Abstract
Paclitaxel is one of the most effective chemotherapeutic agents for treating various types of cancer. However, the clinical application of paclitaxel in cancer treatment is considerably limited due to its poor water solubility and low therapeutic index. Thus, it requires an urgent solution to improve therapeutic efficacy of paclitaxel. In this study, folate decorated paclitaxel loaded PLA–TPGS nanoparticles were prepared by a modified emulsification/solvent evaporation method. The obtained nanoparticles were characterized by Field Emission Scanning Electron Microscopy (FESEM), Fourier Transform Infrared (FTIR) and Dynamic Light Scattering (DLS) method. The spherical nanoparticles were around 50 nm in size with a narrow size distribution. Targeting effect of nanoparticles was investigated in vitro on cancer cell line and in vivo on tumor bearing nude mouse. The results indicated the effective targeting of folate decorated paclitaxel loaded copolymer nanoparticles on cancer cells both in vitro and in vivo.
Keywords: Paclitaxel (PTX), Copolymeric micelle, PLA–TPGS, Fol/PTX/PLA–TPGS NPs
1. Introduction
Paclitaxel (PTX), isolated from the bark of Taxus brevifolia, is one of the most effective chemotherapeutic agents for treating various types of cancers, including ovarian, breast, colon, bladder, esophagus, lung, multiple myeloma and Kaposi’s sarcoma (Singla et al., 2002). However, because of poor aqueous solubility and low therapeutic index, the clinical application of PTX is still limited. Current commercial formulations of PTX with Cremophor EL (Taxol®) and albumin (Abraxane®) result in many severe side effects such as hypersensitivity reactions, neurotoxicity, nephrotoxicity, low red blood cell count, stomatitis, and ocular toxicity (Singla et al., 2002, Miele et al., 2009). Many attempts, therefore, have been made to develop new drug delivery systems (DDSs), such as liposomes (Biswas et al., 2012), polymer–drug conjugates (Meerum Terwogt et al., 2001), lipid-based nanoparticles (Arica Yegin et al., 2006), and copolymeric micelles (Zhang et al., 2011). The advantage of these DDSs compared to conventional DDSs is based on their nano-size which improves the drug accumulation at the tumor site in a passive manner, known as the Enhanced Permeability and Retention (EPR) effect (Dan et al., 2007). Among them, copolymeric micelles have attached a great deal of attention thanks to its highly structural stability, small size and drug controlled release (Deng et al., 2012).
Amphiphilic copolymers are composed of hydrophobic and hydrophilic segments. In aqueous environment, they can self-assemble into core–shell structures (Miyata et al., 2011), called copolymeric micelles. The hydrophobic core can be served as microenvironment for incorporating hydrophobic drugs and protecting them from chemical degradation while the shell helps in stabilizing and improving retention time of micelles in circulatory systems.
In the last decades, biodegradable polymers such as poly(caprolactone) (PCL) and poly(lactide) (PLA) were widely used for the preparation of drug carrier. However, their hydrophobic characteristics and low degradation rate become barriers to produce advanced DDSs. Introduction of hydrophilic polymer such as poly(ethylene glycol) (PEG) or tocopheryl polyethylene glycol 1000 succinate (TPGS) can increase the degradation rate, decrease the hydrophobicity of these polymer carrier and produce novel copolymeric micelle systems (Li et al., 2010, Xiao et al., 2010).
For enhancing the intracellular delivery of DDSs to specific cancer cell in an active manner, the most widely utilized approach is to conjugate with targeting ligands, such as folic acid, aptamers, peptides and antibodies (Byrne et al., 2008). Among them, folic acid has high binding affinity to folate receptors which are overexpressed on cell surface of many human tumors while it highly restricted in normal tissue. Conjugation of folate to DDSs, therefore, facilitated their cellular uptake on cancer cells via an endocytic process and avoided non-specific attacks on normal tissues (Lu and Low, 2002). Pen et.al reported that PTX nano-formulation using folate decorated PLA–TPGS copolymer with the size around 300 nm induced better in vitro targeting effect compared to that of PTX (Pan and Feng, 2008). However, in vivo experiments were not studied. Recent study showed that the optimal size of drug delivery system should be 50 nm that balances extravasation, inward permeation inside tumor tissues, tumor cell internalization, and outward diffusion and clearance from tumor to retain the highest effective drug concentrations in tumors (Tang et al., 2014).
