2. The completion rate generally declined, although adherence with the erectile function assessment increased at the 30-week primary end point compared with the 24-week assessment (Figure 2).
Table 2.
Erectile Function and Sexual and Marital Adjustment of Participantsa
| Mean (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Tadalafil + Radiotherapy | Placebo + Radiotherapy | |||||
| Baseline | Weeks | Baseline | Weeks | |||
| 30 | 52 | 30 | 52 | |||
| Erectile functionb | ||||||
| Respondents, No. (%)c | 109 (100) | 75 (69) | 51 (47) | 108 (100) | 58 (54) | 45 (42) |
| Overall score | 60.8 (58.6–63.0) | 52.3 (48.6–56.4) | 50.9 (45.7–56.1) | 60.8 (58.7–62.9) | 52.2 (48.3–57.3) | 51.0 (45.0–57.0) |
| Erectile function | 24.8 (23.8–25.8) | 20.7 (18.8–22.6) | 21.2 (18.8–23.5) | 25.1 (24.2–26.0) | 20.9 (18.8–23.0) | 20.4 (17.7–23.1) |
| Orgasmic function | 8.9 (8.5–9.2) | 7.2 (6.5–7.8) | 7.0 (6.1–7.9) | 8.7 (8.3–9.0) | 7.4 (6.6–8.2) | 7.3 (6.4–8.2) |
| Sexual desire | 7.7 (7.5–8.0) | 7.2 (6.9–7.6) | 7.0 (6.5–7.5) | 7.8 (7.5–8.1) | 6.9 (6.4–7.4) | 6.8 (6.1–7.4) |
| Intercourse satisfaction | 11.1 (10.5–11.7) | 9.7 (8.8–10.6) | 9.5 (8.2–10.7) | 11.2 (10.6–11.7) | 9.4 (8.3–10.4) | 9.8 (8.5–11.1) |
| Overall satisfaction | 8.4 (8.0–8.7) | 7.3 (6.9–7.8) | 7.1 (6.5–7.7) | 8.2 (7.9–8.5) | 7.3 (6.8–7.9) | 7.2 (6.5–7.9) |
| Sexual adjustmentd | ||||||
| Respondents, No. (%) | 63 (100) | 47 (74) | 36 (57) | 51 (100) | 35 (68) | 24 (47) |
| Overall score | 65.2 (62.9–67.4) | 63.6 (61.4–65.8) | 62.6 (60.3–64.8) | 65.3 (62.6–67.9) | 63.0 (61.5–64.5) | 62.8 (60.6–64.9) |
| Desire | 21.9 (21.1–22.7) | 22.4 (21.5–23.3) | 22.6 (21.4–23.7) | 22.6 (21.7–23.5) | 21.9 (20.9–22.9) | 21.4 (20.0–22.8) |
| Dysfunction | 16.0 (15.2–16.7) | 13.1 (12.2–14.1) | 13.1 (12.1–14.0) | 16.1 (15.1–17.0) | 13.7 (12.8–14.5) | 13.3 (12.3–14.4) |
| Activity | 5.7 (5.0–6.3) | 6.8 (6.2–7.5) | 6.2 (5.4–7.0) | 5.4 (4.7–6.0) | 6.5 (5.9–7.2) | 6.0 (5.0–6.9) |
| Satisfaction | 7.9 (7.5–8.3) | 7.4 (6.8–7.9) | 7.0 (6.3–7.7) | 8.2 (7.8–8.5) | 7.3 (6.7–7.8) | 7.2 (6.4–7.9) |
| Fatigue | 3.7 (3.5–3.9) | 2.1 (1.9–2.4) | 2.4 (2.1–2.7) | 3.7 (3.4–3.9) | 2.2 (1.9–2.4) | 2.4 (1.9–2.8) |
| Marital adjustmente | ||||||
| Respondents, No. (%) | 61 (100) | 35 (57) | 22 (36) | 60 (100) | 29 (48) | 23 (38) |
| Overall score | 94.5 (91.7–97.3) | 92.3 (88.2–96.5) | 95.4 (91.7–99.0) | 92.4 (89.1–95.7) | 91.9 (86.7–97.1) | 94.0 (88.5–99.5) |
Response values represent group mean (95% CI) at the specified times; comparisons of mean values (tadalafil vs placebo) are not significant (P > .05) at any time point overall or within a specific domain. Higher values indicate improved function or well-being.
Based on the International Index of Erectile Function.