In this study, we prepared folate decorated paclitaxel loaded PLA–TPGS nanoparticles with the size around 50 nm and evaluated its targeting effect in vitro on cancer cells and in vivo on tumor bearing nude mouse.
2. Experimental details
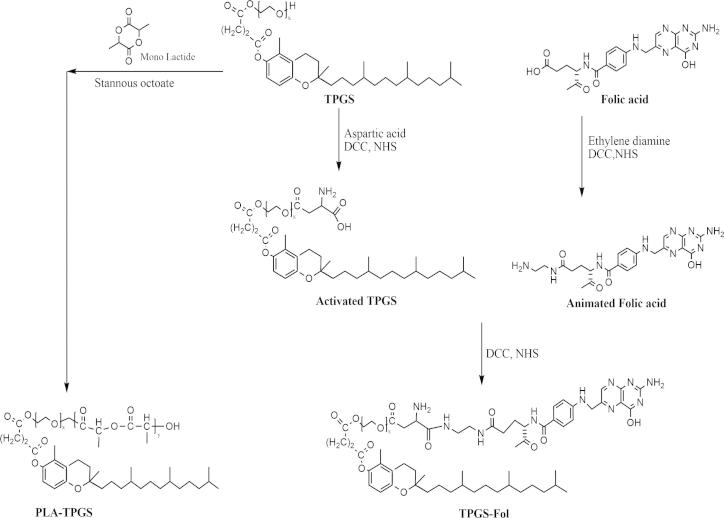
PLA–TPGS copolymer was synthesized by ring-opening method in the presence of stannous octoate as catalyst as described in our previous report (Fig. 1) (Thu et al., 2013). Briefly, a given amount of stannous octoate, PLA and TPGS (1:4 w/w) was dissolved in distilled toluene in an ampoule. The reaction was carried out for 10 h at 130 °C under inert gas atmosphere in a silicone oil bath. After the reaction time, the resultant mixture was gently stirred overnight to evaporate the organic solvent. The product was dissolved in dichloromethane and then precipitated in cold methanol in excess to remove unreacted lactide monomers and TPGS. The final product was obtained by filtration.
Figure 1.
Schematic diagram of polymer synthesis.
Folate was covalently attached to TPGS molecules through a modified process described by Pan and Feng (2008). Firstly, TPGS was activated with aspartic acid instead of glutamic acid through the esterification between the hydroxyl group of TPGS and carboxyl group of aspartic acid. Next, folic acid was animated with ethylene diamine through the formation of an amide bridge. Finally, the activated TPGS was reacted with the animated folic acid to form folate attached TPGS (TPGS–Fol) molecules. All reactions were performed in dimethyl sulfoxide (DMSO), under ambient temperature and in the presence of N-Hydroxysuccinimide (NHS) and N,N′-Dicyclohexylcarbodiimide (DCC) as catalysts (Fig. 1).
Folate decorated paclitaxel loaded PLA–TPGS nanoparticles (Fol/PTX/PLA–TPGS NPs) were prepared by a modified emulsification/ solvent evaporation process. In brief, the blend of PLA–TPGS and TPGS–Fol with the ratio of 5:1 (w/w) was dispersed in an aqueous solution containing 0.03% of TPGS as an emulsifier. Next, a given amount of PTX dissolved in dichloromethane (DCM) was added dropwise into the above solution under magnetic stirring at room temperature. After 48 h stirring, DCM was evaporated and the resulted mixture was centrifuged at 5000 rpm in 5 min. The obtained transparent solution was lyophilized. The lyophilized powder was collected and stored at 4 °C. Paclitaxel loaded PLA–TPGS nanoparticles (PTX/PLA–TPGS NPs) as reference sample were prepared in a similar manner.
The nanoparticles were characterized by FESEM, FTIR and DLS method. Targeting effect of nanoparticles was investigated in vitro on cancer cell line and in vivo on tumor bearing nude mouse.
3. Results and discussion
3.1. Characteristics of nanoparticles
Physicochemical characteristic of nanoparticles was investigated by FTIR (Fig. 2). In the FTIR spectrum of PTX/PLA–TPGS, peak at 1716 cm−1 was attributed to the overlap of C O stretching of PTX at 1712 cm−1 and PLA–TPGS at 1756 cm−1. Characteristic peaks of PTX at 1648 cm−1 (C—C stretching), 1245 cm−1 (C—N stretching), 1074 cm−1 (C—O stretching) (Devi and Gayathri, 2010) were shifted to 1640, 1240, 1069 cm−1, respectively. The presence of peak at 1531 cm−1 was assigned to the absorption band at 1546 cm−1 of aromatic ring of PLA–TPGS. In the FTIR spectrum of Fol/PTX/PLA–TPGS, compared to that of PTX/PLA–TPGS, characteristic peaks of PTX/PLA–TPGS at 1716, 1640, 1240, 1069 cm−1 were shifted to 1677, 1616, 1230, 1064 cm−1, respectively. In addition, the presence of peaks at 1590 cm−1 and 1480 cm−1 was attributed to N—H bending (1605 cm−1) and the absorption of phenyl ring (1485 cm−1) of folic acid (Zhang et al., 2008). All these data gave the evidence for the success in fabricating Fol/PTX/PLA–TPGS NPs.
Figure 2.
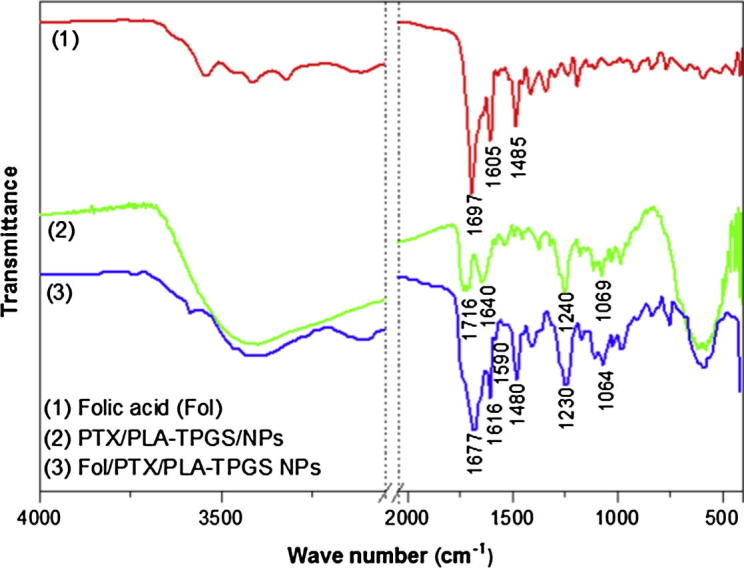
FTIR spectra of (1) folic acid, (2) PTX/PLA–TPGS NPs, and (3) Fol/PTX/PLA–TPGS NPs.
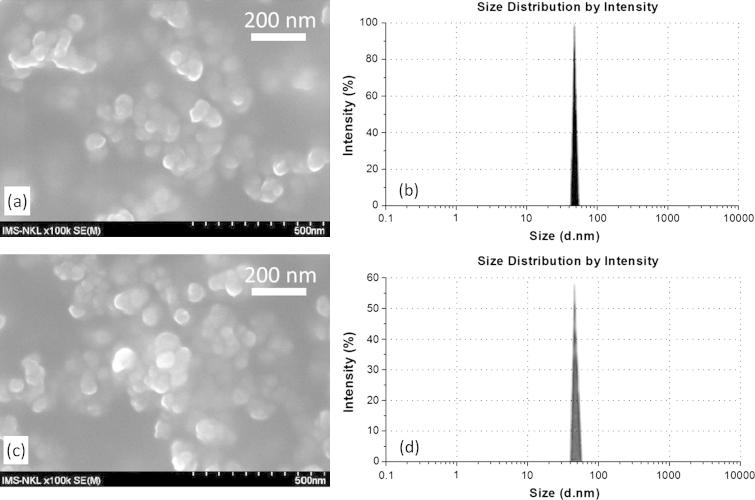
Fig. 3 shows the FESEM images and size distribution of nanoparticles. It can be seen that both PTX/PLA–TPGS NPs and Fol/PTX/PLA–TPGS NPs were spherical shape. There was no noticeable difference in size of these nanoparticles with the size around 50 nm. This result was confirmed by DLS method with the average size of about 55 nm and a narrow distribution. Recent study showed that nanoparticles with particle size below 50 nm induce the best therapeutic efficiency (Tang et al., 2014).