Three participants assigned tadalafil and 1 assigned placebo did not respond to all 15 items.
Based on the Sexual Adjustment Questionnaire.
Based on the Locke Marital Adjustment Test.
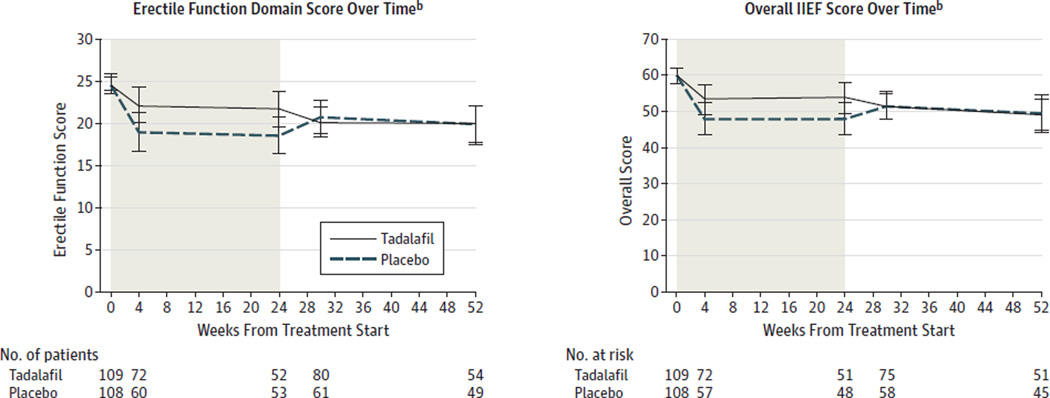
Figure 2. Sexual Function of Participants Over Timea.
Shaded areas represent period during which participants were to take assigned pills. Plot lines indicate group mean values; error bars, 95% CIs.
aAssessed by the International Index of Erectile Function (IIEF).
bThree participants assigned tadalafil and 1 assigned placebo did not respond to all items.
Outcomes
Analysis was conducted on all data collected through March 2013, representing 1-year minimal potential follow-up. The primary outcome was participant-reported spontaneous erectile function assessed by International Index of Erectile Function question 1 response 6 weeks after scheduled completion of the study agent. This was a median of 21 weeks (range, 16–27 weeks) after external radiotherapy and 30 weeks (range, 26–36 weeks) after brachytherapy. Seventy-nine percent (95% CI, 70%–88%) of participants assigned tadalafil retained erectile function, whereas retention was 74% (95%CI, 63%–85%) with placebo (P = .49); an absolute difference of 5% (95% CI, −9% to 19%). This did not support the design hypothesis of a 20% between-group difference. Covariate analysis adjusted for radiotherapy method and age likewise showed no tadalafil effect based on participant-reported responses (score increase, 0.51; 95% CI, −0.34 to 1.35 compared with placebo; P = .24) or imputed responses (score increase, 0.51; 95% CI, −0.20 to 1.22; P = .16). Participants 65 years of age or younger were more likely to retain erectile function than were those older than 65 years (score increase, 0.89; 95% CI, 0.01–1.78; P = .05) from a generalized estimating equation model. Radiotherapy method (external vs brachytherapy) and dose to the corpus spongiosum was not significantly associated with retained erectile function. Tadalafil did not result in a statistically significant difference in erectile function at 1 year, with 72% (95% CI, 60% −84%) of tadalafil-assigned participants reporting erectile function compared with 71% (95% CI, 59%–84%) assigned placebo (P = .93).
A statistically significant between-group difference in participant response to overall erectile function or sexual satisfaction at 28 to 30 weeks and at 1 year was not observed nor was a difference identified within any domain (Table 2). Age was the only factor associated with overall sexual function over time (imputed score, −4.59; 95% CI, −8.05 to −1.11 for age >65 years; P = .01). Sexual function of participants is shown in Figure 2. Treatment assignment did not significantly affect participant marital adjustment.
The partners of 42 men assigned tadalafil and 40 assigned placebo completed the baseline Sexual Adjustment Questionnaire for partners. No between-group differences were observed at baseline, at 28 to 30 weeks, or at 1 year; a correlation between participant and partner response was not found. Although 121 partners completed the baseline Locke Marital Adjustment Test, adherence at 28 to 30 weeks (31 partners) and at 1 year (28 partners) was low. A correlation between participant and partner response was noted at 28 to 30 weeks(P = .02) and at 1 year (P < .001), but differences between study agent assignment were not observed.