Figure 3.
FESEM image and size distribution of (a and b) PTX/PLA–TPGS NPs and (c and d) Fol/PTX/PLA–TPGS NPs.
3.2. In vitro targeting effect of nanoparticles on HeLa cell
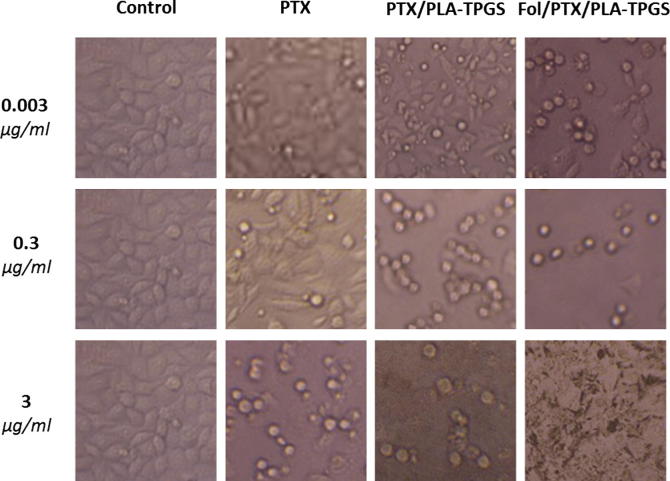
In vitro targeting effect of nanoparticles was investigated based on the quantitative evaluation of morphological change and on HeLa cell line. Our previous publication demonstrated that drug loaded PLA–TPGS nanoparticle induced better apoptosis on cancer cells than free drug through observation of cell morphological change (Thu et al., 2013). HeLa cells were incubated with PTX, PTX/PLA–TPGS NPs, and Fol/PTX/PLA–TPGS NPs and observed by inverted microscopy as shown in Fig. 4. After incubation for 48 h, there were obvious differences in testing samples.
Figure 4.
Morphological change in HeLa cells after 48 h of incubation with different PTX formulations.
At the PTX concentration as low as 0.003 μg/ml, the cancer cells incubated with PTX and PTX/PLA–TPGS NPs had no morphological change while that change was clearly visualized in cells incubated with Fol/PTX/PLA–TPGS NPs. The morphological change was observed more and more obviously when PTX concentration was increased. Compared to PTX, PTX/PLA–TPGS NPs and Fol/PTX/PLA NPs induced much more changes. At the PTX concentration of 3 μg/Ml, all cells were destroyed for Fol/PTX/PLA–TPGS NPs. These evidences demonstrated that PTX loaded nanoparticles induced better targeting effect than free PTX, in which the best effective targeting belonged to Fol/PTX/PLA NPs. This could be explained by an increased cell internalization of Fol/PTX/PLA–TPGS NPs via a folate-receptor-mediated endocytosis process. Folate decorated system would delivery many drug molecules when they were internalized by the cell via folate receptor-mediated endocytosis, causing higher drug concentration than that of non-folate systems which delivery drug via passive diffusion. Zhang et.al also found that folate decorated nanoparticles improve the cellular uptake of drug into cancer cells (Zhang et al., 2011).
3.3. In vivo targeting effect of nanoparticles
In vivo targeting effect of nanoparticles was evaluated by the tumor growth inhibition on colorectal tumor bearing nude mouse. PTX in different formulations (free PTX, PTX/PLA–TPGS NPs and Fol/PTX/PLA–TPGS NPs) was intravenously administrated into mouse. The concentration of PTX is the same in all formulations. Drug administration started on Day 0 and repeated every 7 days, for a total of six times. Tumor volume was measured every 7 days until Day 42. After 7 days of treatment, tumor volume of mouse in PTX formulations treated groups started becoming different compared to saline treated control group. Groups treated with PTX/PLA–TPGS NPs and Fol/PTX/PLA–TPGS NPs showed better tumor inhibitory effect compared with group treated with free PTX during the treatment time (Fig. 5).
Figure 5.
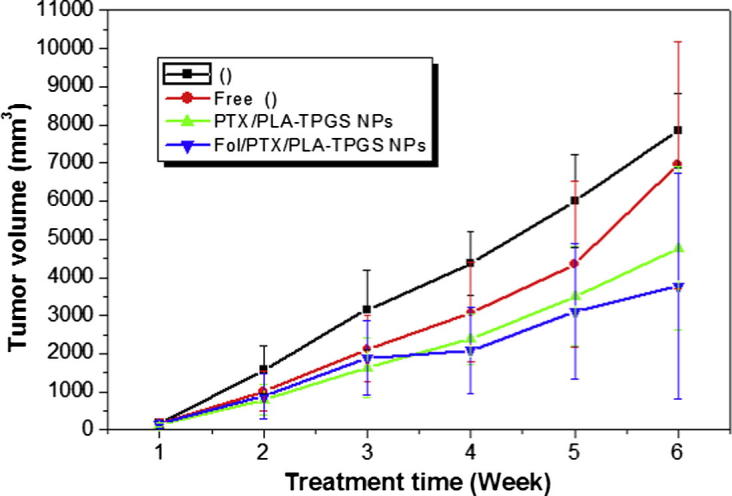
Tumor volume development during treatment time.
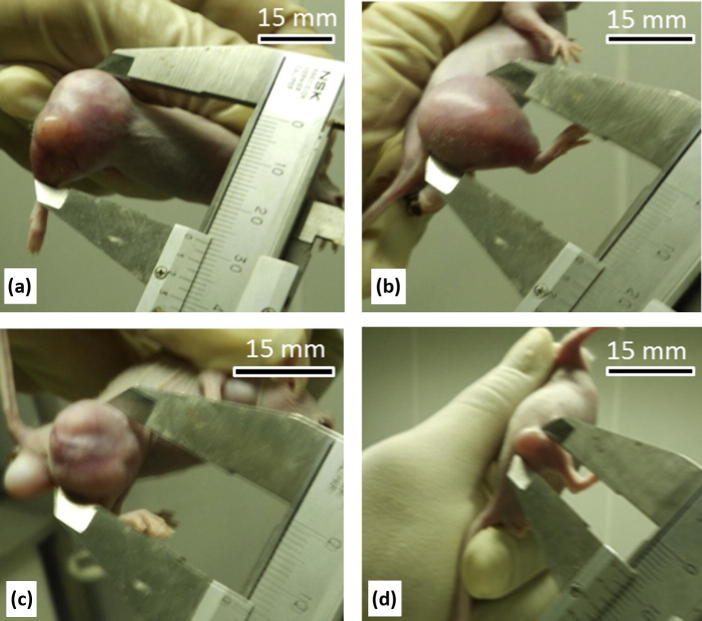
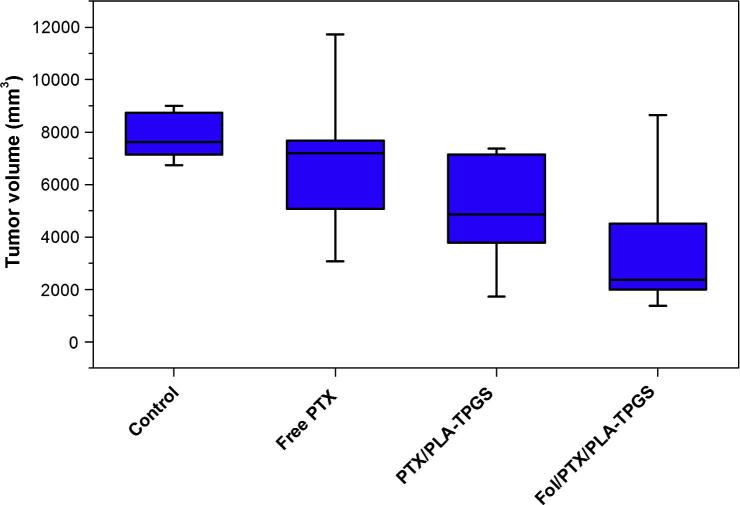
After 42 days of treatment, the Fol/PTX/PLA–TPGS NPs exhibited the best tumor growth inhibition (Figure 6, Figure 7).