Adverse Effects
Adverse event grading reported the greatest severity incident at any time irrespective of its persistence or resolution subsequently. Sixty-five participants (59%; 95% CI, 49%–68%) had a mild or moderate (grade 1–2) adverse event attributed to tadalafil or radiotherapy, and 56 participants (52%, 95% CI, 42%–61%) assigned to placebo had such. Severe or life-threatening adverse events were observed in 3% (95% CI, 0%–6%) of tadalafil and 1% (95% CI, 0%–3%) of placebo participants. The number of participants with an adverse event definitely, probably, or possibly related to tadalafil or radiotherapy is shown in Table 3; some participants had multiple adverse events.
Table 3.
Common Terminology Criteria Adverse Eventsa
| No. (%) | ||||||
|---|---|---|---|---|---|---|
| Tadalafil + Radiotherapyb (n = 111)c |
Placebo + Radiotherapy (n = 108)c |
|||||
| Grade 1 | Grade 2 | Grade 3 | Grade 1 | Grade 2 | Grade 3 | |
| Renal and urinary | 33 (30) | 14 (13) | 2 (2) | 26 (24) | 15 (14) | 0 |
| Frequency | 25 (23) | 10 (9) | 0 | 21 (19) | 9 (8) | 0 |
| Urgency | 14 (13) | 6 (5) | 0 | 5 (5) | 2 (2) | 0 |
| Gastrointestinal | 20 (18) | 6 (5) | 1 (1) | 16 (15) | 2 (2) | 0 |
| Diarrhea | 12 (11) | 2 (2) | 0 | 6 (6) | 1 (1) | 0 |
| Proctitis | 2 (2) | 2 (2) | 1 (1) | 4 (4) | 1 (1) | 0 |
| Nervous system | 11 (10) | 0 | 1 (1) | 3 (3) | 0 | 0 |
| Headache | 8 (7) | 0 | 0 | 3 (3) | 0 | 0 |
| Reproductive | 10 (9) | 16 (14) | 0 | 6 (6) | 15 (14) | 1 (1) |
| Ejaculation | 5 (5) | 2 (2) | 0 | 3 (3) | 2 (2) | 0 |
| Erectile | 5 (5) | 16 (14) | 0 | 6 (6) | 13 (12) | 1 (1) |
| Eye | 3 (3) | 0 | 0 | 1 (1) | 0 | 0 |
| Vascular | 2 (2) | 2 (2) | 1 (1) | 0 | 0 | 0 |
| Cardiac | 1 (1) | 1 (1) | 0 | 0 | 0 | 0 |
| All othersb | 17 (15) | 3 (3) | 1 (1) | 4 (4) | 2 (2) | 0 |
Definitely, probably, or possibly related to treatment (radiotherapy or medication), or attribution unknown. Grade 1 indicates mild; grade 2, moderate; grade 3, severe; grade 4, life-threatening.
One patient with grade 4 adverse event (sepsis).
One participant in each group with missing data.
Discussion
Radiotherapy is a common treatment for prostate cancer,19 but ED may occur thereafter in a substantial proportion of patients.1,2 This is the first study to our knowledge to evaluate tadalafil for ED prevention in men treated with radiotherapy for prostate cancer. The International Index of Erectile Function was chosen to assess erectile function because it is the standard instrument for this type of outcomes research.13 The 15-item assessment is multidimensional, but it focuses heavily on (vaginal) penetration and intercourse, with only 2 items specific to erection alone.11 The direct effect of a phosphodiesterase-5 inhibitor is to promote penile erection, with secondary influence on other aspects of the sexual experience (eg, intercourse, satisfaction, relationship). But, men with prostate cancer are older than the general male population, so they may lack a sexual partner or one who participates in intercourse. Consequently, this study used the single question “How often were you able [over the past 4 weeks] to get an erection during sexual activity?”, which focused on spontaneous erectile function that may be independent of intercourse.
The US Food and Drug Administration approves prescribing 2.5 or 5 mg of tadalafil daily. Selection of 5 mg of tadalafil once daily in this study was well supported by its efficacy profile,20,21 its performance relative to other phosphodiesterase-5 inhibitor medications,7–9 and its pharmacological properties and mechanism of action.5 Despite the soundness of preliminary investigations, we found no benefit to tadalafil as an ED prevention agent after radiotherapy, with not even the slightest suggestion in this regard. This finding was noted across broad measures of outcomes, including the single-item, the erectile function domain, and the total score of the International Index of Erectile Function and the Sexual Assessment Questionnaire. Although tadalafil is indicated for treatment of ED after radiotherapy,3 its use as a preventive agent is not endorsed presently.
This study has several strengths supporting generalization of its results to men yet to receive radiotherapy for prostate cancer. The study group was racially diverse and recruited across a wide geographic distribution and spectrum of medical practices reflective of the population for whom this intervention was eventually intended. Radiotherapy was administered in a standardized manner that reflects current practice standards, which tightly conforms high radiation dose levels to the tumor-containing volume with sparing of erectile tissues.
Other published placebo-controlled studies of ED prevention used sildenafil22–24 or vardenafil25 in association with radiotherapy24 or surgery.22,23,25 These agents share a common mechanism of action with tadalafil, but their pharmacological properties result in intermittent, rather than continual, end-organ effects and erectogenic potential. Some studies observed benefit to scheduled use,22,23 whereas others did not.24,25 With one exception,25 these studies had methodological issues that limit the soundness of their conclusions, including small study cohorts,22–24 early study terminations,23,24 or ongoing daily phosphodiesterase-5 inhibitor use in the “preventive” group.22
The study by Montorsi et al25 merits special comment because it provides further insight into phosphodiesterase-5 inhibitor use as an ED preventive strategy after prostate cancer therapy. On-demand vardenafil after nerve-sparing prostatectomy improved erectile function and sexual encounters compared with placebo or scheduled once-nightly vardenafil. This was observed during the active 9-month treatment phase only, but it did not translate into improved spontaneous off-drug erectile function thereafter. The erectile function domain of the International Index of Erectile Function and questions 2 (vaginal penetration) and 3 (successful intercourse) of the Sexual Encounter Profile were used in that study, and both are influenced heavily by the act of sexual intercourse. The benefit of on-demand vardenafil to enhance sexual encounters is not unexpected7 because participants used vardenafil immediately before sexual activity and were able to titrate dosage to optimal effect. These observations suggest that scheduled, prophylactic phosphodiesterase-5 inhibitor use does not prevent ED, as noted likewise in our study. Montorsi et al25 also noted that an on-demand phosphodiesterase-5 inhibitor was equally effective as ED therapy in the 3 study assignment groups, which is consistent with its effects after radiotherapy also.3
Our study has limitations. First, testing of other tadalafil dosing schedules or other phosphodiesterase-5 inhibitor agents could yield different results, or a larger study cohort may identify a strategy preventive of radiotherapy-related ED in the future. Another limitation is that this study, as with other preventive and respondent-based studies, encountered substantial participant attrition by the time the primary end point was reached, a rate that exceeded the original design assumption. It is possible that the between-group imbalance in attrition masked a small benefit to tadalafil. Our study sought to detect a 20% between-group difference in spontaneous erectile function, but there was not sufficient statistical power to determine whether the 5% difference observed in our study cohort was significant. Lastly, it is possible that longer follow-up of participants in this trial may reveal a late-appearing benefit to tadalafil.
However, based on evidence available presently, there is no support for phosphodiesterase-5 inhibitor use to prevent ED after highly conformal external radiotherapy or low-dose-rate brachytherapy. Alternative strategies to prevent ED in this context appear warranted, perhaps with attention toward alternative dosing, investigation of neuroprotective interventions, or further refinements of radiotherapy delivery methods.
Conclusions
Among men undergoing radiotherapy for prostate cancer, daily use of tadalafil compared with placebo did not result in improved erectile function. These findings do not support the scheduled once-daily use of tadalafil to prevent ED in men undergoing radiotherapy for localized prostate cancer.
Acknowledgments
Dr Raben reported that he received consultancy and lecture payments from Bristol-Myers Squibb. Dr Buyyounouski reported that he received personal fees from Augmenix and General Electric Healthcare, and royalties from Amersys and Up-to-Date. Dr Kachnic reported that she gave expert testimony for Andrew Skinner Inc; received grants from the National Cancer Institute and lecture fees from the American Society for Radiation Oncology, American Society of Clinical Oncology, and Chartrounds TM; and earned royalties from Up-to-Date. Dr Bruner reported that she received grants from the National Cancer Institute and Eli Lilly & Co and travel support from the Community Clinical Oncology Program.
Funding/Support: This trial was conducted by the Radiation Therapy Oncology Group, which was supported by grant U10 CA21661 and by grant U10 CA37422 (Community Clinical Oncology Program) from the National Cancer Institute and by Eli Lilly & Co.