Figure 6.
Tumor images of mouse after 42 days of treatment: (a) control, (b) Free PTX, (c) PTX/PLA–TPGS NPs and (d) Fol/PTX/PLA–TPGS NPs.
Figure 7.
Tumor volume of mouse after 42 days of treatment.
Significant tumor growth inhibition was probably due to the combination of two potential mechanisms: (i) Enhanced Permeability and Retention (EPR) effect; (ii) selective uptake by cancer cells through receptor- mediated endocytosis. The EPR effect was mediated by the small size of nanoparticles (50 nm) promoting the passive permeability at the tumor site and the PEG residue on the nanoparticle conferring the nanoparticles to remain in circulatory system for a longer duration. The receptor-mediated endocytosis was mainly due to the presence of folate moiety on Fol/PTX/PLA–TGPS NPs. After cell surface binding, the Fol/PTX/PLA–TPGS NPs might be internalized into the targeted cell via a folate receptor-mediated endocytosis instead of passive diffusion through the cell membrane. Consequently, higher PTX concentration would be achieved inside the cell causing better tumor growth inhibition.
4. Conclusions
In this study, Paclitaxel loaded nanoparticles composed by PLA–TPGS copolymer were successfully prepared by a simple modified modification/solvent evaporation method. Their targeting effect was evaluated by in vitro on cancer cells and in vivo on tumor bearing mouse. The results showed that PTX loaded nanoparticles exhibit great advantages compared to free PTX and the folate decoration significantly improve the targeted delivery of drug to cancer cell in both in vitro and in vivo.
Acknowledgments
This work was financially supported by L’Oréal-UNESCO For Women in Science, the Vietnam Academy of Science and Technology under Grant No. VAST03.03/13-14 (HPT) and the National Foundation for Science and Technology development of Vietnam-NAFOSTED under Grant No. 106.99-2012.43 (HPT).
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Ha Phuong Thu, Email: thuhp@ims.vast.ac.vn.
Duong Tuan Quang, Email: duongtuanquang@dhsphue.edu.vn.
References
- Arica Yegin B., Benoit J.P., Lamprecht A. Paclitaxel-ioaded lipid nanoparticles prepared by solvent injection or ultrasound emulsification. Drug Dev. Ind. Pharm. 2006;32:1089–1094. doi: 10.1080/03639040600683501. [DOI] [PubMed] [Google Scholar]
- Biswas S., Dodwadkar N.S., Deshpande P.P., Torchilin V.P. Liposomes loaded with paclitaxel and modified with novel triphenylphosphonium-PEG-PE conjugate possess low toxicity, target mitochondria and demonstrate enhanced antitumor effects in vitro and in vivo. J. Control Release. 2012;159:393–402. doi: 10.1016/j.jconrel.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne J.D., Betancourt T., Brannon-Peppas L. Active targeting schemes for nanoparticle systems in cancer therapeutics. Adv. Drug Deliv. Rev. 2008;60:1615–1626. doi: 10.1016/j.addr.2008.08.005. [DOI] [PubMed] [Google Scholar]
- Dan P., Jeffrey M.K., Seungpyo H., Omid C.F., Rimona M., Robert L. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2007;2:751–760. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- Deng C., Jiang Y., Cheng R., Meng F., Zhong Z. Biodegradable polymeric micelles for targeted and controlled anticancer drug delivery: promises, progress and prospects. Nano Today. 2012;7:467–480. [Google Scholar]
- Devi T.R., Gayathri S. FTIR and FT-Raman spectral analysis of paclitaxel drugs. Int. J. Pharm. Sci. Rev. Res. 2010;2:106–110. [Google Scholar]
- Li P.Y., Lai P.S., Hung W.C., Syu W.J. Poly(L-lactide)-vitamin E TPGS nanoparticles enhanced the cytotoxicity of doxorubicin in drug-resistant MCF-7 breast cancer cells. Biomacromolecules. 2010;11:2576–2582. doi: 10.1021/bm1005195. [DOI] [PubMed] [Google Scholar]
- Lu Y., Low P.S. Folate-mediated delivery of macromolecular anticancer therapeutic agents. Adv. Drug Deliv. Rev. 2002;54:675–693. doi: 10.1016/s0169-409x(02)00042-x. [DOI] [PubMed] [Google Scholar]
- Meerum Terwogt J.M., ten Bokkel Huinink W.W., Schellens J.H., Schot M., Mandjes I.A., Zurlo M.G., Rocchetti M., Rosing H., Koopman F.J., Beijnen J.H. Phase I clinical and pharmacokinetic study of PNU166945, a novel water-soluble polymer-conjugated prodrug of paclitaxel. Anticancer Drugs. 2001;12:315–323. doi: 10.1097/00001813-200104000-00003. [DOI] [PubMed] [Google Scholar]
- Miele E., Spinelli G.P., Tomao F., Tomao S. Albumin-bound formulation of paclitaxel (Abraxane ABI-007) in the treatment of breast cancer. Int. J. Nanomed. 2009;4:99–105. doi: 10.2147/ijn.s3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyata K., Christie R.J., Kataoka K. Polymeric micelles for nano-scale drug delivery. React. Funct. Polym. 2011;71:227–234. [Google Scholar]
- Pan J., Feng S.S. Targeted delivery of paclitaxel using folate-decorated poly(lactide)-vitamin E TPGS nanoparticles. Biomaterials. 2008;29:2663–2672. doi: 10.1016/j.biomaterials.2008.02.020. [DOI] [PubMed] [Google Scholar]
- Singla A.K., Garg A., Aggarwal D. Paclitaxel and its formulations. Int. J. Pharm. 2002;235:179–192. doi: 10.1016/s0378-5173(01)00986-3. [DOI] [PubMed] [Google Scholar]
- Tang L., Yang X., Yin Q., Cai K., Wang H., Chaudhury I., Yao C., Zhou Q., Kwon M., Hartman J.A., Dobrucki I.T., Dobrucki L.W., Borst L.B., Lezmi S., Helferich W.G., Ferguson A.L., Fan T.M., Cheng J. Investigating the optimal size of anticancer nanomedicine. Proc. Natl. Acad. Sci. 2014;111:15344–15349. doi: 10.1073/pnas.1411499111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thu H.P., Quang D.T., Trang M.T.T., Ha T.T.H., Nam N.H., Phuc N.X., Nguyet T.T.M., Thong P.Q., Tuyet P.T.H., Oanh V.T.K., Huong L.M. In vitro apoptosis enhancement of Hep-G2 cells by PLA–TPGS and PLA–PEG block copolymer encapsulated curcumin nanoparticles. Chem. Lett. 2013;42:255–267. [Google Scholar]
- Xiao R.Z., Zeng Z.W., Zhou G.L., Wang J.J., Li F.Z., Wang A.M. Recent advances in PEG–PLA block copolymer nanoparticles. Int. J. Nanomed. 2010;5:1057–1065. doi: 10.2147/IJN.S14912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Rana S., Srivastava R.S., Misra R.D.K. On the chemical synthesis and drug delivery response of folate receptor-activated, polyethylene glycol-functionalized magnetite nanoparticles. Acta Biomater. 2008;4:40–48. doi: 10.1016/j.actbio.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Zhang H., Li F., Yi J., Gu C., Fan L., Qiao Y., Tao Y., Cheng C., Wu H. Folate-decorated maleilated pullulan-doxorubicin conjugate for active tumor-targeted drug delivery. Eur. J. Pharm. Sci. 2011;42:517–526. doi: 10.1016/j.ejps.2011.02.006. [DOI] [PubMed] [Google Scholar]