Role of the Sponsors: The study was approved and sponsored by the National Cancer Institute. The Radiation Therapy Oncology Group is solely responsible for the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Drs Bruner and Pugh had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Pisansky, Greenberg, Bruner.
Acquisition, analysis, or interpretation of data: Pisansky, Pugh, Greenberg, Pervez, Reed, Rosenthal, Mowat, Raben, Buyyounouski, Kachnic, Bruner.
Drafting of the manuscript: Pisansky, Pugh, Bruner.
Critical revision of the manuscript for important intellectual content: Pisansky, Pugh, Greenberg, Pervez, Reed, Rosenthal, Mowat, Raben, Buyyounouski, Kachnic, Bruner.
Statistical analysis: Pugh, Bruner.
Obtained funding: Bruner.
Administrative, technical, or material support: Pugh.
Study supervision: Pisansky, Pugh, Greenberg, Bruner.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No other disclosures were reported.
Disclaimers: The views presented herein are those solely of the Radiation Therapy Oncology Group and of the authors, who accept no liability for the consequences of any actions taken on the basis of information provided. This article’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute.
Previous Presentations: Presented in part at the Annual Meeting of the American Society of Clinical Oncology, Chicago, Illinois, May 31-June 4, 2013; and at the International Society for Quality of Life Research 20th Annual Conference, Miami, Florida, October 9–12, 2013.
Additional Contributions: Substantial contribution by nonauthors Snehal Deshmukh, MS, supporting statistician, for identifying and resolving data inconsistencies and providing data analysis; Roseann Bonanni, senior research associate, for developing report forms, Internet logistics, and data inquiries and validation; Dana Robinson, MEd, protocol associate, protocol development and regulatory compliance, for protocol development and management; and Denise Manfredi, BS, RT(T), radiotherapy dosimetry, for radiation therapy quality assurance, all of whom were compensated through the funding sources supporting this trial.
REFERENCES
- 1.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358(12):1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 2.Alemozaffar M, Regan MM, Cooperberg MR, et al. Prediction of erectile function following treatment for prostate cancer. JAMA. 2011;306(11):1205–1214. doi: 10.1001/jama.2011.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Incrocci L, Slagter C, Slob AK, Hop WCJ. A randomized, double-blind, placebo-controlled, cross-over study to assess the efficacy of tadalafil (Cialis) in the treatment of erectile dysfunction following three-dimensional conformal external-beam radiotherapy for prostatic carcinoma. Int J Radiat Oncol Biol Phys. 2006;66(2):439–444. doi: 10.1016/j.ijrobp.2006.04.047. [DOI] [PubMed] [Google Scholar]
- 4.Seftel AD, Buvat J, Althof SE, et al. Improvements in confidence, sexual relationship and satisfaction measures: results of a randomized trial of tadalafil 5 mg taken once daily. Int J Impot Res. 2009;21(4):240–248. doi: 10.1038/ijir.2009.22. [DOI] [PubMed] [Google Scholar]
- 5.Aversa A, Greco E, Bruzziches R, Pili M, Rosano G, Spera G. Relationship between chronic tadalafil administration and improvement of endothelial function in men with erectile dysfunction: a pilot study. Int J Impot Res. 2007;19(2):200–207. doi: 10.1038/sj.ijir.3901513. [DOI] [PubMed] [Google Scholar]
- 6.McMahon C. Comparison of efficacy, safety, and tolerability of on-demand tadalafil and daily dosed tadalafil for the treatment of erectile dysfunction. J Sex Med. 2005;2(3):415–425. doi: 10.1111/j.1743-6109.2005.20360.x. [DOI] [PubMed] [Google Scholar]
- 7.Martin-Morales A, Haro JM, Beardsworth A, Bertsch J, Kontodimas S EDOS Group. Therapeutic effectiveness and patient satisfaction after 6 months of treatment with tadalafil, sildenafil, and vardenafil: results from the erectile dysfunction observational study (EDOS) Eur Urol. 2007;51(2):541–550. doi: 10.1016/j.eururo.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 8.Eardley I, Mirone V, Montorsi F, et al. An open-label, multicentre, randomized, crossover study comparing sildenafil citrate and tadalafil for treating erectile dysfunction in men naïve to phosphodiesterase 5 inhibitor therapy. BJU Int. 2005;96(9):1323–1332. doi: 10.1111/j.1464-410X.2005.05892.x. [DOI] [PubMed] [Google Scholar]
- 9.Mirone V, Fusco F, Rossi A, Sicuteri R, Montorsi F. Tadalafil and vardenafil vs sildenafil: a review of patient-preference studies. BJU Int. 2009;103(9):1212–1217. doi: 10.1111/j.1464-410X.2008.08267.x. [DOI] [PubMed] [Google Scholar]
- 10.Greene FL, Page DL, Fleming ID, et al., editors. AJCC Cancer Staging Manual. 6th ed. New York, NY: Springer-Verlag; 2002. [Google Scholar]
- 11.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 12.Zelen M. The randomization and stratification of patients to clinical trials. J Chronic Dis. 1974;27(7–8):365–375. doi: 10.1016/0021-9681(74)90015-0. [DOI] [PubMed] [Google Scholar]
- 13.Porst H, Vardi Y, Akkus E, et al. Standards for clinical trials in male sexual dysfunctions. J Sex Med. 2010;7(1 pt 2):414–444. doi: 10.1111/j.1743-6109.2009.01623.x. [DOI] [PubMed] [Google Scholar]
- 14.Waterhouse J, Metcalfe MC. Development of the sexual adjustment questionnaire. Oncol Nurs Forum. 1986;13(3):53–59. [PubMed] [Google Scholar]
- 15.Kimmel D, van der Veer F. Factors of marital adjustment in Locke’s Marital Adjustment Test. J Marital Fam Ther. 1974;36(1):57–62. [Google Scholar]
- 16.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 17.Verbecke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York, NY: Springer-Verlag, Inc; 2000. [Google Scholar]
- 18.Henderson AR. The bootstrap: a technique for data-driven statistics: using computer-intensive analyses to explore experimental data. Clin Chim Acta. 2005;359(1–2):1–26. doi: 10.1016/j.cccn.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 19.Wong YN, Mitra N, Hudes G, et al. Survival associated with treatment vs observation of localized prostate cancer in elderly men. JAMA. 2006;296(22):2683–2693. doi: 10.1001/jama.296.22.2683. [DOI] [PubMed] [Google Scholar]
- 20.Porst H, Giuliano F, Glina S, et al. Evaluation of the efficacy and safety of once-a-day dosing of tadalafil 5 mg and 10 mg in the treatment of erectile dysfunction: results of a multicenter, randomized, double-blind, placebo-controlled trial. Eur Urol. 2006;50(2):351–359. doi: 10.1016/j.eururo.2006.02.052. [DOI] [PubMed] [Google Scholar]
- 21.Egerdie RB, Auerbach S, Roehrborn CG, et al. Tadalafil 2.5 or 5 mg administered once daily for 12 weeks in men with both erectile dysfunction and signs and symptoms of benign prostatic hyperplasia: results of a randomized, placebo-controlled, double-blind study. J Sex Med. 2012;9(1):271–281. doi: 10.1111/j.1743-6109.2011.02504.x. [DOI] [PubMed] [Google Scholar]
- 22.Bannowsky A, Schulze H, van der Horst C, Hautmann S, Jünemann KP. Recovery of erectile function after nerve-sparing radical prostatectomy: improvement with nightly low-dose sildenafil. BJU Int. 2008;101(10):1279–1283. doi: 10.1111/j.1464-410X.2008.07515.x. [DOI] [PubMed] [Google Scholar]
- 23.Padma-Nathan H, McCullough AR, Levine LA, et al. Study Group. Randomized, double-blind, placebo-controlled study of postoperative nightly sildenafil citrate for the prevention of erectile dysfunction after bilateral nerve-sparing radical prostatectomy. Int J Impot Res. 2008;20(5):479–486. doi: 10.1038/ijir.2008.33. [DOI] [PubMed] [Google Scholar]
- 24.Ilic D, Hindson B, Duchesne G, Millar JL. A randomised, double-blind, placebo-controlled trial of nightly sildenafil citrate to preserve erectile function after radiation treatment for prostate cancer. J Med Imaging Radiat Oncol. 2013;57(1):81–88. doi: 10.1111/j.1754-9485.2012.02461.x. [DOI] [PubMed] [Google Scholar]
- 25.Montorsi F, Brock G, Lee J, et al. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol. 2008;54(4):924–931. doi: 10.1016/j.eururo.2008.06.083. [DOI] [PubMed] [Google Scholar]